The Role of CRP POC Testing in the Fight against Antibiotic Overuse in European Primary Care: Recommendations from a European Expert Panel
Abstract
1. Introduction
2. Materials and Methods
3. Results
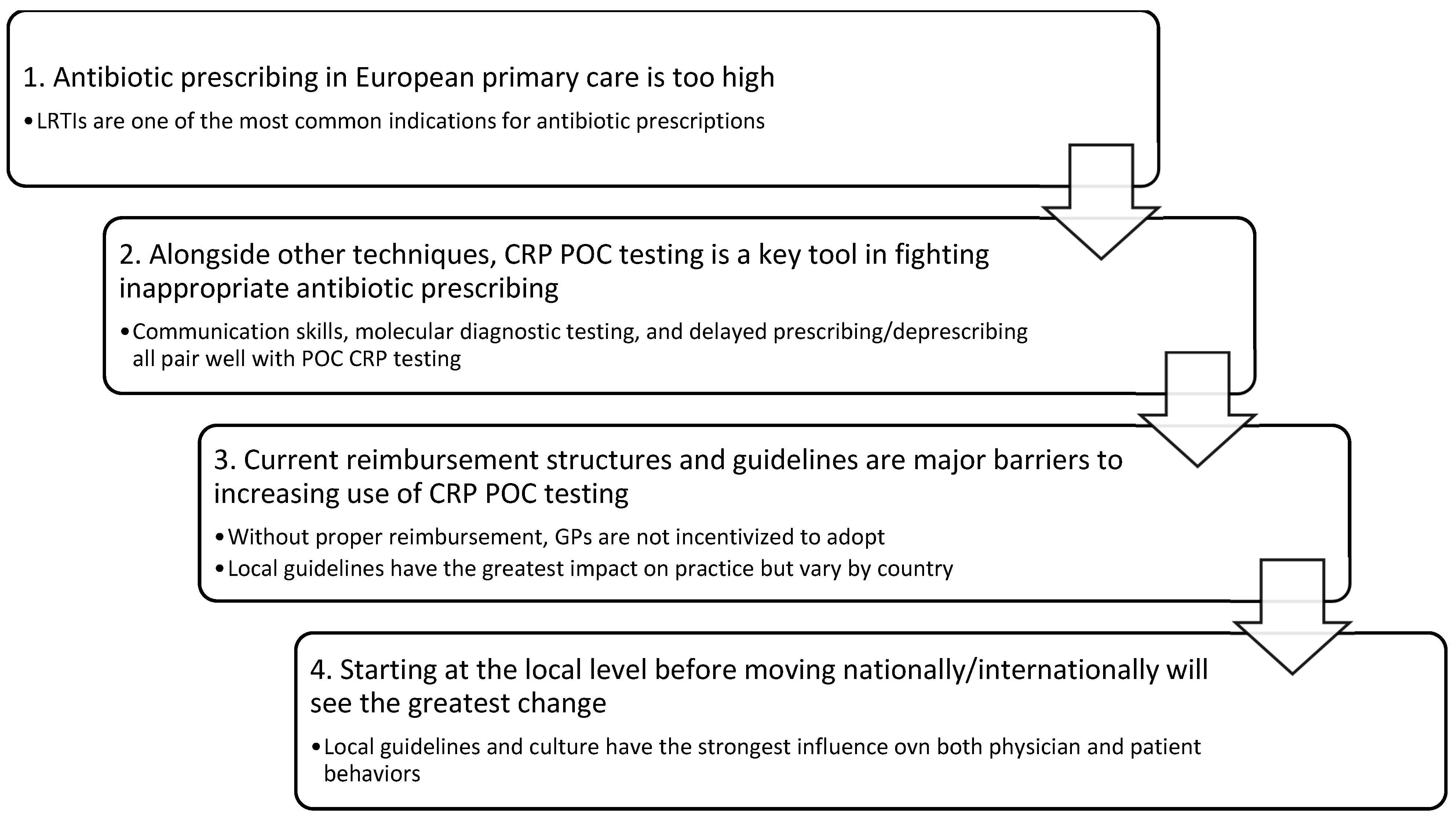
3.1. CRP POC Testing as a Pillar in the Fight against Antibiotic Over-Prescription
3.2. Combining CRP POC Testing with Other Strategies to Reduce Antibiotic Over-Prescription
3.2.1. Communication Skills
3.2.2. Delayed Prescribing and Deprescribing
3.2.3. Molecular Diagnostic Testing
3.3. CRP POC Testing in the COVID Era
3.4. Barriers to Adopting CRP POC Testing
3.4.1. Financial Structure
3.4.2. Logistics
3.4.3. Patient Access to Antibiotics
3.4.4. Implementation Strategy
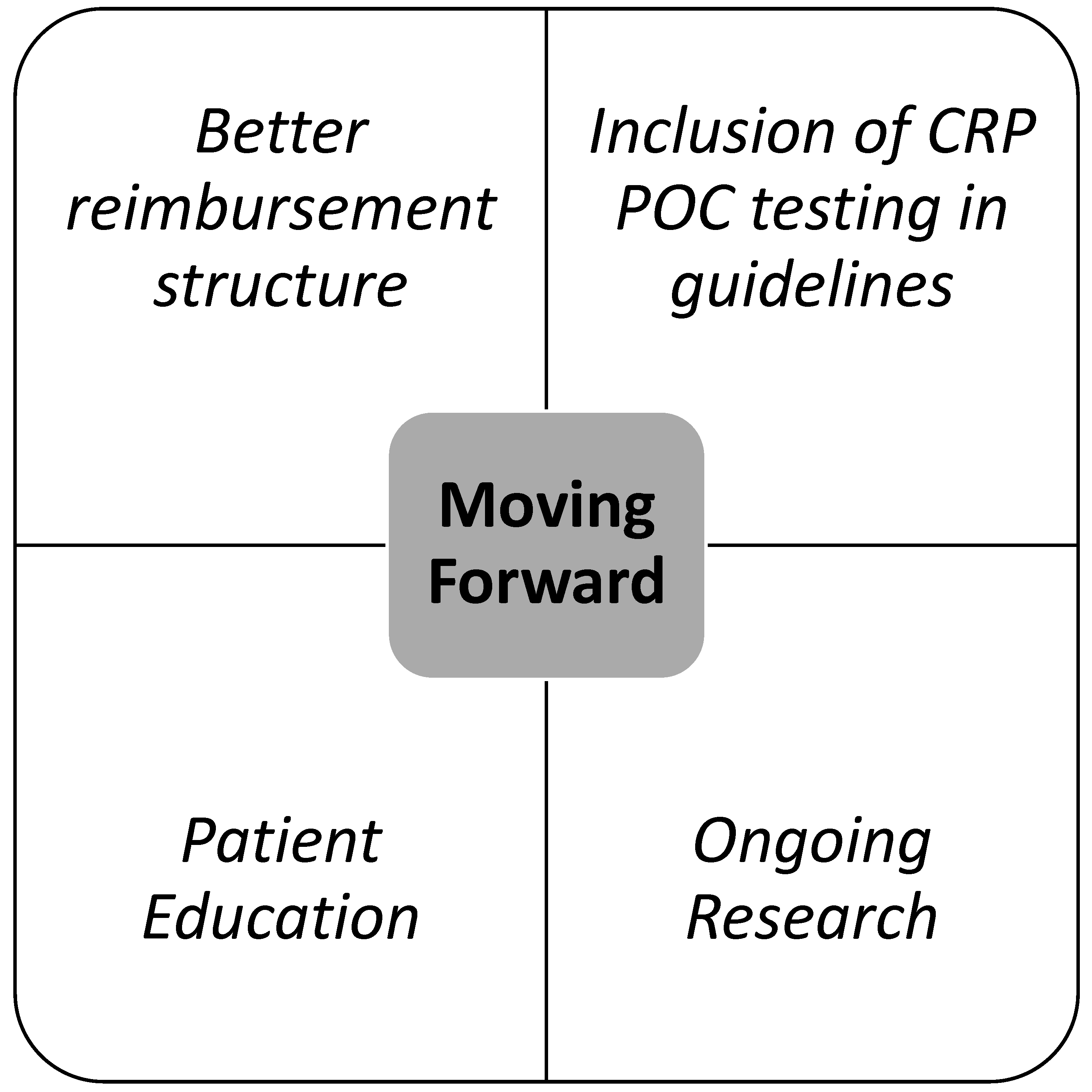
3.5. CRP POC Reimbursement—Current Landscape and Moving Forward
3.6. CRP POC Testing and the Role of Clinical Guidelines
3.7. Anticipated Drivers of Change
3.8. Potential for Research or Public Health Projects
3.9. Think Global, Act Local
4. Conclusions
- Updated recommendations for the use of CRP POC testing for LRTIs and the prescribing of antibiotics;
- Development of a straightforward implementation strategy guiding the use of CRP POC testing in general practice, specifically accounting for local culture and barriers;
- Recommendations for the monitoring of appropriate CRP POC testing and antibiotic prescribing;
- Development of culture-specific educational and communication tools;
- Definition of further research needs.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. World Antimicrobial Awareness Week 18–24 November 2021. 2021. Available online: https://www.who.int/campaigns/world-antimicrobial-awareness-week/2021 (accessed on 13 October 2022).
