Association of Late Radiographic Assessment of Lung Edema Score with Clinical Outcome in Patients with Influenza-Associated Acute Respiratory Distress Syndrome
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Selection
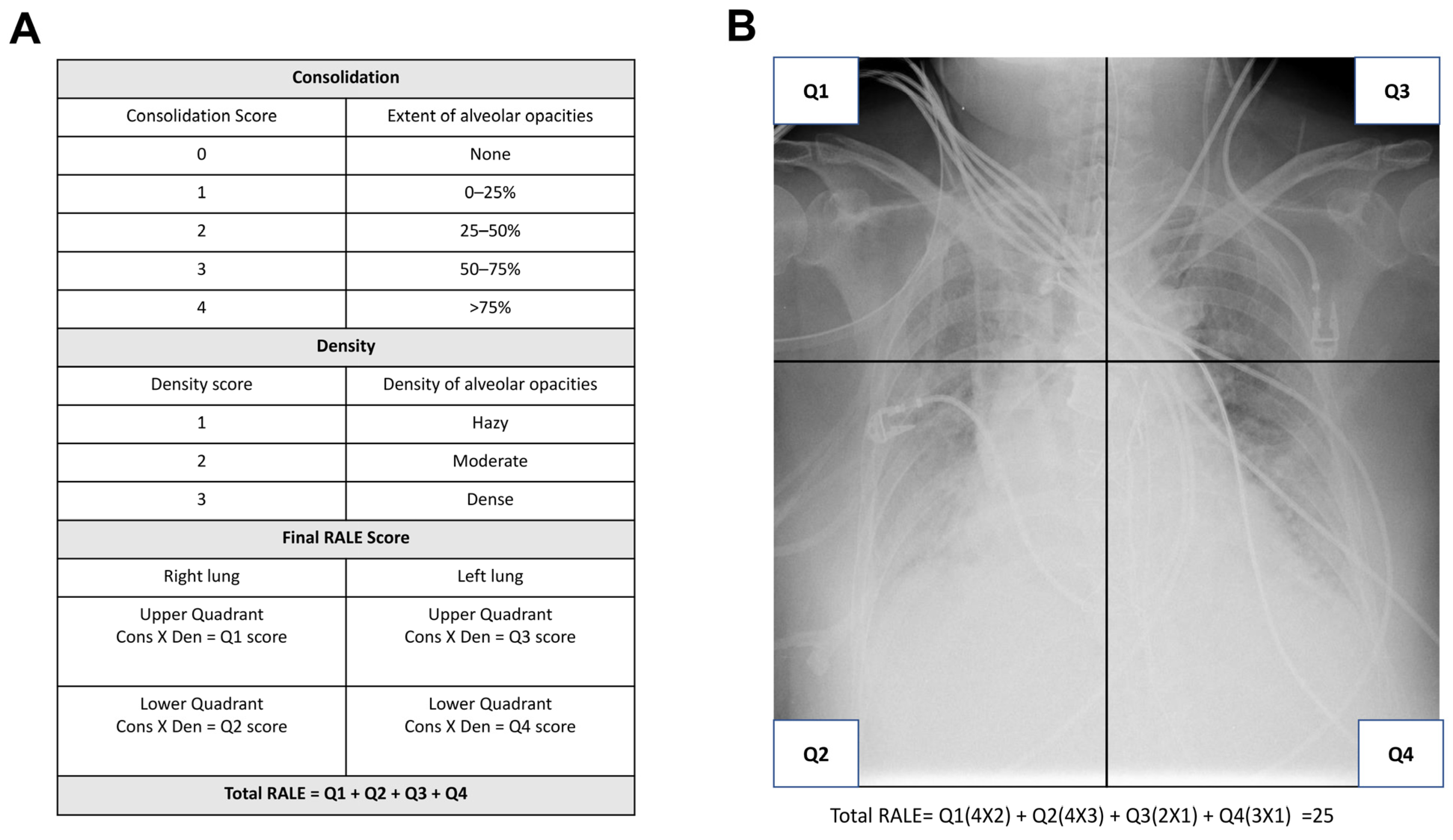
2.2. Definitions of ARDS and RALE Score
2.3. Data Collection and Severity Evaluation
2.4. Outcome Evaluation
2.5. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Demographic and Baseline Clinical Data
3.3. Interobserver Agreement for RALE Scores
3.4. Clinical Complications and Hospital Outcomes
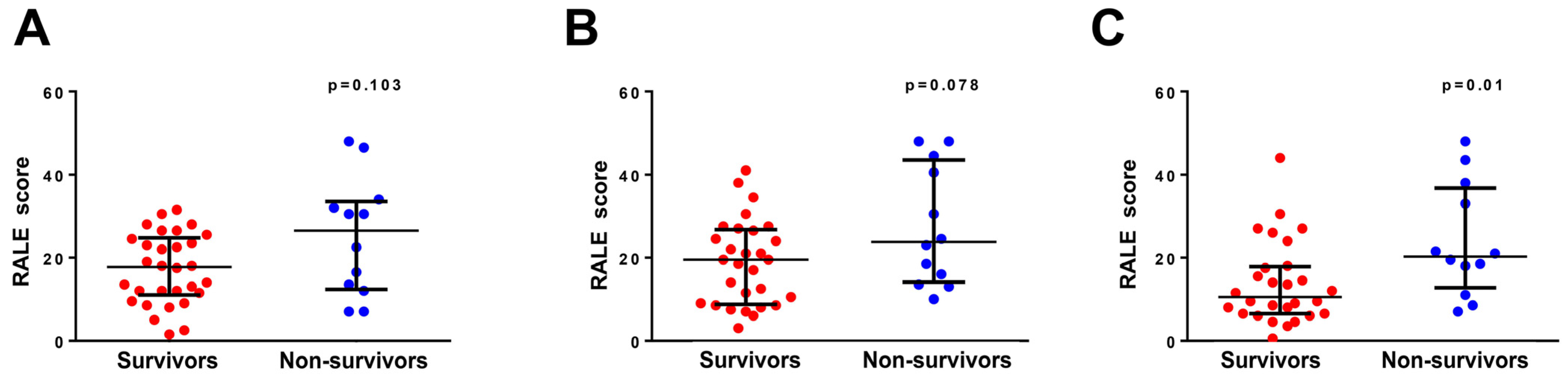
3.5. RALE Score and Survival
3.6. Independent Predicting Factor for In-Hospital Mortality
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A

Appendix B
| aOR (95% CI) | p Value | |
|---|---|---|
| Initial SOFA | 1.082 (0.822–1.423) | 0.576 |
| Vasopressors | 3.004 (0.465–19.424) | 0.248 |
| Bacteremia | 2.771 (0.287–26.786) | 0.379 |
| APACHE II | 1.010 (0.865–1.178) | 0.903 |
| PSI | 1.009 (0.980–1.038) | 0.543 |
| Day 0 RALE | 1.045 (0.954–1.145) | 0.340 |
| aOR (95% CI) | p Value | |
|---|---|---|
| Initial SOFA | 1.090 (0.833–1.427) | 0.529 |
| Vasopressors | 2.218 (0.261–18.863) | 0.466 |
| Bacteremia | 3.249 (0.303–34.886) | 0.330 |
| APACHE II | 0.998 (0.850–1.173) | 0.985 |
| PSI | 1.012 (0.982–1.044) | 0.432 |
| Day 2 RALE | 1.043 (0.955–1.139) | 0.352 |
References
- Krammer, F.; Smith, G.J.D.; Fouchier, R.A.M.; Peiris, M. Influenza. Nat. Rev. Dis. Primers 2018, 4, 3. [Google Scholar] [CrossRef] [PubMed]
- Fiers, W.; De Filette, M.; Birkett, A.; Neirynck, S.; Jou, W.M. A “universal” human influenza A vaccine. Virus Res. 2004, 103, 173–176. [Google Scholar] [CrossRef] [PubMed]
- Brundage, J.F.; Shanks, G.D. Deaths from bacterial pneumonia during 1918-19 influenza pandemic. Emerg. Infect. Dis. 2008, 14, 1193–1199. [Google Scholar] [CrossRef] [PubMed]
- Ramsey, C.; Kumar, A. H1N1: Viral pneumonia as a cause of acute respiratory distress syndrome. Curr. Opin. Crit. Care 2011, 17, 64–71. [Google Scholar] [CrossRef]
