Incidence of Intoxications in the Emergency Department of Galati Hospital with Examples of Cardiovascular Effects of MDMA Intoxication
Abstract
1. Introduction
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Characteristics of Eligible Studies
3. Results
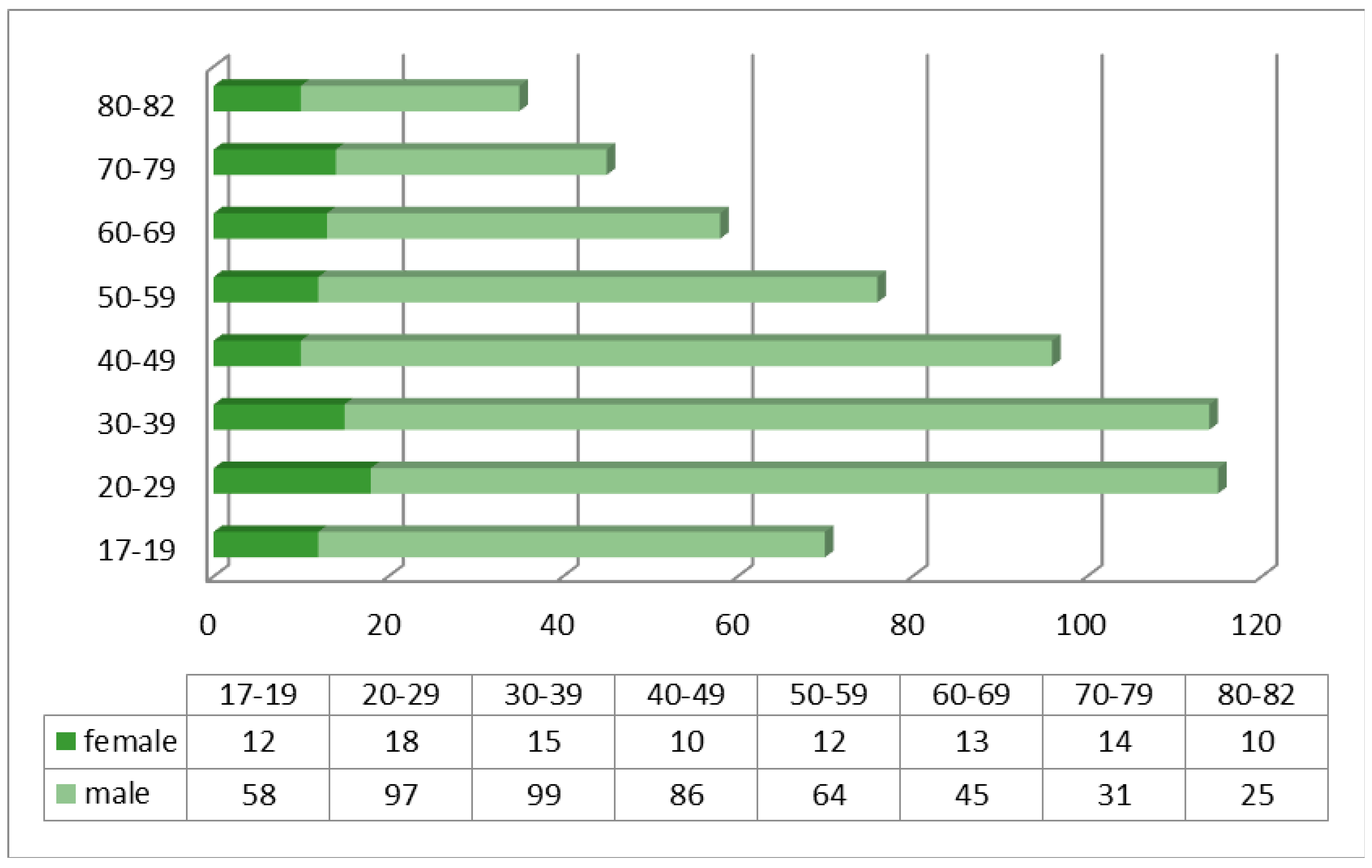
3.1. Characteristics of the Studied Batch
3.2. Characteristics of Intoxications
3.3. Cases Report—Study on the Different Outcomes of Two Patients Admitted to the ED for Acute MDMA Intoxication
- -
- Two peripheral venous lines;
- -
- Intra-osseous access;
- -
- Mechanical ventilation + oro-tracheal intubation without induction;
- -
- Continuous monitoring (blood pressure, SaO2 (Oxygen Saturation), the ventricular allura, the ejection fraction), EKG
- -
- Nasogastric tube mounting;
- -
- Urinary bladder catheter mounting (500 mL of normal urine);
- -
- The cardiological examination: the Cardio-respiratory arrest ≥ with external cardiac massage;
- First patient L.I.: the patient presented leukocytosis in remission during this period, with a gradual decrease in PLT (up to a value of 105). Glycemic values were maintained above the threshold of 150 mg/dL, with a maximum value of 183 mg/dL. Normalization of liver indicators values (with remission of hepatocytolysis syndrome). At the same time, the CRP value was over 30 × normal (Table 4).
