Height Estimation from Vertebral Parameters on Routine Computed Tomography in a Contemporary Elderly Australian Population: A Validation of Existing Regression Models
Abstract
1. Introduction
2. Materials and Methods
2.1. Cohort
2.2. Image Analysis and Measurements
2.3. Data Collection
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
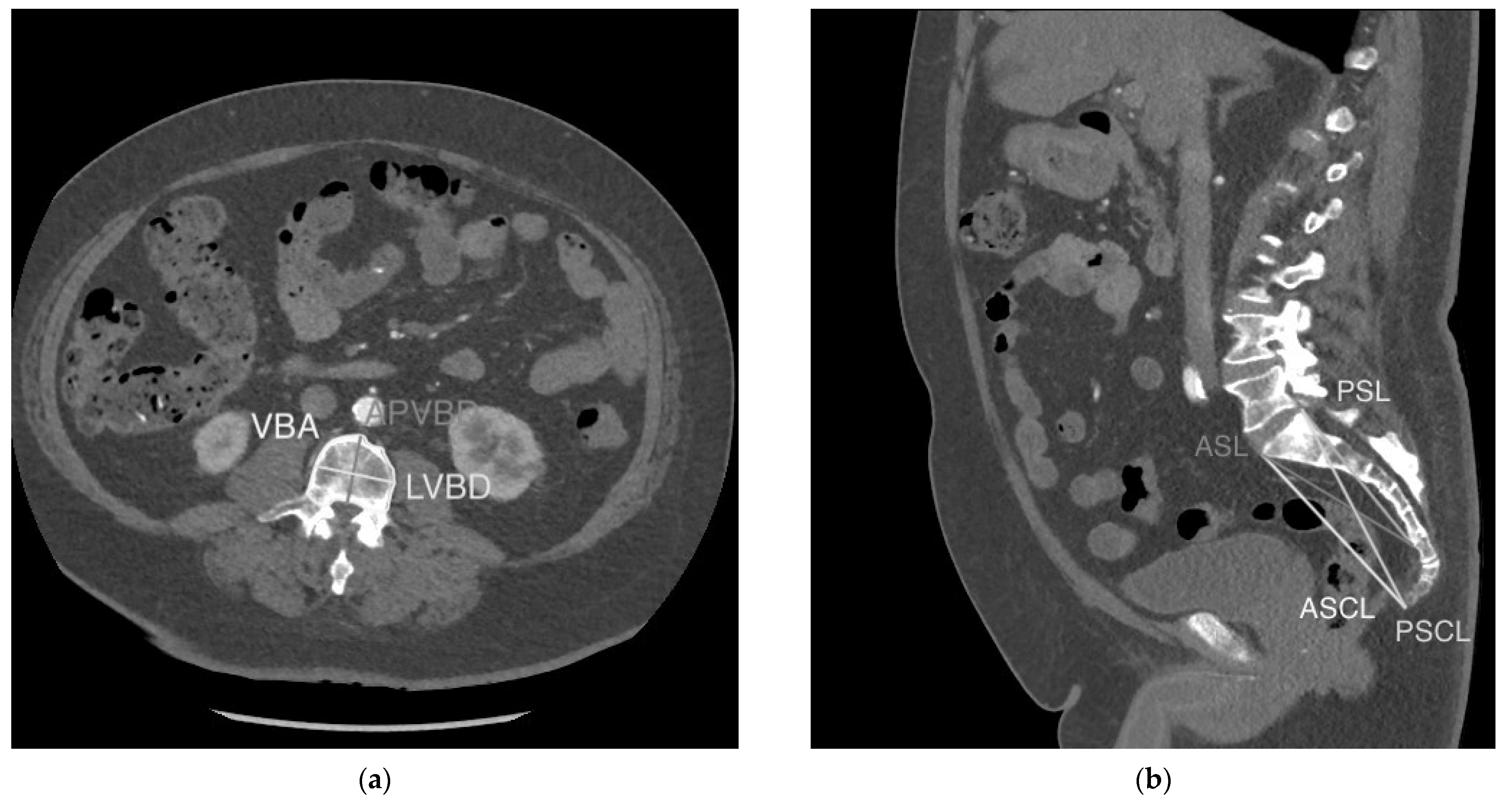
| VBA | Cross-sectional area of the vertebral body just inferior to the superior endplate |
| LVBD | Maximum linear distance between two points on the outer cortex of the vertebral body in the lateral (coronal) dimension on axial imaging just inferior to the superior endplate |
| APVBD | Maximum linear distance between two points on the outer cortex of the vertebral body in the antero-posterior (sagittal) dimension on axial imaging just inferior to the superior endplate |
| ASL | Linear distance between the most anterosuperior point of the first sacral vertebra (S1) and the most anteroinferior point of the fifth sacral vertebra (S5) |
| PSL | Linear distance between the most posterosuperior point of S1 and the most anteroinferior point of the S5 vertebral body |
| ASCL | Linear distance between the most anterosuperior point of S1 and the most anteroinferior point of the last coccygeal vertebral body |
| PSCL | Linear distance between the most posterosuperior point of S1 and the most anteroinferior point of the last coccygeal vertebral body |
References
- Levolger, S.; Van Vugt, J.L.; De Bruin, R.W.; IJzermans, J.N. Systematic review of sarcopenia in patients operated on for gastrointestinal and hepatopancreatobiliary malignancies. Br. J. Surg. 2015, 102, 1448–1458. [Google Scholar] [CrossRef] [PubMed]
- Jones, K.; Gordon-Weeks, A.; Coleman, C.; Silva, M. Radiologically determined sarcopenia predicts morbidity and mortality following abdominal surgery: A systematic review and meta-analysis. World J. Surg. 2017, 41, 2266–2279. [Google Scholar] [CrossRef] [PubMed]