- Tonkin-Crine, S.K.; Tan, P.S.; van Hecke, O.; Wang, K.; Roberts, N.W.; McCullough, A.; Hansen, M.P.; Butler, C.C.; Del Mar, C.B. Clinician-targeted interventions to influence antibiotic prescribing behaviour for acute respiratory infections in primary care: An overview of systematic reviews. Cochrane Database Syst. Rev. 2017, 19, CD012252. [Google Scholar] [CrossRef] [PubMed]
- Ebell, M.H.; Mph, M.B.; Cai, X.; Hulme, C.; Kearney, M. Accuracy of Biomarkers for the Diagnosis of Adult Community-acquired Pneumonia: A Meta-analysis. Acad. Emerg. Med. 2020, 27, 195–206. [Google Scholar] [CrossRef] [PubMed]
- Woodhead, M.; Blasi, F.; Ewig, S.; Garau, J.; Huchon, G.; Ieven, M.; Ortqvist, A.; Schaberg, T.; Torres, A.; van der Heijden, G.; et al. Guidelines for the management of adult lower respiratory tract infections—Full version. Clin. Microbiol. Infect. 2011, 17 (Suppl. 6), E1–E59. [Google Scholar] [CrossRef] [PubMed]
- Athlin, S.; Lidman, C.; Lundqvist, A.; Naucler, P.; Nilsson, A.C.; Spindler, C.; Strålin, K.; Hedlund, J. Management of community-acquired pneumonia in immunocompetent adults: Updated Swedish guidelines 2017. Infect. Dis. 2017, 50, 247–272. [Google Scholar] [CrossRef]
- Luftvejsinfektioner—Diagnose og Behandling 2014. Available online: https://vejledninger.dsam.dk/luftvejsinfektioner/ (accessed on 13 October 2022).
- Fermont, J.; Masconi, K.L.; Jensen, M.T.; Ferrari, R.; AP Di Lorenzo, V.; Marott, J.M.; Schuetz, P.; Watz, H.; Waschki, B.; Müllerova, H.; et al. Biomarkers and clinical outcomes in COPD: A systematic review and meta-analysis. Thorax 2019, 74, 439–446. [Google Scholar] [CrossRef]
- Butler, C.C.; Gillespie, D.; White, P.; Bates, J.; Lowe, R.; Thomas-Jones, E.; Wootton, M.; Hood, K.; Phillips, R.; Melbye, H.; et al. C-Reactive Protein Testing to Guide Antibiotic Prescribing for COPD Exacerbations. N. Engl. J. Med. 2019, 381, 111–120. [Google Scholar] [CrossRef]
- Groeneveld, G.H.; van’t Wout, J.W.; Aarts, N.J.; van Rooden, C.J.; Verheij, T.J.; Cobbaert, C.M.; Kuijper, E.J.; de Vries, J.J.; van Dissel, J.T. Prediction model for pneumonia in primary care patients with an acute respiratory tract infection: Role of symptoms, signs, and biomarkers. BMC Infect Dis. 2019, 19, 976. [Google Scholar] [CrossRef]
- Verbakel, J.Y.; Lee, J.; Goyder, C.; Tan, P.S.; Ananthakumar, T.; Turner, P.; Hayward, G.; Van den Bruel, A. Impact of point-of-care C reactive protein in ambulatory care: A systematic review and meta-analysis. BMJ Open 2019, 9, e025036. [Google Scholar] [CrossRef]
- van der Velden, A.W.; van de Pol, A.C.; Bongard, E.; Cianci, D.; Aabenhus, R.; Balan, A.; Böhmer, F.; Lang, V.B.; Bruno, P.; Chlabicz, S.; et al. Point-of-care testing, antibiotic prescribing, and prescribing confidence for respiratory tract infections in primary care: A prospective audit in 18 European countries. BJGP Open. 2022, 6, BJGPO-2021. [Google Scholar] [CrossRef]
- Martínez-González, N.A.; Keizer, E.; Plate, A.; Coenen, S.; Valeri, F.; Verbakel, J.Y.J.; Rosemann, T.; Neuner-Jehle, S.; Senn, O. Point-of-Care C-Reactive Protein Testing to Reduce Antibiotic Prescribing for Respiratory Tract Infections in Primary Care: Systematic Review and Meta-Analysis of Randomised Controlled Trials. Antibiotics 2020, 9, 610. [Google Scholar] [CrossRef]
- C-Reactive Protein Point-of-Care Testing (Crp Poct) to Guide Antibiotic Prescribing in Primary Care Settings for Acute Respiratory Tract Infections (Rtis) European Union: European Network for Health Technology Assessment (EUnetHTA). 2019. Available online: https://www.eunethta.eu/wp-content/uploads/2019/02/EUnetHTA_OTCA012_CRP-POCT_31012019.pdf (accessed on 13 October 2022).
