Hypertriglyceridemia-Induced Acute Pancreatitis—The Milky Way Constellation—The Seven-Year Experience of a Large Tertiary Centre
Abstract
1. Introduction
1.1. Acute Pancreatitis
1.2. Hypertriglyceridemia
1.3. Study Aims
2. Materials and Methods
2.1. Bucharest Acute Pancreatitis Index (BUC-API) Registry
2.2. Case Selection
2.3. Statistical Tests
3. Results
3.1. Population Characteristics
3.2. Single Attack or Recurrence?
3.3. Severity
3.4. Age
3.5. ICU
3.6. Length of Stay
3.7. Morphology
3.8. Ward of Care
3.9. Other Aims
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ANC | Acute Necrotic Collection |
| AP | acute pancreatitis |
| APFC | Acute Peripancreatic Fluid Collection |
| ASR | adjusted standardized residuals |
| BUC-API | BUCharest Acute Pancreatitis Index |
| DCH | daily cost of hospitalization |
| DM | diabetes mellitus |
| EHR | electronic health records |
| HTG | hypertriglyceridemia |
| HTG-AP | hypertriglyceridemia-induced acute pancreatitis |
| ICD-10 | International Classification of Diseases 10th edition |
| ICU | Intensive Care Unit |
| LoS | length of stay |
| OAP | other-known cause acute pancreatitis |
| RAC | Revised Atlanta Classification |
| RON | ISO code for Romanian Leu (national currency) |
| SAP | severe acute pancreatitis |
| SIRS | Systemic Inflammatory Response Syndrome |
| TG | Triglycerides |
| WON | Walled-Off Necrosis |
References
- Jankowski, C. Pioneers of Light and Sound; Capstone: Mankato, MN, USA, 2009. [Google Scholar]
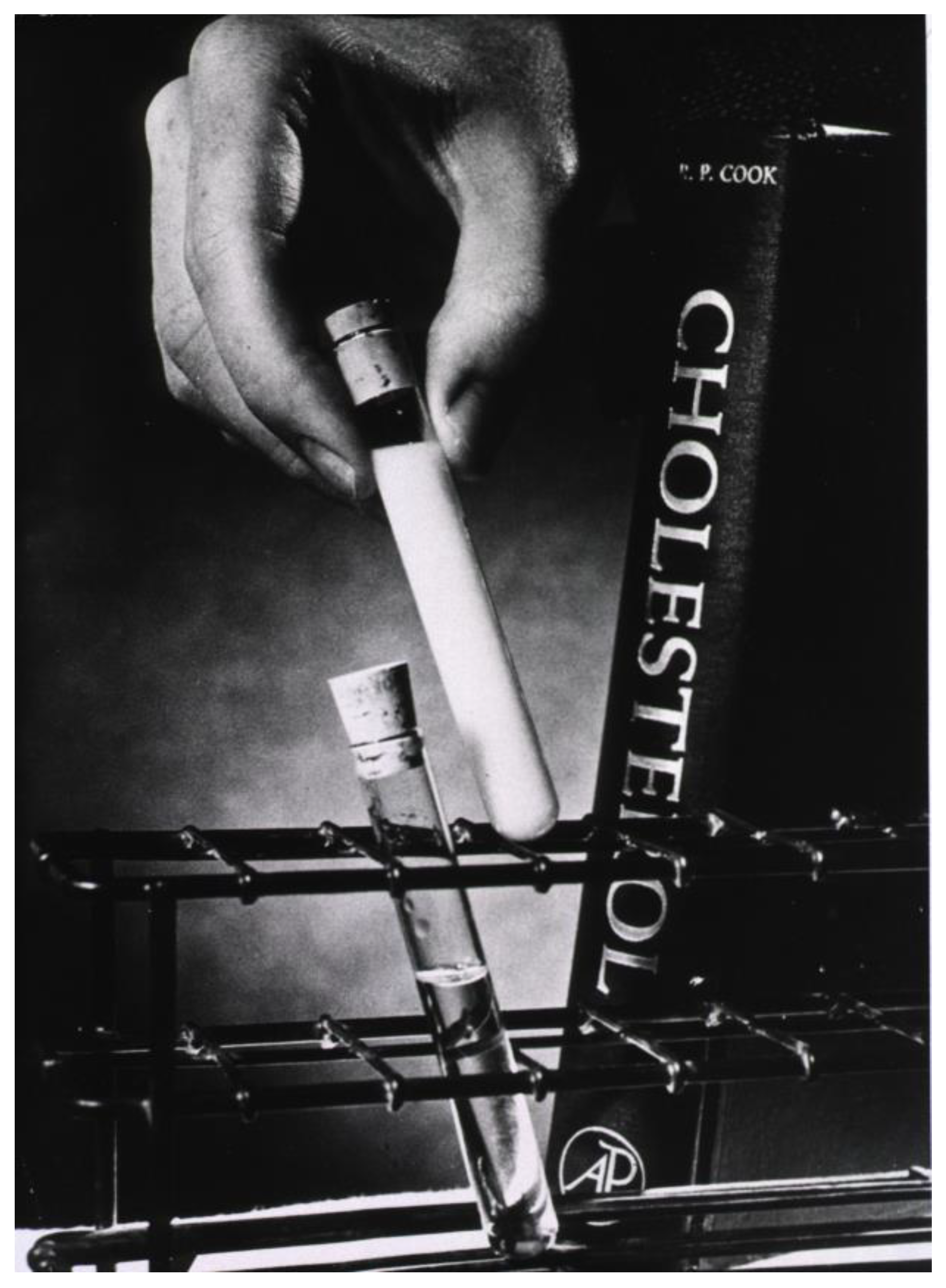
- Allen, T.M.; Viera, A.J. Milk-Like Serum Suggests Markedly Elevated Triglycerides. Am. Fam. Physician 2004, 70, 821. [Google Scholar] [PubMed]
- Iannuzzi, J.P.; King, J.A.; Leong, J.H.; Quan, J.; Windsor, J.W.; Tanyingoh, D.; Coward, S.; Forbes, N.; Heitman, S.J.; Shaheen, A.-A.; et al. Global Incidence of Acute Pancreatitis Is Increasing Over Time: A Systematic Review and Meta-Analysis. Gastroenterology 2022, 162, 122–134. [Google Scholar] [CrossRef] [PubMed]
- Ah-Tye, P.J. Pancreatitis in remote Australia: An indigenous perspective. Aust. J. Rural Health 2001, 9, 134–137. [Google Scholar] [CrossRef]
- Garg, S.K.; Sarvepalli, S.; Campbell, J.P.; Obaitan, I.; Singh, D.; Bazerbachi, F.; Singh, R.; Sanaka, M.R.M. Incidence, Admission Rates, and Predictors, and Economic Burden of Adult Emergency Visits for Acute Pancreatitis: Data from the National Emergency Department Sample, 2006 to 2012. J. Clin. Gastroenterol. 2019, 53, 220–225. [Google Scholar] [CrossRef]
