Diagnostic Performance of Two-Dimensional Ultrasound, Two-Dimensional Sonohysterography and Three-Dimensional Ultrasound in the Diagnosis of Septate Uterus—A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
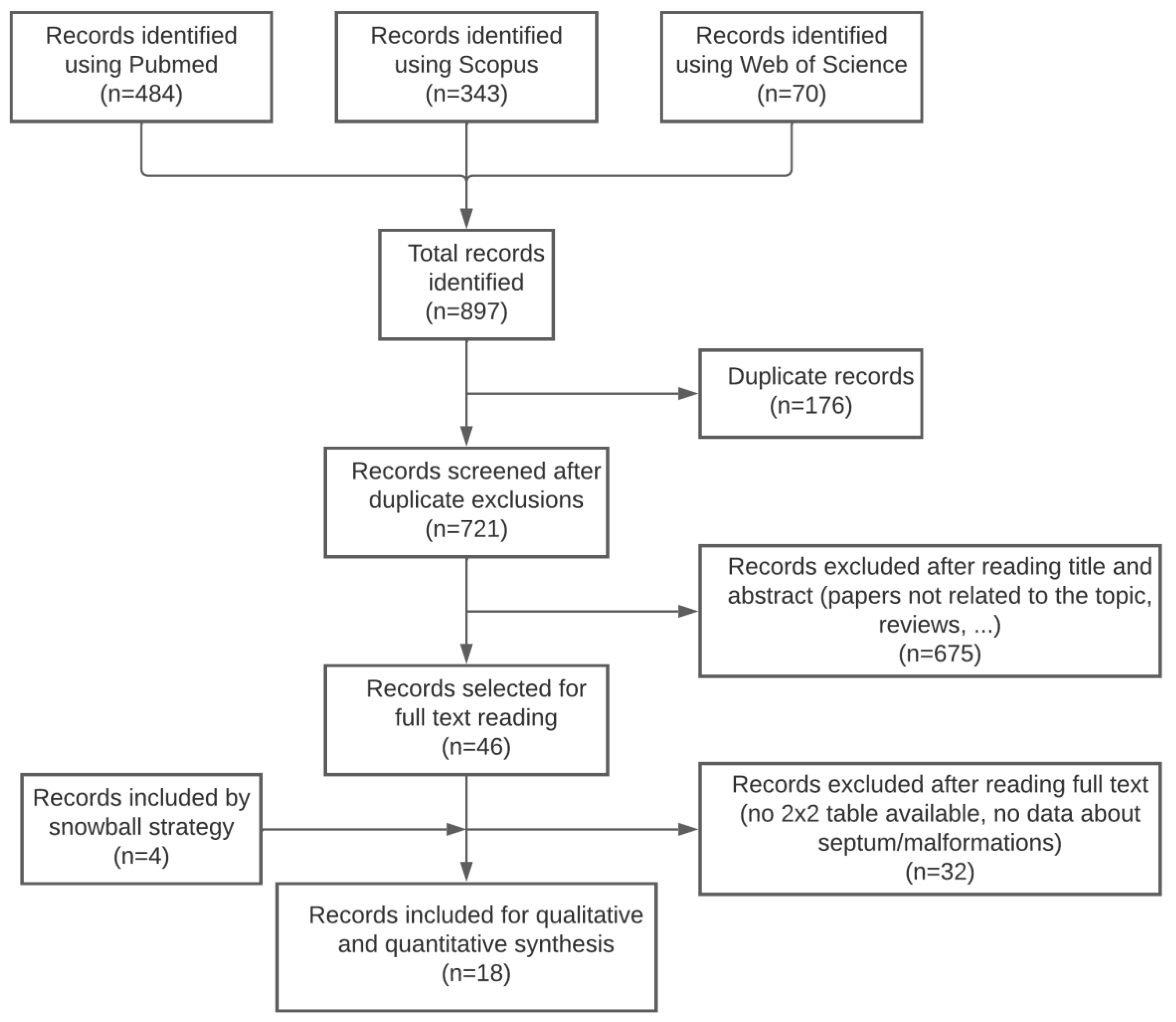
2. Materials and Methods
2.1. Protocol and Registration
2.2. Data Sources and Searches
2.3. Study Selection and Data Collection
- -
- Prospective or retrospective observational cohort studies including women diagnosed with uterine Müllerian anomalies using any of the following methods as index tests: 2D transvaginal ultrasound, 2D sonohysterography, 3D transvaginal ultrasound, or 3D sonohysterography.
- -
- Data reported that allows for the construction of a 2 × 2 table to estimate true positive, true negative, false positive, and false negative cases for any of the index tests assessed.
- -
- Hysteroscopy, with or without combined laparoscopy, as the reference standard
- -
- The exclusion criteria were:
- -
- Studies not related to the topic
- -
- Articles not reporting specific data regarding the septate uterus (complete or partial)
- -
- Letters to the editor, commentaries, narrative reviews, consensus documents, and any other study that does not provide enough data to construct a 2 × 2 table
- -
- Hysteroscopy with or without combined laparoscopy is not used as the gold standard for the diagnosis of uterine Müllerian anomalies.
2.4. Risk of Bias in Individual Studies
2.5. Statistical Analysis
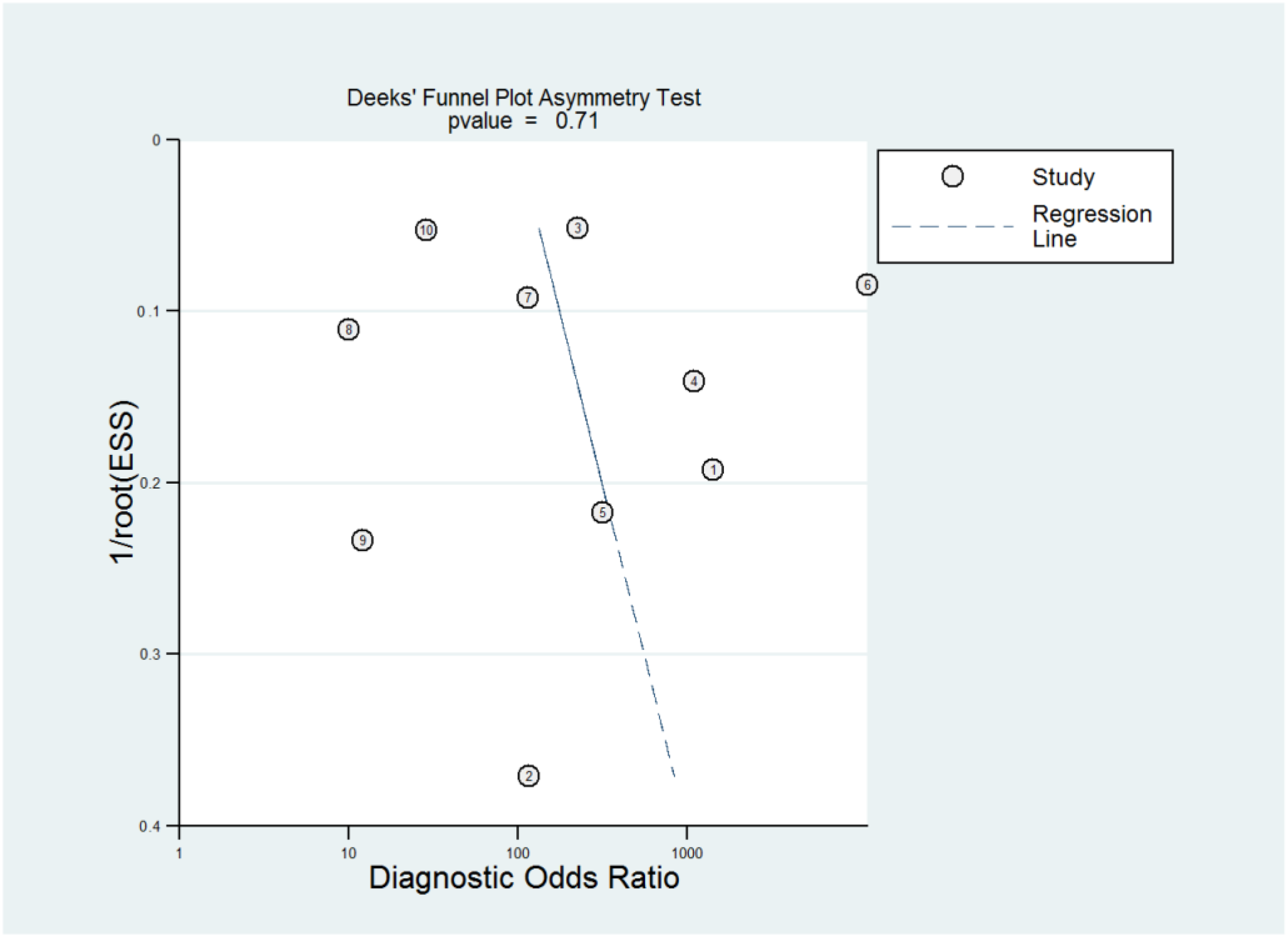
3. Results
3.1. Search Results
3.2. Characteristics of Included Studies
3.3. Methodological Quality of Included Studies
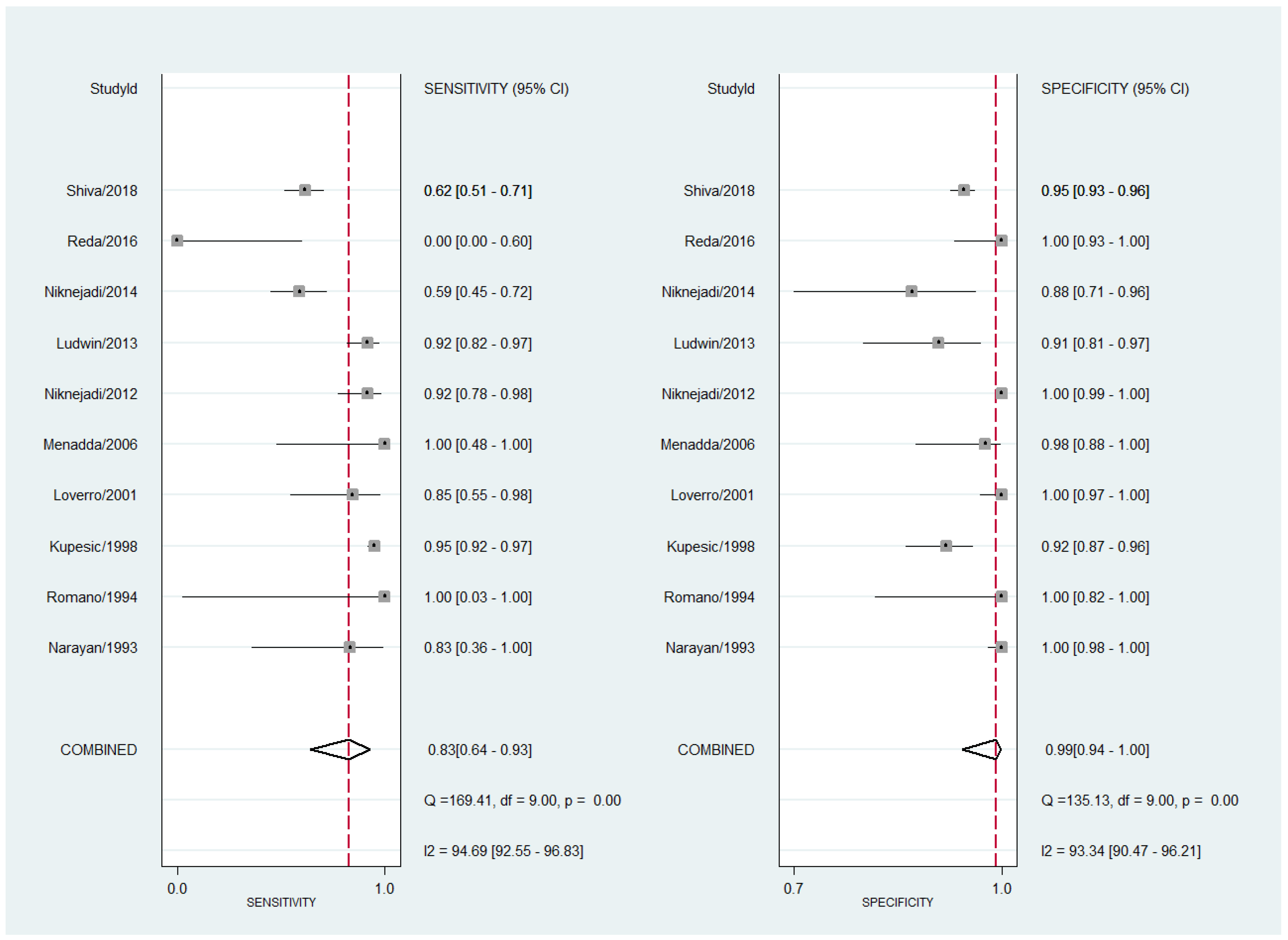
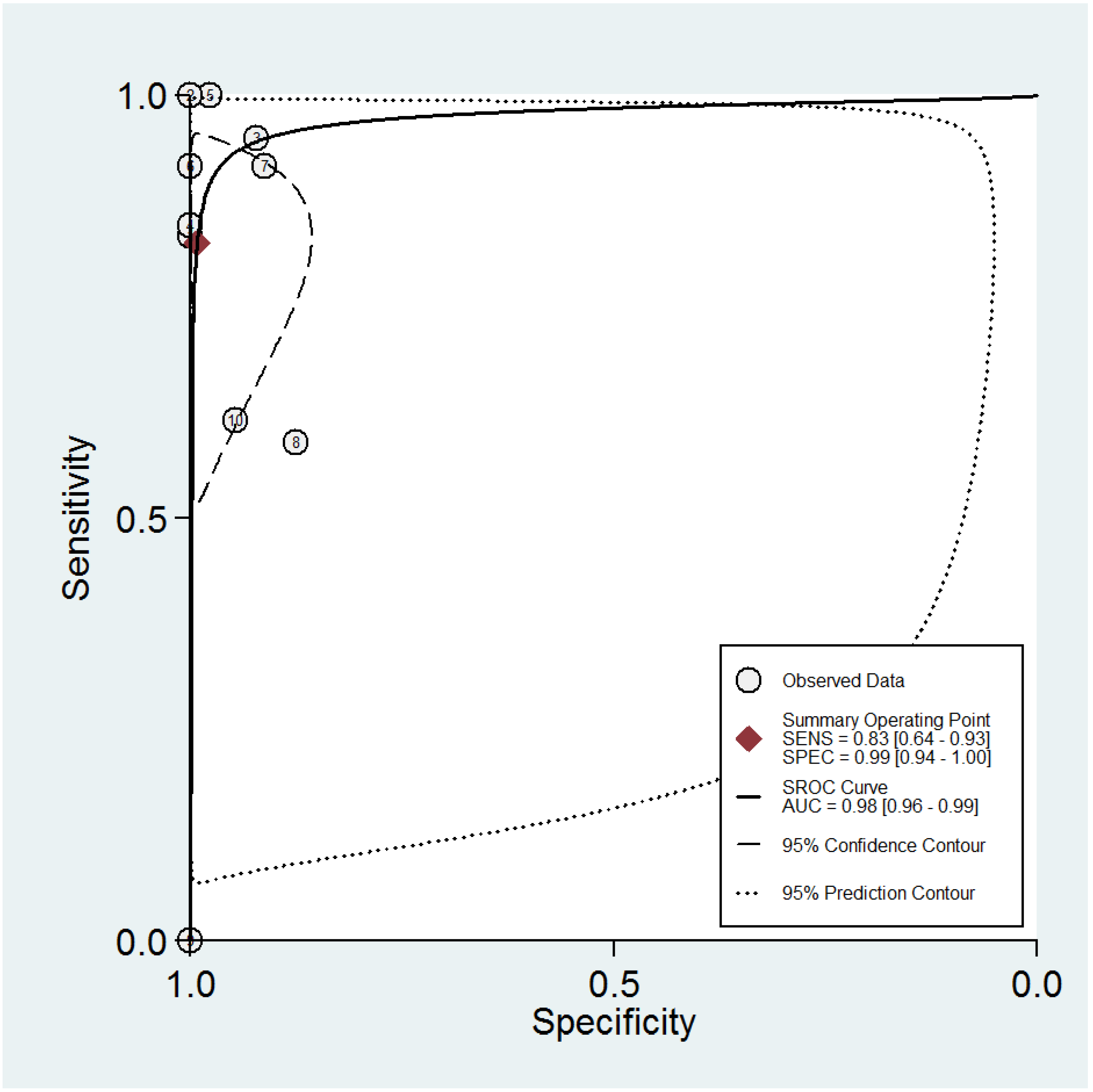
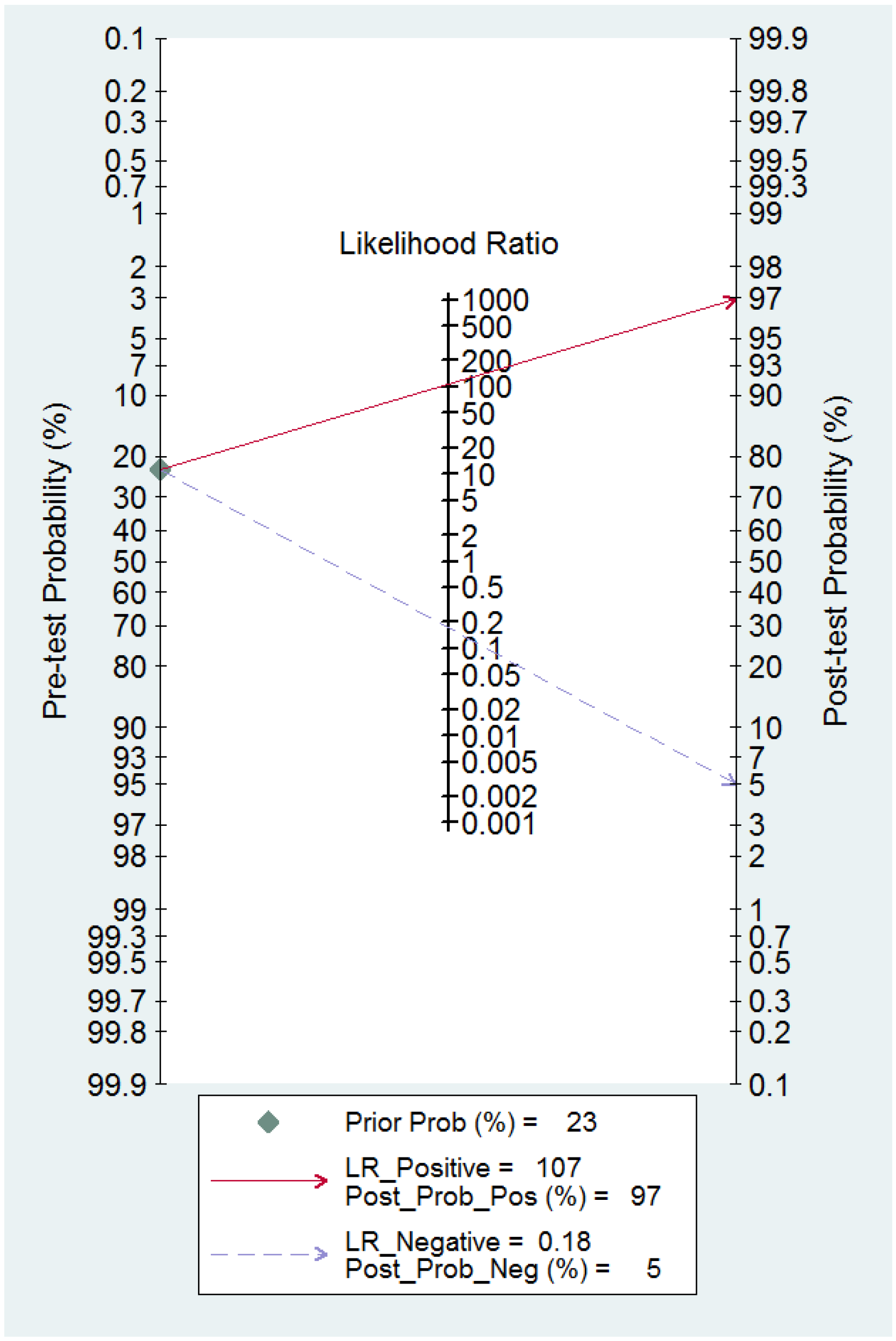
3.4. Diagnostic Performance of 2D TVS and 2D SIS for Uterine Septum Detection
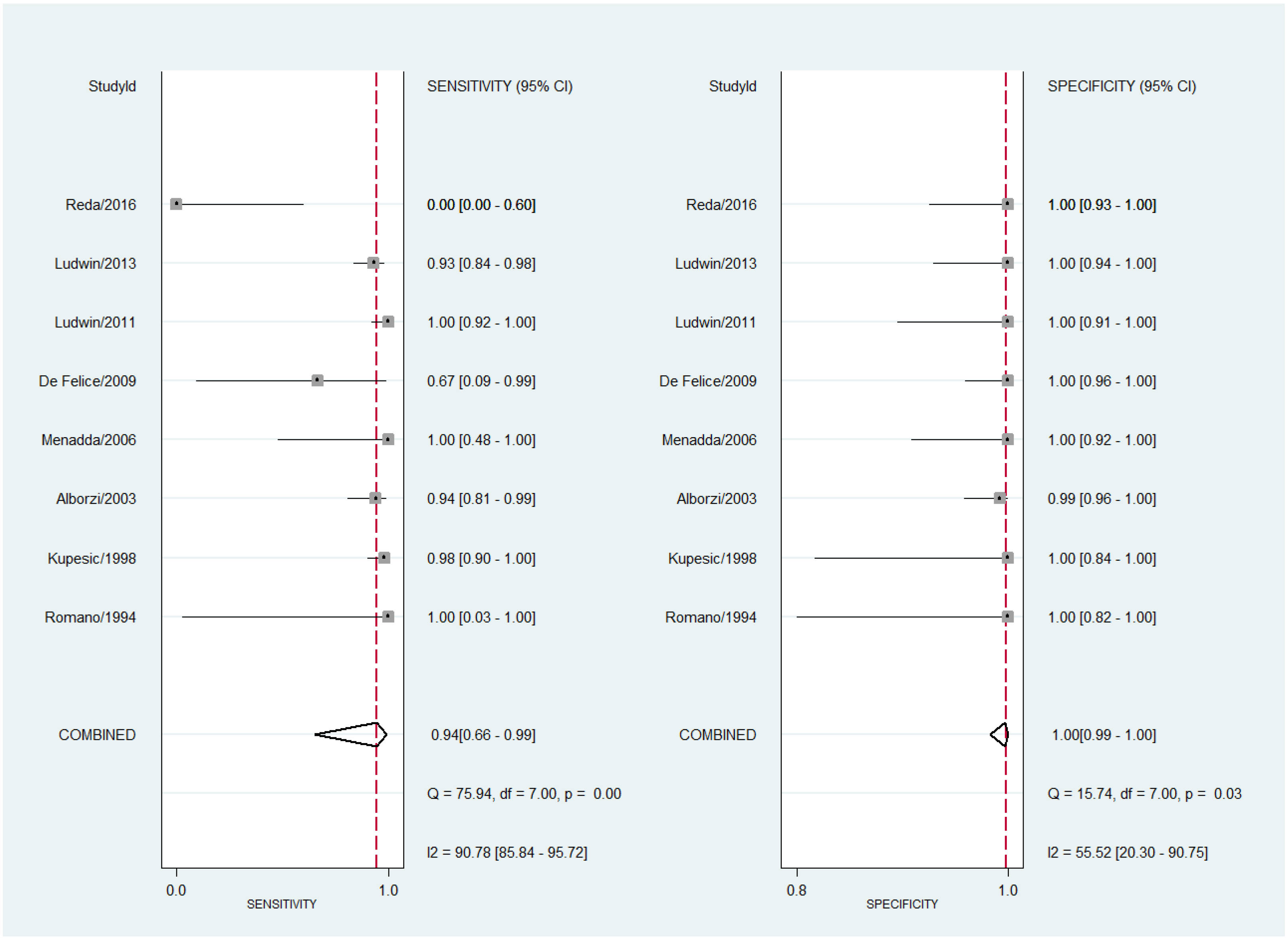
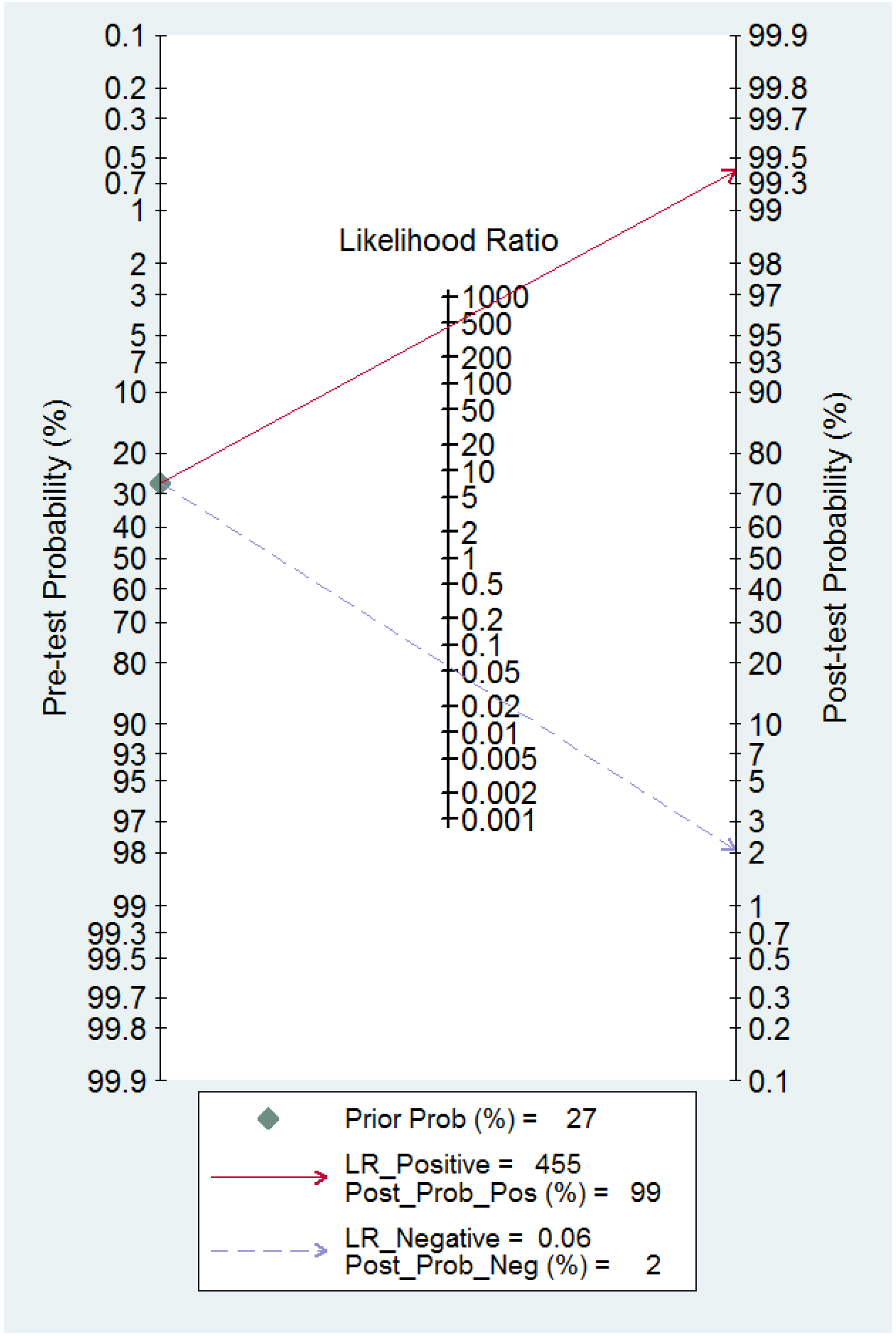
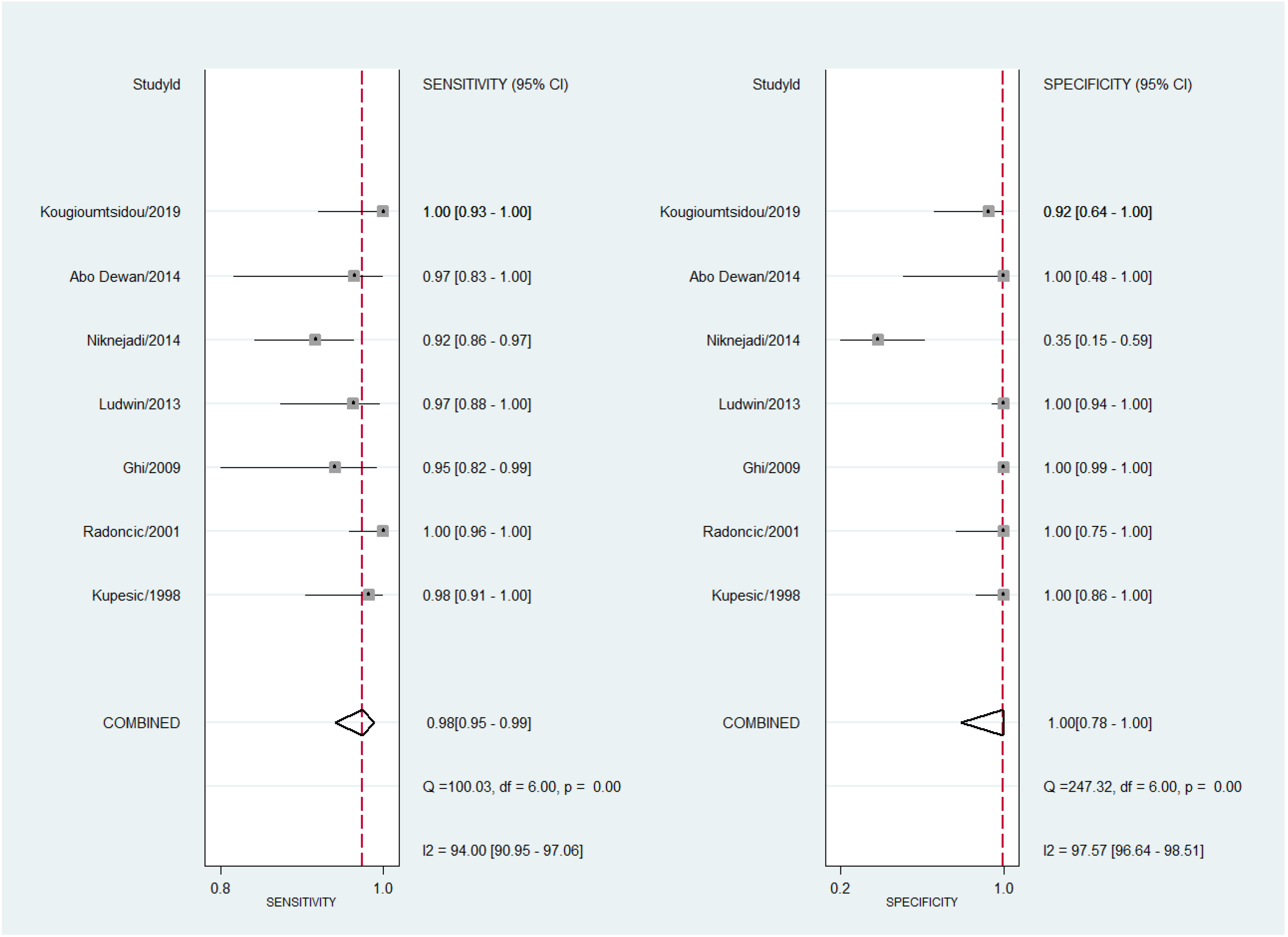
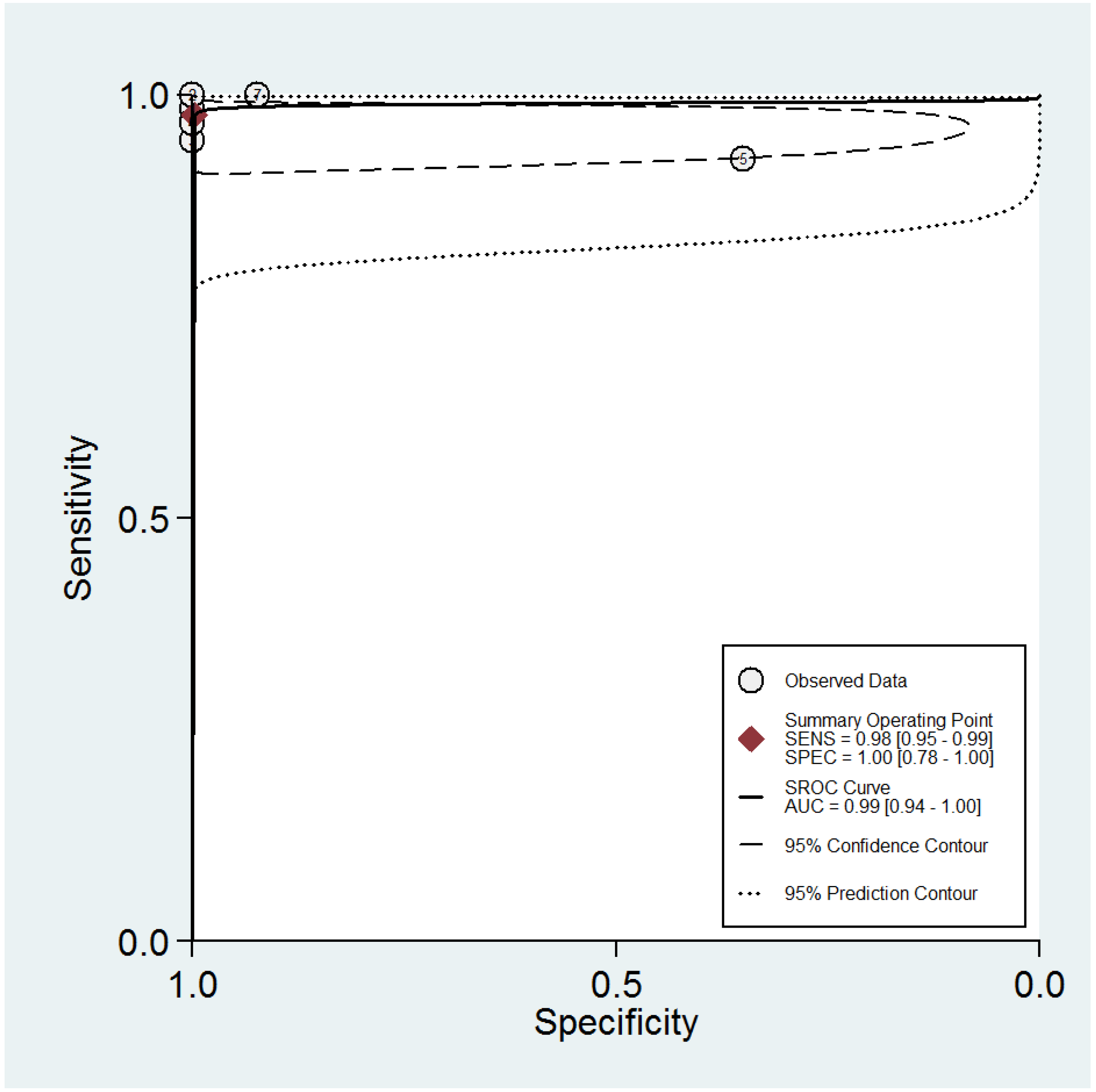
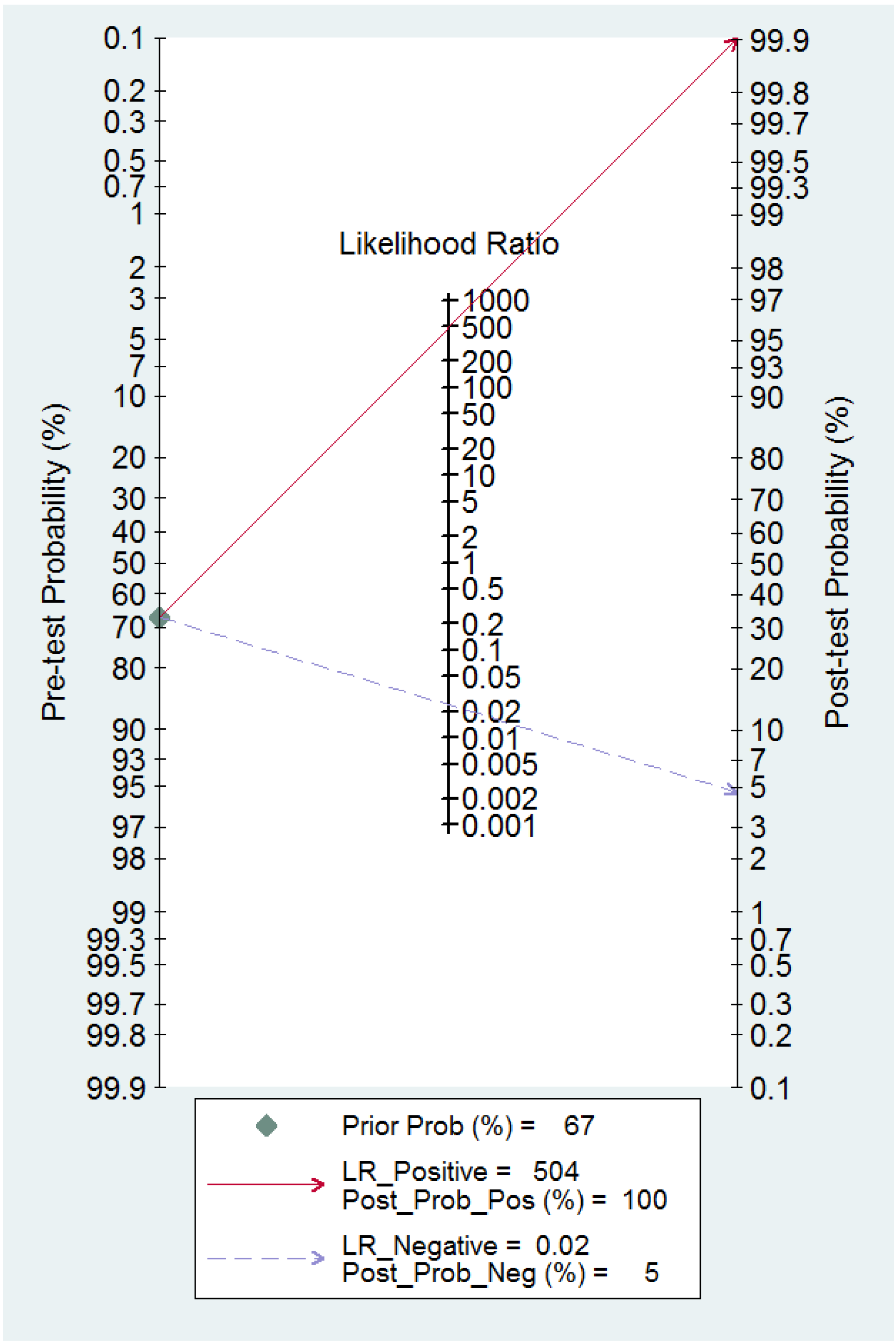
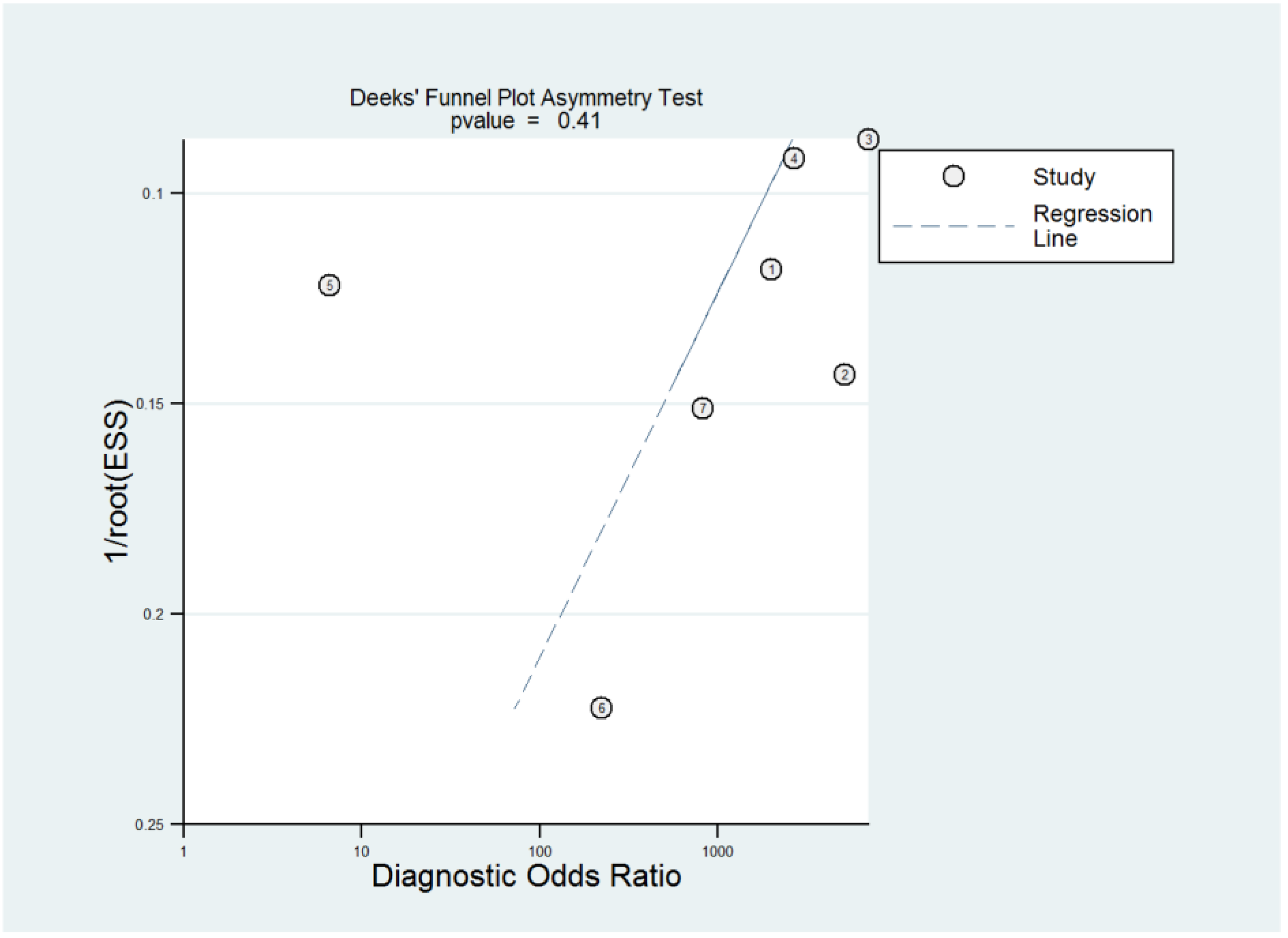
3.5. Diagnostic Performance of 3D TVS and 3D SIS for Uterine Septum Detection
4. Discussion
4.1. Summary of Evidence
4.2. Limitations and Strengths
4.3. Interpretation of Results
4.4. Future Research Agenda