- Boutin, R.D.; Yao, L.; Canter, R.J.; Lenchik, L. Sarcopenia: Current concepts and imaging implications. Am. J. Roentgenol. 2015, 205, W255–W266. [Google Scholar] [CrossRef]
- Fox, C.S.; Massaro, J.M.; Hoffmann, U.; Pou, K.; Maurovich-Horvat, P.; Liu, C. Abdominal visceral and subcutaneous adipose tissue compartments: Association with metabolic risk factors in the Framingham Heart Study. Circulation 2007, 116, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef]
- Heard, R.S.; Ramsay, G.; Hildebrand, D.R. Sarcopaenia in surgical populations: A review. Surgeon 2017, 15, 366–371. [Google Scholar] [CrossRef]
- Pelin, C.; Duyar, I.; Kayahan, E.M.; Zagyapan, R.; Ağildere, A.M.; Erar, A. Body height estimation based on dimensions of sacral and coccygeal vertebrae. J. Forensic Sci. 2005, 50, 294–297. [Google Scholar] [CrossRef]
- Trotter, M.; Gleser, G.C. Estimation of height from long bones of American Whites and Negroes. Am. J. Phys. Anthropol. 1952, 10, 463–514. [Google Scholar] [CrossRef]
- Zhan, M.J.; Fan, F.; Qiu, L.R.; Peng, Z.; Zhang, K.; Deng, Z.H. Estimation of stature and sex from sacrum and coccyx measurements by multidetector computed tomography in Chinese. Leg. Med. 2018, 34, 21–26. [Google Scholar] [CrossRef]
- Waduud, M.A.; Sucharitkul, P.P.; Drozd, M.; Gupta, A.; Hammond, C.; Ashbridge Scott, D.J. Validation of two-dimensional vertebral body parameters in estimating patient height in elderly patients. Br. J. Radiol. 2019, 92, 20190342. [Google Scholar] [CrossRef]
- Torimitsu, S.; Makino, Y.; Saitoh, H.; Ishii, N.; Hayakawa, M.; Yajima, D.; Inokuchi, G.; Motomura, A.; Chiba, F.; Iwase, H. Height estimation in Japanese cadavers using the sacral and coccygeal length measured with multidetector computed tomography. Leg. Med. 2014, 16, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Oura, P.; Korpinen, N.; Niinimäki, J.; Karppinen, J.; Niskanen, M.; Junno, J.A. Estimation of height from dimensions of the fourth lumbar