Interpretation of Heart and Lungs Sounds Acquired via Remote, Digital Auscultation Reached Fair-to-Substantial Levels of Consensus among Specialist Physicians
Abstract
:1. Introduction
1.1. Current Status of Hospital-at-Home Services
1.2. Technology-Based, Telemedicine-Controlled Hospital-at-Home Services
1.3. The Case of Technologically Enabled Remote Physical Examination
1.4. Application of the TytoCareTM System in Telemedicine-Controlled HAH
2. Materials and Methods
2.1. The TytoCareTM System Auscultations
2.2. Patient and Physician Populations
2.3. Statistical Analysis
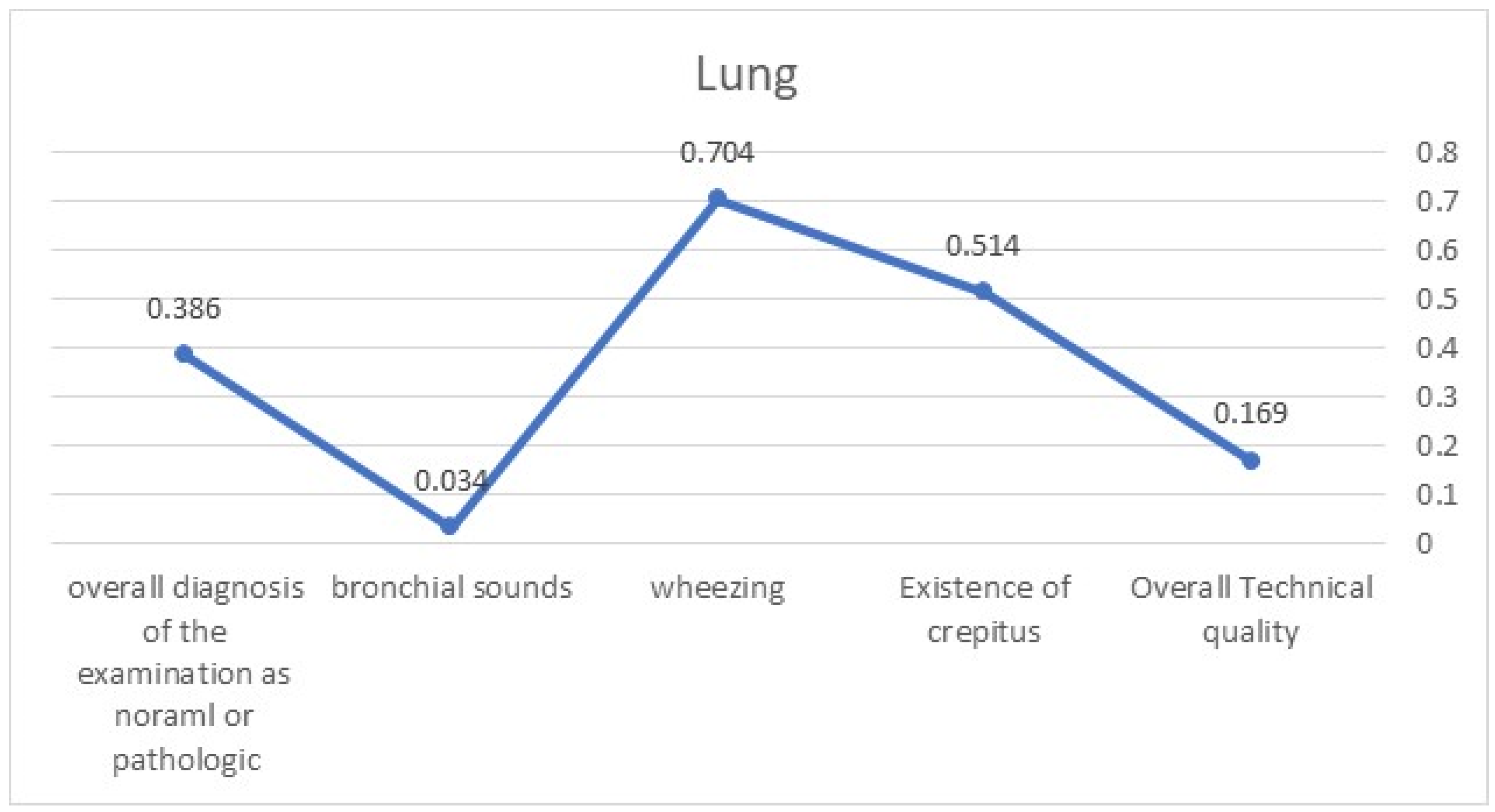
3. Results
4. Discussion
- Recording of auscultations should follow a standardized procedure: In contrast to the traditional physical examination conducted by a physician or a nurse on their own, the attainment of digital bio-signals should be standardized. We approached this issue by dictating the specific points of auscultation performed via TytoCareTM in specific patients’ positioning. This step alone did not achieve a high enough level of agreement among the interpreting physicians. Therefore, we should further standardize the process of recording auscultations related to the positioning of patients, prior training of physicians in the usage of the specific digital device used, the length of recording, controlling the level of surrounding noises, and determining the minimal number of recordings per auscultation point.
