Intraoral Ultrasonography for Periodontal Tissue Exploration: A Review
Abstract
1. Introduction
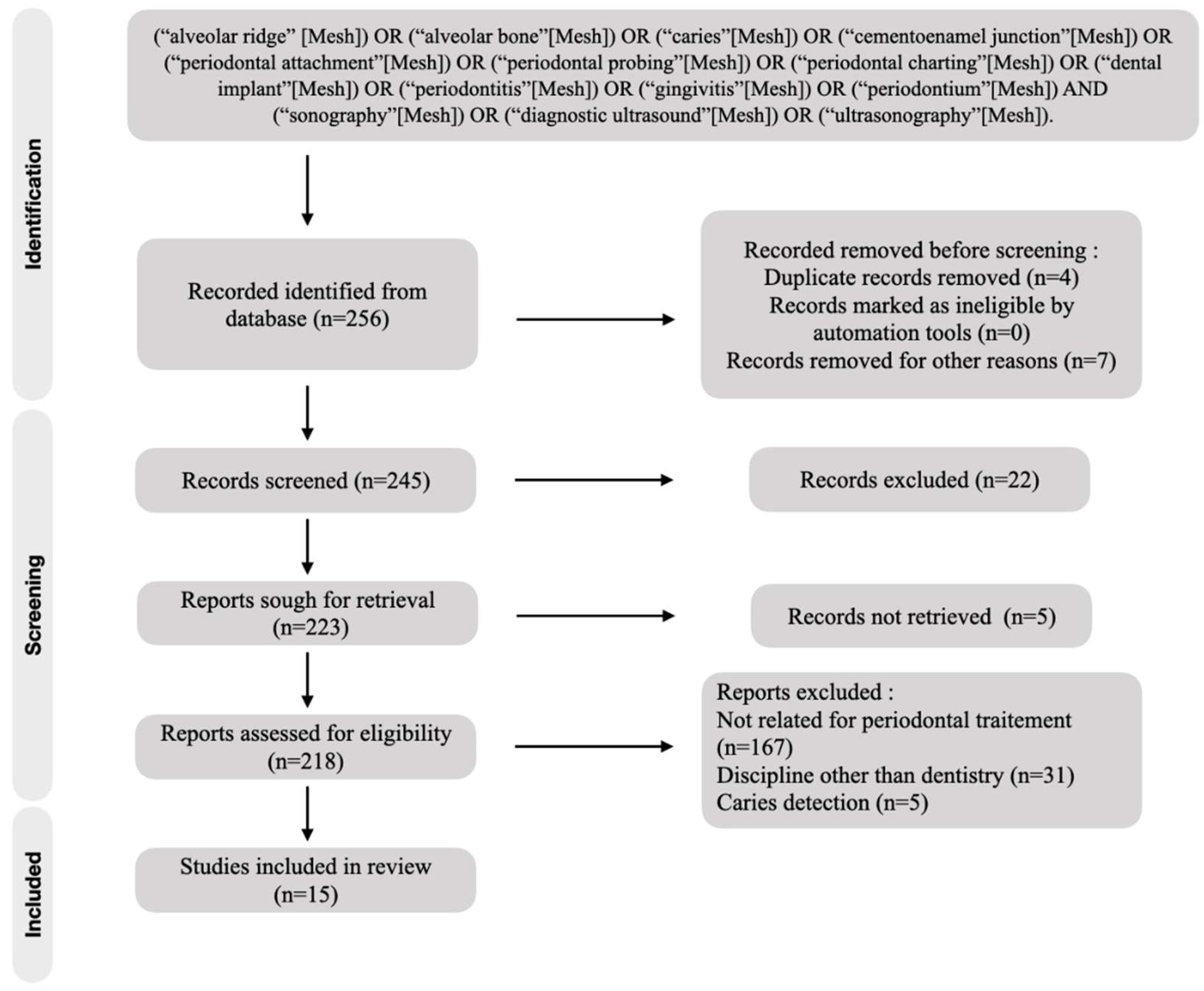
2. Materials and Methods
2.1. Search Strategy
2.2. Study Detection
Inclusion and Exclusion Criteria
2.3. Data Collection
3. Results
3.1. Study Selection
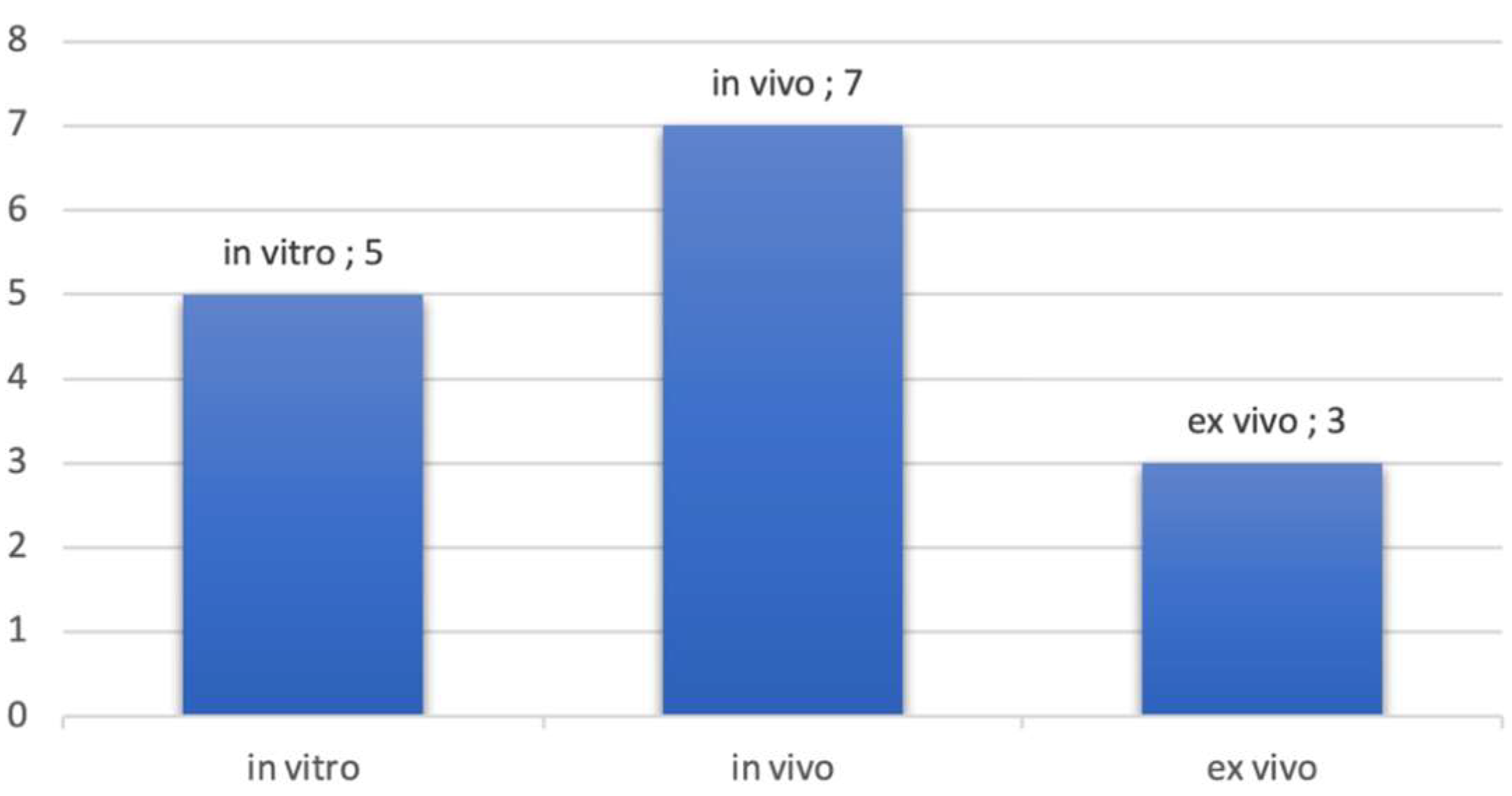
3.2. Test Evolution
3.3. Overview of Ultrasonographic Devices
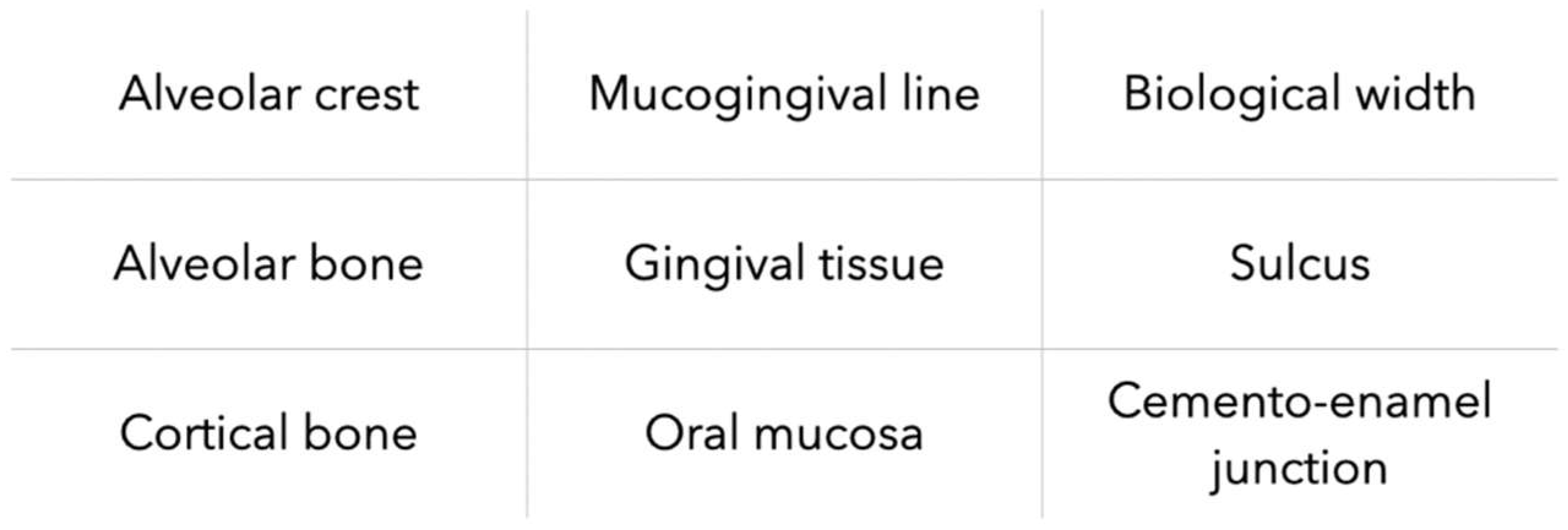
3.4. Periodontal Tissues Description with Ultrasonographic Imagery
3.5. Types of Measurements and Comparison
4. Discussion
5. Limitations
6. Perspectives
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wolf, D.L.; Lamster, I.B. Contemporary Concepts in the Diagnosis of Periodontal Disease. Dent. Clin. N. Am. 2011, 55, 47–61. [Google Scholar] [CrossRef] [PubMed]
- Chapple, I.L.C.; Mealey, B.L.; van Dyke, T.E.; Bartold, P.M.; Dommisch, H.; Eickholz, P.; Geisinger, M.L.; Genco, R.J.; Glogauer, M.; Goldstein, M.; et al. Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium: Consensus report of workgroup 1 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Periodontol. 2018, 89, S74–S84. [Google Scholar] [CrossRef] [PubMed]
- Lang, N.P.; Bartold, P.M. Periodontal health. J. Periodontol. 2018, 89, S9–S16. [Google Scholar] [CrossRef] [PubMed]
- Lang, N.P.; Joss, A.; Tonetti, M.S. Monitoring disease during supportive periodontal treatment by bleeding on probing. Periodontology 2000, 12, 44–48. [Google Scholar] [CrossRef]
- Greenstein, G. The Role of Bleeding upon Probing in the Diagnosis of Periodontal Disease: A Literature Review. J. Periodontol. 1984, 55, 684–688. [Google Scholar] [CrossRef]
- Karayiannis, A.; Lang, N.P.; Joss, A.; Nyman, S. Bleeding on probing as it relates to probing pressure and gingival health in patients with a reduced but healthy periodontium. J. Clin. Periodontol. 1992, 19, 471–475. [Google Scholar] [CrossRef]
- Kour, A.; Kumar, A.; Puri, K.; Khatri, M.; Bansal, M.; Gupta, G. Comparative evaluation of probing depth and clinical attachment level using a manual probe and Florida probe. J. Indian Soc. Periodontol. 2016, 20, 299. [Google Scholar]
- Wikner, S.; Söder, P.Ö.; Frithiof, L.; Wouters, F. The approximal bone height and intrabony defects in young adults, related to the salivary buffering capacity and counts of Streptococcus mutans and lactobacilli. Arch. Oral Biol. 1990, 35, 213–215. [Google Scholar] [CrossRef]
