Associations among Health Status, Occupation, and Occupational Injuries or Diseases: A Multi-Level Analysis
Abstract
1. Introduction
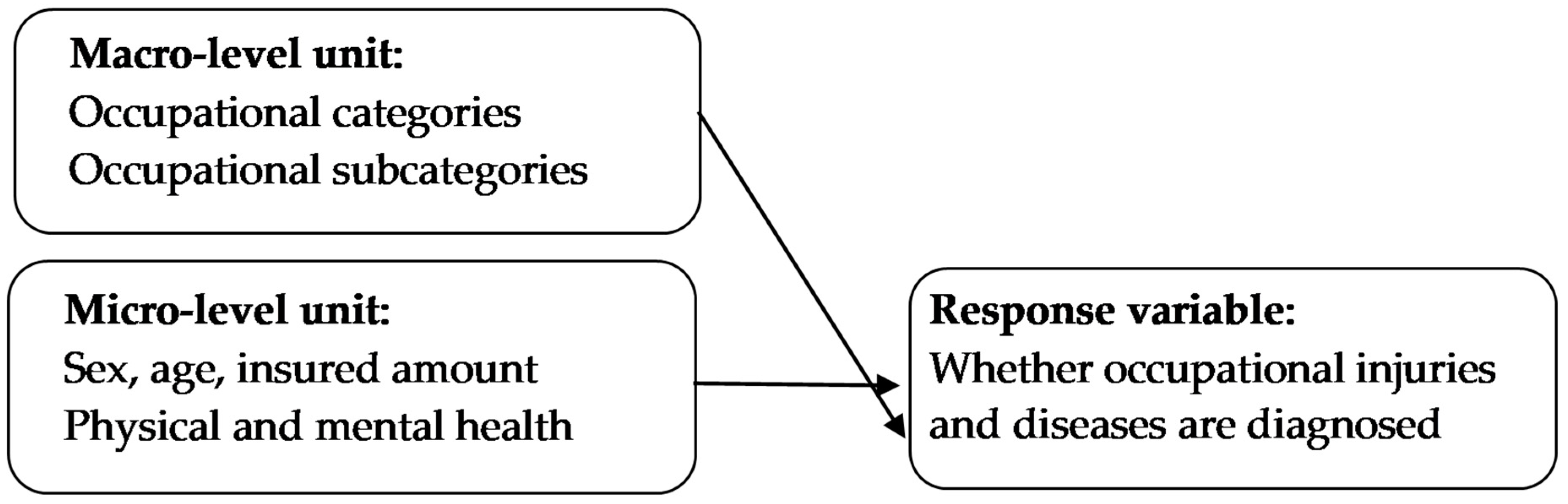
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
- For the occupational subcategories of employees with fixed employers (Subcategory 12 in Category 1), employees of private business organizations (Subcategory 2), and sangha and religionists of Category 6, who were prone to occupational injuries and diseases, the government shall prioritize stipulation of relevant health policy and regulations to facilitate adequate monitoring and intervention.
- Older age as well as long-term exposure to chemical substances increase the risk of occupational injuries and diseases. Therefore, relevant agencies must establish norms to allow free and periodic health examinations for laborers with a certain period of seniority to prevent occupational injuries and diseases.
- Employers must ensure occupational environment safety and health. They should conduct on-the-job training and establish rapid occupational injury report systems to minimize the incidence and reduce the severity of occupational accidents.
- Occupational injury clinics should implement integrated medical procedures. In addition, occupational injury prevention centers shall be established to reduce the time to access medical care in case of occupational injuries.
- Health institutes should periodically monitor patients of occupational accidents or patients with chronic diseases (e.g., hypertension and cardiovascular diseases), remind these patients of the medication safety and side effects that may affect work, and arrange periodic health examinations for the patients to control their conditions.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Administration, H.P. Accidents Ranked the Seventh among the top 10 Causes of Death in Taiwan. Available online: https://www.mohw.gov.tw/cp-16-70314-1.html (accessed on 12 September 2021).