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grimbizis, G.F.; Campo, R. Congenital Malformations of the Female Genital Tract: The Need for a New Classification System. Fertil. Steril. 2010, 94, 401–407. [Google Scholar] [CrossRef]
- Saravelos, S.H.; Cocksedge, K.A.; Li, T.C. Prevalence and Diagnosis of Congenital Uterine Anomalies in Women with Reproductive Failure: A Critical Appraisal. Hum. Reprod. Update 2008, 14, 415–429. [Google Scholar] [CrossRef] [Green Version]
- Chan, Y.Y.; Jayaprakasan, K.; Zamora, J.; Thornton, J.G.; Raine-Fenning, N.; Coomarasamy, A. The Prevalence of Congenital Uterine Anomalies in Unselected and High-Risk Populations: A Systematic Review. Hum. Reprod. Update 2011, 17, 761–771. [Google Scholar] [CrossRef] [Green Version]
- Grimbizis, G.F.; Camus, M.; Tarlatzis, B.C.; Bontis, J.N.; Devroey, P. Clinical Implications of Uterine Malformations and Hysteroscopic Treatment Results. Hum. Reprod. Update 2001, 7, 161–174. [Google Scholar] [CrossRef]
- Tomaževič, T.; Ban-Frangež, H.; Ribič-Pucelj, M.; Premru-Sršen, T.; Verdenik, I. Small Uterine Septum Is an Important Risk Variable for Preterm Birth. Eur. J. Obstet Gynecol. Reprod. Biol. 2007, 135, 154–157. [Google Scholar] [CrossRef]
- Rikken, J.F.W.; Leeuwis-Fedorovich, N.E.; Letteboer, S.; Emanuel, M.H.; Limpens, J.; van der Veen, F.; Goddijn, M.; van Wely, M. The Pathophysiology of the Septate Uterus: A Systematic Review. BJOG 2019, 126, 1192–1199. [Google Scholar] [CrossRef]
- Practice Committee of the American Society for Reproductive Medicine. Uterine Septum: A Guideline. Fertil. Steril. 2016, 106, 530–540. [Google Scholar] [CrossRef] [Green Version]
- Grimbizis, G.F.; Gordts, S.; di Spiezio Sardo, A.; Brucker, S.; de Angelis, C.; Gergolet, M.; Li, T.C.; Tanos, V.; Brölmann, H.; Gianaroli, L.; et al. The ESHRE/ESGE Consensus on the Classification of Female Genital Tract Congenital Anomalies. Hum. Reprod. 2013, 28, 2032–2044. [Google Scholar] [CrossRef] [Green Version]
- Homer, H.A.; Li, T.C.; Cooke, I.D. The Septate Uterus: A Review of Management and Reproductive Outcome. Fertil. Steril. 2000, 73, 1–14. [Google Scholar] [CrossRef]
- Valle, R.F.; Ekpo, G.E. Hysteroscopic Metroplasty for the Septate Uterus: Review and Meta-Analysis. J. Minim Invasive Gynecol. 2013, 20, 22–42. [Google Scholar] [CrossRef]
