Ultrasound Carotid Plaque Score and Severity of Coronary Artery Disease Assessed by Computed Tomography Angiography in Patients with Arterial Hypertension
Abstract
1. Introduction
2. Objectives
3. Materials and Methods
3.1. General Characteristics of the Performed Study
3.2. Computed Tomography
3.3. Carotid Duplex Ultrasound
3.4. Statistical Analysis
4. Results
4.1. Clinical Characteristics in the Study Group
4.2. Coronary Computed Tomography Angiography Parameters in the Study Group
4.3. Coronary Computed Tomography Angiography Parameters in the Study Subgroups Differing in a Carotid Plaque Score: A—Subgroup with the Carotid Plaque Score Equal to or Less Than One, B—Subgroup with Carotid Plaque Score Equal to or Greater Than Two
4.4. Results of Correlation Analysis
4.5. Results of Regression Analysis
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update From the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef] [PubMed]
- SCORE2 working group and ESC Cardiovascular risk collaboration. SCORE2 risk prediction algorithms: New models to estimate 10-year risk of cardiovascular disease in Europe. Eur. Heart J. 2021, 42, 2439–2454. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, R.; Carver, C.; Foley, J.R.; Fent, G.J.; Garg, P.; Ripley, D.P. Cardiovascular imaging techniques for the assessment of coronary artery disease. Br. J. Hosp. Med. 2022, 83, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Kılıçkap, G.; Tekdemir, H.; Bahadır, K.; Çevik, N.İ.; Akdal Dölek, B.; Vural, M. Coronary artery calcium score percentiles: Data from a single center in Turkey. Diagn. Interv. Radiol. 2024, 30, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Safian, R.D. Computed Tomography-Derived Physiology Assessment: State-of-the-Art Review. Cardiol. Clin. 2024, 42, 101–123. [Google Scholar] [CrossRef] [PubMed]