- Inaba, Y.; Hitachi, S.; Watanuki, M.; Chida, K. Occupational radiation dose to eye lenses in CT-guided interventions using MDCT-fluoroscopy. Diagnostics 2021, 11, 646. [Google Scholar] [CrossRef] [PubMed]
- Inaba, Y.; Hitachi, S.; Watanuki, M.; Chida, K. Radiation eye dose for physicians in CT fluoroscopy-guided biopsy. Tomography 2022, 8, 438–446. [Google Scholar] [CrossRef] [PubMed]
- Kouvonen, A.; Kivimäki, M.; Oksanen, T.; Pentti, J.; De Vogli, R.; Virtanen, M.; Vahtera, J. Obesity and occupational injury: A prospective cohort study of 69,515 public sector employees. PLoS ONE 2013, 8, e77178. [Google Scholar] [CrossRef] [PubMed]
- Brown, E.; Choi, S. A Review of Obesity and Body Mass Index and Nonfatal Traumatic Occupational Injuries. In Proceedings of the Annual World Conference of the Society for Industrial and Systems Engineering, Fort Lauderdale, FL, USA, 19–21 October 2015. [Google Scholar]
- Kubo, J.; Goldstein, B.A.; Cantley, L.F.; Tessier-Sherman, B.; Galusha, D.; Slade, M.D.; Chu, I.M.; Cullen, M.R. Contribution of health status and prevalent chronic disease to individual risk for workplace injury in the manufacturing environment. Occup. Environ. Med. 2014, 71, 159–166. [Google Scholar] [CrossRef]
- Leigh, J.P.; Markowitz, S.B.; Fahs, M.; Shin, C.; Landrigan, P.J. Occupational injury and illness in the United States: Estimates of costs, morbidity, and mortality. Arch. Intern. Med. 1997, 157, 1557–1568. [Google Scholar] [CrossRef] [PubMed]
- Jackson, L.L. Non-fatal occupational injuries and illnesses treated in hospital emergency departments in the United States. Injury Prevent. 2001, 7, i21–i26. [Google Scholar] [CrossRef]
- Cheng, T.M. Taiwan’s National Health Insurance system: High value for the dollar. In Six Countries, Six Reform Models—The Healthcare Reform Experience of Israel, the Netherlands, New Zealand, Singapore, Switzerland and Taiwan; Okma, K.G.H., Crivelli, L., Eds.; World Scientific: Hackensack, NJ, USA, 2009; pp. 171–204. [Google Scholar]
- Goetzel, R.Z.; Anderson, D.R.; Whitmer, R.W.; Ozminkowski, R.J.; Dunn, R.L.; Wasserman, J. The relationship between modifiable health risks and health care expenditures: An analysis of the multi-employer HERO health risk and cost database. J. Occup. Environ. Med. 1998, 40, 843–854. [Google Scholar] [CrossRef]
- He, P.X.; Wu, T.J.; Zhao, H.D.; Yang, Y. How to motivate employees for sustained innovation behavior in job stressors? A cross-level analysis of organizational innovation climate. Int. J. Environ. Res. Public Health 2019, 16, 4608. [Google Scholar] [CrossRef]
- Roberts, J. The importance of the intraclass correlation in multilevel and hierarchical linear modeling design. Multiple Linear Regres. Viewp. 2002, 28, 19–31. [Google Scholar]
- Cunningham, T.R.; Guerin, R.J.; Ferguson, J.; Cavallari, J. Work-related fatigue: A hazard for workers experiencing disproportionate occupational risks. Am. J. Ind. Med. 2022, 65, 913–925. [Google Scholar] [CrossRef]
- Lu, J.L. State and trends of occupational health and safety in the Philippines. Acta Med. Philippina 2022, 56. [Google Scholar] [CrossRef]
- Breslin, F.C.; Smith, P. Age-related differences in work injuries: A multivariate, population-based study. Am. J. Ind. Med. 2005, 48, 50–56. [Google Scholar] [CrossRef]