- Digital data related to physical examination should be interpreted by more than one healthcare professional: Currently, recorded auscultations are uploaded to the TytoCareTM cloud, allowing multiple professionals to give their interpretations. These professionals can include two physicians or a combination of physicians, experienced nurses, and paramedics. The specific combination should be separately sought by each healthcare organization utilizing such technologies. At times, a cautious approach should prefer the opinion of a single physician rather than pursue a definitive solution.
- Artificial intelligence applications potentially interpreting bio-signals of telemedicine-gained physical examination outputs should be developed: With advancements in AI algorithms, we anticipate that, in the near future, AI applications will support physicians by providing suggestions for interpreting auscultation findings, among other bio-signals recorded during telemedicine-based physical examination of remotely situated patients [24]. When related to recommendation A, it is advisable to remember that AI algorithms will, initially, offer standardizations for acquired sounds prior to human interpretation and potentially triage sounds, flagging them as “normal” versus “necessitating prompt clinical interpretation”.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cerdan de las Heras, J.; Andersen, S.L.; Matthies, S.; Sandreva, T.V.; Johannesen, C.K.; Nielsen, T.L.; Fuglebjerg, N.; Catalan-Matamoros, D.; Hansen, D.G.; Fischer, T.K. Hospitalisation at Home of Patients with COVID-19: A Qualitative Study of User Experiences. Int. J. Environ. Res. Public Health 2023, 20, 1287. [Google Scholar] [CrossRef] [PubMed]
- Nicolás, D.; Coloma, E.; Pericàs, J.M. Alternatives to conventional hospitalisation that enhance health systems’ capacity to treat COVID-19. Lancet Infect Dis. 2021, 21, 591–593. [Google Scholar] [CrossRef] [PubMed]
- Almathami, H.K.Y.; Than Win, K.; Vlahu-Gjorgievska, E. Barriers and facilitators that influence telemedicine-based, real-time, online consultation at patients’ homes: Systematic literature review. J. Med. Internet Res. 2020, 22, e16407. [Google Scholar] [CrossRef] [PubMed]
- Serrano, L.P.; Maita, K.C.; Avila, F.R.; Torres-Guzman, R.A.; Garcia, J.P.; Eldaly, A.S.; Haider, C.R.; Felton, C.L.; Paulson, M.R.; Maniaci, M.J.; et al. Benefits and Challenges of Remote Patient Monitoring as Perceived by Health Care Practitioners: A Systematic Review. Perm. J. 2023, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens. Int. 2021, 2, 100117. [Google Scholar] [CrossRef] [PubMed]
- Akhtar, M.; Van Heukelom, P.G.; Ahmed, A.; Tranter, R.D.; White, E.; Shekem, N.; Walz, D.; Fairfield, C.; Vakkalanka, J.P.; Mohr, N.M. Telemedicine Physical Examination Utilizing a Consumer Device Demonstrates Poor Concordance with In-Person Physical Examination in Emergency Department Patients with Sore Throat: A Prospective Blinded Study. Telemed. J. e-Health 2018, 24, 790. [Google Scholar] [CrossRef] [PubMed]
- Berger, R.; Berger, R.; Bulmash, B.; Drori, N.; Ben-Assuli, O.; Herstein, R. The patient-physician relationship: An account of the physician’s perspective. Isr. J. Health Policy Res. 2020, 9, 33. [Google Scholar] [CrossRef]