- Rikken, J.F.W.; Kowalik, C.R.; Emanuel, M.H.; Bongers, M.Y.; Spinder, T.; Jansen, F.W.; Mulders, A.G.M.G.J.; Padmehr, R.; Clark, T.J.; van Vliet, H.A.; et al. Septum Resection versus Expectant Management in Women with a Septate Uterus: An International Multicentre Open-Label Randomized Controlled Trial. Hum. Reprod. 2021, 36, 1260–1267. [Google Scholar] [CrossRef]
- Carrera, M.; Pérez Millan, F.; Alcázar, J.L.; Alonso, L.; Caballero, M.; Carugno, J.; Dominguez, J.A.; Moratalla, E. Effect of Hysteroscopic Metroplasty on Reproductive Outcomes in Women with Septate Uterus: Systematic Review and Meta-Analysis. J. Minim Invasive Gynecol. 2022, 29, 465–475. [Google Scholar] [CrossRef]
- Ludwin, A.; Pityński, K.; Ludwin, I.; Banas, T.; Knafel, A. Two- and Three-Dimensional Ultrasonography and Sonohysterography versus Hysteroscopy with Laparoscopy in the Differential Diagnosis of Septate, Bicornuate, and Arcuate Uteri. J. Minim Invasive Gynecol. 2013, 20, 90–99. [Google Scholar] [CrossRef]
- Graupera, B.; Pascual, M.A.; Hereter, L.; Browne, J.L.; Úbeda, B.; Rodríguez, I.; Pedrero, C. Accuracy of Three-Dimensional Ultrasound Compared with Magnetic Resonance Imaging in Diagnosis of Müllerian Duct Anomalies Using ESHRE-ESGE Consensus on the Classification of Congenital Anomalies of the Female Genital Tract. Ultrasound Obstet Gynecol. 2015, 46, 616–622. [Google Scholar] [CrossRef]
- Bermejo, C.; Martínez Ten, P.; Cantarero, R.; Diaz, D.; Pérez Pedregosa, J.; Barrón, E.; Labrador, E.; Ruiz López, L. Three-Dimensional Ultrasound in the Diagnosis of Müllerian Duct Anomalies and Concordance with Magnetic Resonance Imaging. Ultrasound Obstet Gynecol. 2010, 35, 593–601. [Google Scholar] [CrossRef]
- Berger, A.; Batzer, F.; Lev-Toaff, A.; Berry-Roberts, C. Diagnostic Imaging Modalities for Müllerian Anomalies: The Case for a New Gold Standard. J. Minim Invasive Gynecol. 2014, 21, 335–345. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, 105906. [Google Scholar]
- Sotiriadis, A.; Papatheodorou, S.I.; Martins, W.P. Synthesizing Evidence from Diagnostic Accuracy TEsts: The SEDATE Guideline. Ultrasound Obstet Gynecol. 2016, 47, 386–395. [Google Scholar] [CrossRef] [Green Version]
