Navigation and Robotics in Interventional Oncology: Current Status and Future Roadmap
Abstract
1. Introduction
2. Basics of Navigation and Robotic Systems
3. Clinical Applications and the Literature Evidence
4. Where Are We Heading?
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bale, R.J.; Hoser, C.; Rosenberger, R.; Rieger, M.; Benedetto, K.P.; Fink, C. Osteochondral lesions of the talus: Computer-assisted retrograde drilling—Feasibility and accuracy in initial experiences. Radiology 2001, 218, 278–282. [Google Scholar] [CrossRef] [PubMed]
- Bale, R.J.; Kovacs, P.; Dolati, B.; Hinterleithner, C.; Rosenberger, R.E. Stereotactic CT-guided percutaneous stabilization of posterior pelvic ring fractures: A preclinical cadaver study. J. Vasc. Interv. Radiol. 2008, 19, 1093–1098. [Google Scholar] [CrossRef] [PubMed]
- Lanza, C.; Carriero, S.; Buijs, E.F.M.; Mortellaro, S.; Pizzi, C.; Sciacqua, L.V.; Biondetti, P.; Angileri, S.A.; Ianniello, A.A.; Ierardi, A.M.; et al. Robotics in Interventional Radiology: Review of Current and Future Applications. Technol. Cancer Res. Treat. 2023, 22, 15330338231152084. [Google Scholar] [CrossRef] [PubMed]
- Najafi, G.; Kreiser, K.; Abdelaziz, M.E.M.K.; Hamady, M.S. Current State of Robotics in Interventional Radiology. Cardiovasc. Interv. Radiol. 2023, 46, 549–561. [Google Scholar] [CrossRef] [PubMed]
- Grigoriadis, S.; Filippiadis, D.; Stamatopoulou, V.; Alexopoulou, E.; Kelekis, N.; Kelekis, A. Navigation Guidance for Percutaneous Splanchnic Nerve Radiofrequency Neurolysis: Preliminary Results. Medicina 2022, 58, 1359. [Google Scholar] [CrossRef]
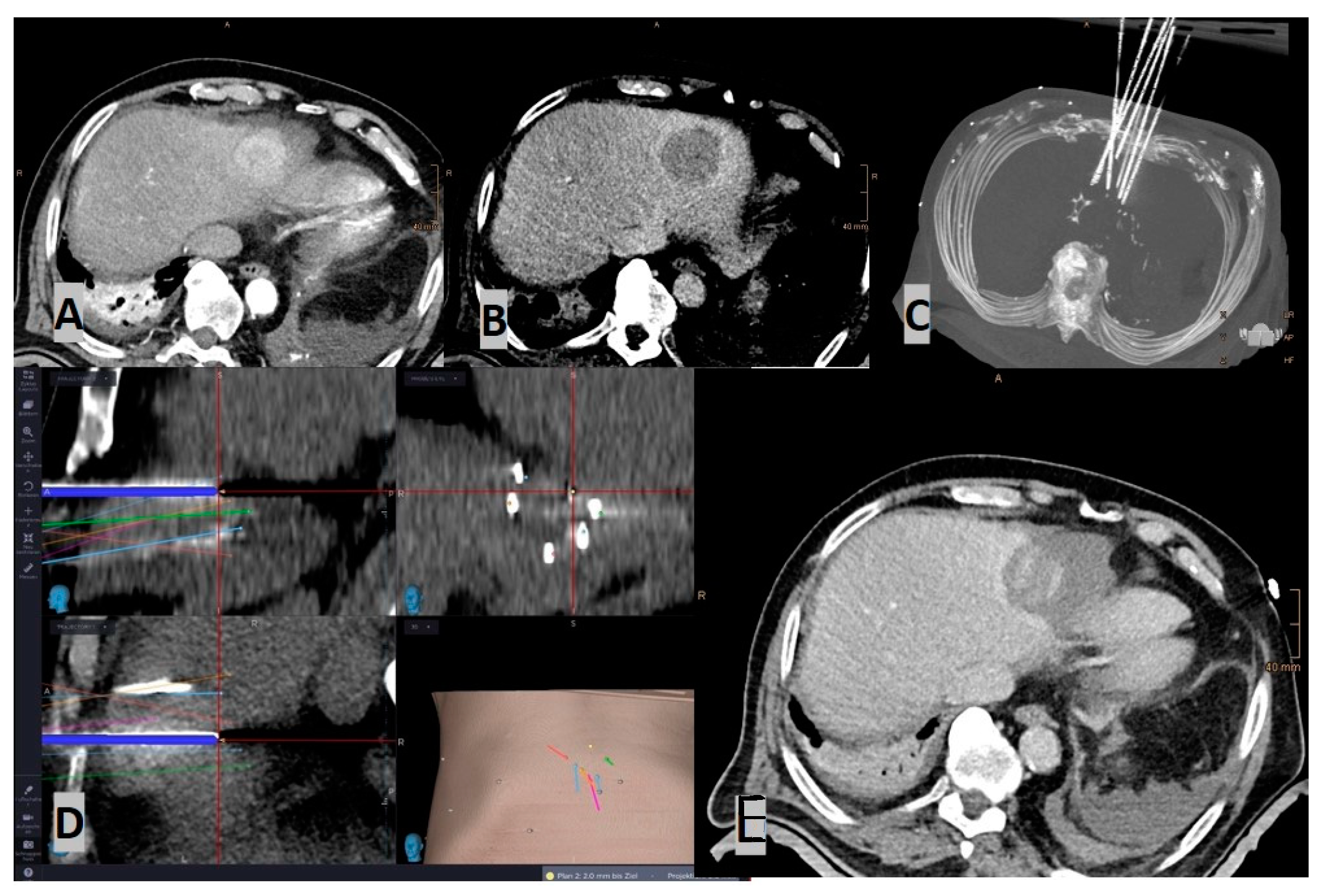
- Laimer, G.; Schullian, P.; Bale, R. Stereotactic Thermal Ablation of Liver Tumors: 3D Planning, Multiple Needle Approach, and Intraprocedural Image Fusion Are the Key to Success-A Narrative Review. Biology 2021, 10, 644. [Google Scholar] [CrossRef]
- Soulen, M.C.; Sofocleous, C.T. Achieving Curative Ablation Outcomes: It Is All about the Imaging. Radiology 2021, 298, 219–220. [Google Scholar] [CrossRef]
- Lin, Y.-M.; Paolucci, I.; O’connor, C.S.; Anderson, B.M.; Rigaud, B.; Fellman, B.M.; Jones, K.A.; Brock, K.K.; Odisio, B.C. Ablative Margins of Colorectal Liver Metastases Using Deformable CT Image Registration and Autosegmentation. Radiology 2023, 307, e221373. [Google Scholar] [CrossRef]
- Laimer, G.; Schullian, P.; Jaschke, N.; Putzer, D.; Eberle, G.; Alzaga, A.; Odisio, B.; Bale, R. Minimal ablative margin (MAM) assessment with image fusion: An independent predictor for local tumor progression in hepatocellular carcinoma after stereotactic radiofrequency ablation. Eur. Radiol. 2020, 30, 2463–2472. [Google Scholar] [CrossRef]
- Laimer, G.; Jaschke, N.; Schullian, P.; Putzer, D.; Eberle, G.; Solbiati, M.; Solbiati, L.; Goldberg, S.N.; Bale, R. Volumetric assessment of the periablational safety margin after thermal ablation of colorectal liver metastases. Eur. Radiol. 2021, 31, 6489–6499. [Google Scholar] [CrossRef]
- Chehab, M.A.; Brinjikji, W.; Copelan, A.; Venkatesan, A.M. Navigational Tools for Interventional Radiology and Interventional Oncology Applications. Semin. Interv. Radiol. 2015, 32, 416–427. [Google Scholar] [CrossRef] [PubMed]