- Ghiță, A.I.; Pahomeanu, M.R.; Negreanu, L. Epidemiological trends in acute pancreatitis: A retrospective cohort in a tertiary center over a seven year period. World J. Methodol. 2023, 13, 118–126. [Google Scholar] [CrossRef] [PubMed]
- Li, C.-L.; Jiang, M.; Pan, C.-Q.; Li, J.; Xu, L.-G. The global, regional, and national burden of acute pancreatitis in 204 countries and territories, 1990-2019. BMC Gastroenterol. 2021, 21, 332. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Popa, S.; Mota, M.; Popa, A.; Mota, E.; Timar, R.; Serafinceanu, C.; Cheta, D.; Graur, M.; Hancu, N. Prevalence of dyslipidemia and its association with cardiometabolic factors and kidney function in the adult Romanian population: The PREDATORR study. Diabetes Metab. Syndr. 2019, 13, 596–602. [Google Scholar] [CrossRef] [PubMed]
- Yang, A.L.; McNabb-Baltar, J. Hypertriglyceridemia and acute pancreatitis. Pancreatology 2020, 20, 795–800. [Google Scholar] [CrossRef] [PubMed]
- Balci, Z.; Kilic, M.O.; Senol, K.; Erdogan, A.; Tez, M. Prognostic scores in acute pancreatitis: A review. Acta Gastro-Enterol. Belg. 2016, 79, 337–347. [Google Scholar]
- Fagenholz, P.J.; Castillo, C.F.-D.; Harris, N.S.; Pelletier, A.J.; Camargo, C.A. Direct medical costs of acute pancreatitis hospitalizations in the United States. Pancreas 2007, 35, 302–307. [Google Scholar] [CrossRef]
- Ingraham, N.E.; King, S.; Proper, J.; Siegel, L.; Zolfaghari, E.J.; Murray, T.A.; Vakayil, V.; Sheka, A.; Feng, R.; Guzman, G.; et al. Morbidity and Mortality Trends of Pancreatitis: An Observational Study. Surg. Infect. 2021, 22, 1021–1030. [Google Scholar] [CrossRef] [PubMed]
- Mosztbacher, D.; Hanák, L.; Farkas, N.; Szentesi, A.; Mikó, A.; Bajor, J.; Sarlós, P.; Czimmer, J.; Vincze, Á.; Hegyi, P.J.; et al. Hypertriglyceridemia-induced acute pancreatitis: A prospective, multicenter, international cohort analysis of 716 acute pancreatitis cases. Pancreatology 2020, 20, 608–616. [Google Scholar] [CrossRef] [PubMed]
- Pulipati, V.P.; Brinton, E.A.; Hatipoglu, B. Management of Mild-to-Moderate Hypertriglyceridemia. Endocr. Pract. 2022, 28, 1187–1195. [Google Scholar] [CrossRef] [PubMed]
- Hypertriglyceridemia: Practice Essentials, Pathophysiology, Etiology. June 2023. Available online: https://emedicine.medscape.com/article/126568-overview (accessed on 30 July 2023).
- Carr, R.A.; Rejowski, B.J.; Cote, G.A.; Pitt, H.A.; Zyromski, N.J. Systematic review of hypertriglyceridemia-induced acute pancreatitis: A more virulent etiology? Pancreatology 2016, 16, 469–476. [Google Scholar] [CrossRef] [PubMed]