- Aabenhus, R.; Jensen, J.-U.S.; Jørgensen, K.J.; Hróbjartsson, A.; Bjerrum, L. Biomarkers as point-of-care tests to guide prescription of antibiotics in patients with acute respiratory infections in primary care. Cochrane Database Syst Rev. 2014, 11, CD010130, Update in Cochrane Database Syst Rev. 2022, 10, CD010130. [Google Scholar] [CrossRef] [PubMed]
- Boere, T.M.; van Buul, L.W.; Hopstaken, R.M.; van Tulder, M.W.; Twisk, J.W.M.R.; Verheij, T.J.M.; Hertogh, C.M. Effect of C reactive protein point-of-care testing on antibiotic prescribing for lower respiratory tract infections in nursing home residents: Cluster randomised controlled trial. BMJ 2021, 374. [Google Scholar] [CrossRef] [PubMed]
- Cooke, J.; Llor, C.; Hopstaken, R.; Dryden, M.; Butler, C. Respiratory tract infections (RTIs) in primary care: Narrative review of C reactive protein (CRP) point-of-care testing (POCT) and antibacterial use in patients who present with symptoms of RTI. BMJ Open Respir. Res. 2020, 7, e000624. [Google Scholar] [CrossRef] [PubMed]
- Little, P.; Stuart, B.; Francis, N.; Douglas, E.; Tonkin-Crine, S.; Anthierens, S.; Cals, J.W.; Melbye, H.; Santer, M.; Moore, M.; et al. Effects of internet-based training on antibiotic prescribing rates for acute respiratory-tract infections: A multinational, cluster, randomised, factorial, controlled trial. Lancet 2013, 382, 1175–1182. [Google Scholar] [CrossRef]
- Schuetz, P.; Amin, D.N.; Greenwald, J.L. Role of Procalcitonin in Managing Adult Patients with Respiratory Tract Infections. Chest 2012, 141, 1063–1073. [Google Scholar] [CrossRef] [PubMed]
- Azzini, A.M.; Dorizzi, R.M.; Sette, P.; Vecchi, M.; Coledan, I.; Righi, E.; Tacconelli, E. A 2020 review on the role of procalcitonin in different clinical settings: An update conducted with the tools of the Evidence Based Laboratory Medicine. Ann. Transl. Med. 2020, 8, 610. [Google Scholar] [CrossRef]
- Simon, L.; Gauvin, F.; Amre, D.K.; Saint-Louis, P.; Lacroix, J. Serum Procalcitonin and C-Reactive Protein Levels as Markers of Bacterial Infection: A Systematic Review and Meta-analysis. Clin. Infect. Dis. 2004, 39, 206–217. [Google Scholar] [CrossRef]
- Lykkegaard, J.; Olsen, J.K.; Sydenham, R.V.; Hansen, M.P. C-reactive protein cut-offs used for acute respiratory infections in Danish general practice. BJGP Open 2020, 5, bjgpopen20X101136. [Google Scholar] [CrossRef]
- Giles, J.T.; Bartlett, S.; Andersen, R.; Thompson, R.; Fontaine, K.R.; Bathon, J.M. Association of body fat with C-reactive protein in rheumatoid arthritis. Arthritis Rheum. 2008, 58, 2632–2641. [Google Scholar] [CrossRef]
- Vuong, J.; Qiu, Y.; La, M.; Clarke, G.; Swinkels, D.W.; Cembrowski, G. Reference intervals of complete blood count constituents are highly correlated to waist circumference: Should obese patients have their own “normal values?”. Am. J. Hematol. 2014, 89, 671–677. [Google Scholar] [CrossRef]
- Kushner, I.; Rzewnicki, D.; Samols, D. What does minor elevation of C-reactive protein signify? Am. J. Med. 2006, 119, 166.e17–166.e28. [Google Scholar] [CrossRef] [PubMed]
- Le Gall, C.; Désidéri-Vaillant, C.; Nicolas, X. Significations of extremely elevated C-reactive protein: About 91 cases in a French hospital center. Pathol. Biol. 2011, 59, 319–320. [Google Scholar] [CrossRef]
