Cardiometabolic Phenotyping in Heart Failure: Differences between Patients with Reduced vs. Preserved Ejection Fraction
Abstract
1. Introduction
2. Methods
2.1. Study Population
2.2. Laboratory Analyses
2.3. Baseline Pulmonary Echography
2.4. Baseline Echocardiography
2.5. Statistical Analysis
3. Results
3.1. Study Population
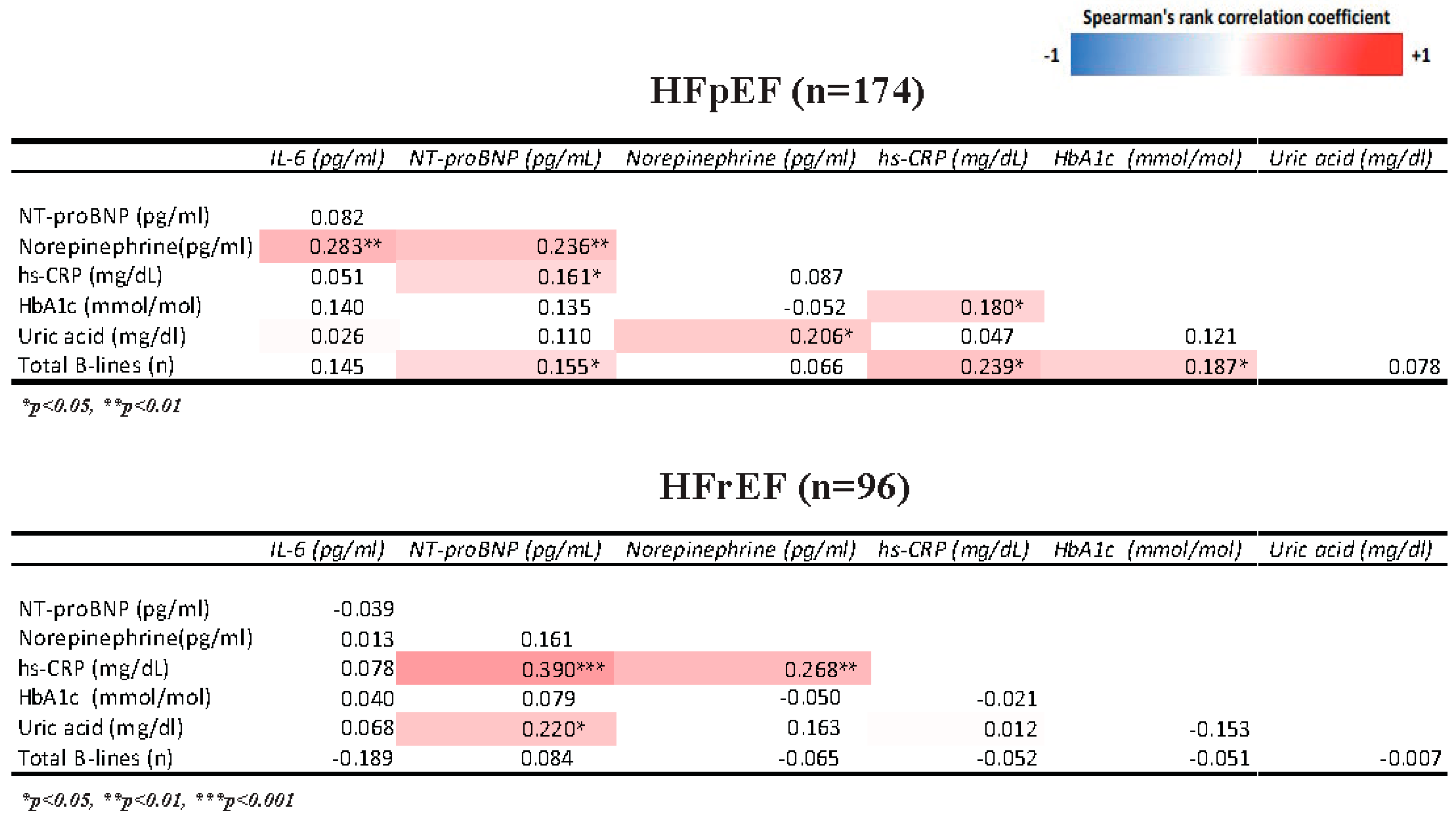
3.2. Association of Cardiometabolic Profile with Inflammation and Congestion Indices (Figure 1)
3.3. Association of Cardiometabolic Profile with Diastolic Function and Right Ventriculo-Arterial Coupling
4. Discussion
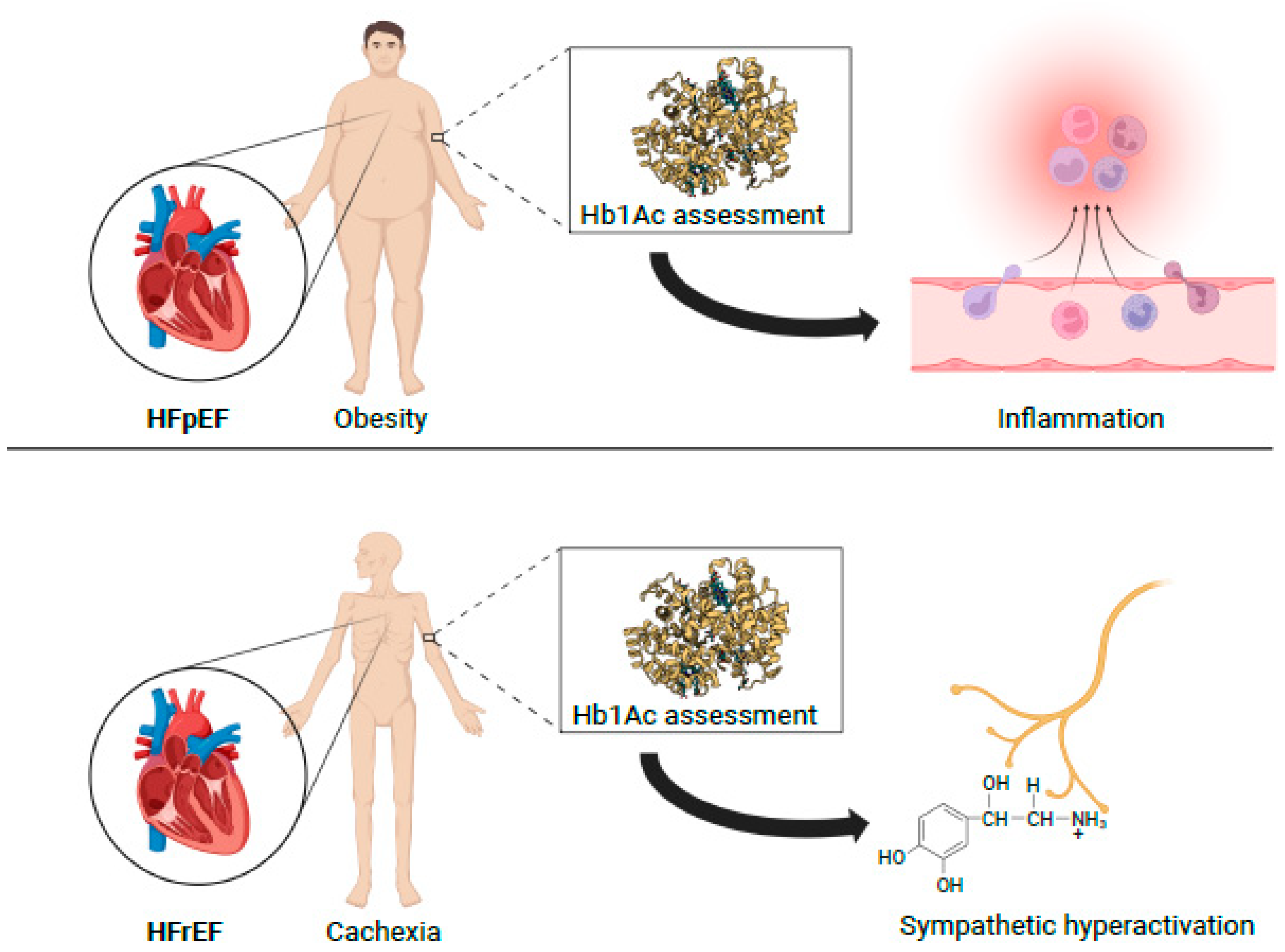
4.1. Correlation of Cardiometabolism with Inflammation and Congestion
4.2. Correlation of Inflammation with Congestion and Adrenergic Activation
4.3. Correlation of Cardiometabolism with Diastolic Dysfunction and Right Ventricular Arterial Coupling
4.4. Clinical Perspectives
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Soto, M.E.; Pérez-Torres, I.; Rubio-Ruiz, M.E.; Manzano-Pech, L.; Guarner-Lans, V. Interconnection between Cardiac Cachexia and Heart Failure—Protective Role of Cardiac Obesity. Cells 2022, 11, 1039. [Google Scholar] [CrossRef]
- Murphy, S.P.; Ibrahim, N.E.; Januzzi, J.L. Heart Failure with Reduced Ejection Fraction: A Review. J. Am. Med. Assoc. 2020, 324, 488–504. [Google Scholar] [CrossRef] [PubMed]
- Hennessy, M. The obesity paradox. Cardiol. Rev. 2012, 28, 55–61. [Google Scholar] [CrossRef]
- Nagarajan, V.; Kohan, L.; Holland, E.; Keeley, E.C.; Mazimba, S. Obesity paradox in heart failure: A heavy matter. ESC Hear. Fail. 2016, 3, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Kistorp, C.; Faber, J.; Galatius, S.; Gustafsson, F.; Frystyk, J.; Flyvbjerg, A.; Hildebrandt, P. Plasma adiponectin, body mass index, and mortality in patients with chronic heart failure. Circulation 2005, 112, 1756–1762. [Google Scholar] [CrossRef] [PubMed]
- Nesti, L.; Pugliese, N.R.; Sciuto, P.; De Biase, N.; Mazzola, M.; Fabiani, I.; Trico, D.; Masi, S.; Natali, A. Mechanisms of reduced peak oxygen consumption in subjects with uncomplicated type 2 diabetes. Cardiovasc. Diabetol. 2021, 20, 124. [Google Scholar] [CrossRef]
