Clinical and Forensic Investigation Protocols for Diagnosing Abusive Head Trauma: A Literature Review
Abstract
:1. Introduction
1.1. Epidemiology of AHT
1.2. False Positives Issue
1.3. Terminology
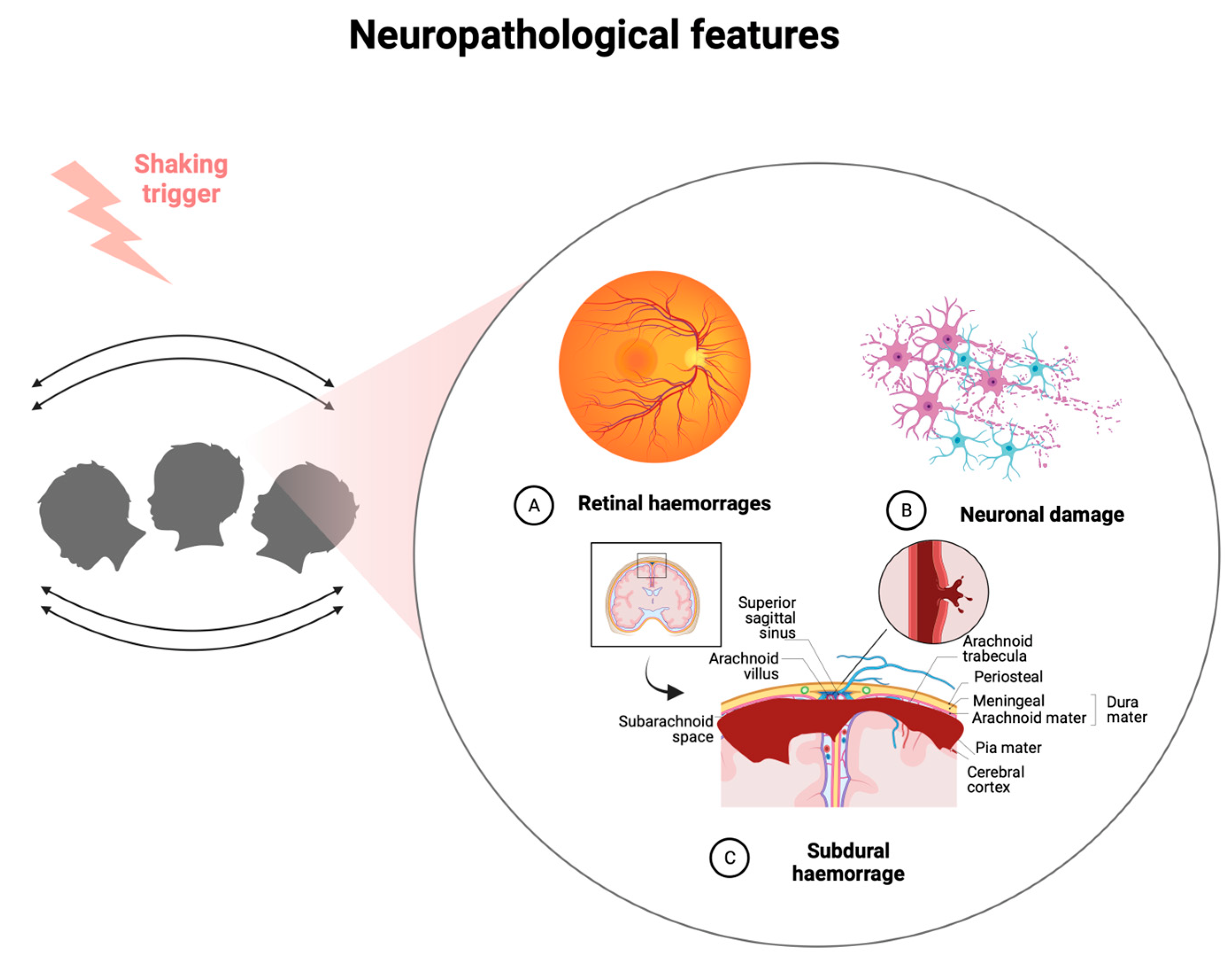
1.4. Pathophysiology of AHT
2. Materials and Methods
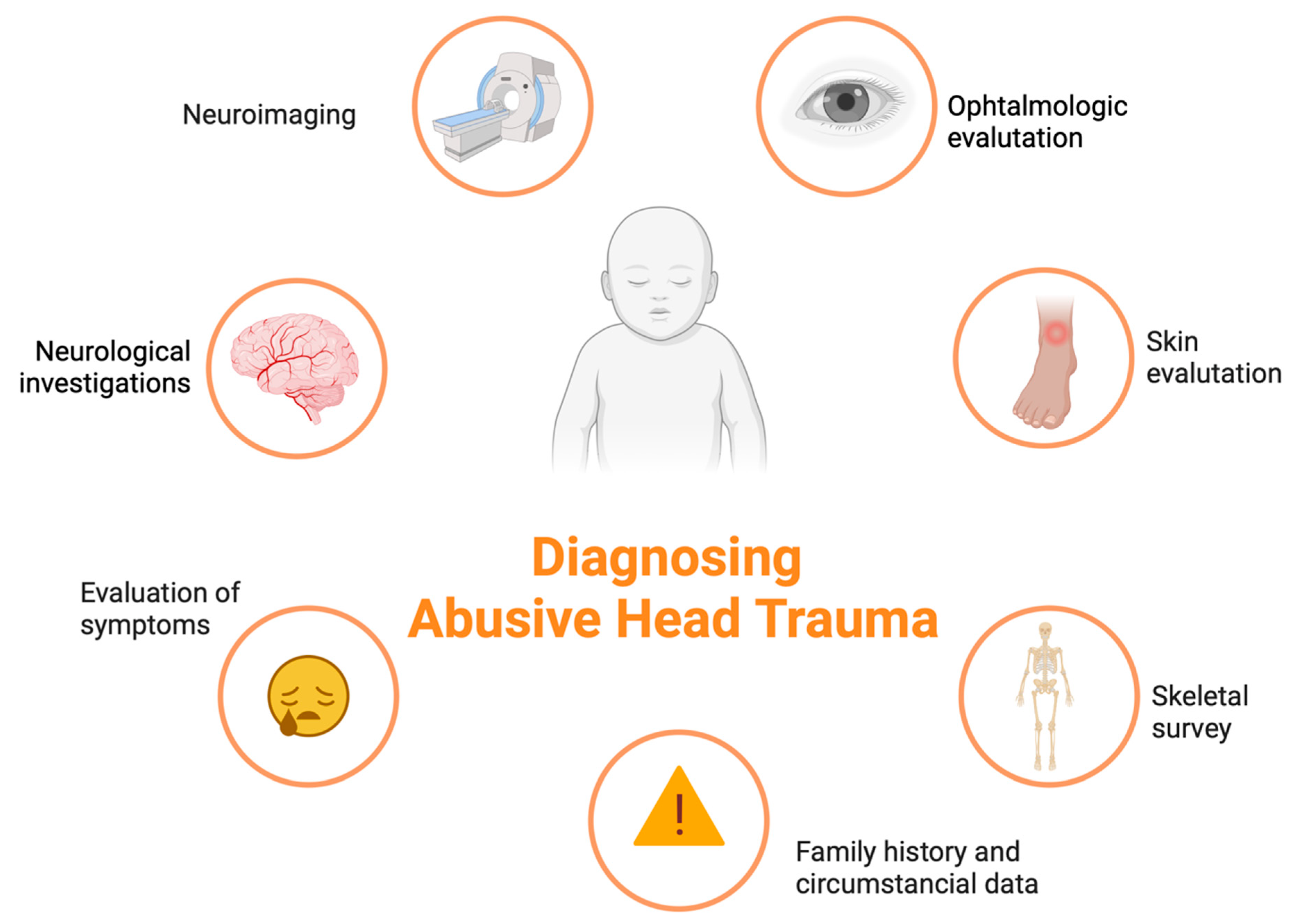
3. Results and Discussion
3.1. Ophtalmological Investigations
3.2. Radiological Investigations
3.3. Brain Injuries
3.4. Laboratory Investigations
3.5. Medico Legal Investigations on Child and Post-Mortem Analysis
3.6. Investigation Protocols for Diagnostics
3.6.1. Clinical Investigation Protocols
3.6.2. Post-Mortem Investigation Protocols
3.6.3. Forensic Investigation of the Perpetrator
3.6.4. Differential Diagnosis with Pathologies Not Related to Abuse
4. Conclusions
Conclusions and Future Research Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hahnemann, M.L.; Kronsbein, K.; Karger, B.; Feld, K.; Banaschak, S.; Helmus, J.; Mentzel, H.-J.; Pfeiffer, H.; Wittschieber, D. Characterization of subdural collections in initial neuroimaging of abusive head trauma: Implications for forensic age diagnostics and clinical decision-making. Eur. J. Radiol. 2023, 159, 110652. [Google Scholar] [CrossRef] [PubMed]
- Beam, A.S.; Stephens, C.P.; Taylor, C.; Bentley, J.; Gonzalez, A.C.; Marwaha, M.; Riley, D.; Wade, C. Imaging and Demographic Risk Factors in the Diagnosis of Pediatric Nonaccidental Trauma. Radiol. Technol. 2023, 94, 419–425. [Google Scholar] [PubMed]
- Emrick, B.B.; Smith, E.; Thompson, L.; Mullett, C.; Pino, E.; Snyder, K.; Kroll, M.-A.; Ayoubi, S.; Phillips, J.; Istfan, S.; et al. Epidemiology of abusive head trauma in West Virginia children <24 months: 2000–2010. Child Abuse Negl. 2019, 93, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Macorano, E.; Gentile, M.; Stellacci, G.; Manzionna, M.; Mele, F.; Calvano, M.; Leonardelli, M.; Duma, S.; De Gabriele, G.; Cristalli, A.; et al. ‘Compressed Baby Head’: A New ‘Abusive Head Trauma’ Entity? Children 2023, 10, 1003. [Google Scholar] [CrossRef] [PubMed]