- The second patient, C.I., presented evolving leukopenia, up to a minimum value of 8.45, with a co-morbid decrease in HBG (minimum value of 14.2). This time, discrete thrombocytopenia was noted, with a decrease in values over the 3 days from 202 to 146. Compared to the previous patient, this young man had low blood glucose values, with a MV of 100 mg/dL. The hepatocytolysis syndrome detected at the time of admission can be justified by MDMA ingestion, with GOT and TGP values exceeding the threshold of 1900 mg/dL. It should be noted that this patient had increased CK values (from 25,003 to 7383) (Table 5).
| Patient L.I. | WBC | HBG | NEU | PLT | TP | INR | TMF | Glucose | TGP | TGO | Creatinine | RA | CK | Cl Serum | Sodium | CRP |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 23 April 2021 | 13.04 | 14.7 | 12.21 | 191 | 15.8 | 1.3 | 151 | 329 | 354 | 1.67 | 35 | 109.9 | 150 | |||
| 24 April 2021 | 30.1 | |||||||||||||||
| 25 April 2021 | 14.85 | 13.2 | 12.84 | 130 | 15.6 | 1.28 | Positive | 169 | 243 | 155 | 1.16 | 34 | 3605 | 112.4 | 151 | |
| 26 April 2021 | 11.8 | 13 | 9.78 | 105 | 14.5 | 1.18 | Positive | 183 | 183 | 75 | 1.03 | 26 | 2671 | 112.1 | 148 |
| Patient C.I. | WBC | HBG | NEU | PLT | TP | INR | TMF | Glucose | TGP | TGO | Creatinine | RA | CK | CL Serum | Sodium | CRP |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 23 April 2021 | 12.26 | 15.06 | 10.33 | 202 | 14.1 | 1.14 | 87 | 2583 | 2583 | 1.14 | 25 | 103 | 141 | |||
| 24 April 2021 | ||||||||||||||||
| 25 April 2021 | 8.55 | 14.8 | 6.35 | 160 | 15.1 | 1.24 | 120 | 1671 | 1701 | 0.9 | 26 | 25,003 | 104.8 | 139 | ||
| 26 April 2021 | 8.45 | 14.2 | 5.88 | 146 | 14.6 | 1.19 | 93 | 309 | 480 | 0.81 | 25 | 7383 | 106.4 | 142 |
- -
- The first patient, L.I., was taken in with extremely serious general condition, comatose, unresponsive to painful stimuli, GCS—3 points, required IOT + MV for stabilization. On arrival in the emergency room, the patient was fully monitored, but during consultations, presented with resuscitable CRA. The cardiological examination showed an EF of 40%, hypokinesis of the cardiac muscle, probably in the context of the existence of a post-internal IMA. During the other days of hospitalization, the parameters normalized, with a slowly favourable evolution.