- Scherer, J.; Singh, V.; Pitchumoni, C.S.; Yadav, D. Issues in Hypertriglyceridemic Pancreatitis—An Update. J. Clin. Gastroenterol. 2014, 48, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S.; Braun, L.T.; de Ferranti, S.; Faiella-Tommasino, J.; Forman, D.E.; et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 139, E1082–E1143. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association. 14. Management of Diabetes in Pregnancy: Standards of Medical Care in Diabetes—2021. Diabetes Care 2021, 44 (Suppl. S1), S200–S210. [Google Scholar] [CrossRef]
- Banks, P.A.; Bollen, T.L.; Dervenis, C.; Gooszen, H.G.; Johnson, C.D.; Sarr, M.G.; Tsiotos, G.G.; Vege, S.S.; Acute Pancreatitis Classification Working Group. Classification of acute pancreatitis—2012: Revision of the Atlanta classification and definitions by international consensus. Gut 2013, 62, 102–111. [Google Scholar] [CrossRef] [PubMed]
- Zafrir, B.; Saliba, W.; Jubran, A.; Hijazi, R.; Shapira, C. Severe Hypertriglyceridemia-Related Pancreatitis: Characteristics and Predictors of Recurrence. Pancreas 2019, 48, 182–186. [Google Scholar] [CrossRef]
- Zheng, Y.; Zhou, Z.; Li, H.; Li, J.; Li, A.; Ma, B.; Zhang, T.; Liao, Q.; Ye, Y.; Zhang, Z.; et al. A Multicenter Study on Etiology of Acute Pancreatitis in Beijing During 5 Years. Pancreas 2015, 44, 409–414. [Google Scholar] [CrossRef]
- Kim, S.J.; Kang, H.; Kim, E.J.; Kim, Y.S.; Cho, J.H. Clinical features and outcomes of hypertriglyceridemia-induced acute pancreatitis: Propensity score matching analysis from a prospective acute pancreatitis registry. Pancreatology 2020, 20, 617–621. [Google Scholar] [CrossRef]
- Pothoulakis, I.; Paragomi, P.; Archibugi, L.; Tuft, M.; Talukdar, R.; Kochhar, R.; Goenka, M.K.; Gulla, A.; Singh, V.K.; Gonzalez, J.A.; et al. Clinical features of hypertriglyceridemia-induced acute pancreatitis in an international, multicenter, prospective cohort (APPRENTICE consortium). Pancreatology 2020, 20, 325–330. [Google Scholar] [CrossRef] [PubMed]
- Yin, G.; Cang, X.; Yu, G.; Hu, G.; Ni, J.; Xiong, J.; Hu, Y.; Xing, M.; Chen, C.; Huang, Y.; et al. Different Clinical Presentations of Hyperlipidemic Acute Pancreatitis: A Retrospective Study. Pancreas 2015, 44, 1105–1110. [Google Scholar] [CrossRef] [PubMed]
- Hajibandeh, S.; Jurdon, R.; Heaton, E.; Hajibandeh, S.; O’Reilly, D. The risk of recurrent pancreatitis after first episode of acute pancreatitis in relation to etiology and severity of disease: A systematic review, meta-analysis and meta-regression analysis. J. Gastroenterol. Hepatol. 2023, 38, 1718–1733. [Google Scholar] [CrossRef] [PubMed]