- Wood, B.J.; Kruecker, J.; Abi-Jaoudeh, N.; Locklin, J.K.; Levy, E.; Xu, S.; Solbiati, L.; Kapoor, A.; Amalou, H.; Venkatesan, A.M. Navigation Systems for Ablation. J. Vasc. Interv. Radiol. 2010, 21 (Suppl. 8), S257–S263. [Google Scholar] [CrossRef] [PubMed]
- Faiella, E.; Castiello, G.; Bernetti, C.; Pacella, G.; Altomare, C.; Andresciani, F.; Zobel, B.B.; Grasso, R.F. Impact of an Augmented Reality Navigation System (SIRIO) on Bone Percutaneous Procedures: A Comparative Analysis with Standard CT-Guided Technique. Curr. Oncol. 2021, 28, 1751–1760. [Google Scholar] [CrossRef] [PubMed]
- Long, D.J.; Li, M.; De Ruiter, Q.M.B.; Hecht, R.; Li, X.; Varble, N.; Blain, M.; Kassin, M.T.; Sharma, K.V.; Sarin, S.; et al. Comparison of Smartphone Augmented Reality, Smartglasses Augmented Reality, and 3D CBCT-guided Fluoroscopy Navigation for Percutaneous Needle Insertion: A Phantom Study. Cardiovasc. Interv. Radiol. 2021, 44, 774–781. [Google Scholar] [CrossRef] [PubMed]
- Hong, C.W.; Xu, S.; Imbesi, K.L.; Wood, B.J. Integrated laser-guided CT biopsy. Clin. Imaging 2013, 37, 1135–1137. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Moser, C.; Becker, J.; Deli, M.; Busch, M.; Boehme, M.; Groenemeyer, D.H. A novel Laser Navigation System reduces radiation exposure and improves accuracy and workflow of CT-guided spinal interventions: A prospective, randomized, controlled, clinical trial in comparison to conventional freehand puncture. Eur. J. Radiol. 2013, 82, 627–632. [Google Scholar] [CrossRef]
- Gruber-Rouh, T.; Lee, C.; Bolck, J.; Naguib, N.N.; Schulz, B.; Eichler, K.; Aschenbach, R.; Wichmann, J.L.; Vogl, T.J.; Zangos, S. Intervention Planning Using a Laser Navigation System for CT-Guided Interventions: A Phantom and Patient Study. Korean J. Radiol. 2015, 16, 729–735. [Google Scholar] [CrossRef]
- Hecht, R.; Li, M.; de Ruiter, Q.M.B.; Pritchard, W.F.; Li, X.; Krishnasamy, V.; Saad, W.; Karanian, J.W.; Wood, B.J. Smartphone Augmented Reality CT-Based Platform for Needle Insertion Guidance: A Phantom Study. Cardiovasc. Interv. Radiol. 2020, 43, 756–764. [Google Scholar] [CrossRef]
- Solbiati, M.; Passera, K.M.; Rotilio, A.; Oliva, F.; Marre, I.; Goldberg, S.N.; Ierace, T.; Solbiati, L. Augmented reality for interventional oncology: Proof-of-concept study of a novel high-end guidance system platform. Eur. Radiol. Exp. 2018, 2, 18. [Google Scholar] [CrossRef]
- Solbiati, M.; Ierace, T.; Muglia, R.; Pedicini, V.; Iezzi, R.; Passera, K.M.; Rotilio, A.C.; Goldberg, S.N.; Solbiati, L.A. Thermal Ablation of Liver Tumors Guided by Augmented Reality: An Initial Clinical Experience. Cancers 2022, 14, 1312. [Google Scholar] [CrossRef]
- Albano, D.; Messina, C.; Gitto, S.; Chianca, V.; Sconfienza, L.M. Bone biopsies guided by augmented reality: A pilot study. Eur. Radiol. Exp. 2023, 7, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Gadodia, G.; Yanof, J.; Hanlon, A.; Bustos, S.; Weunski, C.; West, K.; Martin, C. Early Clinical Feasibility Evaluation of an Augmented Reality Platform for Guidance and Navigation during Percutaneous Tumor Ablation. J. Vasc. Interv. Radiol. 2022, 33, 333–338. [Google Scholar] [CrossRef] [PubMed]