- Chiou, H.; Wen, F. Hierarchical linear modeling of contextual effects: An example of organizational climate of creativity at schools and teacher’s creative performance. J. Educ. Psychol. 2007, 30, 1–35. [Google Scholar]
- Murray, L.; Nguyen, H.; Lee, Y.-F.; Remmenga, M.D.; Smith, D.W. Variance inflation factors in regression models with dummy variables. In Proceedings of the twenty-fourth annual Kansas State University Conference on Applied Statistics in Agriculture, Manhattan, Kansas, 29 April 29–1 May 2012. [Google Scholar]
- Alamgir, H.; Yu, S.; Drebit, S.; Fast, C.; Kidd, C. Are female healthcare workers at higher risk of occupational injury? Occup. Med. 2009, 59, 149–152. [Google Scholar] [CrossRef]
- Feinstein, J.S. The relationship between socioeconomic status and health: A review of the literature. Milbank Qtly. 1993, 71, 279–322. [Google Scholar] [CrossRef]
- Zöller, B.; Li, X.; Sundquist, J.; Sundquist, K. Socioeconomic and occupational risk factors for venous thromboembolism in Sweden: A nationwide epidemiological study. Thromb. Res. 2012, 129, 577–582. [Google Scholar] [CrossRef] [PubMed]
- Berecki-Gisolf, J.; Collie, A.; Hassani-Mahmooei, B.; McClure, R. Use of antidepressant medication after road traffic injury. Injury 2015, 46, 1250–1256. [Google Scholar] [CrossRef]
- Gates, J.; Dubois, S.; Mullen, N.; Weaver, B.; Bédard, M. The influence of stimulants on truck driver crash responsibility in fatal crashes. Forensic Sci. Int. 2013, 228, 15–20. [Google Scholar] [CrossRef]
- Chin, W.S.; Liao, S.C.; Pan, S.C.; Guo, Y.L.L. Occupational and non-occupational injuries can result in prolonged augmentation of psychiatric disorders. J. Epidemiol. 2022, 32, 12–20. [Google Scholar] [CrossRef]
- Lin, K.H.; Chu, P.C.; Kuo, C.Y.; Hwang, Y.H.; Wu, S.C.; Guo, Y.L. Psychiatric disorders after occupational injury among National Health Insurance enrollees in Taiwan. Psychiatry Res. 2014, 219, 645–650. [Google Scholar] [CrossRef]
- Chokkhanchitchai, S.; Tangarunsanti, T.; Jaovisidha, S.; Nantiruj, K.; Janwityanujit, S. The effect of religious practice on the prevalence of knee osteoarthritis. Clin. Rheumatol. 2010, 29, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Bosittipichet, T.; Chinasote, Y.; Leesri, T. Prevalence and related factors of knee osteoarthritis in Buddhist monks in Ayutthaya. Suranaree J. Sci. Technol. 2018, 25, 462–468. [Google Scholar]
- Jeamjitvibool, T.; Tankumpuan, T.; Lukkahatai, N.; Davidson, P.M. Noncommunicable diseases and social determinants of health in Buddhist monks: An integrative review. Res. Nurs. Health 2022, 45, 249–260. [Google Scholar] [CrossRef] [PubMed]
- De Merich, D.; Gnoni, M.; Guglielmi, A.; Micheli, G.; Sala, G.; Tornese, F.; Vitrano, G. Designing national systems to support the analysis and prevention of occupational fatal injuries: Evidence from Italy. Saf. Sci. 2022, 147, 105615. [Google Scholar] [CrossRef]
- Bonauto, D.; Silverstein, B.; Adams, D.; Foley, M. Prioritizing industries for occupational injury and illness prevention and research, Washington State Workers’ compensation claims, 1999-2003. J. Occup. Environ. Med. 2006, 48, 840–851. [Google Scholar] [CrossRef]