- Nesti, L.; Pugliese, N.R.; Sciuto, P.; Natali, A. Type 2 diabetes and reduced exercise tolerance: A review of the literature through an integrated physiology approach. Cardiovasc. Diabetol. 2020, 19, 134. [Google Scholar] [CrossRef]
- Pugliese, N.R.; Pieroni, A.; De Biase, N.; Di Fiore, V.; Nesti, L.; Agostoni, P.; Dini, F.L. Impact of diabetes on cardiopulmonary function: The added value of a combined cardiopulmonary and echocardiography stress test. Heart Fail. Rev. 2021. [Google Scholar] [CrossRef]
- Di Pino, A.; Mangiafico, S.; Urbano, F.; Scicali, R.; Scandura, S.; D’Agate, V.; Piro, S.; Tamburino, C.; Purrello, F.; Rabuazzo, A.M. HbA1c identifies subjects with prediabetes and subclinical left ventricular diastolic dysfunction. J. Clin. Endocrinol. Metab. 2017, 102, 3756–3764. [Google Scholar] [CrossRef]
- Liu, S.; Hempe, J.M.; McCarter, R.J.; Li, S.; Fonseca, V.A. Association between inflammation and biological variation in hemoglobin A1c in U.S. nondiabetic adults. J. Clin. Endocrinol. Metab. 2015, 100, 2364–2371. [Google Scholar] [CrossRef]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Celutkiene, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef]
- Pugliese, N.R.; Paneni, F.; Mazzola, M.; De Biase, N.; Del Punta, L.; Gargani, L.; Mengozzi, A.; Virdis, A.; Nesti, L.; Taddei, S.; et al. Impact of epicardial adipose tissue on cardiovascular haemodynamics, metabolic profile, and prognosis in heart failure. Eur. J. Heart Fail. 2021, 23, 1858–1871. [Google Scholar] [CrossRef] [PubMed]
- Pugliese, N.R.; De Biase, N.; Conte, L.; Gargani, L.; Mazzola, M.; Fabiani, I.; Natali, A.; Dini, F.L.; Frumento, P.; Rosada, J.; et al. Cardiac Reserve and Exercise Capacity: Insights from Combined Cardiopulmonary and Exercise Echocardiography Stress Testing. J. Am. Soc. Echocardiogr. 2021, 34, 38–50. [Google Scholar] [CrossRef] [PubMed]
- Pugliese, N.R.; Pellicori, P.; Filidei, F.; De Biase, N.; Maffia, P.; Guzik, T.J.; Masi, S.; Taddei, S.; Cleland, J.G. Inflammatory pathways in heart failure with preserved left ventricular ejection fraction: Implications for future interventions. Cardiovasc. Res. 2022, 118, 3536–3555. [Google Scholar] [CrossRef] [PubMed]