- Yao, P.; Adam, M.; Clark, S.; Hsu, H.; Stern, M.; Sharma, R.; Mages, K.; Greenwald, P.; Naik, N. A scoping review of the unassisted physical exam conducted over synchronous audio-video telemedicine. Syst. Rev. 2022, 11, 219. [Google Scholar] [CrossRef]
- Lu, A.D.; Veet, C.A.; Aljundi, O.; Whitaker, E.; Smith, W.B.; Smith, J.E. A Systematic Review of Physical Examination Components Adapted for Telemedicine. Telemed. J. e-Health 2022, 28, 1764–1785. [Google Scholar] [CrossRef]
- Haskel, O.; Itelman, E.; Zilber, E.; Barkai, G.; Segal, G. Remote Auscultation of Heart and Lungs as an Acceptable Alternative to Legacy Measures in Quarantined COVID-19 Patients-Prospective Evaluation of 250 Examinations. Sensors 2022, 22, 3165. [Google Scholar] [CrossRef]
- Omboni, S.; Padwal, R.S.; Alessa, T.; Benczúr, B.; Green, B.B.; Hubbard, I.; Kario, K.; Khan, N.A.; Konradi, A.; Logan, A.G.; et al. The worldwide impact of telemedicine during COVID-19: Current evidence and recommendations for the future. Connect. Health 2022, 1, 7–35. [Google Scholar] [CrossRef] [PubMed]
- Chien, J.; Huang, M.C.; Lin YDer Chong, F.C. A study of heart sound and lung sound separation by independent component analysis technique. Conf. Proc. IEEE Eng. Med. Biol. Soc. 2006, 2006, 5708–5711. [Google Scholar] [PubMed]
- Javed, F.; Venkatachalam, P.A.; Hani, A.F.M. Knowledge based system with embedded intelligent heart sound analyser for diagnosing cardiovascular disorders. J. Med. Eng. Technol. 2007, 31, 341–350. [Google Scholar] [CrossRef] [PubMed]
- Grossman, Z.; Chodick, G.; Reingold, S.M.; Chapnick, G.; Ashkenazi, S. The future of telemedicine visits after COVID-19: Perceptions of primary care pediatricians. Isr. J. Health Policy Res. 2020, 9, 53. [Google Scholar] [CrossRef] [PubMed]
- McDaniel, N.L.; Novicoff, W.; Gunnell, B.; Cattell Gordon, D. Comparison of a Novel Handheld Telehealth Device with Stand-Alone Examination Tools in a Clinic Setting. Telemed. J. e-Health 2019, 25, 1225–1230. [Google Scholar] [CrossRef] [PubMed]
- Ford, G.; Compton, M.; Millett, G.; Tzortzis, A. The Role of Digital Disruption in Healthcare Service Innovation. In Service Business Model Innovation in Healthcare and Hospital Management; Springer: Cham, Switzerland, 2017; pp. 57–70. [Google Scholar]
- Hermes, S.; Riasanow, T.; Clemons, E.K.; Böhm, M.; Krcmar, H. The digital transformation of the healthcare industry: Exploring the rise of emerging platform ecosystems and their influence on the role of patients. Bus. Res. 2020, 13, 1033–1069. [Google Scholar] [CrossRef]
- Smith, S.; Newman-Sanders, C. Disrupting the Delivery Mechanisms of Traditional Healthcare. In Hybrid Healthcare; Springer: Cham, Switzerland, 2022; pp. 59–69. [Google Scholar]
- Yoshida, Y.; Patil, S.J.; Brownson, R.C.; Boren, S.A.; Kim, M.; Dobson, R.; Waki, K.; Greenwood, D.A.; Torbjørnsen, A.; Ramachandran, A.; et al. Using the RE-AIM framework to evaluate internal and external validity of mobile phone-based interventions in diabetes self-management education and support. J. Am. Med. Inform. Assoc. 2020, 27, 946–956. [Google Scholar] [CrossRef]
- Ownsworth, T.; Arnautovska, U.; Beadle, E.; Shum, D.H.K.; Moyle, W. Efficacy of Telerehabilitation for Adults with Traumatic Brain Injury: A Systematic Review. J. Head. Trauma Rehabil. 2018, 33, E33–E46. [Google Scholar] [CrossRef]