- Whiting, P.F.; Rutjes, A.W.S.; Westwood, M.E.; Mallett, S.; Deeks, J.J.; Reitsma, J.B.; Leeflang, M.M.G.; Sterne, J.A.C.; Bossuyt, P.M.M. QUADAS-2: A Revised Tool for the Quality Assessment of Diagnostic Accuracy Studies. Ann. Intern. Med. 2011, 155, 529–536. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring Inconsistency in Meta-Analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [Green Version]
- Deeks, J.J.; Macaskill, P.; Irwig, L. The Performance of Tests of Publication Bias and Other Sample Size Effects in Systematic Reviews of Diagnostic Test Accuracy Was Assessed. J. Clin. Epidemiol. 2005, 58, 882–893. [Google Scholar] [CrossRef]
- Narayan, R.; Goswamy, R.K. Transvaginal Sonography of the Uterine Cavity with Hysteroscopic Correlation in the Investigation of Infertility. Ultrasound Obstet Gynecol. 1993, 3, 129–133. [Google Scholar] [CrossRef]
- Romano, F.; Cicinelli, E.; Anastasio, P.S.; Epifani, S.; Fanelli, F.; Galantino, P. Sonohysterography versus Hysteroscopy for Diagnosing Endouterine Abnormalities in Fertile Women. Int. J. Gynecol. Obstet. 1994, 45, 253–260. [Google Scholar] [CrossRef]
- Kupesic, S.; Kurjak, A. Septate Uterus: Detection and Prediction of Obstetrical Complications by Different Forms of Ultrasonography. J. Ultrasound Med. 1998, 17, 631–636. [Google Scholar] [CrossRef]
- Radoncic, E.; Funduk-Kurjak, B. Three-Dimensional Ultrasound for Routine Check-Up in In Vitro Fertilization Patients. Croat Med. J. 2000, 41, 262–265. [Google Scholar]
- Loverro, G.; Nappi, L.; Vicino, M.; Carriero, C.; Vimercati, A.; Selvaggi, L. Uterine Cavity Assessment in Infertile Women: Comparison of Transvaginal Sonography and Hysteroscopy. Eur. J. Obstet. Gynecol. Reprod. Biol. 2001, 100, 67–71. [Google Scholar] [CrossRef]
- Alborzi, S.; Dehbashi, S.; Khodaee, R. Sonohysterosalpingographic Screening for Infertile Patients. Int. J. Gynecol. Obstet. 2003, 82, 57–62. [Google Scholar] [CrossRef]
- Menada Valenzano, M.; Mistrangelo, E.; Lijoi, D.; Fortunato, T.; Lantieri, P.B.; Risso, D.; Costantini, S.; Ragni, N. Transvaginal Sonohysterographic Evaluation of Uterine Malformations. Eur. J. Obstet. Gynecol. Reprod. Biol. 2006, 124, 246–249. [Google Scholar] [CrossRef]
- de Feuce, C.; Porfiri, L.M.; Savelli, S.; Alfano, G.; Pace, S.; Manganaro, L.; Vesteri, A.R.; Drudi, F.M. Infertility in Women: Combined Sonohysterography and Hysterosalpingography in the Evaluation of the Uterine Cavity. Ultraschall der Med. 2009, 30, 52–57. [Google Scholar] [CrossRef]