- Ihle-Hansen, H.; Vigen, T.; Berge, T.; Walle-Hansen, M.M.; Hagberg, G.; Ihle-Hansen, H.; Thommessen, B.; Ariansen, I.; Røsjø, H.; Rønning, O.M.; et al. Carotid Plaque Score for Stroke and Cardiovascular Risk Prediction in a Middle-Aged Cohort From the General Population. J. Am. Heart Assoc. 2023, 12, e030739. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Kesavabhotla, K.; Baradaran, H.; Kamel, H.; Pandya, A.; Giambrone, A.E.; Wright, D.; Pain, K.J.; Mtui, E.E.; Suri, J.S.; et al. Plaque echolucency and stroke risk in asymptomatic carotid stenosis: A systematic review and meta-analysis. Stroke 2015, 46, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Brinjikji, W.; Rabinstein, A.A.; Lanzino, G.; Murad, M.H.; Williamson, E.E.; DeMarco, J.K.; Huston, J., 3rd. Ultrasound Characteristics of Symptomatic Carotid Plaques: A Systematic Review and Meta-Analysis. Cerebrovasc. Dis. 2015, 40, 165–174. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Jamal, A.; Chao, S.; Cammarata, T.M.; Beeman, B.R. Society for Vascular Surgery duplex ultrasound surveillance guidelines are safe and cost effective for transcarotid artery revascularization. J. Vasc. Surg. 2023, 78, 988–994.e1. [Google Scholar] [CrossRef] [PubMed]
- Johri, A.M.; Nambi, V.; Naqvi, T.Z.; Feinstein, S.B.; Kim, E.S.H.; Park, M.M.; Becher, H.; Sillesen, H. Recommendations for the Assessment of Carotid Arterial Plaque by Ultrasound for the Characterization of Atherosclerosis and Evaluation of Cardiovascular Risk: From the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 2020, 33, 917–933. [Google Scholar] [CrossRef] [PubMed]
- Maroules, C.D.; Rajiah, P.; Bhasin, M.; Abbara, S. Current Evidence in Cardiothoracic Imaging: Growing Evidence for Coronary Computed Tomography Angiography as a First-line Test in Stable Chest Pain. J. Thorac. Imaging 2019, 34, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.C.; Hunter, A.; Shah, A.S.V.; Assi, V.; Lewis, S.; Smith, J.; Berry, C.; Boon, N.A.; Clark, E.; Flather, M.; et al. Use of Coronary Computed Tomographic Angiography to Guide Management of Patients With Coronary Disease. J. Am. Coll. Cardiol. 2016, 67, 1759–1768. [Google Scholar] [CrossRef]
- Fernández-Alvarez, V.; Linares-Sánchez, M.; Suárez, C.; López, F.; Guntinas-Lichius, O.; Mäkitie, A.A.; Bradley, P.J.; Ferlito, A. Novel Imaging-Based Biomarkers for Identifying Carotid Plaque Vulnerability. Biomolecules 2023, 13, 1236. [Google Scholar] [CrossRef] [PubMed]