- Goyal, H.; Smith, B.; Bayer, C.; Rutherford, C.; Shelnut, D. Differences in severity and outcomes between hypertriglyceridemia and alcohol-induced pancreatitis. N. Am. J. Med. Sci. 2016, 8, 82–87. [Google Scholar] [CrossRef]
- Garg, R.; Rustagi, T. Management of Hypertriglyceridemia Induced Acute Pancreatitis. BioMed Res. Int. 2018, 2018, 4721357. [Google Scholar] [CrossRef]
- Jo, S.I.; Chang, J.H.; Kim, T.H.; Kim, C.W.; Kim, J.K.; Han, S.W. Subsets associated with developing acute pancreatitis in patients with severe hypertriglyceridemia and the severity of pancreatitis. Pancreatology 2019, 19, 795–800. [Google Scholar] [CrossRef]
- Tan, H.L.E.; McDonald, G.; Payne, A.; Yu, W.; Ismadi, Z.; Tran, H.; Gani, J.; Wynne, K. Incidence and Management of Hypertriglyceridemia-Associated Acute Pancreatitis: A Prospective Case Series in a Single Australian Tertiary Centre. J. Clin. Med. 2020, 9, 3954. [Google Scholar] [CrossRef]
- Hassanloo, J.; Béland-Bonenfant, S.; Paquette, M.; Baass, A.; Bernard, S. Prevalence, severity and management of hypertriglyceridemia-associated pancreatitis; A 7-year retrospective cohort study at Canadian quaternary care hospitals. J. Clin. Lipidol. 2022, 16, 455–462. [Google Scholar] [CrossRef]
- Zhu, Y.; Pan, X.; Zeng, H.; He, W.; Xia, L.; Liu, P.; Zhu, Y.; Chen, Y.; Lv, N. A Study on the Etiology, Severity, and Mortality of 3260 Patients With Acute Pancreatitis According to the Revised Atlanta Classification in Jiangxi, China Over an 8-Year Period. Pancreas 2017, 46, 504–509. [Google Scholar] [CrossRef]
- Dancu, G.; Bende, F.; Danila, M.; Sirli, R.; Popescu, A.; Tarta, C. Hypertriglyceridaemia-Induced Acute Pancreatitis: A Different Disease Phenotype. Diagnostics 2022, 12, 868. [Google Scholar] [CrossRef] [PubMed]
- Baranyai, T.; Terzin, V.; Vajda, Á.; Wittmann, T.; Czakó, L. Hypertriglyceridemia causes more severe course of acute pancreatitis. Clin. Lipidol. 2012, 7, 731–736. [Google Scholar] [CrossRef]
- Sezgin, O.; Ozdogan, O.; Yaras, S.; Ucbilek, E.; Altintas, E. Evaluation of hypertriglyceridemia-induced acute pancreatitis: A single tertiary care unit experience from Turkey. Turk. J. Gastroenterol. 2019, 30, 271–277. [Google Scholar] [CrossRef] [PubMed]
- Vipperla, K.; Somerville, C.; Furlan, A.; Koutroumpakis, E.; Saul, M.; Chennat, J.; Rabinovitz, M.; Whitcomb, D.C.; Slivka, A.; Papachristou, G.I.; et al. Clinical Profile and Natural Course in a Large Cohort of Patients With Hypertriglyceridemia and Pancreatitis. J. Clin. Gastroenterol. 2017, 51, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Pahomeanu, M.-R.; Mateescu, R.B.; Dorobat, B.; Negreanu, L. An Angiographic Treatment for a Pancreatic Pseudoaneurysm. Med. Mod. Mod. Med. 2020, 27, 69–72. [Google Scholar] [CrossRef]