- Fukukita, H.; Yano, T.; Fukumoto, A.; Sawada, K.; Fujimasa, T.; Sunada, I. Development and application of an ultrasonic imaging system for dental diagnosis. J. Clin. Ultrasound 1985, 13, 597–600. [Google Scholar] [CrossRef]
- Gennisson, J.L.; Deffieux, T.; Fink, M.; Tanter, M. Ultrasound elastography: Principles and techniques. Diagn. Interv. Imaging 2013, 94, 487–495. [Google Scholar] [CrossRef]
- Cootney, R.W.; Coatney, R.W. Ultrasound Imaging: Principles and Applications in Rodent Research. ILAR J. 2001, 42, 233–247. [Google Scholar] [CrossRef]
- Banquart, A.; Callé, S.; Levassort, F.; Fritsch, L.; Ossant, F.; Toffessi Siewe, S.; Chevalliot, S.; Capri, A.; Grégoire, J.-M. Piezoelectric P(VDF-TrFE) film inkjet printed on silicon for high-frequency ultrasound applications. J. Appl. Phys. 2021, 129, 195107. [Google Scholar] [CrossRef]
- Siewe, S.T.; Calle, S.; Banquart, A.; Ossant, F.; Gregoire, J.M.; Levassort, F. Properties comparison of three HF (50 MHz) single-element transducer radiation patterns with different focusing principles. In Proceedings of the IEEE International Ultrasonics Symposium (IUS), Vegas, NV, USA, 7–11 September 2020; pp. 1–4. [Google Scholar]
- Kasban, H.; El-Bendary, M.A.M.; Salama, D.H. A Comparative Study of Medical Imaging Techniques. Int. J. Inf. Sci. Intell. Syst. 2015, 4, 37–58. [Google Scholar]
- Azhari, H. Ultrasound: Medical Imaging and Beyond (An Invited Review). Curr. Pharm. Biotechnol. 2012, 13, 2104–2116. [Google Scholar] [CrossRef] [PubMed]
- Izzetti, R.; Vitali, S.; Aringhieri, G.; Nisi, M.; Oranges, T.; Dini, V.; Ferro, F.; Baldini, C.; Romanelli, M.; Caramella, D.; et al. Ultra-High Frequency Ultrasound, A Promising Diagnostic Technique: Review of the Literature and Single-Center Experience. Can. Assoc. Radiol. J. 2021, 72, 418–431. [Google Scholar] [CrossRef] [PubMed]
- Zander, D.; Hüske, S.; Hoffmann, B.; Cui, X.W.; Dong, Y.; Lim, A.; Jenssen, C.; Löwe, A.; Koch, J.B.; Dietrich, C.F. Ultrasound Image Optimization (Knobology): B-Mode. Ultrasound Int. Open 2020, 6, 14–24. [Google Scholar] [CrossRef]
- Krzysztof Mlosek, R.; Malinowska, S. Ultrasonograficzny obraz skóry, aparatura i podstawy obrazowania Ultrasound image of the skin, apparatus and imaging basics. J. Ultrason. 2013, 13, 212–221. [Google Scholar] [CrossRef]
- Silverman, R.H. High-resolution ultrasound imaging of the eye—A review. Clin. Exp. Ophthalmol. 2009, 37, 54–67. [Google Scholar] [CrossRef]
- Kagadis, G.C.; Loudos, G.; Katsanos, K.; Langer, S.G.; Nikiforidis, G.C. In vivo small animal imaging: Current status and future prospects. Med. Phys. 2010, 37, 6421–6442. [Google Scholar] [CrossRef]