- Weichelt, B.; Scott, E.; Burke, R.; Shutske, J.; Gorucu, S.; Sanderson, W.; Madsen, M.; Redmond, E.; Murphy, D.J.; Rautiainen, R. What about the rest of them? Fatal injuries related to production agriculture not captured by the Bureau of Labor Statistics (BLS) Census of Fatal Occupational Injuries (CFOI). J. Agromed. 2022, 27, 35–40. [Google Scholar] [CrossRef]
| Variable | Presence of Occupational Injuries or Diseases | ||
|---|---|---|---|
| OR | 95% C.I. | p-Value | |
| Sex | |||
| Women (reference group) | -- | -- | -- |
| Men | 0.631 | (0.598–0.664) | <0.0001 * |
| Age | |||
| 20–30 years (reference group) | -- | -- | -- |
| 31–40 years | 1.172 | (1.084–1.267) | <0.0001 * |
| 41–50 years | 1.247 | (1.068–1.456) | <0.0001 * |
| 51–60 years | 2.913 | (2.386–3.558) | 0.0053 * |
| >60 years | 14.563 | (11.503–18.437) | <0.0001 * |
| Payroll bracket | |||
| NTD 22,800 or lower (reference group) | -- | -- | -- |
| NTD 22,801–28,800 | 1.353 | (1.067–1.716) | 0.0125 * |
| NTD 28,801–36,300 | 0.958 | (0.926–0.991) | 0.0129 * |
| NTD 36,301–45,800 | 0.914 | (0.874–0.956) | <0.0001 * |
| NTD 45,801–57,800 | 0.997 | (0.931–1.067) | 0.9241 |
| NTD 57,801 or higher | 1.386 | (1.315–1.461) | <0.0001 * |
| Urbanization level | |||
| Highly urbanized cities or counties (reference group) | -- | -- | -- |
| Moderately urbanized cities or counties | 1.062 | (0.997–1.131) | 0.0625 |
| Townships or county-administered cities | 0.881 | (0.812–0.956) | 0.0025 * |
| Aging cities or counties | 1.504 | (0.956–1.162) | 0.2930 |
| Remote townships | 1.060 | (0.885–1.269) | 0.5278 |
| Emerging cities or counties | 1.730 | (1.479–2.025) | <0.0001 * |
| Agricultural cities or counties | 1.169 | (1.033–1.323) | 0.0132 * |
| NHI Administration division | |||
| Taipei Division (reference group) | -- | -- | -- |
| Central Division | 1.325 | (1.277–1.375) | <0.0001 * |
| Northern Division | 0.836 | (0.781–0.895) | <0.0001 * |
| Eastern Division | 1.152 | (1.078–1.231) | <0.0001 * |
| Southern Division | 1.069 | (1.024–1.117) | 0.0025* |
| Kaoping Division | 0.585 | (0.529–0.647) | <0.0001 * |
| Illness | |||
| Mental illness | |||
| Without mental illness | -- | -- | -- |
| With mental illness | 1.258 | (1.209–1.309) | <0.0001 * |
| Obesity | |||
| Not obese | -- | -- | -- |
| Obese | 1.138 | (1.088–1.191) | <0.0001 * |
| Diabetes | |||
| Without diabetes | -- | -- | -- |
| With diabetes | 1.997 | (1.974–1.997) | <0.0001 * |
| Asthma | |||
| Without asthma | -- | -- | -- |
| With asthma | 1.138 | (1.088–1.191) | <0.0001 * |
| Chronic heart disease | |||
| Without chronic heart disease | -- | -- | -- |
| With chronic heart disease | 1.004 | (1.004–1.1.024) | <0.0001 * |
| Hypertension | |||
| Without hypertension | -- | -- | -- |
| With hypertension | 1.965 | (1.948–1.983) | 0.0001 * |
| Medication | |||
| Sedative–hypnotics | |||
| Not taking sedative–hypnotics | -- | -- | -- |
| Taking sedative–hypnotics | 1.076 | (1.106–1.140) | 0.0127 * |
| Antipsychotics | |||
| Not taking antipsychotics | -- | -- | -- |
| Taking antipsychotics | 1.844 | (1.760–1.938) | 0.0017 * |
| Controlled analgesics | |||
| Not taking controlled analgesics | -- | -- | -- |
| Taking controlled analgesics | 1.060 | (0.895–1.255) | 0.0012 * |
| Cardiovascular medications | |||