vertebra in contemporary middle-aged Finns. Forensic Sci. Int. 2018, 292, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Karakas, H.M.; Celbis, O.; Harma, A.; Alicioglu, B. Total body height estimation using sacrum height in Anatolian Caucasians: Multidetector computed tomography-based virtual anthropometry. Skelet. Radiol. 2011, 40, 623–630. [Google Scholar] [CrossRef] [PubMed]
- Giroux, C.L.; Wescott, D.J. Height estimation based on dimensions of the bony pelvis and proximal femur. J. Forensic Sci. 2008, 53, 65–68. [Google Scholar] [CrossRef]
- Waduud, M.A.; Drozd, M.; Linton, E.; Wood, B.; Manning, J.; Bailey, M.A.; Hammond, C.; Scott, J.A. Influences of clinical experience in the quantification of morphometric sarcopaenia: A cohort study. Br. J. Radiol. 2018, 91, 20180067. [Google Scholar] [CrossRef]
- Maijanen, H. Testing anatomical methods for height estimation on individuals from the WM Bass donated skeletal collection. J. Forensic Sci. 2009, 54, 746–752. [Google Scholar] [CrossRef]
- Krishan, K.; Kanchan, T.; Menezes, R.G.; Ghosh, A. Forensic anthropology casework—Essential methodological considerations in height estimation. J. Forensic Nurs. 2012, 8, 45–50. [Google Scholar] [CrossRef]
- Zhang, K.; Chang, Y.F.; Fan, F.; Deng, Z.H. Estimation of height from radiologic anthropometry of the lumbar vertebral dimensions in Chinese. Leg. Med. 2015, 17, 483–488. [Google Scholar] [CrossRef]
- Pickhardt, P.J.; Graffy, P.M.; Zea, R.; Lee, S.J.; Liu, J.; Sandfort, V.; Summers, R.M. Automated CT biomarkers for opportunistic prediction of future cardiovascular events and mortality in an asymptomatic screening population: A retrospective cohort study. Lancet Digit. Health 2020, 2, e192–e200. [Google Scholar] [CrossRef]
- Zopfs, D.; Theurich, S.; Grosse Hokamp, N.; Knuever, J.; Gerecht, L.; Borggrefe, J.; Schlaak, M.; dos Santos, D.P. Single-slice CT measurements allow for accurate assessment of sarcopenia and body composition. Eur. Radiol. 2020, 30, 1701–1708. [Google Scholar] [CrossRef]
