Characteristics of Pre-Lens Tear Film Behavior in Eyes Wearing Delefilcon A Silicone Hydrogel Water Gradient Contact Lenses
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Clinical Assessment
2.2.1. Assessment of Tear Volume by Video-Meniscometry
2.2.2. Assessment of PCTF and PLTF Dynamics and Stability by Video-Interferometry
2.2.3. Assessment of PLTF Dynamics and Stability by Video-Keratography
2.3. Study Protocol
2.4. Statistical Analyses
3. Results
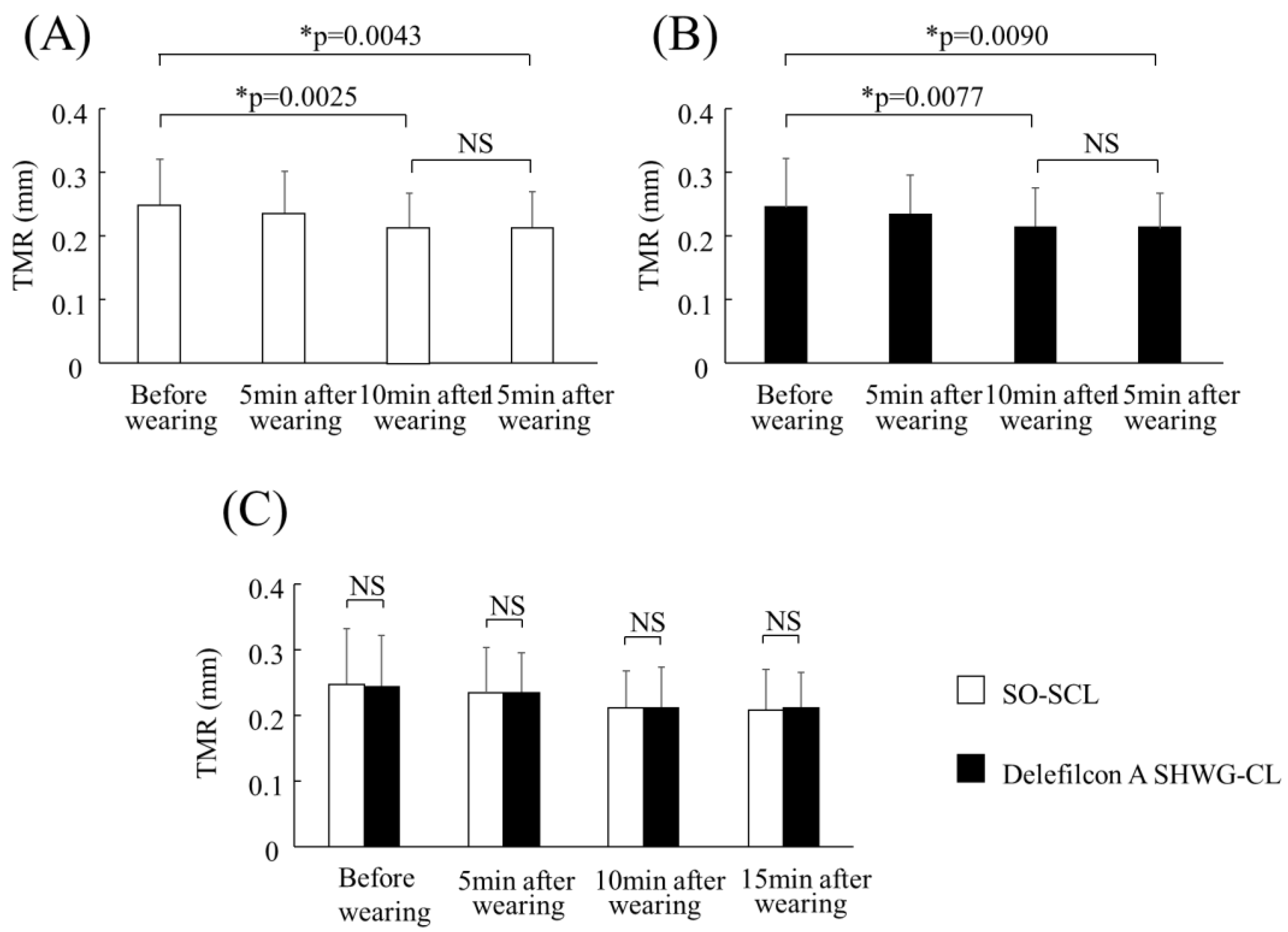
3.1. Comparison of the Time-Dependent Change in TMR
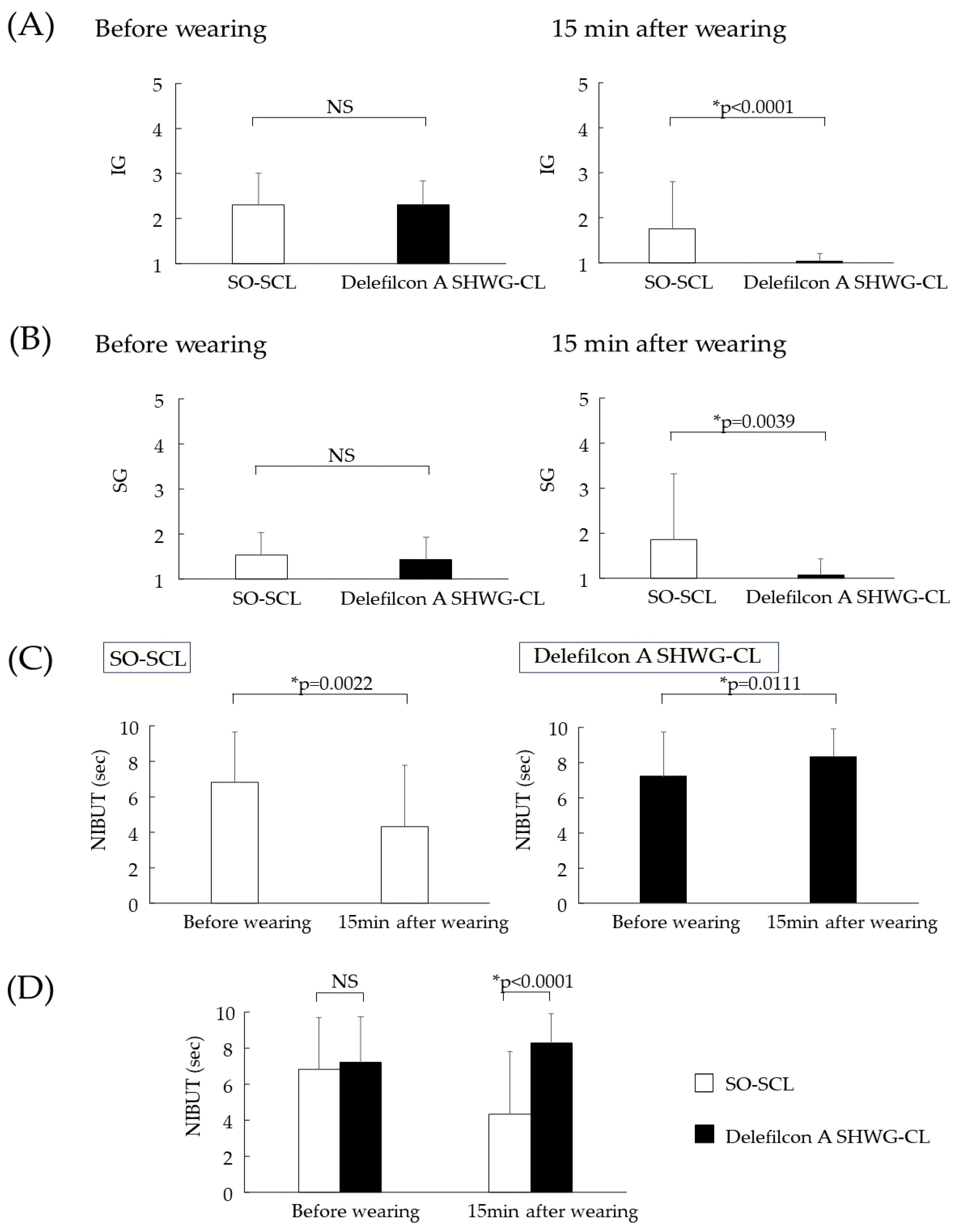
3.2. Comparison of IG, SG, and NIBUT
3.3. Comparison of TDV and IRDV
3.4. Subjective Symptoms, Fitting of the SCLs, Comfort of the Eye, and OS Damage through SCL Wear
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Markoulli, M.; Kolanu, S. Contact lens wear and dry eyes: Challenges and solutions. Clin. Optom. 2017, 9, 41–48. [Google Scholar] [CrossRef]
- Hui, A. Where have all of the contact lens wearers gone? Cont. Lens Spectrum. 2019, 34, 25–27. [Google Scholar]
- Nichols, K.K.; Redfern, R.L.; Jacob, J.T.; Nelson, J.D.; Fonn, D.; Forstot, S.L.; Huang, J.F.; Holden, B.A.; Nichols, J.J.; Members of TFOS International Workshop on Contact Lens Discomfort. The TFOS International Workshop on Contact Lens Discomfort: Report of the Definition and Classification Subcommittee. Investig. Ophthalmol. Vis. Sci. 2013, 54, TFOS14–TFOS19. [Google Scholar] [CrossRef] [PubMed]
- Yokoi, N.; Eftimov, P.; Georgiev, G.A. Dynamic aspects of pre-soft contact lens tear film and their relation to dry eye: Basic science and clinical relevance. Life 2023, 13, 859. [Google Scholar] [CrossRef]
- Nagahara, Y.; Koh, S.; Maeda, N.; Nishida, K.; Watanabe, H. Prominent decrease of tear meniscus height with contact lens wear and efficacy of eye drop instillation. Eye Contact Lens 2015, 14, 318–322. [Google Scholar] [CrossRef] [PubMed]
- Creech, J.L.; Do, L.T.; Fatt, I.; Radke, C.J. In vivo tear-film thickness determination and implications for tear-film stability. Curr. Eye Res. 1998, 17, 1058–1066. [Google Scholar] [CrossRef] [PubMed]
- King-Smith, P.E.; Fink, B.A.; Hill, R.M.; Koelling, K.W.; Tiffany, J.M. The thickness of the tear film. Curr. Eye Res. 2004, 29, 357–368. [Google Scholar] [CrossRef]