- Pugliese, N.R.; Masi, S.; Taddei, S. The renin-angiotensin-aldosterone system: A crossroad from arterial hypertension to heart failure. Heart Fail. Rev. 2020, 25, 31–42. [Google Scholar] [CrossRef] [PubMed]
- Simmonds, S.J.; Cuijpers, I.; Heymans, S.; Jones, E.A.V. Cellular and Molecular Differences between HFpEF and HFrEF: A Step Ahead in an Improved Pathological Understanding. Cells 2020, 9, 242. [Google Scholar] [CrossRef]
- Stanley, W.C.; Recchia, F.A.; Lopaschuk, G.D. Myocardial substrate metabolism in the normal and failing heart. Physiol. Rev. 2005, 85, 1093–1129. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.V.; Li, D.L.; Hill, J.A. Heart failure and loss of metabolic control. J. Cardiovasc. Pharmacol. 2014, 63, 302–313. [Google Scholar] [CrossRef]
- Aubert, G.; Martin, O.J.; Horton, J.L.; Lai, L.; Vega, R.B.; Leone, T.C.; Koves, T.; Gardell, S.J.; Krüger, M.; Hoppel, C.L.; et al. The Failing Heart Relies on Ketone Bodies as a Fuel. Circulation 2016, 133, 698–705. [Google Scholar] [CrossRef]
- Voros, G.; Ector, J.; Garweg, C.; Droogne, W.; Van Cleemput, J.; Peersman, N.; Vermeersch, P.; Janssens, S. Increased Cardiac Uptake of Ketone Bodies and Free Fatty Acids in Human Heart Failure and Hypertrophic Left Ventricular Remodeling. Circ. Heart Fail. 2018, 11, e004953. [Google Scholar] [CrossRef]
- Ramchandra, R.; Hood, S.G.; Xing, D.; Lambert, G.W.; May, C.N. Mechanisms underlying the increased cardiac norepinephrine spillover in heart failure. Am. J. Physiol.-Hear. Circ. Physiol. 2018, 315, H340–H347. [Google Scholar] [CrossRef] [PubMed]
- Yuan, T.; Yang, T.; Chen, H.; Fu, D.; Hu, Y.; Wang, J.; Yuan, Q.; Yu, H.; Xu, W.; Xie, X. New insights into oxidative stress and inflammation during diabetes mellitus-accelerated atherosclerosis. Redox Biol. 2019, 20, 247–260. [Google Scholar] [CrossRef] [PubMed]
- Clark, K.A.A.; Velazquez, E.J. Heart Failure with Preserved Ejection Fraction: Time for a Reset. J. Am. Med. Assoc. 2020, 324, 1506–1508. [Google Scholar] [CrossRef]