- Tsiolis, F.I.; Needleman, I.G.; Griffiths, G.S. Periodontal ultrasonography. J. Clin. Periodontol. 2003, 30, 849–854. [Google Scholar] [CrossRef]
- Eger, T.; Müller, H.P.; Heinecke, A. Ultrasonic determination of gingival thickness. J. Clin. Periodontol. 1996, 23, 839–845. [Google Scholar] [CrossRef]
- Zimbran, A.; Dudea, S.; Dudea, D. Evaluation of periodontal tissues using 40MHz ultrasonography. Preliminary report. Med. Ultrason. 2013, 15, 6–9. [Google Scholar] [CrossRef] [PubMed]
- Salmon, B.; le Denmat, D. Intraoral ultrasonography: Development of a specific high-frequency probe and clinical pilot study. Clin. Oral Investig. 2011, 16, 643–649. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef]
- Chifor, R.; Badea, M.E.; Hedeşiu, M.; Şerbănescu, A.; Badea, A.F. Experimental model for measuring and characterisation of the dento-alveolar system using high frequencies ultrasound techniques. Med. Ultrason. 2010, 12, 127–132. [Google Scholar]
- Chifor, R.; HedeÅŸiu, M.; Bolfa, P.; Catoi, C.; Crisan, M.; Serbanescu, A.; Badea, A.; Moga, I.; Badea, E. The evaluation of 20 MHz ultrasonography, computed tomography scans as compared to direct microscopy for periodontal system assessment. Med. Ultrason. 2011, 13, 120–126. [Google Scholar]
- Chifor, R.; Eugenia Badea, M.; Hedeşiu, M.; Chifor, I. Identification of the anatomical elements used in periodontal diagnosis on 40 MHz periodontal ultrasonography. Rom. J. Morphol. Embryol. 2015, 56, 149–153. [Google Scholar]
- Chifor, R.; Badea, M.E.; Vesa, Ş.C.; Chifor, I. The utility of 40 MHz periodontal ultrasonography in the assessment of gingival inflammation evolution following professional teeth cleaning. Med. Ultrason. 2015, 17, 34–38. [Google Scholar] [CrossRef]
- Chifor, R.; Badea, M.E.; Mitrea, D.A.; Badea, I.C.; Crisan, M.; Chifor, I.; Avram, R. Computer-assisted identification of the gingival sulcus and periodontal epithelial junction on high-frequency ultrasound images. Med. Ultrason. 2015, 17, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, K.C.T.; Le, L.H.; Kaipatur, N.R.; Zheng, R.; Lou, E.H.; Major, P.W. High-Resolution Ultrasonic Imaging of Dento-Periodontal Tissues Using a Multi-Element Phased Array System. Ann. Biomed. Eng. 2016, 44, 2874–2886. [Google Scholar] [CrossRef]
- Chan, H.L.; Sinjab, K.; Chung, M.P.; Chiang, Y.C.; Wang, H.L.; Giannobile, W.V.; Kripfgans, O.D. Non-invasive evaluation of facial crestal bone with ultrasonography. PLoS ONE 2017, 12, e0171237. [Google Scholar] [CrossRef] [PubMed]