- Yokoi, N.; Georgiev, G.A.; Kato, H.; Komuro, A.; Sonomura, Y.; Sotozono, C.; Tsubota, K.; Kinoshita, S. Classification of fluorescein breakup patterns: A novel method of differential diagnosis for dry eye. Am. J. Ophthalmol. 2017, 180, 72–85. [Google Scholar] [CrossRef]
- Yokoi, N.; Georgiev, G.A. Tear film-oriented diagnosis and tear film-oriented therapy for dry eye based on tear film dynamics. Investig. Ophthalmol. Vis. Sci. 2018, 59, DES13–DES22. [Google Scholar] [CrossRef]
- Koh, S. Contact Lens Wear and Dry Eye: Beyond the Known. Asia Pac. J. Ophthalmol. 2020, 9, 498–504. [Google Scholar] [CrossRef] [PubMed]
- Yokoi, N.; Georgiev, G.A. Tear-film-oriented diagnosis for dry eye. Jpn. J. Ophthalmol. 2019, 63, 127–136. [Google Scholar] [CrossRef]
- Lin, M.C.; Svitova, T.F. Contact lenses wettability in vitro: Effect of surface-active ingredients. Optom. Vis. Sci. 2010, 87, 440–447. [Google Scholar] [CrossRef]
- Tiffany, J.M. Measurement of wettability of the corneal epithelium. II. Contact angle method. Acta. Ophthalmol. 1990, 68, 182–187. [Google Scholar] [CrossRef]
- Nichols, J.J.; Mitchell, G.L.; King-Smith, P.E. Thinning rate of the precorneal and prelens tear films. Investig. Ophthalmol. Vis. Sci. 2005, 46, 2353–2361. [Google Scholar] [CrossRef]
- Bertrand, E.; Blake, T.D.; De Coninck, J. Dynamics of dewetting. Colloids Surf. A Physicochem. Eng. Asp. 2010, 369, 141–147. [Google Scholar] [CrossRef]
- Guillon, M.; Dumbleton, K.A.; Theodoratos, P.; Wong, S.; Patel, K.; Banks, G.; Patel, T. Association Between Contact Lens Discomfort and Pre-lens Tear Film Kinetics. Optom. Vis. Sci. 2016, 93, 881–891. [Google Scholar] [CrossRef] [PubMed]
- Korb, D.R.; Greiner, J.V.; Herman, J.P.; Hebert, E.; Finnemore, V.M.; Exford, J.M.; Glonek, T.; Olson, M.C. Lid-wiper epitheliopathy and dry-eye symptoms in contact lens wearers. CLAO J. 2002, 28, 211–216. [Google Scholar] [PubMed]
- Shiraishi, A.; Yamaguchi, M.; Ohashi, Y. Prevalence of upper- and lower-lid-wiper epitheliopathy in contact lens wearers and non-wearers. Eye Contact Lens 2014, 40, 220–224. [Google Scholar] [CrossRef]
- Lakkis, C.; Brennan, N.A. Bulbar conjunctival fluorescein staining in hydrogel contact lens wearers. CLAO J. 1996, 22, 189–194. [Google Scholar] [PubMed]