- Knappstein, J.; Reed, P.W.; Kelly, P. ICD-10 codes for surveillance of non-fatal abusive head trauma in Aotearoa New Zealand: A retrospective cohort study. BMJ Open 2023, 13, e069199. [Google Scholar] [CrossRef]
- Pfeifer, C.M.; Henry, M.K.; Caré, M.M.; Christian, C.W.; Servaes, S.; Milla, S.S.; Strouse, P.J. Debunking Fringe Beliefs in Child Abuse Imaging: AJRExpert Panel Narrative Review. AJR Am. J. Roentgenol. 2021, 217, 529–540. [Google Scholar] [CrossRef]
- Wiley, M.; Schultheis, A.; Francis, B.; Tiyyagura, G.; Leventhal, J.M.; Rutherford, H.J.; Mayes, L.C.; Bechtel, K. Parents’ Perceptions of Infant Crying: A Possible Path to Preventing Abusive Head Trauma. Acad. Pediatr. 2020, 20, 448–454. [Google Scholar] [CrossRef]
- Talvik, I.; Alexander, R.C.; Talvik, T. Shaken baby syndrome and a baby’s cry. Acta Paediatr. 2008, 97, 782–785. [Google Scholar] [CrossRef]
- Högberg, U.; Eriksson, G.; Högberg, G.; Wahlberg, Å. Parents’ experiences of seeking health care and encountering allegations of shaken baby syndrome: A qualitative study. PLoS ONE 2020, 15, e0228911. [Google Scholar] [CrossRef]
- Lynøe, N.; Eriksson, A. Agreements and disagreements regarding "shaken baby syndrome". Childs Nerv. Syst. 2022, 38, 2047–2049. [Google Scholar] [CrossRef]
- Di Fazio, N.; Delogu, G.; Morena, D.; Cipolloni, L.; Scopetti, M.; Mazzilli, S.; Frati, P.; Fineschi, V. New Insights into the Diagnosis and Age Determination of Retinal Hemorrhages from Abusive Head Trauma: A Systematic Review. Diagnostics 2023, 13, 1722. [Google Scholar] [CrossRef] [PubMed]
- Christian, C.W.; Block, R.; Committee on Child Abuse and Neglect; American Academy of Pediatrics. Abusive head trauma in infants and children. Pediatrics 2009, 123, 1409–1411. [Google Scholar] [CrossRef] [PubMed]