- Cappola, T.P.; Kass, D.A.; Nelson, G.S.; Berger, R.D.; Rosas, G.O.; Kobeissi, Z.A.; Marbán, E.; Hare, J.M. Allopurinol improves myocardial efficiency in patients with idiopathic dilated cardiomyopathy. Circulation 2001, 104, 2407–2411. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Ma, R. Cardiac sympathetic afferent reflexes in heart failure. Heart Fail. Rev. 2000, 5, 57–71. [Google Scholar] [CrossRef]
- Givertz, M.M.; Anstrom, K.J.; Redfield, M.M.; Deswal, A.; Haddad, H.; Butler, J.; Tang, W.H.W.; Dunlap, M.E.; LeWinter, M.M.; Mann, D.L.; et al. Effects of xanthine oxidase inhibition in hyperuricemic heart failure patients: The xanthine oxidase inhibition for hyperuricemic heart failure patients (EXACT-HF) study. Circulation 2015, 131, 1763–1771. [Google Scholar] [CrossRef] [PubMed]
- Lymperopoulos, A.; Rengo, G.; Koch, W.J. Adrenergic nervous system in heart failure: Pathophysiology and therapy. Circ. Res. 2013, 113, 739–753. [Google Scholar] [CrossRef]
- Pugliese, N.R.; de Biase, N.; Balletti, A.; Filidei, F.; Pieroni, A.; D’Angelo, G.; Armenia, S.; Mazzola, M.; Gargani, L.; Del Punta, L.; et al. Characterization of hemodynamic and metabolic abnormalities in the heart failure spectrum: The role of combined cardiopulmonary and exercise echocardiography stress test. Minerva Cardiol. Angiol. 2022, 70, 370–384. [Google Scholar] [CrossRef]
- Pugliese, N.R.; Mazzola, M.; Madonna, R.; Gargani, L.; De Biase, N.; Dini, F.L.; Taddei, S.; De Caterina, R.; Masi, S. Exercise-induced pulmonary hypertension in HFpEF and HFrEF: Different pathophysiologic mechanism behind similar functional impairment. Vascul. Pharmacol. 2022, 144, 106978. [Google Scholar] [CrossRef]
- Pugliese, N.R.; Mazzola, M.; Fabiani, I.; Gargani, L.; De Biase, N.; Pedrinelli, R.; Natali, A.; Dini, F.L. Haemodynamic and metabolic phenotyping of hypertensive patients with and without heart failure by combining cardiopulmonary and echocardiographic stress test. Eur. J. Heart Fail. 2020, 22, 458–468. [Google Scholar] [CrossRef]
- Pugliese, N.R.; Pellicori, P.; Filidei, F.; Del Punta, L.; De Biase, N.; Balletti, A.; Di Fiore, V.; Mengozzi, A.; Taddei, S.; Gargani, L.; et al. The incremental value of multi-organ assessment of congestion using ultrasound in outpatients with heart failure. Eur. Hear. J.-Cardiovasc. Imaging 2023, jeac254. [Google Scholar] [CrossRef]