- Ghi, T.; Casadio, P.; Kuleva, M.; Perrone, A.M.; Savelli, L.; Giunchi, S.; Meriggiola, M.C.; Gubbini, G.; Pilu, G.; Pelusi, C.; et al. Accuracy of Three-Dimensional Ultrasound in Diagnosis and Classification of Congenital Uterine Anomalies. Fertil. Steril. 2009, 92, 808–813. [Google Scholar] [CrossRef]
- Ludwin, A.; Ludwin, I.; Banas, T.; Knafel, A.; Miedzyblocki, M.; Basta, A. Diagnostic Accuracy of Sonohysterography, Hysterosalpingography and Diagnostic Hysteroscopy in Diagnosis of Arcuate, Septate and Bicornuate Uterus. J. Obstet. Gynaecol. Res. 2011, 37, 178–186. [Google Scholar] [CrossRef]
- Niknejadi, M.; Haghighi, H.; Ahmadi, F.; Niknejad, F.; Chehrazi, M.; Vosough, A.; Moenian, D. Diagnostic Accuracy of Transvaginal Sonography in the Detection of Uterine Abnormalities in Infertile Women. Iran. J. Radiol. 2012, 9, 139–144. [Google Scholar] [CrossRef]
- Ahmadi, F.; Rashidy, Z.; Sc, B.; Haghighi, H.; Akhoond, M.; Niknejadi, M.; Hemat, M.; Candidate, P.D. Uterine Cavity Assessment in Infertile Women: Sensitivity and Specificity of Three-Dimensional Hysterosonography versus Hysteroscopy. Iran. J. Reprod. Med. 2013, 11, 977. [Google Scholar]
- Niknejadi, M.; Akhbari, F.; Niknejad, F.; Khalili, G.; Shiva, M. Comparison of Two Dimensional and Live Three Dimensional Ultrasounds for the Diagnosis of Septated Uterus. Iran J. Reprod. Med. 2014, 12, 547–554. [Google Scholar]
- Abo Dewan, K.A.A.; Hefeda, M.M.; Elkholy, D.G.E. Septate or Bicornuate Uterus: Accuracy of Three-Dimensional Trans-Vaginal Ultrasonography and Pelvic Magnetic Resonance Imaging. Egypt. J. Radiol. Nucl. Med. 2014, 45, 987–995. [Google Scholar] [CrossRef] [Green Version]
- Reda, A.; Hamid, A.S.A.; Mostafa, R.; Refaei, E. Comparison between Findings of Saline Infusion Sonohysterography and Office Hysteroscopy in Patients with Recurrent Implantation Failure. J. Hum. Reprod. Sci. 2016, 9, 236–240. [Google Scholar] [CrossRef]
- Shiva, M.; Ahmadi, F.; Arabipoor, A.; Oromiehchi, M.; Chehrazi, M. Accuracy of Two-Dimensional Transvaginal Sonography and Office Hysteroscopy for Detection of Uterine Abnormalities in Patients with Repeated Implantation Failures or Recurrent Pregnancy Loss. Int. J. Fertil. Steril. 2018, 11, 287–292. [Google Scholar]