- Chan, H.L.; Wang, H.L.; Fowlkes, J.B.; Giannobile, W.V.; Kripfgans, O.D. Non-ionizing real-time ultrasonography in implant and oral surgery: A feasibility study. Clin. Oral Implant Res. 2017, 28, 341–347. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.Y.; Chen, F.; Hariri, A.; Chen, C.J.; Wilder-Smith, P.; Takesh, T.; Jokerst, J.V. Photoacoustic Imaging for Noninvasive Periodontal Probing Depth Measurements. J. Dent. Res. 2018, 97, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Barootchi, S.; Chan, H.L.; Namazi, S.S.; Wang, H.L.; Kripfgans, O.D. Ultrasonographic characterization of lingual structures pertinent to oral, periodontal, and implant surgery. Clin. Oral Implants Res. 2020, 31, 352–359. [Google Scholar] [CrossRef]
- Sun, M.; Yao, W.; Deng, Y.; Cao, J.; Meng, H. Measurements of buccal gingival and alveolar crest thicknesses of premolars using a noninvasive method. Med. Ultrason. 2020, 22, 409–414. [Google Scholar] [CrossRef]
- Tattan, M.; Sinjab, K.; Lee, E.; Arnett, M.; Oh, T.J.; Wang, H.L.; Chan, H.-L.; Kripfgans, O.D. Ultrasonography for chairside evaluation of periodontal structures: A pilot study. J. Periodontol. 2020, 91, 890–899. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef]

| Reference | Study Design | Study Quality | Objectives | Frequency of Ultrasound Devices | Nature of Tissues | Comparison | Main Results and Limitations |
|---|---|---|---|---|---|---|---|
| Tsiolis et al., 2003 [21] | In vitro study. N = 4, 3 posterior teeth per pig jaw, measurement repeated 2 times | Grade B* | To study high-frequency ultrasound imaging for periodontal examination | f = 20 MHz | Alveolar crest and gingival tissue | Transgingival probing, direct probing, histological comparison | The periodontal structures could be imaged. Measurements with ultrasound are precise and reproducible: less than 0.5 mm difference for all measurements with ultrasound compared to direct measurements. Possible distortion of ultrasound images providing cuts according to an Incomplete buccal-lingual section. Its need to work to have the soft tissues and the hard tissues distinctly. |
| Chifor et al., 2010 [26] | In vitro study. N = 4, 20 teeth. Measurement of the lingual mandibular part | Grade B* | Establishment of an experimental model to establish whether high-frequency ultrasound can provide relevant information about the periodontal tissues | f = 20 MHz | Alveolar and cortical bone, root surface, periodontal space width, gingival tissues | Literature regarding dento-periodontal anatomy in the domestic pig | Measurement with an accuracy of one hundredth of a millimeter. Ultrasound can be an alternative to conventional imaging. Need for a miniaturized transducer. |