- Raghupathi, R.; Prasad, R.; Fox, D.; Huh, J.W. Repeated mild closed head injury in neonatal rats results in sustained cognitive deficits associated with chronic microglial activation and neurodegeneration. J. Neuropathol. Exp. Neurol. 2023, 82, 707–721. [Google Scholar] [CrossRef]
- Kato, M.; Nonaka, M.; Akutsu, N.; Narisawa, A.; Harada, A.; Park, Y.-S. Correlations of intracranial pathology and cause of head injury with retinal hemorrhage in infants and toddlers: A multicenter, retrospective study by the J-HITs (Japanese Head injury of Infants and Toddlers study) group. PLoS ONE 2023, 18, e0283297. [Google Scholar] [CrossRef] [PubMed]
- Harris, C.K.; Stagner, A.M. The Eyes Have It: How Critical are Ophthalmic Findings to the Diagnosis of Pediatric Abusive Head Trauma? Semin. Ophthalmol. 2023, 38, 3–8. [Google Scholar] [CrossRef]
- Miller, D.C.; Stacy, C.C.; Duff, D.J.; Guo, S.; Morse, P. Neuropathology and Ophthalmological Pathology of Fatal Central Nervous System Injuries in Young Children: Forensic Neuropathology of Deaths of Children Under Age 2, 2008–2016, in Central Missouri. J. Neuropathol. Exp. Neurol. 2022, 81, 854–864. [Google Scholar] [CrossRef]
- Finnie, J.W.; Blumbergs, P.C. Animal models of pediatric abusive head trauma. Childs Nerv. Syst. 2022, 38, 2317–2324. [Google Scholar] [CrossRef]
- Mavroudis, I.; Kazis, D.; Chowdhury, R.; Petridis, F.; Costa, V.; Balmus, I.-M.; Ciobica, A.; Luca, A.-C.; Radu, I.; Dobrin, R.P.; et al. Post-Concussion Syndrome and Chronic Traumatic Encephalopathy: Narrative Review on the Neuropathology, Neuroimaging and Fluid Biomarkers. Diagnostics 2022, 12, 740. [Google Scholar] [CrossRef]
- Stray-Pedersen, A.; Strisland, F.; Rognum, T.O.; Schiks, L.A.H.; Loeve, A.J. Violent Infant Surrogate Shaking: Continuous High-Magnitude Centripetal Force and Abrupt Shift in Tangential Acceleration May Explain High Risk of Subdural Hemorrhage. Neurotrauma Rep. 2021, 2, 224–231. [Google Scholar] [CrossRef]