- Kougioumtsidou, A.; Mikos, T.; Grimbizis, G.F.; Karavida, A.; Theodoridis, T.D.; Sotiriadis, A.; Tarlatzis, B.C.; Athanasiadis, A.P. Three-Dimensional Ultrasound in the Diagnosis and the Classification of Congenital Uterine Anomalies Using the ESHRE/ESGE Classification: A Diagnostic Accuracy Study. Arch. Gynecol. Obstet. 2019, 299, 779–789. [Google Scholar] [CrossRef]
- la Sala, G.B.; Blasi, I.; Gallinelli, A.; Debbi, C.; Lopopolo, G.; Vinci, V.; Villani, M.T.; Iannotti, F. Diagnostic Accuracy of Sonohysterography and Transvaginal Sonography as Compared with Hysteroscopy and Endometrial Biopsy: A Prospective Study. Minerva Ginecol. 2011, 63, 421–427. [Google Scholar]
- Ludwin, A.; Martins, W.P.; Nastri, C.O.; Ludwin, I.; Coelho Neto, M.A.; Leitão, V.M.; Acién, M.; Alcazar, J.L.; Benacerraf, B.; Condous, G.; et al. Congenital Uterine Malformation by Experts (CUME): Better Criteria for Distinguishing between Normal/Arcuate and Septate Uterus? Ultrasound Obstet. Gynecol. 2018, 51, 101–109. [Google Scholar] [CrossRef]
- Knez, J.; Saridogan, E.; van den Bosch, T.; Mavrelos, D.; Ambler, G.; Jurkovic, D. ESHRE/ESGE Female Genital Tract Anomalies Classification System-the Potential Impact of Discarding Arcuate Uterus on Clinical Practice. Hum. Reprod. 2018, 33, 600–606. [Google Scholar] [CrossRef]
- Ludwin, A.; Ludwin, I. Comparison of the ESHRE-ESGE and ASRM Classifications of Müllerian Duct Anomalies in Everyday Practice. Hum. Reprod. 2015, 30, 569–580. [Google Scholar] [CrossRef]
- di Spiezio Sardo, A.; Campo, R.; Gordts, S.; Spinelli, M.; Cosimato, C.; Tanos, V.; Brucker, S.; Li, T.C.; Gergolet, M.; de Angelis, C.; et al. The Comprehensiveness of the ESHRE/ESGE Classification of Female Genital Tract Congenital Anomalies: A Systematic Review of Cases Not Classified by the AFS System. Hum. Reprod. 2015, 30, 1046–1058. [Google Scholar] [CrossRef] [Green Version]


| Author | Year | Country | Study Design | Index Test | Reference Test | Uterine Septum Definition | Examiner Blinded |
|---|---|---|---|---|---|---|---|
| Narayan | 1993 | UK | NA | 2D TVS | HSC | Authors’ own definition | NA |
| Romano | 1994 | Italy | Retrospective | 2D TVS, 2D SIS | HSC | Own definition | Yes |
| Kupesic | 1998 | Croatia | NA | 2D TVS, 2D SIS, 3D TVS | HSC + LPS | ASRM | NA |