- Salazar, F.; Bignell, E.; Brown, G.D.; Cook, P.C.; Warris, A. Pathogenesis of respiratory viral and fungal coinfections. Clin. Microbiol. Rev. 2022, 35, e0009421. [Google Scholar] [CrossRef]
- Goka, E.; Vallely, P.; Mutton, K.; Klapper, P. Influenza A viruses dual and multiple infections with other respiratory viruses and risk of hospitalisation and mortality. Influenza Other Respir. Viruses 2013, 7, 1079–1087. [Google Scholar] [CrossRef]
- ARDS Definition Task Force; Ranieri, V.M.; Rubenfeld, G.D.; Thompson, B.T.; Ferguson, N.D.; Caldwell, E.; Fan, E.; Camporota, L.; Slutsky, A.S. Acute respiratory distress syndrome: The Berlin Definition. JAMA 2012, 307, 2526–2533. [Google Scholar]
- Matthay, M.A.; Ware, L.B.; Zimmerman, G.A. The acute respiratory distress syndrome. J. Clin. Investig. 2012, 122, 2731–2740. [Google Scholar] [CrossRef]
- Warren, M.A.; Zhao, Z.; Koyama, T.; Bastarache, J.A.; Shaver, C.M.; Semler, M.W.; Rice, T.W.; Matthay, M.A.; Calfee, C.S.; Ware, L.B. Severity scoring of lung oedema on the chest radiograph is associated with clinical outcomes in ARDS. Thorax 2018, 73, 840–846. [Google Scholar] [CrossRef]
- Jabaudon, M.; Audard, J.; Pereira, B.; Jaber, S.; Lefrant, J.Y.; Blondonnet, R.; Godet, T.; Futier, E.; Lambert, C.; Bazin, J.E.; et al. Early changes over time in the radiographic assessment of lung edema score are associated with survival in ARDS. Chest 2020, 158, 2394–2403. [Google Scholar] [CrossRef]
- Kotok, D.; Yang, L.; Evankovich, J.W.; Bain, W.; Dunlap, D.G.; Shah, F.; Zhang, Y.; Manatakis, D.V.; Benos, P.V.; Barbash, I.J.; et al. The evolution of radiographic edema in ARDS and its association with clinical outcomes: A prospective cohort study in adult patients. J. Crit. Care 2020, 56, 222–228. [Google Scholar] [CrossRef] [PubMed]
- Todur, P.; Srikant, N.; Prakash, P. Correlation of oxygenation and radiographic assessment of lung edema (RALE) score to lung ultrasound score (LUS) in acute respiratory distress syndrome (ARDS) patients in the intensive care unit. Can. J. Respir. Ther. 2021, 57, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Al-Yousif, N.; Komanduri, S.; Qurashi, H.; Korzhuk, A.; Lawal, H.O.; Abourizk, N.; Schaefer, C.; Mitchell, K.J.; Dietz, C.M.; Hughes, E.K.; et al. Radiographic assessment of lung edema (RALE) scores are highly reproducible and prognostic of clinical outcomes for inpatients with COVID-19. medRxiv 2022. [Google Scholar] [CrossRef]
