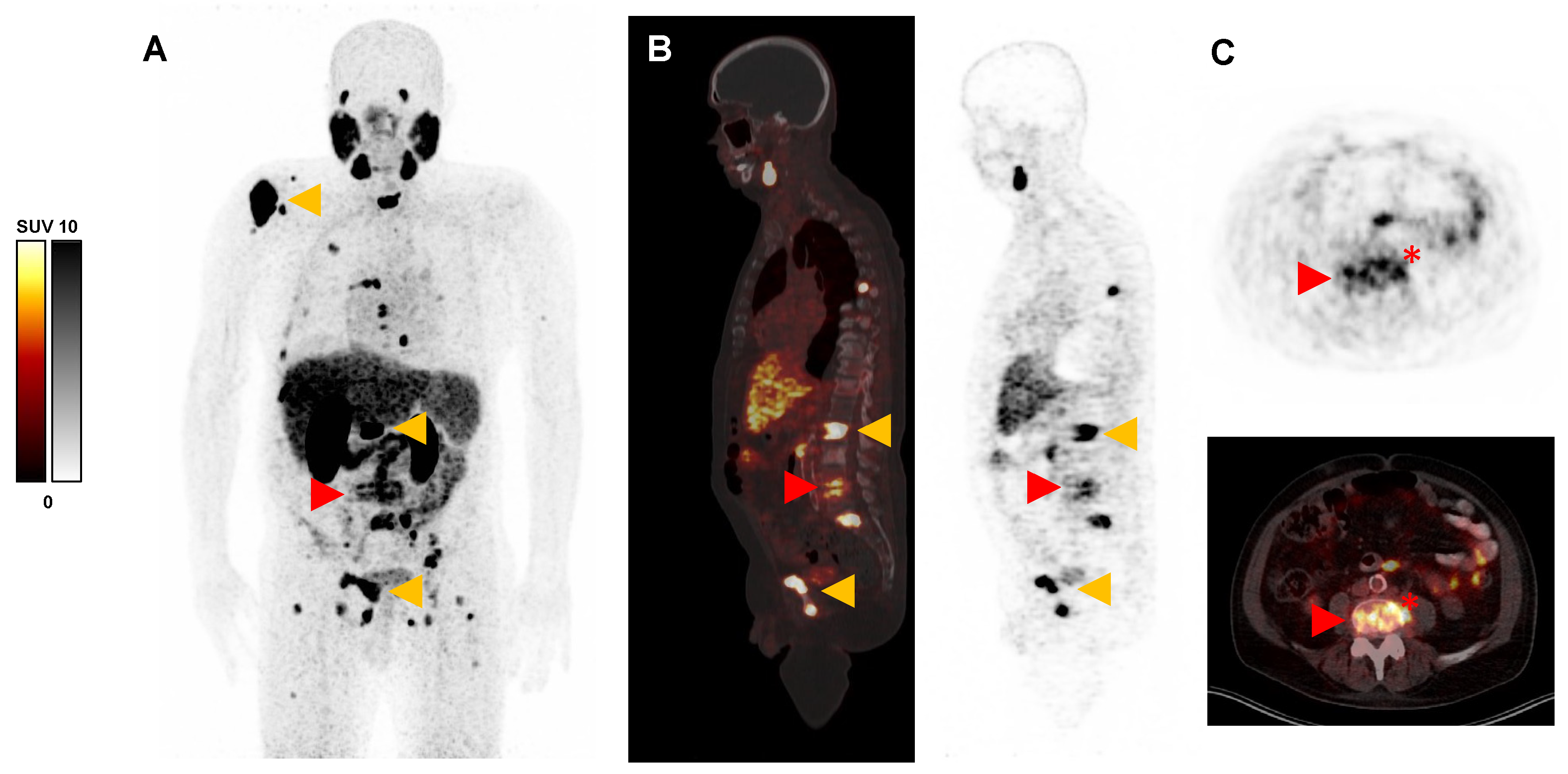
Active Lumbar Spondylodiscitis on [68Ga]Ga-PSMA-11 PET/CT Mimicking Bone Metastasis
Abstract
:
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zimmerli, W. Clinical practice. Vertebral osteomyelitis. N. Engl. J. Med. 2010, 362, 1022–1029. [Google Scholar] [CrossRef] [PubMed]
- Gouliouris, T.; Aliyu, S.H.; Brown, N.M. Spondylodiscitis: Update on diagnosis and management. J. Antimicrob. Chemother. 2010, 65, iii11–iii24. [Google Scholar] [CrossRef] [PubMed]
- Kouijzer, I.J.E.; Scheper, H.; de Rooy, J.W.J.; Bloem, J.L.; Janssen, M.J.R.; Hoven, L.v.D.; Hosman, A.J.F.; Visser, L.G.; Oyen, W.J.G.; Bleeker-Rovers, C.P.; et al. The diagnostic value of 18F-FDG-PET/CT and MRI in suspected vertebral osteomyelitis—A prospective study. Eur. J. Nucl. Med. Mol. Imaging 2018, 45, 798–805. [Google Scholar] [CrossRef] [PubMed]
- Prodromou, M.L.; Ziakas, P.D.; Poulou, L.S.; Karsaliakos, P.; Thanos, L.; Mylonakis, E. FDG PET is a robust tool for the diagnosis of spondylodiscitis: A meta-analysis of diagnostic data. Clin. Nucl. Med. 2014, 39, 330–335. [Google Scholar] [CrossRef] [PubMed]
- Smids, C.; Kouijzer, I.J.E.; Vos, F.J.; Sprong, T.; Hosman, A.J.F.; de Rooy, J.W.J.; Aarntzen, E.H.J.G.; de Geus-Oei, L.-F.; Oyen, W.J.G.; Bleeker-Rovers, C.P. A comparison of the diagnostic value of MRI and 18F-FDG-PET/CT in suspected spondylodiscitis. Infection 2017, 45, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Klingenberg, S.; Jochumsen, M.R.; Pedersen, B.G.; Bouchelouche, K. 68Ga-PSMA Uptake in Escherichia coli Spondylodiscitis. Clin. Nucl. Med. 2019, 44, 916–919. [Google Scholar] [CrossRef] [PubMed]