- Knuuti, J.; Wijns, W.; Saraste, A.; Capodanno, D.; Barbato, E.; Funck-Brentano, C.; Prescott, E.; Storey, R.F.; Deaton, C.; Cuisset, T.; et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur. Heart J. 2020, 41, 407–477. [Google Scholar] [CrossRef]
- Den Ruijter, H.M.; Peters, S.A.E.; Anderson, T.J.; Britton, A.R.; Dekker, J.M.; Eijkemans, M.J.; Engström, G.; Evans, G.W.; de Graaf, J.; Grobbee, D.E.; et al. Common carotid intima-media thickness measurements in cardiovascular risk prediction: A meta-analysis. JAMA 2012, 308, 796–803. [Google Scholar] [CrossRef] [PubMed]
- Sebastian, S.A.; Co, E.L.; Tidd-Johnson, A.; Chowdhury, S.; Jain, E.; Davidson, M.; Johal, G. Usefulness of Carotid Ultrasound Screening in Primary Cardiovascular Prevention: A Systematic Review. Curr. Probl. Cardiol. 2024, 49, 102147. [Google Scholar] [CrossRef] [PubMed]
- Garg, P.K.; Bhatia, H.S.; Allen, T.S.; Grainger, T.; Pouncey, A.L.; Dichek, D.; Virmani, R.; Golledge, J.; Allison, M.A.; Powell, J.T. Assessment of Subclinical Atherosclerosis in Asymptomatic People In Vivo: Measurements Suitable for Biomarker and Mendelian Randomization Studies. Arterioscler. Thromb. Vasc. Biol. 2024, 44, 24–47. [Google Scholar] [CrossRef] [PubMed]
- Pini, R.; Faggioli, G.; Rocchi, C.; Fronterrè, S.; Lodato, M.; Vacirca, A.; Gallitto, E.; Gargiulo, M. The mid-term results of the Carotid Asymptomatic Stenosis (CARAS) observational study. J. Stroke Cerebrovasc. Dis. Off. J. Natl. Stroke Assoc. 2024, 33, 107508. [Google Scholar] [CrossRef] [PubMed]
- Saba, L.; Cau, R.; Murgia, A.; Nicolaides, A.N.; Wintermark, M.; Castillo, M.; Staub, D.; Kakkos, S.K.; Yang, Q.; Paraskevas, K.I.; et al. Carotid Plaque-RADS: A Novel Stroke Risk Classification System. JACC. Cardiovasc. Imaging 2024, 17, 62–75. [Google Scholar] [CrossRef] [PubMed]
| Number | 83 |
|---|---|
| Age (years) | 71.3 ± 8.5 |
| BMI (kg/m2) | 27.2 ± 2.9 |
| Gender (%) | |
| Men | 44.6 |
| Women | 55.4 |
| Grades of arterial hypertension according to ESH/ECS (%) | |
| Mild | 37.3 |
| Moderate | 51.9 |
| Severe | 10.8 |