- Taniguchi, H.; Ohya, A.; Yamagata, H.; Iwashita, M.; Abe, T.; Takeuchi, I. Prolonged mechanical ventilation in patients with severe COVID-19 is associated with serial modified-lung ultrasound scores: A single-centre cohort study. PLoS ONE 2022, 17, e0271391. [Google Scholar] [CrossRef] [PubMed]
- Zimatore, C.; Pisani, L.; Lippolis, V.; Warren, M.A.; Calfee, C.S.; Ware, L.B.; Algera, A.G.; Smit, M.R.; Grasso, S.; Schultz, M.J. Accuracy of the radiographic assessment of lung edema score for the siagnosis of ARDS. Front. Physiol. 2021, 12, 672823. [Google Scholar] [CrossRef]
- Voigt, I.; Mighali, M.; Manda, D.; Aurich, P.; Bruder, O. Radiographic assessment of lung edema (RALE) score is associated with clinical outcomes in patients with refractory cardiogenic shock and refractory cardiac arrest after percutaneous implantation of extracorporeal life support. Intern. Emerg. Med. 2022, 17, 1463–1470. [Google Scholar] [CrossRef]
- Valk, C.M.A.; Zimatore, C.; Mazzinari, G.; Pierrakos, C.; Sivakorn, C.; Dechsanga, J.; Grasso, S.; Beenen, L.; Bos, L.D.J.; Paulus, F.; et al. The prognostic capacity of the radiographic assessment for lung edema score in patients with COVID-19 acute respiratory distress syndrome-An international multicenter observational study. Front. Med. 2021, 8, 772056. [Google Scholar] [CrossRef]
- Short, K.R.; Kroeze, E.; Fouchier, R.A.M.; Kuiken, T. Pathogenesis of influenza-induced acute respiratory distress syndrome. Lancet Infect. Dis. 2014, 14, 57–69. [Google Scholar] [CrossRef]
- Kalil, A.C.; Thomas, P.G. Influenza virus-related critical illness: Pathophysiology and epidemiology. Crit. Care 2019, 23, 258. [Google Scholar] [CrossRef]
- Vijayanand, P.; Wilkins, E.; Woodhead, M. Severe acute respiratory syndrome (SARS): A review. Clin. Med. 2004, 4, 152–160. [Google Scholar] [CrossRef]