| Chifor et al., 2011 [27] | In vitro study. N = 4, 20 teeth. Measurement of the lingual mandibular part | Grade B* | Identify by ultrasonography the reference points necessary to monitor the horizontal bone resorption and to assess the accuracy of the measurements | f = 20 MHz | Cemento-enamel junction, root surface, periodontal space width, alveolar and cortical bone | CBCT, direct microscopy section | Strong parametric correlation between microscopy versus US p < 0.001. Linear regression shows a statistically significant correlation between CBCT measurements and microscopy for alveolar bone p < 0.05. Usefulness in the screening and monitoring of bone resorptions. |
| Salmon et al., 2012 [24] | Clinical study. N = 3, teeth were explored on the lingual and buccal sides (162 samples) by two independent radiologists | Grade B* | Present clinical intraoral ultrasound images interpretable, to identify the relevant applications of this novel tool and to design future oral studies. Test the ergonomics of the device. | f = 25 MHz | Tooth surface, alveolar bone, gingival epithelium, sulcular space, mucogingival line, oral mucosa | NC | Periodontal tissues are visible in more than 90% of cases. The ergonomics of this device is adapted and allows a fast and comfortable measurement. |
| Zimbran et al., 2013 [23] | Clinical study. N = 4, 4 posteriors teeth of the lower jaw were imaged from buccal incidence | Grade B* | To investigate the possibility to use high-frequency ultrasound imaging for the assessment of periodontal tissues | f = 40 MHz | Alveolar bone, crown tooth, sulcular space, free gum | Clinical measure: periodontal probing, clinical crown measurement | No statistical difference between clinical measurements and ultrasound measurements |
| Chifor et al., 2015 [28] | Clinical study. N = 10, 49 teeth with marginal periodontal disease, on upper and lower pre-molars and frontal teeth, 245 measurements. | Grade B* | Identify the information for diagnosis and staging of periodontal disease using ultrasonography. | f = 40 MHz | Alveolar crest, cemento-enamel crest, free gum, root surface/gum recession, sulcular space | Clinical examination (periodontal probing) and digital periapical X-rays | All structures could be accurately imaged. Very good correlation on all US measurements versus clinical measurements with student test and correlation coefficient R. Scan time decreases as operator learns. |