| Not taking cardiovascular medications | -- | -- | -- |
| Taking cardiovascular medications | 1.818 | (1.794–1.842) | <0.0001 * |
| Diuretics | |||
| Not taking diuretics | -- | -- | -- |
| Taking diuretics | 1.889 | (1.791–1.999) | 0.0073 * |
| Surgery | |||
| Having not undergone surgery | -- | -- | -- |
| Having undergone surgery | 1.709 | (1.609–1.815) | <0.0001 * |
| Variable | p-Value | OR | 95% Confidence Limits |
|---|---|---|---|
| Intercept (reference groups) | -- | -- | -- |
| (civil servants, labor, workers, and self-employed owners of businesses: civil servants at central agencies) | 0.0133 * | 1.4657 | (1.0828–1.9840) |
| (civil servant, labor, and self-employed owners of businesses: civil servants at provincial (city) agencies and agencies below the level) | <0.0001 * | 2.0726 | (1.5323–2.8030) |
| (civil servant, labor, and self-employed owners of businesses: civil servants at local agencies) | 0.7269 | 0.9127 | (0.5466–1.5239) |
| (civil servant, labor, and self-employed owners of businesses: employees of private junior colleges and schools) | 0.0875 | 1.4706 | (0.9448–2.2890) |
| (civil servant, labor, and self-employed owners of businesses: teachers of private high and elementary schools) | 0.0300 * | 1.7477 | (1.0557–2.8936) |
| (civil servant, labor, and self-employed owners of businesses: entry-level workers at publicly owned enterprises and institutions [public employee insurance program]) | 0.9923 | 1.0015 | (0.7386–1.3580) |
| (civil servant, labor, and self-employed owners of businesses: entry-level workers at public owned enterprises and institutions [labor insurance program]) | 0.0002 * | 0.5780 | (0.4320–0.7735) |
| (civil servant, labor, and self-employed owners of businesses: employees of privately owned enterprises and institutions) | <0.0001 * | 0.4475 | (0.3405–0.5880) |
| civil servant, labor, and self-employed owners of businesses: entry-level workers at central agencies and national junior colleges) | <0.0001 * | 0.5177 | (0.3749–0.7149) |
| (civil servant, labor, and self-employed owners of businesses: entry-level workers at schools and provincial (city) agencies and agencies below the level) | <0.0001 * | 0.4354 | (0.3267–0.5805) |
| (civil servant, labor, and self-employed owners of businesses: entry-level workers at private schools) | 0.1817 | 0.7034 | (0.4197–1.1789) |
| (civil servant, labor, and self-employed owners of businesses: employees employed by particular employers) | <0.0001 * | 4.1074 | (2.8210–5.9799) |
| (civil servant, labor, and self-employed owners of businesses: employees of nonprofit enterprises and institutions) | <0.0001 * | 0.4296 | (0.3229–0.5716) |
| (civil servant, labor, and self-employed owners of businesses: independently practicing professionals and technicians) | 0.9114 | 1.0721 | (0.3147–3.6517) |
| (professionals, seamen, and sea captains: members of an occupational union) | <0.0001 * | 0.3809 | (0.2897–0.5009) |
| (professionals, seamen, and sea captains: seamen serving on foreign vessels who are members of the National Seamen’s Union or the Master Mariners’ Association) | 0.6969 | 1.2571 | (0.3976–3.9749) |
| (farmers and fishermen: farmers) | 0.0121 * | 1.4310 | (1.0817–2.9496) |