- Arabi, Y.M.; Balkhy, H.H.; Hayden, F.G.; Bouchama, A.; Luke, T.; Baillie, J.K.; Al-Omari, A.; Hajeer, A.H.; Senga, M.; Denison, M.R.; et al. Middle East Respiratory Syndrome. N. Engl. J. Med. 2017, 376, 584–594. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Guo, J.; Wang, C.; Luo, F.; Yu, X.; Zhang, W.; Li, J.; Zhao, D.; Xu, D.; Gong, Q.; et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: A retrospective review of medical records. Lancet 2020, 395, 809–815. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Xie, Y.; Pang, G.; Liao, Z.; Verjans, J.; Li, W.; Sun, Z.; He, J.; Li, Y.; Shen, C.; et al. Viral Pneumonia Screening on Chest X-rays Using Confidence-Aware Anomaly Detection. IEEE Trans. Med. Imaging 2021, 40, 879–890. [Google Scholar] [CrossRef] [PubMed]

| Survivors (n = 30) | Non-Survivors (n = 12) | p Value | |
|---|---|---|---|
| Age (years) | 65 [55–80] | 65 [56–81] | 0.933 |
| Male sex | 22 (73) | 10 (83) | 0.492 |
| BMI (kg/m2) | 23 [21–27] | 24 [21–27] | 0.933 |
| Comorbidities | |||
| Diabetes mellitus | 12 (40) | 5 (42) | 0.921 |
| Cardiovascular disease | 19 (63) | 6 (50) | 0.426 |
| Chronic kidney disease | 4 (13) | 1 (8) | 0.651 |
| At ICU admission | |||
| WBC (103/mm3) | 8.4 [6.9–14.0] | 7.6 [5.1–11.5] | 0.411 |
| Albumin (g/dL) | 2.9 [2.4–3.1] | 2.6 [2.4–2.8] | 0.228 |
| CRP (mg/dL) | 21.4 [6.3–30.0] | 12.3 [8.2–15.0] | 0.344 |
| Lactate (mg/dL) | 13.8 [8.2–19.8] | 14.7 [10.6–20.4] | 0.616 |
| Creatine kinase (U/L) | 144.0 [67.0–484.5] | 186.5 [49.0–313.0] | 0.954 |
| ALT (IU/L) | 28.5 [17.4–40.3] | 42.0 [20.3–90.8] | 0.200 |
| Severity | |||
| CURB-65 | 3.0 [1.0–4.0] | 2.5 [2.0–3.8] | 0.830 |
| PSI | 114.5 [97.0–148.8] | 126.0 [124.0–144.8] | 0.140 |
| SOFA | 7.0 [4.0–8.0] | 7.5 [6.3–12.8] | 0.049 |
| APACHEII | 20.5 [15.0–29.3] | 25.5 [20.5–30.0] | 0.112 |
| RALE score | |||
| Day 0 | 17.8 [11.0–24.8] | 26.5 [12.4–33.5] | 0.103 |
| Day 2 | 19.5 [8.8–26.8] | 23.8 [14.1–43.5] | 0.078 |
| Day 7 | 9.5 [6.3–17.8] | 20.3 [12.8–36.8] | 0.010 |
| Survivors (n = 30) | Non-Survivors (n = 12) | p Value | |