- Bokolo, A.J. Exploring the adoption of telemedicine and virtual software for care of outpatients during and after COVID-19 pandemic. Ir. J. Med. Sci. 2021, 190, 1–10. [Google Scholar] [CrossRef]
- Solaiman, B. Telehealth in the Metaverse: Legal & Ethical Challenges for Cross-Border Care in Virtual Worlds. J. Law Med. Ethics 2023, 51, 287–300. [Google Scholar]
- Fan, M.; Wang, Q.; Liu, J.; Su, L.; Wang, B.; Xu, H.; Li, Q.; Zhang, Z. Real-world evaluation of the Stemoscope electronic tele-auscultation system. Biomed. Eng. Online 2022, 21, 63. [Google Scholar] [CrossRef]
- Park, S.; Wahab, A.; Usman, M.; Naseem, I.; Khan, S. Editorial: Artificial intelligence in bioimaging and signal processing. Front. Physiol. 2023, 14, 1267632. [Google Scholar] [CrossRef]

| Main complaint | (e.g., chest pain) |
| Background diagnoses | (e.g., congestive heart failure) |
| Technical quality | high/low/does not enable interpretation |
| Crepitus with or without crackles | Yes/No |
| Wheezing | Yes/No |
| Bronchial sounds | Yes/No |
| Summary | normal/pathologic/does not enable interpretation |
| Main complaint | (e.g., cough) |
| Background diagnoses | (e.g., congestive heart failure) |
| Technical quality | high/low/does not enable interpretation |
| Regular | Yes/No |
| Murmurs | Yes/No |
| Remote sounds | Yes/No |
| Summary | normal/pathologic/does not enable interpretation |
| κ | Interpretation |
|---|---|
| <0 | Poor agreement |
| 0.01–0.20 | Slight agreement |
| 0.21–0.40 | Fair agreement |
| 0.41–0.60 | Moderate agreement |
| 0.61–0.80 | Substantial agreement |
| 0.81–1.00 | Almost perfect agreement |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Magor, D.; Berkov, E.; Siomin, D.; Karniel, E.; Lasman, N.; Waldman, L.R.; Gringauz, I.; Stern, S.; Kassif, R.L.; Barkai, G.; et al. Interpretation of Heart and Lungs Sounds Acquired via Remote, Digital Auscultation Reached Fair-to-Substantial Levels of Consensus among Specialist Physicians. Diagnostics 2023, 13, 3153. https://doi.org/10.3390/diagnostics13193153
Magor D, Berkov E, Siomin D, Karniel E, Lasman N, Waldman LR, Gringauz I, Stern S, Kassif RL, Barkai G, et al. Interpretation of Heart and Lungs Sounds Acquired via Remote, Digital Auscultation Reached Fair-to-Substantial Levels of Consensus among Specialist Physicians. Diagnostics. 2023; 13(19):3153. https://doi.org/10.3390/diagnostics13193153
Chicago/Turabian StyleMagor, Diana, Evgeny Berkov, Dmitry Siomin, Eli Karniel, Nir Lasman, Liat Radinsky Waldman, Irina Gringauz, Shai Stern, Reut Lerner Kassif, Galia Barkai, and et al. 2023. "Interpretation of Heart and Lungs Sounds Acquired via Remote, Digital Auscultation Reached Fair-to-Substantial Levels of Consensus among Specialist Physicians" Diagnostics 13, no. 19: 3153. https://doi.org/10.3390/diagnostics13193153
APA StyleMagor, D., Berkov, E., Siomin, D., Karniel, E., Lasman, N., Waldman, L. R., Gringauz, I., Stern, S., Kassif, R. L., Barkai, G., Lewy, H., & Segal, G. (2023). Interpretation of Heart and Lungs Sounds Acquired via Remote, Digital Auscultation Reached Fair-to-Substantial Levels of Consensus among Specialist Physicians. Diagnostics, 13(19), 3153. https://doi.org/10.3390/diagnostics13193153