- Wang, Q.; Wang, G.; Qiu, Z.; He, X.; Liu, C. Elevated Serum Triglycerides in the Prognostic Assessment of Acute Pancreatitis: A Systematic Review and Meta-Analysis of Observational Studies. J. Clin. Gastroenterol. 2017, 51, 586–593. [Google Scholar] [CrossRef] [PubMed]
- Birrell, L.; McGuinness, M.; Elliott, B.; Harmston, C. Effect of rurality and ethnicity in severity and outcomes in patients with acute pancreatitis. ANZ J. Surg. 2021, 91, 1558–1562. [Google Scholar] [CrossRef] [PubMed]
- Kurti, F.; Shpata, V.; Kuqo, A.; Duni, A.; Roshi, E.; Basho, J. Incidence of Acute Pancreatitis in Albanian Population. Mater. Socio Medica 2015, 27, 376–379. [Google Scholar] [CrossRef] [PubMed]
- Rashid, N.; Sharma, P.P.; Scott, R.D.; Lin, K.J.; Toth, P.P. All-Cause and Acute Pancreatitis Health Care Costs in Patients with Severe Hypertriglyceridemia. Pancreas 2017, 46, 57–63. [Google Scholar] [CrossRef]
- Jin, M.; Bai, X.; Chen, X.; Zhang, H.; Lu, B.; Li, Y.; Lai, Y.; Qian, J.; Yang, H. A 16-year trend of etiology in acute pancreatitis: The increasing proportion of hypertriglyceridemia-associated acute pancreatitis and its adverse effect on prognosis. J. Clin. Lipidol. 2019, 13, 947–953.e1. [Google Scholar] [CrossRef]
- Talamini, G.; Bassi, C.; Falconi, M.; Frulloni, L.; Di Francesco, V.; Vaona, B.; Bovo, P.; Rigo, L.; Castagnini, A.; Angelini, G.; et al. Cigarette smoking: An independent risk factor in alcoholic pancreatitis. Pancreas 1996, 12, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Amblee, A.; Mohananey, D.; Morkos, M.; Basu, S.; Abegunde, A.T.; Ganesh, M.; Bhalerao, N.; George, A.M.; Jain, M.; Fogelfeld, L. Acute Pancreatitis in Patients with Severe Hypertriglyceridemia in a Multi-Ethnic Minority Population. Endocr. Pract. 2018, 24, 429–436. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Hou, C.; Peng, Y.; Zhu, X.; Shi, C.; Zhang, K.; Tu, M.; Guo, F.; Huang, D.; Miao, Y. Diabetes and Younger Age Are Vital and Independent Risk Factors for Acute Pancreatitis in Patients with Severe Hypertriglyceridemia. BioMed Res. Int. 2019, 2019, 2620750. [Google Scholar] [CrossRef] [PubMed]
| AP cases | 1855 |
| Recurrence | |
| Acute pancreatitis (first known attack) | 1536 (82.8%) |
| Recurrent AP | 319 (17.2%) |
| Age (years) | |
| Median | 57 (IQR = 26.0) |
| Mean | 56.9 (SD = 17.1) |