|---|---|---|---|
| Complications | |||
| Bacteremia | 2 (7) | 1 (33) | 0.026 |
| Treatments | |||
| IMV | 27 (90) | 12 (100) | 0.256 |
| Corticosteroid use | 16 (53) | 8 (67) | 0.430 |
| Vasopressors use | 10 (33) | 9 (75) | 0.014 |
| Outcomes | |||
| ICU days | 18 [9–22] | 26 [16–38] | 0.062 |
| Hospitalization days | 28 [16–55] | 30 [18–48] | 0.944 |
| IMV days | 16 [11–31] | 18 [12–38] | 0.503 |
| aOR (95% CI) | p Value | |
|---|---|---|
| Initial SOFA | 1.068 (0.795–1.435) | 0.660 |
| Vasopressors | 1.606 (0.205–12.573) | 0.652 |
| Bacteremia | 9.669 (0.587–159.133) | 0.112 |
| APACHE II | 0.974 (0.831–1.143) | 0.750 |
| PSI | 1.027 (0.991–1.065) | 0.144 |
| Day 7 RALE | 1.121 (1.014–1.240) | 0.025 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shen, H.-C.; Chen, C.-C.; Chen, W.-C.; Yu, W.-K.; Yang, K.-Y.; Chen, Y.-M. Association of Late Radiographic Assessment of Lung Edema Score with Clinical Outcome in Patients with Influenza-Associated Acute Respiratory Distress Syndrome. Diagnostics 2023, 13, 3572. https://doi.org/10.3390/diagnostics13233572
Shen H-C, Chen C-C, Chen W-C, Yu W-K, Yang K-Y, Chen Y-M. Association of Late Radiographic Assessment of Lung Edema Score with Clinical Outcome in Patients with Influenza-Associated Acute Respiratory Distress Syndrome. Diagnostics. 2023; 13(23):3572. https://doi.org/10.3390/diagnostics13233572
Chicago/Turabian StyleShen, Hsiao-Chin, Chun-Chia Chen, Wei-Chih Chen, Wen-Kuang Yu, Kuang-Yao Yang, and Yuh-Min Chen. 2023. "Association of Late Radiographic Assessment of Lung Edema Score with Clinical Outcome in Patients with Influenza-Associated Acute Respiratory Distress Syndrome" Diagnostics 13, no. 23: 3572. https://doi.org/10.3390/diagnostics13233572
APA StyleShen, H.-C., Chen, C.-C., Chen, W.-C., Yu, W.-K., Yang, K.-Y., & Chen, Y.-M. (2023). Association of Late Radiographic Assessment of Lung Edema Score with Clinical Outcome in Patients with Influenza-Associated Acute Respiratory Distress Syndrome. Diagnostics, 13(23), 3572. https://doi.org/10.3390/diagnostics13233572