- Vanderschueren, S.; Deeren, D.; Knockaert, D.C.; Bobbaers, H.; Bossuyt, X.; Peetermans, W. Extremely elevated C-reactive protein. Eur. J. Intern. Med. 2006, 17, 430–433. [Google Scholar] [CrossRef] [PubMed]
- Flanders, S.A.; Stein, J.; Shochat, G.; Sellers, K.; Holland, M.; Maselli, J.; Drew, W.; Reingold, A.L.; Gonzales, R. Performance of a bedside c-reactive protein test in the diagnosis of community-acquired pneumonia in adults with acute cough. Am. J. Med. 2004, 116, 529–535. [Google Scholar] [CrossRef] [PubMed]
- Bari, S.F.; Khan, A.; Lawson, T. C reactive protein may not be reliable as a marker of severe bacterial infection in patients receiving tocilizumab. BMJ Case Rep. 2013, 2013, bcr2013010423. [Google Scholar] [CrossRef]
- Nanki, T.; Onoue, I.; Nagasaka, K.; Takayasu, A.; Ebisawa, M.; Hosoya, T.; Shirai, T.; Sugihara, T.; Hirata, S.; Kubota, T.; et al. Suppression of elevations in serum C reactive protein levels by anti-IL-6 autoantibodies in two patients with severe bacterial infections. Ann. Rheum. Dis. 2013, 72, 1100–1102. [Google Scholar] [CrossRef]
- Stuart, B.; Hounkpatin, H.; Becque, T.; Yao, G.; Zhu, S.; Alonso-Coello, P.; Altiner, A.; Arroll, B.; Böhning, D. Delayed antibiotic prescribing for respiratory tract infections: Individual patient data meta-analysis. BMJ 2021, 373, n808. [Google Scholar] [CrossRef]
- Ryves, R.; Eyles, C.; Moore, M.; McDermott, L.; Little, P.; Leydon, G.M. Understanding the delayed prescribing of antibiotics for respiratory tract infection in primary care: A qualitative analysis. BMJ Open 2016, 6, e011882. [Google Scholar] [CrossRef]
- Llor, C.; Moragas, A.; Bayona, C.; Cots, J.M.; Hernández, S.; Calviño, O.; Rodríguez, M.; Miravitlles, M. Efficacy and safety of discontinuing antibiotic treatment for uncomplicated respiratory tract infections when deemed unnecessary. A multicentre, randomized clinical trial in primary care. Clin. Microbiol. Infect. 2021, 28, 241–247. [Google Scholar] [CrossRef]
- Lentner, J.; Adams, T.; Knutson, V.; Zeien, S.; Abbas, H.; Moosavi, R.; Manuel, C.; Wallace, T.; Harmon, A.; Waters, R.; et al. C-reactive protein levels associated with COVID-19 outcomes in the United States. J. Am. Osteopat. Assoc. 2021, 121, 869–873. [Google Scholar] [CrossRef]
- Gallo Marin, B.; Aghagoli, G.; Lavine, K.; Yang, L.; Siff, E.J.; Chiang, S.S.; Salazar-Mather, T.P.; Dumenco, L.; Savaria, M.C.; Aung, S.N.; et al. Predictors of COVID-19 severity: A literature review. Rev. Med. Virol. 2021, 31, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Ali, N. Elevated level of C-reactive protein may be an early marker to predict risk for severity of COVID-19. J. Med. Virol. 2020, 92, 2409–2411. [Google Scholar] [CrossRef] [PubMed]
- Smilowitz, N.R.; Kunichoff, D.; Garshick, M.; Shah, B.; Pillinger, M.; Hochman, J.S.; Berger, J.S. C-reactive protein and clinical outcomes in patients with COVID-19. Eur. Heart J. 2021, 42, 2270–2279. [Google Scholar] [CrossRef] [PubMed]
- Health Nio. Covid Treatment Guidelines 2022. Available online: https://www.covid19treatmentguidelines.nih.gov/ (accessed on 13 October 2022).