- Oruç, M.; Dündar, A.S.; Okumuş, H.; Görmez, M.; Şamdancı, E.T.; Celbiş, O. Shaken baby syndrome resulting in death: A case series. Turk. J. Pediatr. 2021, 63, 31–36. [Google Scholar] [CrossRef]
- Moskwa, R.; Todeschi, J.; Wiedemann-Fode, A.; Stella, I.; Joud, A.; Klein, O. Ophthalmological lesions in shaken baby syndrome: A retrospective analysis of 133 consecutive cases (1992–2018). Neurochirurgie 2022, 68, 367–372. [Google Scholar] [CrossRef] [PubMed]
- Yamazaki, J.; Yoshida, M.; Mizunuma, H. Experimental analyses of the retinal and subretinal haemorrhages accompanied by shaken baby syndrome/abusive head trauma using a dummy doll. Injury 2014, 45, 1196–1206. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, M.; Yamazaki, J.; Mizunuma, H. A finite element analysis of the retinal hemorrhages accompanied by shaken baby syndrome/abusive head trauma. J. Biomech. 2014, 47, 3454–3458. [Google Scholar] [CrossRef] [PubMed]
- Maguire, S.A.; Watts, P.O.; Shaw, A.D.; Holden, S.; Taylor, R.H.; Watkins, W.J.; Mann, M.K.; Tempest, V.; Kemp, A.M. Retinal haemorrhages and related findings in abusive and non-abusive head trauma: A systematic review. Eye 2013, 27, 28–36. [Google Scholar] [CrossRef]
- Ang, J.L.; Collis, S.; Dhillon, B.; Cackett, P. The Eye in Forensic Medicine: A Narrative Review. Asia Pac. J. Ophthalmol. 2021, 10, 486–494. [Google Scholar] [CrossRef]
- Kadom, N.; Khademian, Z.; Vezina, G.; Shalaby-Rana, E.; Rice, A.; Hinds, T. Usefulness of MRI detection of cervical spine and brain injuries in the evaluation of abusive head trauma. Pediatr. Radiol. 2014, 44, 839–848. [Google Scholar] [CrossRef]
- Vinchon, M. Shaken baby syndrome: What certainty do we have? Child’s Nerv. Syst. 2017, 33, 1727–1733. [Google Scholar] [CrossRef] [PubMed]