- Racadio, J.M.; Nachabe, R.; Homan, R.; Schierling, R.; Racadio, J.M.; Babić, D. Augmented Reality on a C-Arm System: A Preclinical Assessment for Percutaneous Needle Localization. Radiology 2016, 281, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Bapst, B.; Lagadec, M.; Breguet, R.; Vilgrain, V.; Ronot, M. Cone Beam Computed Tomography (CBCT) in the Field of Interventional Oncology of the Liver. Cardiovasc. Interv. Radiol. 2016, 39, 8–20. [Google Scholar] [CrossRef] [PubMed]
- Key, B.M.; Tutton, S.M.; Scheidt, M.J. Cone-Beam CT With Enhanced Needle Guidance and Augmented Fluoroscopy Overlay: Applications in Interventional Radiology. Am. J. Roentgenol. 2023, 221, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Busser, W.M.H.; Braak, S.J.; Fütterer, J.J.; van Strijen, M.J.L.; Hoogeveen, Y.L.; de Lange, F.; Kool, L.J.S. Cone beam CT guidance provides superior accuracy for complex needle paths compared with CT guidance. Br. J. Radiol. 2013, 86, 20130310. [Google Scholar] [CrossRef] [PubMed]
- Cazzato, R.L.; Battistuzzi, J.B.; Catena, V.; Grasso, R.F.; Zobel, B.B.; Schena, E.; Buy, X.; Palussiere, J. Cone-Beam Computed Tomography (CBCT) Versus CT in Lung Ablation Procedure: Which is Faster? Cardiovasc. Intervent. Radiol. 2015, 38, 1231–1236. [Google Scholar] [CrossRef]
- Floridi, C.; Muollo, A.; Fontana, F.; Rotolo, N.; Ierardi, A.M.; Duka, E.; Pellegrino, C.; Carrafiello, G. C-arm cone-beam computed tomography needle path overlay for percutaneous biopsy of pulmonary nodules. La Radiol. Med. 2014, 119, 820–827. [Google Scholar] [CrossRef]
- Braak, S.J.; van Melick, H.H.; Onaca, M.G.; van Heesewijk, J.P.; van Strijen, M.J. 3D cone-beam CT guidance, a novel technique in renal biopsy--results in 41 patients with suspected renal masses. Eur. Radiol. 2012, 22, 2547–2552. [Google Scholar] [CrossRef]
- Tselikas, L.; Joskin, J.; Roquet, F.; Farouil, G.; Dreuil, S.; Hakimé, A.; Teriitehau, C.; Auperin, A.; de Baere, T.; Deschamps, F. Percutaneous bone biopsies: Comparison between flat-panel cone-beam CT and CT-scan guidance. Cardiovasc. Interv. Radiol. 2014, 38, 167–176. [Google Scholar] [CrossRef]
- Wallace, M.J.; Kuo, M.D.; Glaiberman, C.; Binkert, C.A.; Orth, R.C.; Soulez, G. Three-dimensional C-arm cone-beam CT: Applications in the interventional suite. J. Vasc. Interv. Radiol. 2008, 19, 799–813. [Google Scholar] [CrossRef] [PubMed]
- Iwazawa, J.; Ohue, S.; Hashimoto, N.; Muramoto, O.; Mitani, T. Survival after C-arm CT-assisted chemoembolization of unresectable hepatocellular carcinoma. Eur. J. Radiol. 2012, 81, 3985–3992. [Google Scholar] [CrossRef] [PubMed]
- Fuhrmann, I.; Probst, U.; Wiggermann, P.; Beyer, L. Navigation Systems for Treatment Planning and Execution of Percutaneous Irreversible Electroporation. Technol. Cancer Res. Treat. 2018, 17, 1533033818791792. [Google Scholar] [CrossRef] [PubMed]
- Ward, T.J.; Goldman, R.E.; Weintraub, J.L. Electromagnetic navigation with multimodality image fusion for image-guided percutaneous interventions. Tech. Vasc. Interv. Radiol. 2013, 16, 177–181. [Google Scholar] [CrossRef] [PubMed]