- Vahey, G.M.; McDonald, E.; Marshall, K.; Martin, S.W.; Chun, H.; Herlihy, R.; Tate, J.E.; Kawasaki, B.; Midgley, C.M.; Alden, N.; et al. Risk factors for hospitalization among persons with COVID-19—Colorado. PLoS ONE 2021, 16, e0256917. [Google Scholar] [CrossRef]
- Pisaturo, M.; De Angelis, G.; Maggi, P.; Sangiovanni, V.; Numis, F.; Gentile, I.; Masullo, A.; Rescigno, C.; Calabria, G.; Megna, A.S.; et al. Clinical Features of Patients with Home Isolation Sars-Cov-2 Infection: A Multicenter Retrospective Study in Southern Italy. Life 2021, 11, 347. [Google Scholar] [CrossRef]
- Hergens, M.P.; Bell, M.; Haglund, P.; Sundström, J.; Lampa, E.; Nederby-Öhd, J.; Östlund, M.R.; Cars, T. Risk factors for COVID-19-related death, hospitalization and intensive care: A population-wide study of all inhabitants in Stockholm. Eur. J. Epidemiol. 2022, 37, 157–165. [Google Scholar] [CrossRef]
- Platto, S.; Wang, Y.; Zhou, J.; Carafoli, E. History of the COVID-19 pandemic: Origin, explosion, worldwide spreading. Biochem. Biophys. Res. Commun. 2020, 538, 14–23. [Google Scholar] [CrossRef]



| Attila ALTINER | GERMANY | Professor at the Institut für Allgemeinmedizin and Head of the Institute of General Practice of the University of Rostock |
| Nick FRANCIS | UK | Professor of Primary Care Research at the University of Southampton/School of Medicine, Neuadd Meirionnydd, University Hospital of Wales |
| Carl LLOR | SPAIN | General practitioner at the Primary Healthcare Centre, Via Roma, Barcelona, Spain, and Associate Professor at the Department of Public Health and Primary Care at the University of Southern Denmark, Odense |
| Ivan GENTILE | ITALY | Professor of Infectious Diseases, Chief of the Infectious Diseases Unit AOU Federico II, Director of the Residency Program of Infectious & Tropical Diseases University of Naples Federico II, Naples, Italy |
| Hasse MELBYE | NORWAY | Professor of General Practice, General Practice Research Unit, Department of Community Medicine, The Arctic University of Norway |
| Oliver SENN | SWITZERLAND | Professor at the Institute of Primary Care, University of Zurich and University Hospital of Zurich |
| Rogier HOPSTAKEN | NETHERLANDS | General practitioner and innovation specialist at Star-shl diagnostic centers and chair of the special interest group for POCT of the World Organization of Family Doctors (WONCA) |
| Current CRP POC Test Use: | Advantages | Disadvantages |
|---|---|---|
| Diagnostic uncertainty following clinical assessment |
|
|
| Confirmatory test after decision to prescribe |
|
|
| Quantitative CRP POCT |
|
| Semi-quantitative CRP POCT |
|
| Delayed prescribing |
|
| Communication training and tools |
|
| Procalcitonin (POCT) |
|
| Influenza A and B POCT |
|
| Strep A POCT |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gentile, I.; Schiano Moriello, N.; Hopstaken, R.; Llor, C.; Melbye, H.; Senn, O. The Role of CRP POC Testing in the Fight against Antibiotic Overuse in European Primary Care: Recommendations from a European Expert Panel. Diagnostics 2023, 13, 320. https://doi.org/10.3390/diagnostics13020320
Gentile I, Schiano Moriello N, Hopstaken R, Llor C, Melbye H, Senn O. The Role of CRP POC Testing in the Fight against Antibiotic Overuse in European Primary Care: Recommendations from a European Expert Panel. Diagnostics. 2023; 13(2):320. https://doi.org/10.3390/diagnostics13020320
Chicago/Turabian StyleGentile, Ivan, Nicola Schiano Moriello, Rogier Hopstaken, Carl Llor, Hasse Melbye, and Oliver Senn. 2023. "The Role of CRP POC Testing in the Fight against Antibiotic Overuse in European Primary Care: Recommendations from a European Expert Panel" Diagnostics 13, no. 2: 320. https://doi.org/10.3390/diagnostics13020320
APA StyleGentile, I., Schiano Moriello, N., Hopstaken, R., Llor, C., Melbye, H., & Senn, O. (2023). The Role of CRP POC Testing in the Fight against Antibiotic Overuse in European Primary Care: Recommendations from a European Expert Panel. Diagnostics, 13(2), 320. https://doi.org/10.3390/diagnostics13020320