- -
- The second patient, C.I., (with the same characteristics—age 32 years, male) showed the following at the time of pick-up by the ambulance crew: GCS = 15 points, conscious, hardly cooperative, responds with difficulty to painful and verbal stimuli. He associates liver damage during admission, with marked hepatocytolysis syndrome, with consequent increase in CK and LDH, respectively.
4. Discussion
Limits of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACE | Angiotensin Converting Enzyme |
| BP | Blood Pressure |
| CRA | Cardio-Respiratory Arrest |
| ICU | Intensive Care Unit |
| IMA | Acute infarction of the myocardium |
| ED | Emergency Department |
| EF | Fraction the ejection |
| GCS | Glasgow Coma Scale |
| HBG | haemoglobin |
| HDL | hight density lipoproteins |
| NEU | neutrophil |
| PLT | platelets |
| TP | prothrombin time |
| IRN | International Normalized Ratio |
| TMF | fibrin monomer test |
| RA | alkaline reserve |
| CK | creatinine kinase |
| Cl | Clearance serum |
| CRP | C-reactive protein |
| WBC | Leukocytes count/ white blood cell count |
| MDMA | methylene-dioxy-methAmphetamine |
| SaO2 | Oxygen Saturation |
| GTP(ALAT) | Transaminase |
| GOT(ASAT) | Transaminase |
| VM | Mechanical ventilation |
| IOT | Orotracheal intubation |
References
- Vermes, A.; Roelofsen, E.E.; Sabadi, G.; van den Berg, B.; de Quelerij, M.; Vulto, A.G. Therapeutic and illicit drug intoxication and hospitalization in a Dutch university hospital. Dutch J. Med. 2003, 61, 168–172. [Google Scholar]
- Indig, D.; Copeland, J.; Conigrave, K.M.; Arcuri, A. Characteristics and comorbidity of drug- and alcohol-related Emergency Department presentations detected by medical triage text. Addiction 2010, 105, 897–906. [Google Scholar] [CrossRef] [PubMed]
- Verelst, S.; Moonen, P.J.; Desruelles, D.; Gillet, J.B. Emergency Department visits due to alcohol intoxication: Patient characteristics and impact on the Emergency Room. Alcohol Alcohol. 2012, 47, 433–438. [Google Scholar] [CrossRef]
- Newton, A.; Sarker, S.J.; Pahal, G.S.; van den Bergh, E.; Young, C. The impact of the new UK licensing law on Emergency Hospital attendances: A cohort study. Emerg. Med. J. 2007, 24, 532–534. [Google Scholar] [CrossRef] [PubMed]
- Parkinson, K.; Newbury-Birch, D.; Phillipson, A.; Hindmarch, P.; Kaner, E.; Stamp, E.; Vale, L.; Wright, J.; Connolly, J. Prevalence of alcohol related attendance at an inner-city emergency department and its impact: A dual prospective and retrospective cohort study. Emerg. Med. J. 2016, 33, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Rood, P.P.; Haagsma, J.A.; MBoersma, S.; Tancica, A.; Van Lieshout, E.M.; Mulligan, T.; Van De Mheen, D.; Van Beeck, E.F.; Patka, P. Psychoactive substance (drugs and alcohol) uses by Emergency Department patients before injury. Eur. J. Emerg. Med. Off. J. Eur. Soc. Emerg. Med. 2016, 23, 147–154. [Google Scholar] [CrossRef]
- European Monitoring Centre for Drugs and Drug Addiction. 2000 Annual Report on the State of the Drugs Problem in the European Union; Publications Office of the European Union: Luxembourg, 2000. [Google Scholar]