- Appelbaum, L.; Solbiati, L.; Sosna, J.; Nissenbaum, Y.; Greenbaum, N.; Goldberg, S.N. Evaluation of an electromagnetic image-fusion navigation system for biopsy of small lesions: Assessment of accuracy in an in vivo swine model. Acad. Radiol. 2013, 20, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Appelbaum, L.; Mahgerefteh, S.Y.; Sosna, J.; Goldberg, S.N. Image-guided fusion and navigation: Applications in tumor ablation. Tech. Vasc. Interv. Radiol. 2013, 16, 287–295. [Google Scholar] [CrossRef] [PubMed]
- Phee, S.J.; Yang, K. Interventional navigation systems for treatment of unresectable liver tumor. Med. Biol. Eng. Comput. 2010, 48, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Narsule, C.K.; Dos Santos, R.S.; Gupta, A.; Ebright, M.I.; Rivas, R.; Daly, B.D.; Fernando, H.C. The efficacy of electromagnetic navigation to assist with computed tomography-guided percutaneous thermal ablation of lung tumors. Innovations 2012, 7, 187–190. [Google Scholar]
- Penzkofer, T.; Bruners, P.; Isfort, P.; Schoth, F.; Günther, R.W.; Schmitz-Rode, T.; Mahnken, A.H. Free-hand CT-based electromagnetically guided interventions: Accuracy, efficiency and dose usage. Minim. Invasive Ther. Allied Technol. 2011, 20, 226–233. [Google Scholar] [CrossRef]
- Wu, B.; Xiao, Y.-Y.; Zhang, X.; Zhang, A.-L.; Li, H.-J.; Gao, D.-F. Magnetic resonance imaging-guided percutaneous cryoablation of hepatocellular carcinoma in special regions. Hepatobiliary Pancreat. Dis. Int. 2010, 9, 384–392. [Google Scholar]
- Maeda, T.; Hong, J.; Konishi, K.; Nakatsuji, T.; Yasunaga, T.; Yamashita, Y.-I.; Taketomi, A.; Kotoh, K.; Enjoji, M.; Nakashima, H.; et al. Tumor ablation therapy of liver cancers with an open magnetic resonance imaging-based navigation system. Surg. Endosc. 2009, 23, 1048–1053. [Google Scholar] [CrossRef] [PubMed]
- Faiella, E.; Frauenfelder, G.; Santucci, D.; Luppi, G.; Schena, E.; Zobel, B.B.; Grasso, R.F. Percutaneous low-dose CT-guided lung biopsy with an augmented reality navigation system: Validation of the technique on 496 suspected lesions. Clin. Imaging 2018, 49, 101–105. [Google Scholar] [CrossRef] [PubMed]
- Schullian, P.; Widmann, G.; Lang, T.B.; Knoflach, M.; Bale, R. Accuracy and diagnostic yield of CT-guided stereotactic liver biopsy of primary and secondary liver tumors. Comput. Aided Surg. 2011, 16, 181–187. [Google Scholar] [CrossRef] [PubMed]
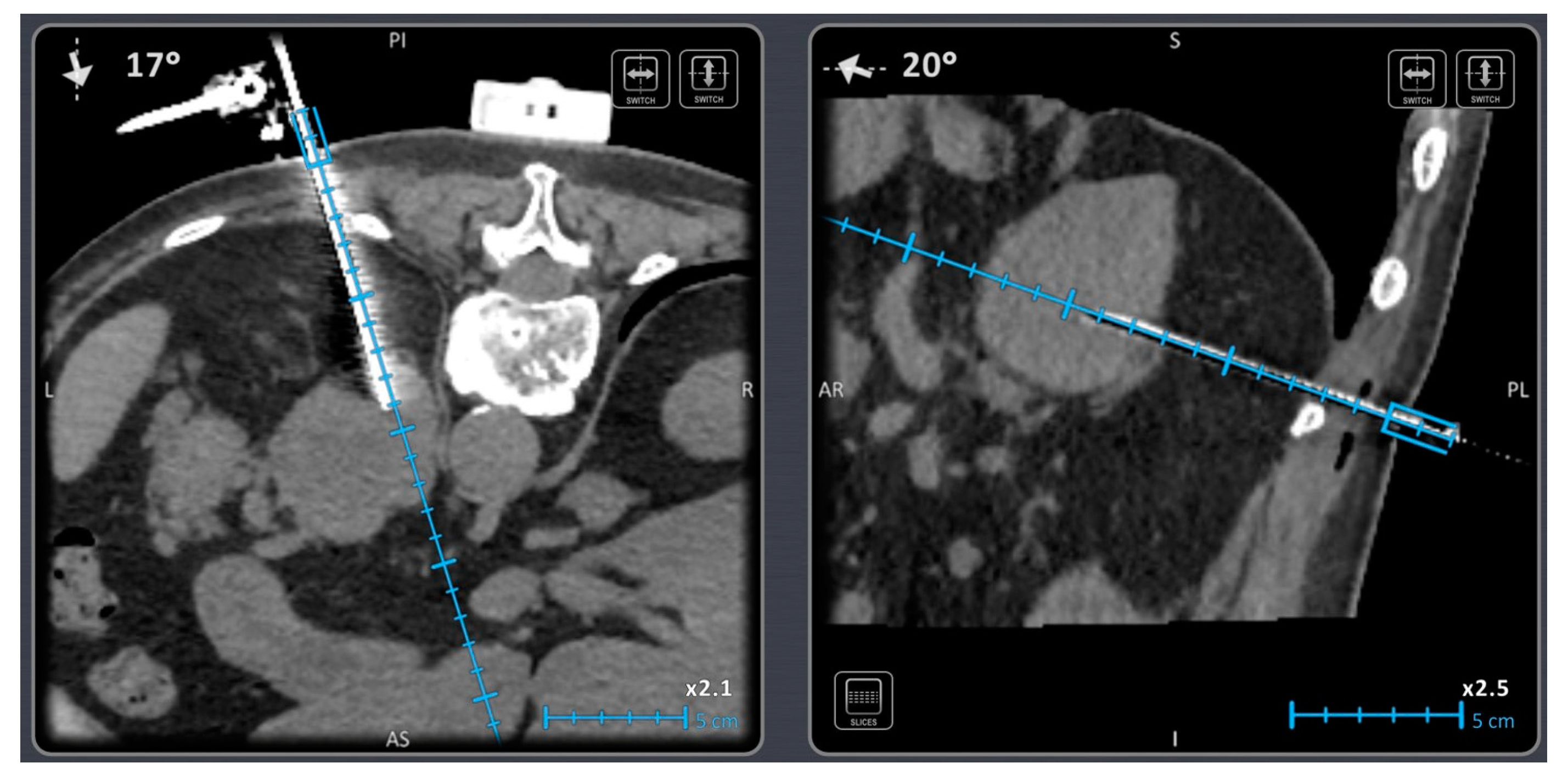
- Bale, R.; Widmann, G. Navigated CT-guided interventions. Minim. Invasive Ther. Allied Technol. 2007, 16, 196–204. [Google Scholar] [CrossRef] [PubMed]
- Bale, R.; Widmann, G.; Stoffner, D.R. Stereotaxy: Breaking the limits of current radiofrequency ablation techniques. Eur. J. Radiol. 2010, 75, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Bale, R.; Laimer, G.; Schullian, P.; Alzaga, A. Stereotactic ablation: A game changer? J. Med. Imaging. Radiat. Oncol. 2023. [Google Scholar] [CrossRef] [PubMed]
- Solomon, S.B.; Patriciu, A.; Bohlman, M.E.; Kavoussi, L.R.; Stoianovici, D.; Hiraki, T.; Kamegawa, T.; Matsuno, T.; Sakurai, J.; Kirita, Y.; et al. Robotically driven interventions: A method of using CT fluoroscopy without radiation exposure to the physician. Radiology 2002, 225, 277–282. [Google Scholar] [CrossRef]