- Willey, P.; Falsetti, T. Inaccuracy of height information on driver’s licenses. J. Forensic Sci. 1991, 36, 813–819. [Google Scholar] [CrossRef] [PubMed]
- Beaudart, C.; Dawson, A.; Shaw, S.C.; Harvey, N.C.; Kanis, J.A.; Binkley, N.; Reginster, J.Y.; Chapurlat, R.; Chan, D.C.; Bruyère, O.; et al. Nutrition and physical activity in the prevention and treatment of sarcopenia: Systematic review. Osteoporos. Int. 2017, 28, 1817–1833. [Google Scholar] [CrossRef] [PubMed]
- Choong, C.L.; Alias, A.; Abas, R.; Wu, Y.S.; Shin, J.Y.; Gan, Q.F.; Thu, K.M.; Choy, K.W. Application of anthropometric measurements analysis for stature in human vertebral column: A systematic review. Forensic Imaging 2020, 20, 200360. [Google Scholar] [CrossRef]
- Klein, A.; Nagel, K.; Gührs, J.; Poodendaen, C.; Püschel, K.; Morlock, M.M.; Huber, G. On the relationship between height and anthropometric measurements of lumbar vertebrae. Sci. Justice 2015, 55, 383–387. [Google Scholar] [CrossRef]
| Study | Age (Mean +/− SD) | Vertebral Parameter Used | Regression Equation (H = Height (cm)) | Accuracy |
|---|---|---|---|---|
| Zhan et al. (2018) [9] Contemporary Chinese population (n = 160) | 50 ± 13 | ASL | SEE = 5.546 | |
| PSL | SEE = 5.268 | |||
| ASCL | SEE = 5.525 | |||
| PSCL | SEE = 5.239 | |||
| Torimitsu et al. (2014) [11] Contemporary Japanese cadaveric population (n = 106) | 56 ± 20 | ASL | SEE = 7.84 cm | |
| PSL | SEE = 7.15 cm | |||
| ASCL | SEE = 7.41 cm | |||
| PSCL | SEE = 6.68 cm | |||
| Oura et al. (2018) [12] Contemporary middle-aged Finnish population (n = 742) | 47 ± 0 | VBA | SEE = 4.971 cm | |
| Waduud et al. (2019) [10] Contemporary elderly British population (n = 255, combined sex cohort) | 75 ± 8 (combined sex cohort) | L3 VBA | Difference from actual height (mean ± SD): 0.6 ± 6.3 (p = 0.276) | |
| L3 APVBD | Difference from actual height (mean ± SD): 0.8 ± 6.6 (p = 0.164) | |||