- Oyefeso, A.; Ghodse, H.; Clancy, C.; Corkery, J.; Goldfinch, R. Drug abuse-related mortality: A study of teenage addicts over a 20-year period. Soc. Psychiatry Psychiatr. Epidemiol. 1999, 34, 437–441. [Google Scholar] [CrossRef]
- Kalant, H. The pharmacology and toxicology of “ecstasy” (MDMA) and related drugs. CMAJ 2001, 165, 917–928. [Google Scholar]
- Rochester, J.A.; Kirchner, J.T. Ecstasy (3,4-methylenedioxymethamphetamine): History, neurochemistry, and toxicology. J. Am. Board Fam. Pract. 1999, 12, 137–142. [Google Scholar] [CrossRef]
- Shannon, M. Methylenedioxymethamphetamine (MDMA, “Ecstasy”). Pediatr. Emerg. Care 2000, 16, 377–380. [Google Scholar] [CrossRef]
- Thompson, J.P. Acute effects of drugs of abuse. Clin. Med. 2003, 3, 123. [Google Scholar] [CrossRef] [PubMed]
- Ghuran, A.; Nolan, J. Recreational drug misuse: Issues for the cardiologist. Heart 2000, 83, 627–633. [Google Scholar] [CrossRef] [PubMed]
- Gummin, D.D.; Mowry, J.B.; Spyker, D.A.; Brooks, D.E.; Fraser, M.O.; Banner, W. 2016 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 34th Annual Report. Clin. Toxicol. 2017, 55, 1072–1252. [Google Scholar] [CrossRef] [PubMed]
- Ambrosius, R.G.; Vroegop, M.P.; Jansman, F.G.; Hoedemaekers, C.W.; Aarnoutse, R.E.; van der Wilt, G.J.; Kramers, C. Patients with acute poisoning presenting to an Emergency Department in the Netherlands: Admitted or not? Prospective testing of two algorithms. Emerg. Med. J. 2012, 29, 467–472. [Google Scholar] [CrossRef]
- Kowalenko, T.; Burgess, B.; Szpunar, S.M.; Irvin-Babcock, C.B. Alcohol and trauma—In every age group. Am. J. Emerg. Med. 2013, 31, 705–709. [Google Scholar] [CrossRef]
- Mullins, P.M.; Mazer-Amirshahi, M.; Pines, J.M. Alcohol-Related Visits to US Emergency Departments, 2001–2011. Alcohol Alcohol. 2017, 52, 119–125. [Google Scholar] [CrossRef]
- Cherpitel, C.J.; Ye, Y. Trends in alcohol- and drug-related emergency department and primary care visits: Data from four U.S. national surveys (1995–2010). J. Stud. Alcohol Drugs 2012, 73, 454–458. [Google Scholar] [CrossRef]
- Crane, E.H. Highlights of the 2011 drug abuse warning network (DAWN) findings on drug-related emergency department visits. In The CBHSQ Report; Substance Abuse and Mental Health Services Administration: Rockville, Australia, 2013. [Google Scholar]
- Wood, D.M.; Greene, S.L.; Dargan, P.I. Five-year trends in self-reported recreational drugs associated with presentation to a UK emergency department with suspected drug-related toxicity. Eur. J. Emerg. Med. Off. J. Eur. Soc. Emerg. Med. 2013, 20, 263–267. [Google Scholar] [CrossRef]
- Bush, D.M. Emergency department visits involving nonmedical use of the anti-anxiety medication alprazolam. In The CBHSQ Report; Substance Abuse and Mental Health Services Administration: Rockville, Australia, 2014. [Google Scholar]
- Maughan, B.C.; Bachhuber, M.A.; Mitra, N.; Starrels, J.L. Prescription monitoring programs and emergency department visits involving opioids, 2004–2011. Drug Alcohol Depend. 2015, 156, 282–288. [Google Scholar] [CrossRef]
- Jann, M.; Kennedy, W.K.; Lopez, G. Benzodiazepines: A major component in unintentional prescription drug overdoses with opioid analgesics. J. Pharm. Pract. 2014, 27, 5–16. [Google Scholar] [CrossRef]