| Chifor et al., 2015 [29] | Clinical study. N = 18, teeth without restorations having subgingival calculus (upper and lower premolars and frontal teeth). Measurements realized before and after periodontal treatment (J + 2 and J + 7), gingival Index and Sulcus Bleeding Index calculated. | Grade B* | To evaluate the usefulness of periodontal ultrasonography in the assessment of gingival inflammation, following professional teeth cleaning. | f = 40 MHz | Alveolar and cortical bone, enamel, cementum, cemento-enamel junction, keratinized epithelium | NC | Ultrasound measurements are accurate and repeatable (p < 0.001). Usefulness in the measurement of bone resorption and gingival inflammation. Non-invasive and efficient method requiring further studies with control groups. Requires new transducers adapted to the oral cavity. |
| Chifor et al., 2015 [30] | In vitro study. N = 8, 36 sites on lingual surfaces | Grade B* | To demonstrate that periodontal ultrasonography is a reliable method with which to identify and evaluate the attachment level of the gingival junctional epithelium. | f = 20 MHz | Enamel, root surface, sulcular space, free gum, alveolar and cortical bone | Direct microscopy | Variation between processed images and microscopy measurements between 0.06 and 1.75. Need for more clinical studies. Transducer size should be reduced. |
| Nguyen et al., 2016 [31] | In vitro study. N = 4, 2 porcine lower incisors, 6 measures per tooth. | Grade B* | To measure periodontal soft and hard tissues | f = 20 MHz | Enamel, dentine, dentin-pulp junction, cemento-enamel junction, free and attached gum, alveolar and cortical bone | CBCT | All the structures could be precisely identified with a difference of less than 10% between ultrasound versus CBCT measurements. R < 0.5 mm. The probe head is small enough to consider clinical trials on all dental sites. |
| Chan et al., 2017 [32] | Ex vivo study. N = 6, dental and periodontal tissues at the mid-facial site of each tooth on fresh cadavers (144 teeth in total) | Grade B* | To evaluate the accuracy of using ultrasound to measure facial crestal bone level and thickness | f = 14 MHz | Alveolar crest, cemento-enamel junction | CBCT, direct measurements | Correlation coefficient r > 0.80 for CBCT versus ultrasound and ultrasound versus direct measurements. Difference of measurement means: <0.1 mm. |