- Frankenstein, L.; Zugck, C.; Schellberg, D.; Nelles, M.; Froehlich, H.; Katus, H.; Remppis, A. Prevalence and prognostic significance of adrenergic escape during chronic β-blocker therapy in chronic heart failure. Eur. J. Heart Fail. 2009, 11, 178–184. [Google Scholar] [CrossRef] [PubMed]
- Riehle, C.; Bauersachs, J. Key inflammatory mechanisms underlying heart failure. Herz 2019, 44, 96–106. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Hu, K.; Lau, K.; Kiwitz, T.; Robitzkat, K.; Hammel, C.; Lengenfelder, B.D.; Ertl, G.; Frantz, S.; Nordbeck, P. Impact of diastolic dysfunction on outcome in heart failure patients with mid-range or reduced ejection fraction. ESC Hear. Fail. 2021, 8, 2802–2815. [Google Scholar] [CrossRef] [PubMed]
- Obokata, M.; Borlaug, B.A. The strengths and limitations of E/e’ in heart failure with preserved ejection fraction. Eur. J. Heart Fail. 2018, 20, 1312–1314. [Google Scholar] [CrossRef] [PubMed]
- Guazzi, M.; Bandera, F.; Pelissero, G.; Castelvecchio, S.; Menicanti, L.; Ghio, S.; Temporelli, P.L.; Arena, R. Tricuspid annular plane systolic excursion and pulmonary arterial systolic pressure relationship in heart failure: An index of right ventricular contractile function and prognosis. Am. J. Physiol.-Hear. Circ. Physiol. 2013, 305, H1373–H1381. [Google Scholar] [CrossRef]
- Pestelli, G.; Fiorencis, A.; Trevisan, F.; Luisi, G.A.; Smarrazzo, V.; Mele, D. New measures of right ventricle-pulmonary artery coupling in heart failure: An all-cause mortality echocardiographic study. Int. J. Cardiol. 2021, 329, 234–241. [Google Scholar] [CrossRef]
- Nishino, M.; Egami, Y.; Kawanami, S.; Sugae, H.; Ukita, K.; Kawamura, A.; Nakamura, H.; Matsuhiro, Y.; Yasumoto, K.; Tsuda, M.; et al. Lowering Uric Acid May Improve Prognosis in Patients With Hyperuricemia and Heart Failure With Preserved Ejection Fraction. J. Am. Heart Assoc. 2022, 11, e026301. [Google Scholar] [CrossRef]
- Vaduganathan, M.; Docherty, K.F.; Claggett, B.L.; Jhund, P.S.; de Boer, R.A.; Hernandez, A.F.; Inzucchi, S.E.; Kosiborod, M.N.; Lam, C.S.P.; Martinez, F.; et al. SGLT-2 inhibitors in patients with heart failure: A comprehensive meta-analysis of five randomised controlled trials. Lancet 2022, 400, 757–767. [Google Scholar] [CrossRef]