- Gupta, N.; Elumalai, R.K.; Verma, R.; Belho, E.S.; Dhawan, S. Spinal Tuberculosis Mimicking as Prostate Cancer Metastases in Ga-68 Prostate-specific Membrane Antigen Positron-emission Tomography/Computed Tomography. Indian J. Nucl. Med. 2020, 35, 271–273. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, F.d.G.; Queiroz, M.A.; Nunes, R.F.; Costa, L.B.; Zaniboni, E.C.; Marin, J.F.G.; Cerri, G.G.; Buchpiguel, C.A. Nonprostatic diseases on PSMA PET imaging: A spectrum of benign and malignant findings. Cancer Imaging 2020, 20, 23. [Google Scholar] [CrossRef] [PubMed]
- Malan, N.; Vangu, M.-T. Normal Variants, Pitfalls, and Artifacts in Ga-68 Prostate Specific Membrane Antigen (PSMA) PET/CT Imaging. Front. Nucl. Med. 2022, 2, 825512. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rosar, F.; Burgard, C.; Gargiulo, R.; Ezziddin, S. Active Lumbar Spondylodiscitis on [68Ga]Ga-PSMA-11 PET/CT Mimicking Bone Metastasis. Diagnostics 2023, 13, 3616. https://doi.org/10.3390/diagnostics13243616
Rosar F, Burgard C, Gargiulo R, Ezziddin S. Active Lumbar Spondylodiscitis on [68Ga]Ga-PSMA-11 PET/CT Mimicking Bone Metastasis. Diagnostics. 2023; 13(24):3616. https://doi.org/10.3390/diagnostics13243616
Chicago/Turabian StyleRosar, Florian, Caroline Burgard, Raffaele Gargiulo, and Samer Ezziddin. 2023. "Active Lumbar Spondylodiscitis on [68Ga]Ga-PSMA-11 PET/CT Mimicking Bone Metastasis" Diagnostics 13, no. 24: 3616. https://doi.org/10.3390/diagnostics13243616
APA StyleRosar, F., Burgard, C., Gargiulo, R., & Ezziddin, S. (2023). Active Lumbar Spondylodiscitis on [68Ga]Ga-PSMA-11 PET/CT Mimicking Bone Metastasis. Diagnostics, 13(24), 3616. https://doi.org/10.3390/diagnostics13243616