- Riley, C.; Young, G.; Chalmers, R. Prevalence of ocular surface symptoms, signs, and uncomfortable hours of wear in contact lens wearers: The effect of refitting with daily-wear silicone hydrogel lenses (senofilcon A). Eye Contact Lens 2006, 32, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Bishop, M.J.; Sun, C.K.; Coles-Brennan, C.; Gallois-Bernos, A. Evaluation of daily disposable senofilcon A contact lenses in a symptomatic population. Cont. Lens Anterior Eye 2022, 45, 101574. [Google Scholar] [CrossRef]
- Eftimov, P.; Yokoi, N.; Peev, N.; Georgiev, G.A. Impact of air exposure time on the water contact angles of daily disposable silicone hydrogels. Int. J. Mol. Sci. 2019, 20, 1313. [Google Scholar] [CrossRef]
- Eftimov, P.B.; Yokoi, N.; Peev, N.; Paunski, Y.; Georgiev, G.A. Relationships between the material properties of silicone hydrogels: Desiccation, wettability and lubricity. J. Biomater. Appl. 2021, 35, 933–946. [Google Scholar] [CrossRef]
- Goto, E.; Dogru, M.; Kojima, T.; Tsubota, K. Computer-synthesis of an interference color chart of human tear lipid layer, by a colorimetric approach. Investig. Ophthalmol. Vis. Sci. 2003, 44, 4693–4697. [Google Scholar] [CrossRef]
- Goto, E.; Tseng, S.C. Differentiation of lipid tear deficiency dry eye by kinetic analysis of tear interference images. Arch. Ophthalmol. 2003, 121, 173–180. [Google Scholar] [CrossRef]
- Yokoi, N.; Kusada, N.; Kato, H.; Furusawa, Y.; Sotozono, C.; Georgiev, G.A. Successful Detection of the Characteristics of Tear Film Breakup Appearing Immediately after Eye Opening by Videokeratography with a Newly-Developed Indicator. Diagnostics 2023, 13, 240. [Google Scholar] [CrossRef]
- Kusada, N.; Yokoi, N.; Kato, H.; Furusawa, Y.; Sakai, R.; Sotozono, C. Evaluation of Dry Eye With Videokeratographer Using a Newly Developed Indicator. Am. J. Ophthalmol. 2023, 252, 135–146. [Google Scholar] [CrossRef] [PubMed]
- Nelson, J.D.; Shimazaki, J.; Benitez-del-Castillo, J.M.; Craig, J.P.; McCulley, J.P.; Den, S.; Foulks, G.N. The international workshop on meibomian gland dysfunction: Report of the definition and classification subcommittee. Investig. Ophthalmol. Vis. Sci. 2011, 52, 1930–1937. [Google Scholar] [CrossRef] [PubMed]
- Bandlitz, S.; Purslow, C.; Murphy, P.J.; Pult, H.; Bron, A.J. A new portable digital meniscometer. Optom. Vis. Sci. 2014, 91, e1–e8. [Google Scholar] [CrossRef] [PubMed]