- Stoffner, R.; Augschöll, C.; Widmann, G.; Böhler, D.; Bale, R. Accuracy and feasibility of frameless stereotactic and robot-assisted CT-based puncture in interventional radiology: A comparative phantom study. Rofo 2009, 181, 851–858. [Google Scholar] [CrossRef]
- Anzidei, M.; Argirò, R.; Porfiri, A.; Boni, F.; Anile, M.; Zaccagna, F.; Vitolo, D.; Saba, L.; Napoli, A.; Leonardi, A.; et al. Preliminary clinical experience with a dedicated interventional robotic system for CT-guided biopsies of lung lesions: A comparison with the conventional manual technique. Eur. Radiol. 2015, 25, 1310–1316. [Google Scholar] [CrossRef]
- Lim, S.; Jun, C.; Chang, D.; Petrisor, D.; Han, M.; Stoianovici, D. Robotic Transrectal Ultrasound Guided Prostate Biopsy. IEEE Trans. Biomed. Eng. 2019, 66, 2527–2537. [Google Scholar] [CrossRef]
- Schouten, M.G.; Bomers, J.G.R.; Yakar, D.; Huisman, H.; Rothgang, E.; Bosboom, D.; Scheenen, T.W.J.; Misra, S.; Fütterer, J.J. Evaluation of a robotic technique for transrectal MRI-guided prostate biopsies. Eur. Radiol. 2012, 22, 476–483. [Google Scholar] [CrossRef] [PubMed]
- Zangos, S.; Melzer, A.; Eichler, K.; Sadighi, C.; Thalhammer, A.; Bodelle, B.; Wolf, R.; Gruber-Rouh, T.; Proschek, D.; Hammerstingl, R.; et al. MR-compatible assistance system for biopsy in a high-field-strength system: Initial results in patients with suspicious prostate lesions. Radiology 2011, 259, 903–910. [Google Scholar] [CrossRef] [PubMed]
- Kumar, R.; Singh, S.K.; Mittal, B.R.; Vadi, S.K.; Kakkar, N.; Singh, H.; Krishnaraju, V.S.; Kumar, S.; Bhattacharya, A. Safety and Diagnostic Yield of 68Ga Prostate-specific Membrane Antigen PET/CT-guided Robotic-assisted Transgluteal Prostatic Biopsy. Radiology 2022, 303, 392–398. [Google Scholar] [CrossRef] [PubMed]
- Tilak, G.; Tuncali, K.; Song, S.-E.; Tokuda, J.; Olubiyi, O.; Fennessy, F.; Fedorov, A.; Penzkofer, T.; Tempany, C.; Hata, N. 3T MR-guided in-bore transperineal prostate biopsy: A comparison of robotic and manual needle-guidance templates. J. Magn. Reson. Imaging 2015, 42, 63–71. [Google Scholar] [CrossRef]
- Cleary, K.; Watson, V.; Lindisch, D.; Taylor, R.H.; Fichtinger, G.; Xu, S.; White, C.S.; Donlon, J.; Taylor, M.; Patriciu, A.; et al. Precision placement of instruments for minimally invasive procedures using a "needle driver" robot. Int. J. Med. Robot 2005, 1, 40–47. [Google Scholar] [CrossRef]
- Hiraki, T.; Kamegawa, T.; Matsuno, T.; Sakurai, J.; Komaki, T.; Yamaguchi, T.; Tomita, K.; Uka, M.; Matsui, Y.; Iguchi, T.; et al. Robotic needle insertion during computed tomography fluoroscopy–guided biopsy: Prospective first-in-human feasibility trial. Eur. Radiol. 2020, 30, 927–933. [Google Scholar] [CrossRef]
- Levy, S.; Goldberg, S.N.; Roth, I.; Shochat, M.; Sosna, J.; Leichter, I.; Flacke, S. Clinical evaluation of a robotic system for precise CT-guided percutaneous procedures. Abdom. Imaging 2021, 46, 5007–5016. [Google Scholar] [CrossRef]
- Christou, A.S.; Amalou, A.; Lee, H.; Rivera, J.; Li, R.; Kassin, M.T.; Varble, N.; Tse, Z.T.H.; Xu, S.; Wood, B.J. Image-Guided Robotics for Standardized and Automated Biopsy and Ablation. Semin. Interv. Radiol. 2021, 38, 565–575. [Google Scholar] [CrossRef]