- La Grotta, R.; de Candia, P.; Olivieri, F.; Matacchione, G.; Giuliani, A.; Rippo, M.R.; Tagliabue, E.; Mancino, M.; Rispoli, F.; Ferroni, S.; et al. Anti-inflammatory effect of SGLT-2 inhibitors via uric acid and insulin. Cell. Mol. Life Sci. 2022, 79, 273. [Google Scholar] [CrossRef]
- Scisciola, L.; Cataldo, V.; Taktaz, F.; Fontanella, R.A.; Pesapane, A.; Ghosh, P.; Franzese, M.; Puocci, A.; De Angelis, A.; Sportiello, L.; et al. Anti-inflammatory role of SGLT2 inhibitors as part of their anti-atherosclerotic activity: Data from basic science and clinical trials. Front. Cardiovasc. Med. 2022, 9, 2508. [Google Scholar] [CrossRef] [PubMed]
- Zelniker, T.A.; Braunwald, E. Mechanisms of Cardiorenal Effects of Sodium-Glucose Cotransporter 2 Inhibitors: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2020, 75, 422–434. [Google Scholar] [CrossRef] [PubMed]
| Variable | HFrEF (n = 96) | HFpEF (n = 174) | p-Value |
|---|---|---|---|
| Demographics | |||
| Age, years | 73 ± 11.4 | 75 ± 11.6 | 0.1 |
| Male | 77 (80.2) | 97 (55.7) | 0.1 |
| BMI, Kg/m2 | 25.5 (23.2–28.9) | 27.5 (25.4–30.2) | <0.001 |
| Waist circumference, cm | 80 (71–91) | 95 (91–106) | <0.001 |
| Obesity | 25 (26) | 44 (25.3) | 0.8 |
| Smoker | 21 (21.9) | 28 (16) | 0.2 |
| Clinical evaluation | |||
| NYHA I | 27 (28.1) | 45 (25.8) | <0.001 |
| NYHA II | 49 (51) | 83 (47.7) | 0.1 |
| NYHA III | 14 (14.5) | 41 (23.5) | 0.1 |
| Arterial hypertension | 57 (59.3) | 126 (72.4) | 0.028 |
| Dyslipidaemia # | 60 (62.5) | 94 (54) | 0.1 |
| Stroke/TIA | 8 (8.3) | 24 (13.7) | 0.2 |
| Diabetes mellitus | 29 (30.2) | 56 (32.1) | 0.7 |
| CKD | 50 (42) | 43(38) | 0.5 |
| CAD | 38 (39.5) | 49 (28.1) | 0.05 |
| Previous PCI/CABG | 33 (34.4) | 43 (24.7) | 0.09 |
| Previous MI | 29 (30.2) | 27 (15.5) | 0.004 |
| ICD | 25 (26) | 22 (12.6) | 0.006 |
| Therapy | |||
| Beta-blocker | 82 (70) | 102 (64) | <0.0001 |
| DHP CCB | 33 (16) | 47 (25) | 0.08 |
| Non-DHP CCB | 0 | 4 (2) | 0.1 |
| ACEi or ARB | 87 (71) | 132 (70) | 0.1 |
| MRA | 83 (49) | 71 (38) | <0.0001 |
| Digoxin | 21 (10) | 13 (7) | 0.01 |
| ARNI | 45 (22) | 0 | <0.0001 |
| Statins | 87 (65) | 90 (49) | <0.0001 |