- Kojima, T.; Dogru, M.; Kawashima, M.; Nakamura, S.; Tsubota, K. Advances in the diagnosis and treatment of dry eye. Prog. Retin. Eye Res. 2020, 29, 100842. [Google Scholar] [CrossRef]
- Hosaka, E.; Kawamorita, T.; Ogasawara, Y.; Nakayama, N.; Uozato, H.; Shimizu, K.; Dogru, M.; Tsubota, K.; Goto, E. Interferometry in the evaluation of precorneal tear film thickness in dry eye. Am. J. Ophthalmol. 2010, 151, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Xie, W.J.; Xu, Y.S.; Zhang, X.; Yao, Y.F. Assessments of tear meniscus height, tear film thickness, and corneal epithelial thickness after deep anterior lamellar keratoplasty. J. Zhejiang Univ. Sci. B. 2018, 19, 218–226. [Google Scholar] [CrossRef] [PubMed]
- Shen, M.; Li, J.; Wang, J.; Ma, H.; Cai, C.; Tao, A.; Yuan, Y.; Lu, F. Upper and lower tear menisci in the diagnosis of dry eye. Investig. Ophthalmol. Vis. Sci. 2009, 50, 2722–2726. [Google Scholar] [CrossRef]
- Golding, T.R.; Bruce, A.S.; Mainstone, J.C. Relationship between tear-meniscus parameters and tear-film breakup. Cornea 1997, 16, 649–661. [Google Scholar] [CrossRef]
- Nguyen, P.; Huang, D.; Li, Y.; Sadda, S.R.; Ramos, S.; Pappuru, R.R.; Yiu, S.C. Correlation between optical coherence tomography-derived assessments of lower tear meniscus parameters and clinical features of dry eye disease. Cornea 2012, 31, 680–685. [Google Scholar] [CrossRef] [PubMed]
- Kojima, T. Contact Lens-Associated Dry Eye Disease: Recent Advances Worldwide and in Japan. Investig. Ophthalmol. Vis. Sci. 2018, 59, DES102–DES108. [Google Scholar] [CrossRef]
- Goto, E.; Dogru, M.; Kojima, T.; Suzuki, S.; Ishida, R.; Honda, R.; Tsubota, K. Color mapping of tear lipid layer thickness distribution from the image analysis in DR–1 tear lipid layer interference images. Investig. Ophthalmol. Vis. Sci. 2004, 45, 3458. [Google Scholar]
- Yokoi, N.; Yamada, H.; Mizukasa, Y.; Bron, A.J.; Tiffany, J.M.; Kato, T.; Kinoshita, S. Rheology of tear film lipid layer spread in normal and aqueous tear-deficient dry eyes. Investig. Ophthalmol. Vis. Sci. 2008, 49, 5319–5324. [Google Scholar] [CrossRef]
- Komuro, A.; Yokoi, N.; Kato, H.; Sonomura, Y.; Sotozono, C. A simple and useful clinical method for evaluating the severity of dry eye. Investig. Ophthalmol. Vis. Sci. 2019, 60, 6787. [Google Scholar]