| Chan et al., 2017 [33] | Ex vivo study. N = 1, multiple measurements relevant to the facial bone surface and soft tissue of maxillary anterior teeth, the greater palatine foramen, the mental foramen, and the lingual nerve. | Grade B* | To investigate ultrasound to image soft tissue, hard tissue surface topography and specific vital structures. | f = 14 MHz | Distance alveolar edge–cemento-enamel junction, oral mucosal thickness, greater palatine foramen diameter and associated mucosal thickness, mental foramen diameter, lingual nerve diameter | CBCT, direct measurements, anatomical dissection | Enamel, cement-enamel junction, root surface, alveolar bone surface visible with cone of shadow behind these structures. Requires clinical studies with a larger sample. Possibility of using ultrasound for minimally invasive surgery. |
| Lin et al., 2017 [34] | In vitro study. 39 porcine teeth (12 teeth with artificially deeper pockets), 4 measures per tooth, i.e., 156 measures. | Grade B* | To investigate photoacoustic ultrasound for high–spatial resolution imaging of probing depths. Specific contrast from dental pockets was achieved with food-grade cuttlefish ink as a contrast medium. | f = 21 MHz or 40 MHz | Marginal gingiva, alveolar bone, root surface | Periodontal probing, endodontic file | Statistically significant differences between the 2 measurement approaches. The photoacoustic imaging approach also offered 0.01-mm precision and could cover the entire pocket, as opposed to the probe-based approach, which is limited to only a few sites. |
| Barootchi et al., 2020 [35] | Ex vivo study. N = 9, 3 areas in the lingual mandible (premolar, molar and retromolar). N = 19, 1 measure per patient (lingual nerve) | Grade B* | To validate ultrasound in measuring the mandibular lingual structures on human cadavers and to test its feasibility in imaging the lingual nerve in live humans | NC | Lingual mucosa, mylohyoid muscle, lingual nerve | Histological section | R correspondence (p < 0.05) between histological and ultrasound measurements. First publication demonstrating the accuracy of ultrasound for measurements at the level of anatomical structures. |