- Witkowska, A.; Levy, S.; Roth, I.; Shochat, M.; Bradbury, D.; Sosna, J.; Leichter, I.; Goldberg, S.N.; Flacke, S. Feasibility and Accuracy of a Novel Hands-Free Robotic System for Percutaneous Needle Insertion and Steering. Surg. Technol. Int. 2022, 41, sti41-1624. [Google Scholar]
- Ben-David, E.; Shochat, M.; Roth, I.; Nissenbaum, I.; Sosna, J.; Goldberg, S.N. Evaluation of a CT-Guided Robotic System for Precise Percutaneous Needle Insertion. J. Vasc. Interv. Radiol. 2018, 29, 1440–1446. [Google Scholar] [CrossRef]
- Lanouzière, M.; Varbédian, O.; Chevallier, O.; Griviau, L.; Guillen, K.; Popoff, R.; Aho-Glélé, S.-L.; Loffroy, R. Computed Tomography-Navigation™ Electromagnetic System Compared to Conventional Computed Tomography Guidance for Percutaneous Lung Biopsy: A Single-Center Experience. Diagnostics 2021, 11, 1532. [Google Scholar] [CrossRef] [PubMed]
- Durand, P.; Moreau-Gaudry, A.; Silvent, A.-S.; Frandon, J.; Chipon, E.; Médici, M.; Bricault, I. Computer assisted electromagnetic navigation improves accuracy in computed tomography guided interventions: A prospective randomized clinical trial. PLoS ONE 2017, 12, e0173751. [Google Scholar] [CrossRef] [PubMed]
- Ahdoot, M.; Wilbur, A.R.; Reese, S.E.; Lebastchi, A.H.; Mehralivand, S.; Gomella, P.T.; Bloom, J.; Gurram, S.; Siddiqui, M.; Pinsky, P.; et al. MRI-Targeted, Systematic, and Combined Biopsy for Prostate Cancer Diagnosis. New Engl. J. Med. 2020, 382, 917–928. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, M.M.; Rais-Bahrami, S.; Turkbey, B.; George, A.K.; Rothwax, J.; Shakir, N.; Okoro, C.; Raskolnikov, D.; Parnes, H.L.; Linehan, W.M.; et al. Comparison of MR/ultrasound fusion-guided biopsy with ultrasound-guided biopsy for the diagnosis of prostate cancer. JAMA 2015, 313, 390–397. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, B.J.J.; Yeong, C.H.; Goh, K.L.; Yoong, B.K.; Ho, G.F.; Yim, C.C.W.; Kulkarni, A. Robot-assisted radiofrequency ablation of primary and secondary liver tumours: Early experience. Eur. Radiol. 2014, 24, 79–85. [Google Scholar] [CrossRef]
- Beyer, L.P.; Pregler, B.; Michalik, K.; Niessen, C.; Dollinger, M.; Müller, M.; Schlitt, H.J.; Stroszczynski, C.; Wiggermann, P. Evaluation of a robotic system for irreversible electroporation (IRE) of malignant liver tumors: Initial results. Int. J. Comput. Assist. Radiol. Surg. 2017, 12, 803–809. [Google Scholar] [CrossRef]
- Mbalisike, E.C.; Vogl, T.J.; Zangos, S.; Eichler, K.; Balakrishnan, P.; Paul, J. Image-guided microwave thermoablation of hepatic tumours using novel robotic guidance: An early experience. Eur. Radiol. 2015, 25, 454–462. [Google Scholar] [CrossRef]
- Braunwarth, E.; Schullian, P.; Kummann, M.; Reider, S.; Putzer, D.; Primavesi, F.; Stättner, S.; Öfner, D.; Bale, R. Aggressive local treatment for recurrent intrahepatic cholangiocarcinoma—Stereotactic radiofrequency ablation as a valuable addition to hepatic resection. PLoS ONE 2022, 17, e0261136. [Google Scholar] [CrossRef]
- Schullian, P.; Laimer, G.; Johnston, E.; Putzer, D.; Eberle, G.; Scharll, Y.; Widmann, G.; Kolbitsch, C.; Bale, R. Technical efficacy and local recurrence after stereotactic radiofrequency ablation of 2653 liver tumors: A 15-year single-center experience with evaluation of prognostic factors. Int. J. Hyperth. 2022, 39, 421–430. [Google Scholar] [CrossRef]