- Staff, R.O. Lipid Layer Spread Can Indicate Dry Eye Severity. Review of Optometry. Available online: https://www.reviewofoptometry.com/article/lipid-layer-spread-can-indicate-dry-eye-severity (accessed on 25 November 2023).
- Pruitt, J.; Qiu, Y.; Thekveli, S.; Hart, R. Surface characterization of a water gradient silicone hydrogel contact lens (delefilcon A). Investig. Ophthalmol. Vis. Sci. 2012, 53, 6107. [Google Scholar]
- Fujimoto, H.; Ochi, S.; Yamashita, T.; Inoue, Y.; Kiryu, J. Role of the water gradient structure in inhibiting thin aqueous layer break in silicone hydrogel-soft contact lens. Transl. Vis. Sci. Technol. 2021, 10, 5. [Google Scholar] [CrossRef] [PubMed]
- King-Smith, P.E.; Fink, B.A.; Nichols, J.J.; Nichols, K.K.; Braun, R.J.; McFadden, G.B. The contribution of lipid layer movement to tear film thinning and breakup. Investig. Ophthalmol. Vis. Sci. 2009, 50, 2747–2756. [Google Scholar] [CrossRef]
- Goto, E.; Tseng, S.C.G. Kinetic analysis of tear interference images in aqueous tear deficiency dry eye before and after punctal occlusion. Investig. Ophthalmol. Vis. Sci. 2003, 44, 1897–1905. [Google Scholar] [CrossRef]
- Owens, H.; Phillips, J. Spreading of the tears after a blink: Velocity and stabilization time in healthy eyes. Cornea 2001, 20, 484–487. [Google Scholar] [CrossRef]
- Redon, C.; Brochard-Wyart, F.; Rondelez, F. Dynamics of dewetting. Phys. Rev. Lett. 1991, 66, 715–718. [Google Scholar] [CrossRef] [PubMed]
- Varikooty, J.; Schulze, M.M.; Dumbleton, K.; Keir, N.; Woods, C.A.; Fonn, D.; Jones, L.W. Clinical performance of three silicone hydrogel daily disposable lenses. Optom. Vis. Sci. 2015, 92, 301–311. [Google Scholar] [CrossRef] [PubMed]
- Itokawa, T.; Okajima, Y.; Suzuki, T.; Koji Kakisu, K.; Iwashita, H.; Murakami, Y.; Hori, Y. Association Between Ocular Surface Temperature and Tear Film Stability in Soft Contact Lens Wearers. Investig. Ophthalmol. Vis. Sci. 2018, 59, 771–775. [Google Scholar] [CrossRef] [PubMed]
- Wolffsohn, J.S.; Mroczkowska, S.; Hunt, O.A.; Bilkhu, P.; Drew, T.; Sheppard, A. Crossover Evaluation of Silicone Hydrogel Daily Disposable Contact Lenses. Optom. Vis. Sci. 2015, 92, 1063–1068. [Google Scholar] [CrossRef]