- Whiteford, H.A.; Degenhardt, L.; Rehm, J.; Baxter, A.J.; Ferrari, A.J.; Erskine, H.E.; Charlson, F.J.; Norman, R.E.; Flaxman, A.D.; Johns, N.; et al. Global burden of disease attributable to mental and substance use disorders: Findings from the Global Burden of Disease Study 2010. Lancet 2013, 382, 1575–1586. [Google Scholar] [CrossRef] [PubMed]
- Patel, V.; Chisholm, D.; Parikh, R.; Charlson, F.J.; Degenhardt, L.; Dua, T.; Ferrari, A.J.; Hyman, S.; Laxminarayan, R.; Levin, C.; et al. Addressing the burden of mental, neurological, and substance use disorders: Key messages from Disease Control Priorities, 3rd edition. Lancet 2016, 387, 1672–1685. [Google Scholar] [CrossRef] [PubMed]
- Egerton-Warburton, D.; Gosbell, A.; Wadsworth, A.; Moore, K.; Richardson, D.B.; Fatovich, D.M. Perceptions of Australasian emergency department staff of the impact of alcohol-related presentations. Med. J. Aust. 2016, 204, 155. [Google Scholar] [CrossRef] [PubMed]
- Pirmohamed, M.; Brown, C.; Owens, L.; Luke, C.; Gilmore, I.T.; Breckenridge, A.M.; Park, B.K. The burden of alcohol misuse on an inner-city general hospital. QJM Mon. J. Assoc. Physicians 2000, 93, 291–295. [Google Scholar] [CrossRef] [PubMed]
- Statistics Netherlands. Stat Line Database. Available online: https://opendata.cbs.nl/statline/#/CBS/nl/dataset/70072ned/table?dl=24235 (accessed on 15 November 2022).
- Ghodse, H.; Clancy, C.; Oyefeso, A.; Pollard, M.; Corkery, J.; Lind, J. Drug Related Deaths Asreported by the Coroners in England and Wales July–December 1998; Centre for Addiction Studies, St George’s Hospital Medical School: London, UK, 1999. [Google Scholar]
- Vongpatanasin, W.; Mansour, Y.; Chavoshan, B.; Arbique, D.; Victor, R.G. Cocaine stimulates the human cardiovascular system via a central mechanism of action. Circulation 1999, 100, 497–502. [Google Scholar] [CrossRef] [PubMed]
- Imlach Gunasekara, F.; Butler, S.; Cech, T.; Curtis, E.; Douglas, M.; Emmerson, L.; Greenwood, R.; Huse, S.; Jonggowisastro, J.; Lees, C.; et al. How do intoxicated patients impact staff in the emergency department? An exploratory study. N. Z. Med. J. 2011, 124, 14–23. [Google Scholar] [PubMed]
- Mouhaffel, A.H.; Madu, E.C.; Satmary, W.A.; Fraker, T.D., Jr. Cardiovascular complications of cocaine. Chest 1995, 107, 1426–1434. [Google Scholar] [CrossRef] [PubMed]
- Bonsignore, A.; Barranco, R.; Morando, A.; FraternaliOrcioni, G.; Ventura, F. MDMA Induced Cardio-toxicity and Pathological Myocardial Effects: A Systematic Review of Experimental Data and Autopsy Findings. Cardiovasc. Toxicol. 2019, 19, 493–499. [Google Scholar] [CrossRef]
- Kafle, P.; Shrestha, B.; Mandal, A.; Sharma, D.; Bhandari, M.; Amgai, B.; Khalid, M.; Sidhu, J.S.; Solaimanzadeh, I.; Gayam, V.; et al. Ecstasy induced acute systolic heart failure and Non-Ischemic Cardiomyopathy in a young female: A rare case report and literature review. J. Community Hosp. Intern. Med. Perspect. 2019, 9, 336–339. [Google Scholar] [CrossRef]
- Koczor, C.A.; Ludlow, I.; Hight, R.S., 2nd; Jiao, Z.; Fields, E.; Ludaway, T.; Russ, R.; Torres, R.A.; Lewis, W. Ecstasy (MDMA) Alters Cardiac Gene Expression and DNA Methylation: Implications for Circadian Rhythm Dysfunction in the Heart. Toxicol. Sci. Off. J. Soc. Toxicol. 2015, 148, 183–191. [Google Scholar] [CrossRef]