| Days of hospitalization | |
| Median | 7.0 (IQR = 6.0) |
| Mean | 8.8 (SD = 7.8) |
| Length of stay ICU (days) | |
| Median | 3.0 (SD = 5.4) |
| Mean | 5.2 (IQR = 5.0) |
| Daily cost of hospitalization (EUR) | |
| Median | 184.9 (IQR = 86.8) |
| Mean | 432.3 (SD = 3439.7) |
| Aetiology | |
| Hypertriglyceridemia | 58 (3.1%) |
| Idiopathic | 283 (15.2%) |
| All other known causes, out of which: | 1514 (81.7%) |
| Biliary | 732 (39.5%) |
| Alcoholic | 628 (33.9%) |
| Diabetes mellitus | 55(3.0%) |
| Pharmacological | 30 (1.6%) |
| Trauma | 19 (1.0%) |
| Other known causes | 50 (2.7%) |
| Sex | |
| Male | 1098 (59.2%) |
| Female | 757 (40.8%) |
| Severity | |
| Mild | 954 (51.4%) |
| Moderately severe | 677 (36.5%) |
| Severe | 224 (12.1%) |
| Morphology | |
| Interstitial | 715 (38.5%) |
| Normal pancreas | 274 (14.8%) |
| APFC | 136 (7.3%) |
| ANC | 87 (4.7%) |
| Pseudocyst | 76 (4.1%) |
| WON | 5 (0.3%) |
| No data | 562 (30.3%) |
| Outcome | |
| Healed/ameliorated | 1540 (83.0%) |
| Discharge-at-will | 116 (6.3%) |
| Deceased | 108 (5.8%) |
| Transferred | 79 (4.3%) |
| Stationary | 12 (0.6%) |
| ICU | |
| No | 1676 (90.4%) |
| Yes | 179 (9.6%) |
| Tobacco smoking | |
| Active | 324 (17.5%) |
| Former (>4 weeks) | 90 (4.9%) |
| Never | 35 (1.9%) |
| No data | 1406 (75.8%) |
| Ward of origin | |
| Gastroenterology | 941 (50.7%) |
| Surgery | 914 (49.3%) |
| Place of origin | |
| Urban | 1332 (71.8%) |
| Rural | 507 (27.3%) |
| No data | 16 (0.9%) |
| HTG-AP (n = 58) | OAP (n = 1514) | p-Value | |
|---|---|---|---|
| Severity | |||
| Mild | 19 (32.8%) | 796 (52.6%) | p < 0.01 |
| Moderately severe | 28 (48.3%) | 551 (36.4%) | |
| Severe | 11 (19.0%) | 167 (11.0%) | |
| ICU | |||
| No | 48 (82.8%) | 1389 (91.7%) | p = 0.02 |
| Yes | 10 (17.2%) | 125 (8.3%) | |
| Ward of care | |||
| Gastroenterology | 42 (72.4%) | 744 (49.1%) | p < 0.01 |
| Surgery | 16 (27.6%) | 770 (50.9%) | |
| Gender | |||
| Male | 37 (63.8%) | 917 (60.6%) | p = 0.62 |
| Female | 21 (36.2%) | 597 (39.4%) | |
| Outcome | |||
| Healed/ameliorated | 48 (82.8%) | 1270 (83.9%) | p = 0.63 |
| Stationary | 1 (1.7%) | 10 (0.7%) | |
| Transfer | 1 (1.7%) | 72 (4.8%) | |
| Discharge at will | 5 (8.6%) | 95 (6.3%) | |
| Deceased | 3 (5.2%) | 67 (4.4%) | |
| Recurrence | |||
| First attack | 40 (69.0%) | 1249 (82.5%) | p < 0.01 |
| Recurrence | 18 (31.0%) | 265 (17.5%) | |
| Morphology/local complications | |||
| Interstitial | 26 (44.8%) | 597 (39.4%) | p = 0.02 |
| APFC | 9 (15.5%) | 110 (7.3%) | |
| Pseudocyst | 4 (6.9%) | 56 (3.7%) | |
| ANC | 3 (5.2%) | 58 (3.8%) | |