| Radoncić | 2000 | Croatia | NA | 3D TVS | HSC | NA | NA |
| Loverro | 2001 | Italy | NA | 2D TVS | HSC | NA | NA |
| Alborzi | 2003 | Iran | Prospective | 2D SIS | HSC + LPS | Own definition | Yes |
| Menada | 2006 | Italy | Retrospective | 2D TVS, 2D SIS | HSC +/− LPS | Own definition | NA |
| De Feuce | 2009 | Italy | NA | 2D SIS | HSC +/− LPS | NA | NA |
| Ghi | 2009 | Italy | Prospective | 3D TVS | HSC +/− LPS | ASRM | Yes |
| Ludwin | 2011 | Poland | Prospective | 2D SIS | HSC + LPS | Own definition | Yes |
| Niknejadi | 2012 | Iran | Cross-sectional | 2D TVS | HSC | ASRM | Yes |
| Ludwin | 2013 | Poland | Prospective | 2D TVS, 2D SIS, 3D TVS, 3D SIS | HSC + LPS | ASRM | Yes |
| Ahmadi | 2013 | Iran | Cross sectional | 3D SIS | HSC | ASRM | NA |
| Niknejadi | 2014 | Iran | Retrospective | 2D TVS, 3D TVS | HSC | ASRM | NA |
| Abo Dewan | 2014 | Egypt | Retrospective | 3D TVS | HSC | ASRM | NA |
| Reda | 2016 | Egypt | Prospective | 2D TVS, 2D SIS | HSC | NA | Yes |
| Shiva | 2018 | Iran | Prospective | 2D TVS | HSC | Own definition | Yes |
| Kougioumtsidou | 2019 | Greece | Prospective | 3D TVS | HSC + LPS | ESHRE-ESGE | Yes |
| Study | Year | Risk of Bias | Concerns about Applicability | |||||
|---|---|---|---|---|---|---|---|---|
| Patient Selection | Index Test | Reference Standard | Flow and Timing | Patient Selection | Index Test | Reference Standard | ||
| Narayan | 1993 | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Romano | 1994 | High risk | High risk | Low risk | Low risk | High risk | Low risk | Low risk |
| Kupesic | 1998 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Radoncić | 2000 | High risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Loverro | 2001 | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Alborzi | 2003 | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Menada | 2006 | High risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk |
| De Feuce | 2009 | Low risk | Unclear risk | Low risk | Unclear risk | Low risk | Low risk | Low risk |
| Ghi | 2009 | High risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Ludwin | 2011 | High risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk |
| Niknejadi | 2012 | High risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Ludwin | 2013 | High risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk |
| Ahmadi | 2013 | High risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Niknejadi | 2014 | High risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Abo Dewan | 2014 | High risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk |
| Reda | 2016 | High risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Shiva | 2018 | High risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Kougioumtsidou | 2019 | High risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alcázar, J.L.; Carriles, I.; Cajas, M.B.; Costa, S.; Fabra, S.; Cabrero, M.; Castro, E.; Tomaizeh, A.; Laza, M.V.; Monroy, A.; et al. Diagnostic Performance of Two-Dimensional Ultrasound, Two-Dimensional Sonohysterography and Three-Dimensional Ultrasound in the Diagnosis of Septate Uterus—A Systematic Review and Meta-Analysis. Diagnostics 2023, 13, 807. https://doi.org/10.3390/diagnostics13040807
Alcázar JL, Carriles I, Cajas MB, Costa S, Fabra S, Cabrero M, Castro E, Tomaizeh A, Laza MV, Monroy A, et al. Diagnostic Performance of Two-Dimensional Ultrasound, Two-Dimensional Sonohysterography and Three-Dimensional Ultrasound in the Diagnosis of Septate Uterus—A Systematic Review and Meta-Analysis. Diagnostics. 2023; 13(4):807. https://doi.org/10.3390/diagnostics13040807
Chicago/Turabian StyleAlcázar, Juan Luis, Isabel Carriles, María Belén Cajas, Susana Costa, Sofia Fabra, Maria Cabrero, Elena Castro, Aida Tomaizeh, María Victoria Laza, Alba Monroy, and et al. 2023. "Diagnostic Performance of Two-Dimensional Ultrasound, Two-Dimensional Sonohysterography and Three-Dimensional Ultrasound in the Diagnosis of Septate Uterus—A Systematic Review and Meta-Analysis" Diagnostics 13, no. 4: 807. https://doi.org/10.3390/diagnostics13040807
APA StyleAlcázar, J. L., Carriles, I., Cajas, M. B., Costa, S., Fabra, S., Cabrero, M., Castro, E., Tomaizeh, A., Laza, M. V., Monroy, A., Martinez, I., Aguilar, M. I., Hernani, E., Castellet, C., Oliva, A., Pascual, M. Á., & Guerriero, S. (2023). Diagnostic Performance of Two-Dimensional Ultrasound, Two-Dimensional Sonohysterography and Three-Dimensional Ultrasound in the Diagnosis of Septate Uterus—A Systematic Review and Meta-Analysis. Diagnostics, 13(4), 807. https://doi.org/10.3390/diagnostics13040807