- Ghuran, A.; van Der Wieken, L.R.; Nolan, J. Cardiovascular complications of recreational drugs. BMJ 2001, 323, 464–466. [Google Scholar] [CrossRef] [PubMed]
- De La Torre, R.; Yubero-Lahoz, S.; Pardo-Lozano, R.; Farré, M. MDMA, methamphetamine, and CYP2D6 pharmacogenetics: What is clinically relevant? Front. Genet. 2012, 3, 235. [Google Scholar] [CrossRef] [PubMed]
- Di Nunno, N.; Esposito, M.; Argo, A.; Salerno, M.; Sessa, F. Pharmacogenetics and Forensic Toxicology: A New Step towards a Multidisciplinary Approach. Toxics 2021, 9, 292. [Google Scholar] [CrossRef] [PubMed]



| Year | Number of Patients |
|---|---|
| 2014 | 86,560 |
| 2015 | 85,610 |
| 2016 | 85,990 |
| Type of Intoxication | Day |
|---|---|
| Intentional exposure | 85 |
| Unintentional exposure | 15 |
| Day of presentation in ED | |
| Monday-Thursday | 38 |
| Friday-Sunday | 62 |
| Time of presentation | |
| Presentation hour 08:00–20:00 | 55 |
| 20:00–08:00 | 45 |
| Admission to Internal Medicine Department | 25 |
| Intensive Care Admission | 15 |
| Discharge home | 66 |
| Addiction centre/police orientation | 5 |
| Left Emergency Department without medical advice | 4 |
| Solution of Intoxications | Female | Male |
|---|---|---|
| Chlorine | 8 | 9 |
| Detergent | 4 | 3 |
| Paint | 1 | 1 |
| Hydrogen Peroxide | 1 | 0 |
| Rodenticide | 2 | 3 |
| Antifreeze | 2 | 2 |
| Furadan | 1 | 1 |
| Sodium hydroxide | 1 | 3 |
| Organophosphorus | 3 | 6 |
| Pesticide | 1 | 0 |
| Formaldehyde | 1 | 0 |
| Carbon-monoxide | 0 | 3 |
| Pre-release | 0 | 1 |
| Thinner | 0 | 4 |
| Descaling agent | 3 | 1 |
| Tomoxan | 0 | 1 |
| Royal water | 0 | 1 |
| Iodpovidone | 0 | 1 |
| Copper Sulphate | 0 | 1 |
| Petrol | 1 | 0 |
| Diesel | 0 | 1 |
| Plant fertiliser | 0 | 1 |
| Paint and thinner | 0 | 1 |
| Chlorine and detergent | 0 | 3 |
| Chlorine and antifreeze | 0 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dragomir, L.; Marina, V.; Anghele, M.; Anghele, A.-D.; Moscu, C.A. Incidence of Intoxications in the Emergency Department of Galati Hospital with Examples of Cardiovascular Effects of MDMA Intoxication. Diagnostics 2023, 13, 940. https://doi.org/10.3390/diagnostics13050940
Dragomir L, Marina V, Anghele M, Anghele A-D, Moscu CA. Incidence of Intoxications in the Emergency Department of Galati Hospital with Examples of Cardiovascular Effects of MDMA Intoxication. Diagnostics. 2023; 13(5):940. https://doi.org/10.3390/diagnostics13050940
Chicago/Turabian StyleDragomir, Liliana, Virginia Marina, Mihaela Anghele, Aurelian-Dumitrache Anghele, and Cosmina Alina Moscu. 2023. "Incidence of Intoxications in the Emergency Department of Galati Hospital with Examples of Cardiovascular Effects of MDMA Intoxication" Diagnostics 13, no. 5: 940. https://doi.org/10.3390/diagnostics13050940
APA StyleDragomir, L., Marina, V., Anghele, M., Anghele, A.-D., & Moscu, C. A. (2023). Incidence of Intoxications in the Emergency Department of Galati Hospital with Examples of Cardiovascular Effects of MDMA Intoxication. Diagnostics, 13(5), 940. https://doi.org/10.3390/diagnostics13050940