| (farmers and fishermen: members of the Irrigation Association) | 0.6014 | 1.3492 | (0.4386–1.5506) |
| (farmers and fishermen: members of the National Fishermen’s Association) | 0.0778 | 0.7671 | (0.5713–1.7706) |
| (military personnel: bereaved family members of military personnel who are receiving pensions due to the death of the military personnel members and military personnel’s dependents who lost their support) | 0.0389 * | 0.6987 | (0.4972–1.6441) |
| (military personnel: military school students who receive grants from the government and people who are in mandatory military service) | 0.0363 * | 0.5423 | (0.30571.3576) |
| (military personnel: people who are in alternative military service) | 0.9363 | 1.0518 | (0.3053–1.3570) |
| (members of low-income families: members of low-income families who are placed in social welfare service institutions) | 0.2500 | 1.5536 | (0.7334–2.0821) |
| (members of low-income families: members of low-income families whose group insurance applicants are village [township, municipal, or district] administration offices) | 0.1220 | 0.7772 | (0.5646–1.7587) |
| (members of the Sangha and other Taiwanese nationals: veterans placed in social welfare service institutions) | 0.2587 | 1.6361 | (0.6964–2.0064) |
| (members of the Sangha and other Taiwanese nationals: veterans and bereaved family members of veterans) | 0.9363 | 0.7893 | (0.5986–1.8195) |
| members of the Sangha and other Taiwanese nationals: members of the Sangha and religious workers | 0.0104 * | 2.0079 | (1.1777–3.2470) |
| residents of social welfare service institutions | 0.5121 | 1.4447 | (0.4810–1.6177) |
| Variable | Reference Group | BLR | HGLM |
|---|---|---|---|
| Sex | Female | ✓ | ✓ |
| Age | 20–30 years | ✓ | ✓ |
| Insured amount | NTD 22,800 or lower | ✓ | ✓ |
| Mental disorders | Without | ✓ | ✓ |
| Obesity | Without | ✓ | ✓ |
| Diabetes | Without | ✓ | |
| Chronic heart diseases | Without | ✓ | |
| Hypertension | Without | ✓ | ✓ |
| Asthma | Without | ✓ | ✓ |
| Sedative–hypnotic drugs | Did not use | ✓ | |
| Antipsychotics | Did not use | ✓ | ✓ |
| Controlled analgesics | Did not use | ✓ | |
| Cardiovascular drugs | Did not use | ✓ | ✓ |
| Diuretics | Did not use | ✓ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Su, S.-Y.; Li, Y.-W.; Wen, F.-H.; Yao, C.-Y.; Wang, J.-Y. Associations among Health Status, Occupation, and Occupational Injuries or Diseases: A Multi-Level Analysis. Diagnostics 2023, 13, 381. https://doi.org/10.3390/diagnostics13030381
Su S-Y, Li Y-W, Wen F-H, Yao C-Y, Wang J-Y. Associations among Health Status, Occupation, and Occupational Injuries or Diseases: A Multi-Level Analysis. Diagnostics. 2023; 13(3):381. https://doi.org/10.3390/diagnostics13030381
Chicago/Turabian StyleSu, Shu-Yuan, Yu-Wen Li, Fur-Hsing Wen, Chi-Yu Yao, and Jong-Yi Wang. 2023. "Associations among Health Status, Occupation, and Occupational Injuries or Diseases: A Multi-Level Analysis" Diagnostics 13, no. 3: 381. https://doi.org/10.3390/diagnostics13030381
APA StyleSu, S.-Y., Li, Y.-W., Wen, F.-H., Yao, C.-Y., & Wang, J.-Y. (2023). Associations among Health Status, Occupation, and Occupational Injuries or Diseases: A Multi-Level Analysis. Diagnostics, 13(3), 381. https://doi.org/10.3390/diagnostics13030381