| Thiazides | 28 (14) | 20 (10) | 0.05 |
| Furosemide | 89 (70) | 20 (11) | 0.001 |
| Insulin | 7 (7) | 16 (9) | 0.001 |
| SGLT2i | 29 (30) | 22 (13) | 0.001 |
| Other oral hypoglycaemic drugs | 21 (22) | 33 (19) | 0.5 |
| Variable | HFrEF (n = 96) | HFpEF (n = 174) | p-Value |
|---|---|---|---|
| HbA1c, mmol/mol | 41 (37.8–45) | 40 (37–44) | 0.5 |
| Norepinephrine, pg/mL | 297 (153–403) | 354 (255–523) | 0.03 |
| Uric acid, mg/dL | 6.3 (4.8–7.5) | 8.1 (5.9–9.9) | 0.01 |
| hs-CRP, mg/dL | 0.31 (0.21–0.57) | 0.44 (0.31–0.63) | 0.03 |
| NT-pro BNP, pg/ml | 1428 (506–3155) | 885 (442–1163) | 0.01 |
| Interleukin-6, pg/mL | 3.85 (1.5–9) | 4.25 (1.6–8.42) | 0.6 |
| Total pulmonary B lines | 2 (0–8) | 2 (0–7) | 0.9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Balletti, A.; De Biase, N.; Del Punta, L.; Filidei, F.; Armenia, S.; Masi, F.; Di Fiore, V.; Mazzola, M.; Bacca, A.; Dini, F.L.; et al. Cardiometabolic Phenotyping in Heart Failure: Differences between Patients with Reduced vs. Preserved Ejection Fraction. Diagnostics 2023, 13, 790. https://doi.org/10.3390/diagnostics13040790
Balletti A, De Biase N, Del Punta L, Filidei F, Armenia S, Masi F, Di Fiore V, Mazzola M, Bacca A, Dini FL, et al. Cardiometabolic Phenotyping in Heart Failure: Differences between Patients with Reduced vs. Preserved Ejection Fraction. Diagnostics. 2023; 13(4):790. https://doi.org/10.3390/diagnostics13040790
Chicago/Turabian StyleBalletti, Alessio, Nicolò De Biase, Lavinia Del Punta, Francesco Filidei, Silvia Armenia, Filippo Masi, Valerio Di Fiore, Matteo Mazzola, Alessandra Bacca, Frank L. Dini, and et al. 2023. "Cardiometabolic Phenotyping in Heart Failure: Differences between Patients with Reduced vs. Preserved Ejection Fraction" Diagnostics 13, no. 4: 790. https://doi.org/10.3390/diagnostics13040790
APA StyleBalletti, A., De Biase, N., Del Punta, L., Filidei, F., Armenia, S., Masi, F., Di Fiore, V., Mazzola, M., Bacca, A., Dini, F. L., Taddei, S., Masi, S., & Pugliese, N. R. (2023). Cardiometabolic Phenotyping in Heart Failure: Differences between Patients with Reduced vs. Preserved Ejection Fraction. Diagnostics, 13(4), 790. https://doi.org/10.3390/diagnostics13040790