- de Baere, T.; Roux, C.; Deschamps, F.; Tselikas, L.; Guiu, B. Evaluation of a New CT-Guided Robotic System for Percutaneous Needle Insertion for Thermal Ablation of Liver Tumors: A Prospective Pilot Study. Cardiovasc. Intervent Radiol. 2022, 45, 1701–1709. [Google Scholar] [CrossRef]
- Schullian, P.; Johnston, E.; Laimer, G.; Scharll, Y.; Putzer, D.; Eberle, G.; Kolbitsch, C.; Amann, A.; Stättner, S.; Bale, R. Stereotactic radiofrequency ablation of tumors at the hepatic venous confluence. HPB 2022, 24, 1044–1054. [Google Scholar] [CrossRef] [PubMed]
- Schullian, P.; Laimer, G.; Putzer, D.; Levy, E.; Braunwarth, E.; Stättner, S.; Bale, R. Stereotactic radiofrequency ablation as first-line treatment of recurrent HCC following hepatic resection. Eur. J. Surg. Oncol. 2020, 46, 1503–1509. [Google Scholar] [CrossRef] [PubMed]
- Schullian, P.; Johnston, E.W.; Putzer, D.; Laimer, G.; Waroschitz, G.; Braunwarth, E.; Amann, A.; Maglione, M.; Bale, R. Stereotactic radiofrequency ablation (SRFA) for recurrent colorectal liver metastases after hepatic resection. Eur. J. Surg. Oncol. (EJSO) 2021, 47, 866–873. [Google Scholar] [CrossRef] [PubMed]
- Schullian, P.; Johnston, E.W.; Putzer, D.; Eberle, G.; Laimer, G.; Bale, R. Safety and efficacy of stereotactic radiofrequency ablation for very large (≥8 cm) primary and metastatic liver tumors. Sci. Rep. 2020, 10, 1618. [Google Scholar] [CrossRef] [PubMed]
- Filippiadis, D.K.; Velonakis, G.; Mazioti, A.; Tsochatzis, A.; Vrachliotis, T.; Kelekis, A.; Kelekis, N. Percutaneous Navigation under Local Anesthesia for Computed Tomography-Guided Microwave Ablation of Malignant Liver Lesions Located in the Hepatic Dome. Medicina 2021, 57, 1056. [Google Scholar] [CrossRef]
- Volpi, S.; Tsoumakidou, G.; Loriaud, A.; Hocquelet, A.; Duran, R.; Denys, A. Electromagnetic navigation system combined with High-Frequency-Jet-Ventilation for CT-guided hepatic ablation of small US-Undetectable and difficult to access lesions. Int. J. Hyperth. 2019, 36, 1051–1057. [Google Scholar] [CrossRef]
- Schullian, P.; Laimer, G.; Johnston, E.; Putzer, D.; Eberle, G.; Widmann, G.; Scharll, Y.; Bale, R. Reliability of Stereotactic Radiofrequency Ablation (SRFA) for Malignant Liver Tumors: Novice versus Experienced Operators. Biology 2023, 12, 175. [Google Scholar] [CrossRef]
- Moulin, B.; Tselikas, L.; De Baere, T.; Varin, F.; Abed, A.; Debays, L.; Bardoulat, C.; Hakime, A.; Teriitehau, C.; Deschamps, F.; et al. CT guidance assisted by electromagnetic navigation system for percutaneous fixation by internal cemented screws (FICS). Eur. Radiol. 2020, 30, 943–949. [Google Scholar] [CrossRef]
- Teriitehau, C.; Rabeh, H.; Pessis, E.; Sénéchal, Q.; Besse, F.; Bravetti, M. Reduction of patient radiation dose during percutaneous CT vertebroplasty: Impact of a new computer-assisted navigation (CAN) system. Radioprotection 2020, 55, 11–16. [Google Scholar] [CrossRef]