| L3 LVBD | Difference from actual height (mean ± SD): 0.7 ± 6.6 (0.222) |
| Study | Age (Mean ± SD) | Vertebral Parameter Used | Regression Equation (H = Height (cm)) | Accuracy |
|---|---|---|---|---|
| Zhan et al. (2018) [9] Contemporary Chinese population (n = 190) | 55 ± 11 | ASL | SEE = 5.829 | |
| PSL | SEE = 5.716 cm | |||
| ASCL | SEE = 6.094 | |||
| PSCL | SEE = 6.012 | |||
| Torimitsu et al. (2014) [11] Contemporary Japanese cadaveric population (n = 110) | 57 ± 20 | ASL | SEE = 5.98 cm | |
| PSL | SEE = 5.83 cm | |||
| ASCL | SEE = 5.94 cm | |||
| PSCL | SEE = 5.98 cm | |||
| Karakas et al. (2011) [13] Contemporary Anatolian Caucasian population (n = 66) | 42 ± 15 | ASL | SEE = 5.69 cm | |
| Oura et al. (2018) [12] Contemporary middle-aged Finnish population (n = 616) | 47 ± 0 | L4 VBA | SEE = 5.412 cm | |
| Waduud et al. (2019) [10] Contemporary elderly British population (n = 255, combined sex cohort) | 75 ± 8 (combined sex cohort) | L3 VBA | Difference from actual height (mean ± SD): 0.6 ± 6.3 (p = 0.276) | |
| L3 APVBD | Difference from actual height (mean ± SD): 0.8 ± 6.6 (p = 0.164) | |||
| L3 LVBD | Difference from actual height (mean ± SD): 0.7 ± 6.6 (0.222) |
| Female Participants, n = 45 | Male Participants, n = 51 | |||||||
|---|---|---|---|---|---|---|---|---|
| Minimum | Maximum | Mean | Std. Deviation | Minimum | Maximum | Mean | Std. Deviation | |
| Age (years) | 62.0 | 92.0 | 81.8 | ±6.2 | 57.0 | 92.0 | 79.1 | ±7.7 |
| Height (cm) | 140.0 | 180.0 | 158.2 | ±7.9 | 155.0 | 192.0 | 171.3 | ±6.9 |
| Weight (kg) | 40 | 143 | 68.9 | 21.7 | 49 | 146 | 81.6 | 20 |
| L3 VBA | 9.9 | 16.0 | 12.8 | ±1.6 | 12.5 | 22.5 | 16.0 | ±2.3 |
| L3 LVBD | 32.5 | 52.6 | 43.9 | ±4.4 | 41.6 | 59.9 | 49.2 | ±3.7 |
| L3 APVBD | 30 | 46.5 | 33.3 | ±3.1 | 31.8 | 46.5 | 37.0 | ±3.2 |
| L4 VBA | 9.9 | 16.1 | 13.5 | ±1.7 | 12.2 | 24.3 | 16.8 | ±2.6 |
| L4 LVBD | 36.5 | 55.5 | 45.6 | ±4.1 | 43.3 | 72.8 | 50.7 | ±4.8 |