| Sun et al., 2020 [36] | In vitro study. N = 4, 6 measurements per teeth. And clinical study. N = 50, 400 premolars with healthy periodontium | Grade B* | To measure the buccal gingival thickness and alveolar crest thickness of premolars using ultrasonography and to explore the relationship between gingival thickness and alveolar crest thickness | f = 15 MHz | Alveolar bone, alveolar crest, cemento-enamel junction, gingival tissue | Periodontal probing, endodontic file | Strong correlation between ultrasound measurements (r > 0.8) and with the file on pork jawbone (p < 0.05). The gingiva at the level of the maxillary premolars and the alveolar ridge thickness are greater in men compared to women (p < 0.05). Limits: recruitment with a reduced age group with a sample that will have to be larger |
| Tattan et al., 2020 [37] | Clinical study. N = 20, 40 teeth and 20 single missing tooth gaps from 20 patients scheduled to receive a dental implant surgery | Grade B* | To evaluate the correlation and accuracy of ultrasound in measuring periodontal dimensions, compared to direct clinical and cone-beam computed tomography methods | f = 24 MHz | Interdental papilla, gingival tissue, oral gum, alveolar crest | CBCT, periodontal probing | The mean difference in mucosal thickness between the ultrasound and direct readings was −0.015 mm (95% CI: −0.655 to 0.624 mm) without statistical significance. ICC between ultrasound and CBCT ranged from 0.654 to 0.849 among the measured parameters. The mean differences between ultrasound and CBCT range from −0.213 to 0.455 mm, without statistics significance. Ultrasonic imaging can be valuable for accurate and real-time periodontal diagnosis without concerns about ionizing radiation. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Renaud, M.; Delpierre, A.; Becquet, H.; Mahalli, R.; Savard, G.; Micheneau, P.; Carayon, D.; Denis, F. Intraoral Ultrasonography for Periodontal Tissue Exploration: A Review. Diagnostics 2023, 13, 365. https://doi.org/10.3390/diagnostics13030365
Renaud M, Delpierre A, Becquet H, Mahalli R, Savard G, Micheneau P, Carayon D, Denis F. Intraoral Ultrasonography for Periodontal Tissue Exploration: A Review. Diagnostics. 2023; 13(3):365. https://doi.org/10.3390/diagnostics13030365
Chicago/Turabian StyleRenaud, Matthieu, Alexis Delpierre, Hervé Becquet, Rachid Mahalli, Guillaume Savard, Pierre Micheneau, Delphine Carayon, and Frederic Denis. 2023. "Intraoral Ultrasonography for Periodontal Tissue Exploration: A Review" Diagnostics 13, no. 3: 365. https://doi.org/10.3390/diagnostics13030365
APA StyleRenaud, M., Delpierre, A., Becquet, H., Mahalli, R., Savard, G., Micheneau, P., Carayon, D., & Denis, F. (2023). Intraoral Ultrasonography for Periodontal Tissue Exploration: A Review. Diagnostics, 13(3), 365. https://doi.org/10.3390/diagnostics13030365