- Capote-Puente, R.; Sánchez-González, J.M.; Sánchez-González, M.C.; Bautista-Llamas, M.J. Evaluation of Celligent® biomimetic water gradient contact lens effects on ocular surface and subjective symptoms. Diagnostics 2023, 13, 1258. [Google Scholar] [CrossRef]

| Groups | Characteristics | Number of Subjects |
|---|---|---|
| Group I | NI/LWC | 1 |
| Group II | NI/HWC | 4 |
| Group III | I/LWC | 0 |
| Group IV | I/HWC | 11 |
| Group V-A | I/NWC | 0 |
| Group V-B | NI/HWC | 0 |
| Group V-Cm | NI/LWC, ST | 2 |
| Group V-C | NI/LWC, ST/HM | 1 |
| Group V-Cr | NI/LWC, Non-ST/SIN | 11 |
| SO-SCL | Delefilcon A SHWG-CL | |||
|---|---|---|---|---|
| Grade | before Lens Wear | 15 min after Lens Wear | before Lens Wear | 15 min after Lens Wear |
| IG | ||||
| 1 | 2 | 15 | 0 | 29 |
| 2 | 19 | 11 | 22 | 1 |
| 3 | 7 | 1 | 7 | 0 |
| 4 | 2 | 2 | 1 | 0 |
| 5 | 0 | 1 | 0 | 0 |
| mean ± SD | 2.3 ± 0.7 | 1.8 ± 1.0 | 2.3 ± 0.5 | 1.0 ± 0.2 |
| SG | ||||
| 1 | 14 | 21 | 17 | 29 |
| 2 | 16 | 1 | 13 | 0 |
| 3 | 0 | 2 | 0 | 1 |
| 4 | 0 | 3 | 0 | 0 |
| 5 | 0 | 3 | 0 | 0 |
| mean ± SD | 1.5 ± 0.5 | 1.9 ± 1.5 | 1.4 ± 0.5 | 1.1 ± 0.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yokoi, N.; Furusawa, Y.; Kato, H.; Kusada, N.; Sotozono, C.; Eftimov, P.; Georgiev, G.A. Characteristics of Pre-Lens Tear Film Behavior in Eyes Wearing Delefilcon A Silicone Hydrogel Water Gradient Contact Lenses. Diagnostics 2023, 13, 3642. https://doi.org/10.3390/diagnostics13243642
Yokoi N, Furusawa Y, Kato H, Kusada N, Sotozono C, Eftimov P, Georgiev GA. Characteristics of Pre-Lens Tear Film Behavior in Eyes Wearing Delefilcon A Silicone Hydrogel Water Gradient Contact Lenses. Diagnostics. 2023; 13(24):3642. https://doi.org/10.3390/diagnostics13243642
Chicago/Turabian StyleYokoi, Norihiko, Yuki Furusawa, Hiroaki Kato, Natsuki Kusada, Chie Sotozono, Petar Eftimov, and Georgi As. Georgiev. 2023. "Characteristics of Pre-Lens Tear Film Behavior in Eyes Wearing Delefilcon A Silicone Hydrogel Water Gradient Contact Lenses" Diagnostics 13, no. 24: 3642. https://doi.org/10.3390/diagnostics13243642
APA StyleYokoi, N., Furusawa, Y., Kato, H., Kusada, N., Sotozono, C., Eftimov, P., & Georgiev, G. A. (2023). Characteristics of Pre-Lens Tear Film Behavior in Eyes Wearing Delefilcon A Silicone Hydrogel Water Gradient Contact Lenses. Diagnostics, 13(24), 3642. https://doi.org/10.3390/diagnostics13243642