| L4 APVBD | 28.6 | 38.0 | 33.1 | ±2.0 | 31.8 | 45.1 | 36.9 | ±3.1 |
| ASSL | 69.5 | 133.0 | 108.0 | ±13.5 | 98.0 | 147.0 | 115.8 | ±10.8 |
| PSSL | 78.0 | 139.0 | 109.1 | ±12.4 | 100.0 | 146.0 | 119.5 | ±10.4 |
| ASCL | 86.4 | 152.0 | 118.5 | ±15.3 | 103 | 157 | 130.0 | ±11.4 |
| PSCL | 98.4 | 157 | 126.4 | ±14.4 | 118 | 165 | 141.9 | ±10.3 |
| Comorbidity | Female Sex, Number (%) | Male Sex, Number (%) |
|---|---|---|
| Osteoporosis | 6 (13) | 1 (2) |
| Hypertension | 34 (78) | 45 (88) |
| Ischaemic heart disease | 10 (22) | 27 (53) |
| Cerebrovascular disease | 7 (16) | 10 (20) |
| Diabetes mellitus | 12 (27) | 20 (39) |
| Chronic kidney disease | 11 (24) | 12 (24) |
| Chronic liver disease | 2 (4) | 2 (4) |
| Cancer | 11 (24) | 9 (18) |
| Study | Regression Equation | Calculated Height (Mean ± SD) | Difference from Actual Height (Mean ± SD) | p-Value |
|---|---|---|---|---|
| Zhan et al., 2018 [9] | 154.9 ± 2.6 | 3.3 ± 6.7 | 0.002 | |
| Zhan et al., 2018 [9] | 155.3 ± 3.9 | 2.9 ± 6.8 | 0.007 | |
| Zhan et al., 2018 [9] | 154.5 ± 2.5 | 3.7 ± 7.0 | 0.001 | |
| Zhan et al., 2018 [9] | 154.7 ± 3.6 | 3.5 ± 7.1 | 0.002 | |
| Torimitsu et al., 2014 [11] | 156.4 ± 5.2 | 1.8 ± 6.5 | 0.063 | |
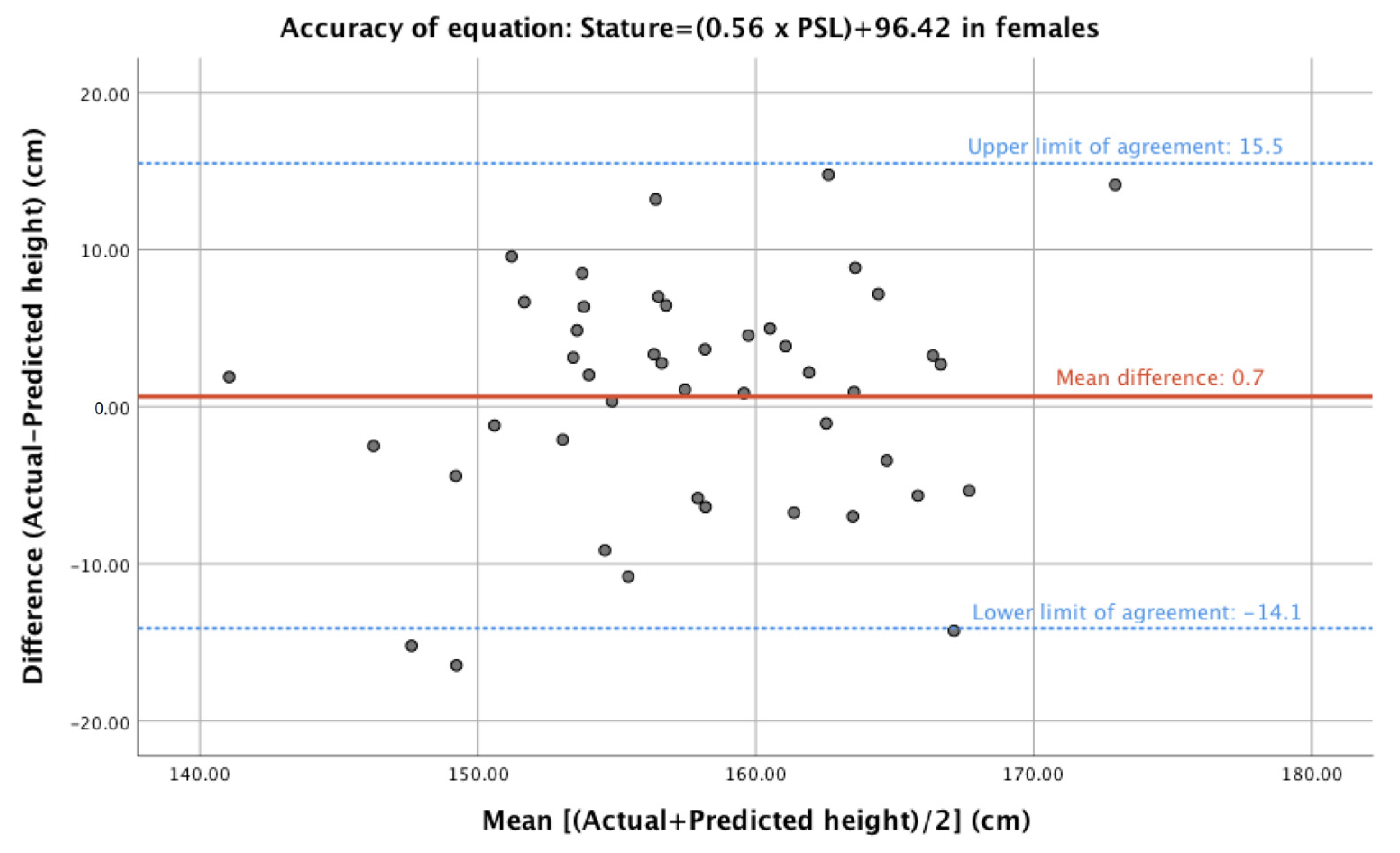
| Torimitsu et al., 2014 [11] | 157.5 ± 7.0 | 0.7 ± 7.4 | 0.523 | |
| Torimitsu et al., 2014 [11] | 154.6 ± 7.2 | 3.6 ± 7.5 | 0.003 | |
| Torimitsu et al., 2014 [11] | 156.1 ± 8.0 | 2.1 ± 8.4 | 0.100 | |
| Oura et al., 2018 [12] | 171.6 ± 3.8 | −13.4 ± 7.3 | 0.000 | |
| Waduud et al., 2019 [10] | 165.9 ± 2.0 | −7.7 ± 7.6 | <0.001 | |
| Waduud et al., 2019 [10] | 165.3 ± 2.8 | −7.1 ± 8.3 | 0.000 | |
| Waduud et al., 2019 [10] | 166.0 ± 2.5 | −7.8 ± 7.6 | 0.000 |
| Study | Regression Equation | Calculated Height (Mean ± SD) | Difference from Actual Height (Mean ± SD) | p-Value |
|---|---|---|---|---|
| Zhan et al., 2018 [9] | 167.3 ± 2.9 | 4.0 ± 7.2 | 0.000 | |
| Zhan et al., 2018 [9] | 168.1 ± 3.3 | 3.2 ± 7.0 | 0.002 | |