| Hypotensive treatment (%) | 100.00 |
| Monotherapy | 28.9 |
| Combination therapy | 71.1 |
| Hypotensive drugs (%) | 100.00 |
| ACE inhibitors | 56.6 |
| β-blockers | 53.0 |
| Diuretics | 30.1 |
| Calcium channel blockers | 26.5 |
| Angiotensin receptor blockers | 7.2 |
| Systolic blood pressure (mmHg) | 137.4 ± 16.2 |
| Diastolic blood pressure (mmHg) | 85.0 ± 7.9 |
| Type 2 of diabetes (%) | 9.6 |
| Fasting glucose (mg/dL) | 117.4 ± 53.6 |
| Hypercholesterolemia (%) | 54.2 |
| Total cholesterol (mg/dL) | 219.3 ± 45.4 |
| Smoking (%) | 34.9 |
| Cigarette years | 267.6 ± 161.7 |
| Indication to Coronary Computed Tomography Angiography (%) | |
|---|---|
| Chronic CAD suspicion | 75.9 |
| Chest pain | 48.2 |
| Numerous CAD risk factors | 43.4 |
| Low intermediate CAD risk | 30.1 |
| Inconclusive exercise test | 16.9 |
| Nondiagnostic exercise test | 12.0 |
| Regional wall motion abnormalities of left ventricular | 4.8 |
| Sudden cardiac death in the family history | 1.2 |
| CACS | 249.3 ± 67.3 |
| CAD-RADS (%) | |
| 0 | 6.0 |
| 1 | 34.9 |
| 2 | 47.0 |
| 3 | 7.2 |
| 4 | 3.6 |
| 5 | 1.2 |
| Subgroup A (n = 51) | Subgroup B ( n= 32) | p | |
|---|---|---|---|
| Carotid plaque score | 0.3 ± 0.2 | 4.4 ± 1.2 | <0.05 |
| CACS | 93.5 ± 31.8 | 411.3 ± 70.1 | <0.05 |
| CAD-RADS (%) | |||
| 0 | 7.8 | 3.1 | ns |
| 1 | 43.1 | 21.9 | <0.05 |
| 2 | 43.1 | 53.1 | <0.05 |
| 3 | 2.0 | 15.6 | <0.05 |
| 4 | 2.0 | 6.2 | ns |
| 5 | 2.0 | 0.0 | ns |
| CAD-RADS ≥ 3 (%) | 6.0 | 21.8 | <0.05 |
| Carotid Plaque Score | CACS | CAD-RADS | |
|---|---|---|---|
| Age (years) | 0.29 | 0.42 | 0.34 |
| BMI (kg/m2) | 0.32 | 0.44 | ns |
| Systolic blood pressure (mmHg) | ns | 0.31 | ns |
| Diastolic blood pressure (mmHg) | ns | ns | ns |
| Fasting glucose (mg/dL) | ns | ns | ns |
| Total cholesterol (mg/dL) | 0.49 | 0.47 | 0.30 |
| Cigarette years | ns | 0.46 | ns |
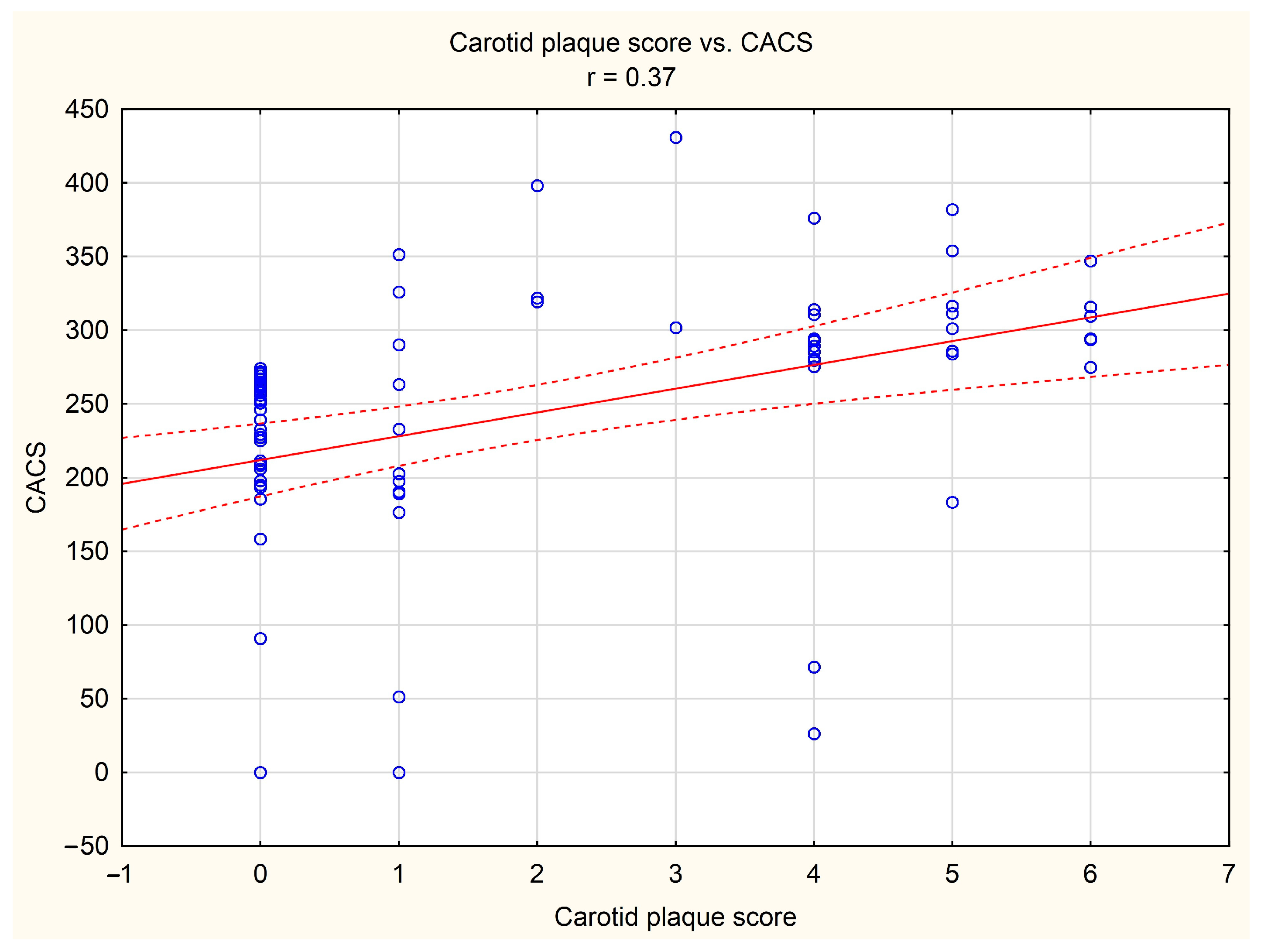
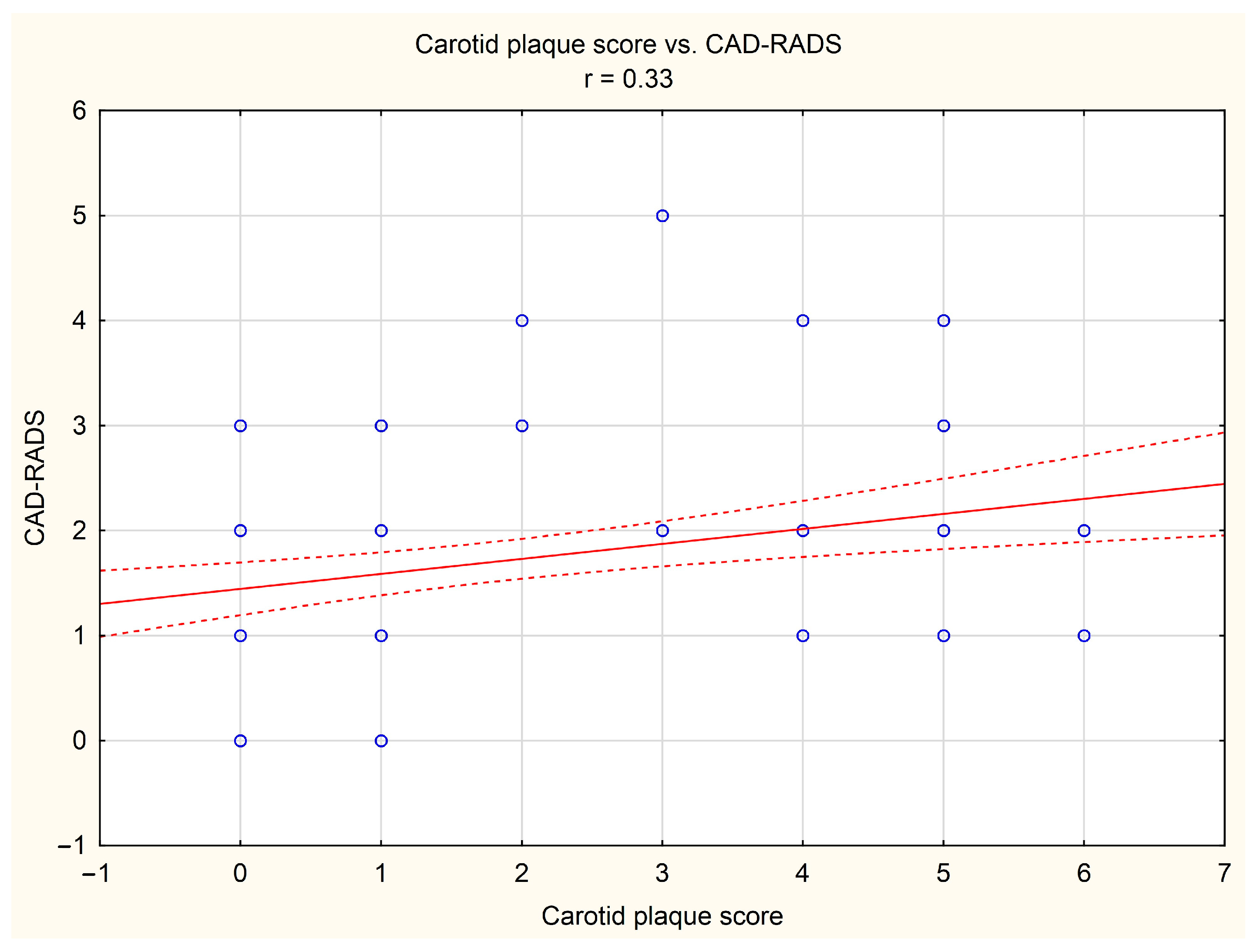
| Carotid plaque score | 1.00 | 0.37 | 0.33 |
| CACS | 0.37 | 1.00 | 0.41 |
| CAD-RADS | 0.33 | 0.41 | 1.00 |
| (A) Risk factors for higher coronary artery calcium score (CACS) | ||||
| Model for: CACS | ||||