- Schubert, T.; Jacob, A.L.; Pansini, M.; Liu, D.; Gutzeit, A.; Kos, S. CT-guided interventions using a free-hand, optical tracking system: Initial clinical experience. Cardiovasc. Interv. Radiol. 2013, 36, 1055–1062. [Google Scholar] [CrossRef]
- Boeken, T.; Pouliquen, G.; Premat, K.; Benac, B.; Shotar, E.; Cormier; Talbi, A.; Bonaccorsi, R.; Morardet, L.; Morel, V.; et al. Initial experience, feasibility, and technical development with an electromagnetic navigation assistance in percutaneous pelvic bone cementoplasty: Retrospective analysis. Eur. Radiol. 2023, 33, 2605–2611. [Google Scholar] [CrossRef] [PubMed]
- Boeken, T.; Shotar, E.; Cormier; Puyraimond-Zemmour, D.; Talbi, A.; Bonaccorsi, R.; Mahtout, J.; Drir, M.; Clarençon, F.; Premat, K. The “Eiffel Tower” technique: Novel long-axis sacroplasty under electromagnetic navigation assistance; feasibility and descriptive study. Eur. Radiol. 2022, 32, 7640–7646. [Google Scholar] [CrossRef] [PubMed]
- Park, B.J.; Hunt, S.J.; Martin, C.; Nadolski, G.J.; Wood, B.J.; Gade, T.P. Augmented and Mixed Reality: Technologies for Enhancing the Future of IR. J. Vasc. Interv. Radiol. 2020, 31, 1074–1082. [Google Scholar] [CrossRef] [PubMed]
- Han, K.; Kim, J.H.; Yang, S.G.; Park, S.H.; Choi, H.-K.; Chun, S.-Y.; Kim, P.N.; Park, J.; Lee, M. A Single-Center Retrospective Analysis of Periprocedural Variables Affecting Local Tumor Progression after Radiofrequency Ablation of Colorectal Cancer Liver Metastases. Radiology 2021, 298, 212–218. [Google Scholar] [CrossRef]
- Paolucci, I.; Lin, Y.-M.; Jones, A.K.; Brock, K.K.; Odisio, B.C. Use of Contrast Media During CT-guided Thermal Ablation of Colorectal Liver Metastasis for Procedure Planning is Associated with Improved Immediate Outcomes. Cardiovasc. Interv. Radiol. 2023, 46, 327–336. [Google Scholar] [CrossRef]
- Sofocleous, C.T. Automated Segmentation of CT-guided Ablation Margins in Colorectal Liver Metastases: How We Move Forward to a Standardization of Ablation Zone Assessment. Radiology 2023, 307, e223276. [Google Scholar] [CrossRef]
- Hovet, S.; Ren, H.; Xu, S.; Wood, B.; Tokuda, J.; Tse, Z.T.H. MRI-powered biomedical devices. Minim. Invasive Ther. Allied Technol. 2018, 27, 191–202. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Charalampopoulos, G.; Bale, R.; Filippiadis, D.; Odisio, B.C.; Wood, B.; Solbiati, L. Navigation and Robotics in Interventional Oncology: Current Status and Future Roadmap. Diagnostics 2024, 14, 98. https://doi.org/10.3390/diagnostics14010098
Charalampopoulos G, Bale R, Filippiadis D, Odisio BC, Wood B, Solbiati L. Navigation and Robotics in Interventional Oncology: Current Status and Future Roadmap. Diagnostics. 2024; 14(1):98. https://doi.org/10.3390/diagnostics14010098
Chicago/Turabian StyleCharalampopoulos, Georgios, Reto Bale, Dimitrios Filippiadis, Bruno C. Odisio, Bradford Wood, and Luigi Solbiati. 2024. "Navigation and Robotics in Interventional Oncology: Current Status and Future Roadmap" Diagnostics 14, no. 1: 98. https://doi.org/10.3390/diagnostics14010098
APA StyleCharalampopoulos, G., Bale, R., Filippiadis, D., Odisio, B. C., Wood, B., & Solbiati, L. (2024). Navigation and Robotics in Interventional Oncology: Current Status and Future Roadmap. Diagnostics, 14(1), 98. https://doi.org/10.3390/diagnostics14010098