| Zhan et al., 2018 [9] | 166.6 ± 1.9 | 4.7 ± 6.8 | 0.000 | |
| Zhan et al., 2018 [9] | 167.2 ± 2.0 | 4.1 ± 6.5 | 0.000 | |
| Torimitsu et al., 2014 [11] | 169.7 ± 3.4 | 1.5 ± 7.4 | 0.145 | |
| Torimitsu et al., 2014 [11] | 195.0 ± 4.5 | −23.8 ± 7.4 | 0.000 | |
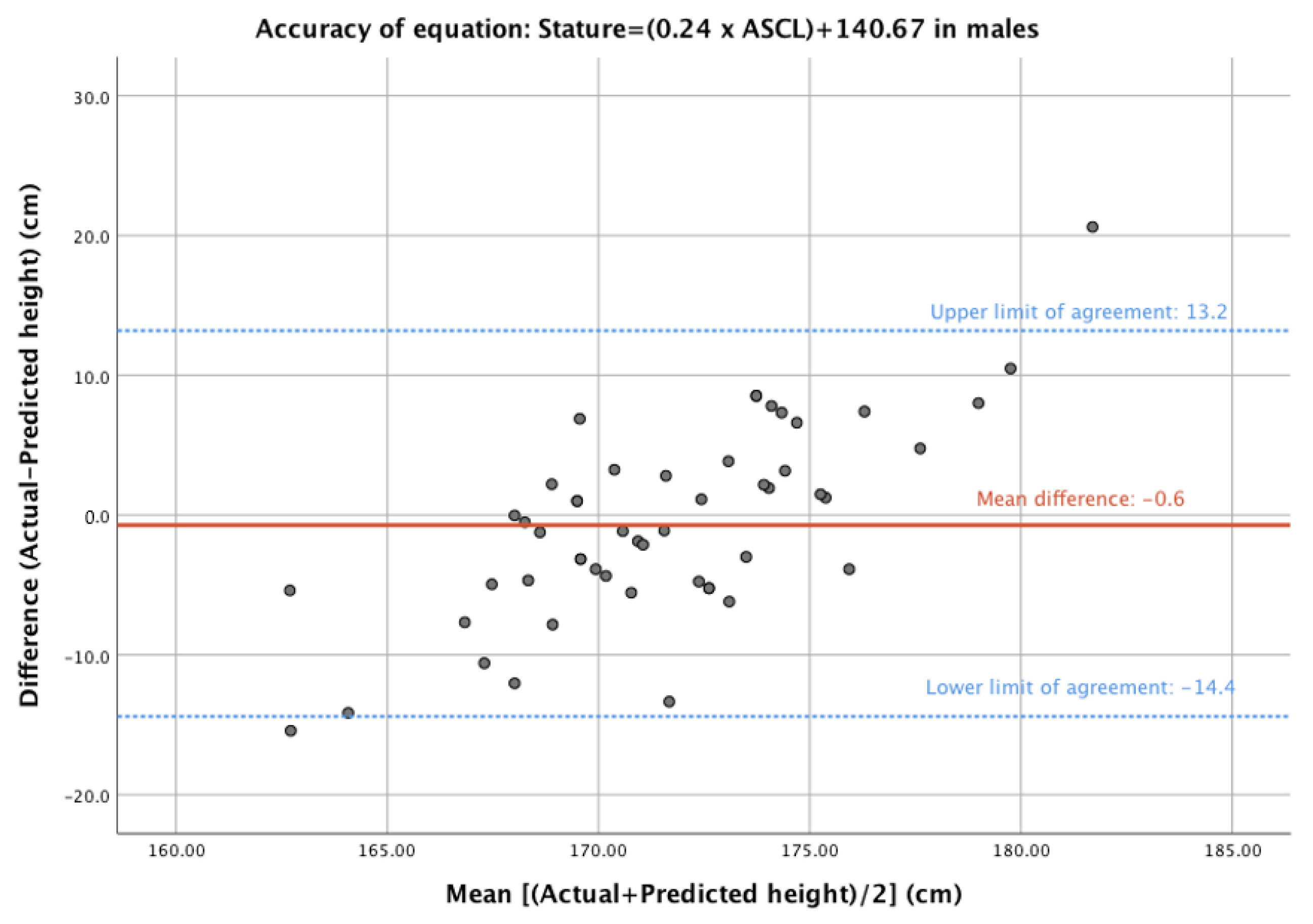
| Torimitsu et al., 2014 [11] | 171.9 ± 2.7 | −0.6 ± 6.9 | 0.544 | |
| Torimitsu et al., 2014 [11] | 214.4 ± 4.3 | −43.1 ± 6.9 | 0.000 | |
| Karakas et al., 2011 [13] | 173.3 ± 3.3 | −2.1 ± 7.3 | 0.051 | |
| Oura et al., 2018 [12] | 184.7 ± 4.4 | −13.4 ± 7.6 | 0.000 | |
| Waduud et al., 2019 [10] | 177.0 ± 3.0 | −5.74 ± 6.9 | 0.000 | |
| Waduud et al., 2019 [10] | 175.7 ± 3.1 | −4.4 ± 6.4 | 0.000 | |
| Waduud et al., 2019 [10] | 177.2 ± 2.1 | −6.0 ± 6.9 | 0.000 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Flanders, D.; Lai, T.; Kutaiba, N. Height Estimation from Vertebral Parameters on Routine Computed Tomography in a Contemporary Elderly Australian Population: A Validation of Existing Regression Models. Diagnostics 2023, 13, 1222. https://doi.org/10.3390/diagnostics13071222
Flanders D, Lai T, Kutaiba N. Height Estimation from Vertebral Parameters on Routine Computed Tomography in a Contemporary Elderly Australian Population: A Validation of Existing Regression Models. Diagnostics. 2023; 13(7):1222. https://doi.org/10.3390/diagnostics13071222
Chicago/Turabian StyleFlanders, Damian, Timothy Lai, and Numan Kutaiba. 2023. "Height Estimation from Vertebral Parameters on Routine Computed Tomography in a Contemporary Elderly Australian Population: A Validation of Existing Regression Models" Diagnostics 13, no. 7: 1222. https://doi.org/10.3390/diagnostics13071222
APA StyleFlanders, D., Lai, T., & Kutaiba, N. (2023). Height Estimation from Vertebral Parameters on Routine Computed Tomography in a Contemporary Elderly Australian Population: A Validation of Existing Regression Models. Diagnostics, 13(7), 1222. https://doi.org/10.3390/diagnostics13071222