| Intercept | Age (years) | Smoking # | Carotid plaque score | |
| Regression coefficient | 50.496 | 4.962 | 181.634 | 112.055 |
| SEM of Rc | 13.485 | 1.742 | 71.348 | 36.177 |
| p | <0.05 | <0.05 | <0.05 | <0.05 |
| (B) Risk factors for higher disease severity in the CAD-RADS classification | ||||
| Model for: CAD-RADS | ||||
| Intercept | Age (years) | Carotid plaque score | ||
| Regression coefficient | 1.311 | 0.051 | 1.317 | |
| SEM of Rc | 0.378 | 0.015 | 0.549 | |
| p | <0.05 | <0.05 | <0.05 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wysocki, A.; Fułek, M.; Macek, P.; Michałek-Zrąbkowska, M.; Kraik, K.; Poręba, M.; Fułek, K.; Martynowicz, H.; Mazur, G.; Gać, P.; et al. Ultrasound Carotid Plaque Score and Severity of Coronary Artery Disease Assessed by Computed Tomography Angiography in Patients with Arterial Hypertension. Diagnostics 2024, 14, 1101. https://doi.org/10.3390/diagnostics14111101
Wysocki A, Fułek M, Macek P, Michałek-Zrąbkowska M, Kraik K, Poręba M, Fułek K, Martynowicz H, Mazur G, Gać P, et al. Ultrasound Carotid Plaque Score and Severity of Coronary Artery Disease Assessed by Computed Tomography Angiography in Patients with Arterial Hypertension. Diagnostics. 2024; 14(11):1101. https://doi.org/10.3390/diagnostics14111101
Chicago/Turabian StyleWysocki, Andrzej, Michał Fułek, Piotr Macek, Monika Michałek-Zrąbkowska, Krzysztof Kraik, Małgorzata Poręba, Katarzyna Fułek, Helena Martynowicz, Grzegorz Mazur, Paweł Gać, and et al. 2024. "Ultrasound Carotid Plaque Score and Severity of Coronary Artery Disease Assessed by Computed Tomography Angiography in Patients with Arterial Hypertension" Diagnostics 14, no. 11: 1101. https://doi.org/10.3390/diagnostics14111101
APA StyleWysocki, A., Fułek, M., Macek, P., Michałek-Zrąbkowska, M., Kraik, K., Poręba, M., Fułek, K., Martynowicz, H., Mazur, G., Gać, P., & Poręba, R. (2024). Ultrasound Carotid Plaque Score and Severity of Coronary Artery Disease Assessed by Computed Tomography Angiography in Patients with Arterial Hypertension. Diagnostics, 14(11), 1101. https://doi.org/10.3390/diagnostics14111101