| WON | 0 (0.0%) | 4 (0.3%) | |
| Normal pancreas | 1 (1.7%) | 241 (15.9%) | |
| No data | 15 (25.9%) | 448 (29.6%) | |
| Smoking tobacco | |||
| Active | 9 (15.5%) | 283 (18.7%) | p = 0.09 |
| Former | 7 (12.1%) | 74 (4.9%) | |
| Never | 1 (1.7%) | 25 (1.7%) | |
| No data | 41 (70.7%) | 1132 (74.7%) | |
| Rurality | |||
| Urban | 41 (70.7%) | 1073 (70.9%) | p = 0.74 |
| Rural | 17 (29.3%) | 426 (28.1%) | |
| No data | 0 (0.0%) | 15 (1.0%) | |
| Age (years) | |||
| Mean | 44.3 (SD = 7.8) | 57.2 (SD = 17.0) | p < 0.01 |
| Median | 44.5 (IQR = 9) | 57.0 (IQR = 25) | |
| Length of stay (days) | |||
| Mean | 11.2 (SD = 8.3) | 8.7 (SD = 7.2) | p = 0.01 |
| Median | 8.3 (IQR = 9.3) | 7.0 (IQR = 5.0) | |
| Length of stay ICU (days) | |||
| Mean | 12.5 (SD = 11.4) | 4.6 (SD = 4.1) | p < 0.01 |
| Median | 7.0 (IQR = 22.5) | 3.0 (IQR = 4.0) | |
| Daily Cost of Hospitalization (RON) | |||
| Mean | 210.7 (SD = 121.76) | 439.1 (SD = 3556.7) | p = 0.59 |
| Median | 167.6 (IQR = 101.4) | 186.9 (IQR = 84.1) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Edu, A.V.; Pahomeanu, M.R.; Ghiță, A.I.; Constantinescu, D.I.; Grigore, D.G.; Bota, A.D.; Luta-Dumitrașcu, D.M.; Țieranu, C.G.; Negreanu, L. Hypertriglyceridemia-Induced Acute Pancreatitis—The Milky Way Constellation—The Seven-Year Experience of a Large Tertiary Centre. Diagnostics 2024, 14, 1105. https://doi.org/10.3390/diagnostics14111105
Edu AV, Pahomeanu MR, Ghiță AI, Constantinescu DI, Grigore DG, Bota AD, Luta-Dumitrașcu DM, Țieranu CG, Negreanu L. Hypertriglyceridemia-Induced Acute Pancreatitis—The Milky Way Constellation—The Seven-Year Experience of a Large Tertiary Centre. Diagnostics. 2024; 14(11):1105. https://doi.org/10.3390/diagnostics14111105
Chicago/Turabian StyleEdu, Andrei Vicențiu, Mihai Radu Pahomeanu, Andreea Irina Ghiță, Dalia Ioana Constantinescu, Daniela Gabriela Grigore, Andreea Daniela Bota, Daniela Maria Luta-Dumitrașcu, Cristian George Țieranu, and Lucian Negreanu. 2024. "Hypertriglyceridemia-Induced Acute Pancreatitis—The Milky Way Constellation—The Seven-Year Experience of a Large Tertiary Centre" Diagnostics 14, no. 11: 1105. https://doi.org/10.3390/diagnostics14111105
APA StyleEdu, A. V., Pahomeanu, M. R., Ghiță, A. I., Constantinescu, D. I., Grigore, D. G., Bota, A. D., Luta-Dumitrașcu, D. M., Țieranu, C. G., & Negreanu, L. (2024). Hypertriglyceridemia-Induced Acute Pancreatitis—The Milky Way Constellation—The Seven-Year Experience of a Large Tertiary Centre. Diagnostics, 14(11), 1105. https://doi.org/10.3390/diagnostics14111105