- Koumellis, P.; McConachie, N.S.; Jaspan, T. Spinal subdural haematomas in children with non-accidental head injury. Arch. Dis. Child. 2009, 94, 216–219. [Google Scholar] [CrossRef]
- Cartocci, G.; Fineschi, V.; Padovano, M.; Scopetti, M.; Rossi-Espagnet, M.C.; Giannì, C. Shaken Baby Syndrome: Magnetic Resonance Imaging Features in Abusive Head Trauma. Brain Sci. 2021, 11, 179. [Google Scholar] [CrossRef]
- Bradford, R.; Choudhary, A.K.; Dias, M.S. Serial neuroimaging in infants with abusive head trauma: Timing abusive injuries. J. Neurosurgery: Pediatr. 2013, 12, 110–119. [Google Scholar] [CrossRef]
- Snelling, P.J.; Thanasingam, A.A.; Jones, P.; Connors, J. Comparison of abusive head trauma versus non-inflicted subdural haematoma in infants: A retrospective cohort study. Emerg. Med. Australas. 2022, 34, 968–975. [Google Scholar] [CrossRef] [PubMed]
- Dashti, S.R.; Decker, D.D.; Razzaq, A.; Cohen, A.R. Current Patterns of Inflicted Head Injury in Children. Pediatr. Neurosurg. 1999, 31, 302–306. [Google Scholar] [CrossRef] [PubMed]
- Vinchon, M.; de Foort-Dhellemmes, S.; Desurmont, M.; Delestret, I. Confessed abuse versus witnessed accidents in infants: Comparison of clinical, radiological, and ophthalmological data in corroborated cases. Childs Nerv. Syst. 2010, 26, 637–645. [Google Scholar] [CrossRef] [PubMed]
- Keenan, H.T.; Runyan, D.K.; Marshall, S.W.; Nocera, M.A.; Merten, D.F. A Population-Based Comparison of Clinical and Outcome Characteristics of Young Children with Serious Inflicted and Noninflicted Traumatic Brain Injury. Pediatrics 2004, 114, 633–639. [Google Scholar] [CrossRef] [PubMed]
- Wiskott, K.; Gilardi, F.; Hainard, A.; Sanchez, J.; Thomas, A.; Sajic, T.; Fracasso, T. Blood proteome of acute intracranial hemorrhage in infant victims of abusive head trauma. Proteomics 2023, 23, e2200078. [Google Scholar] [CrossRef]
- Feld, K.; Ricken, T.; Feld, D.; Helmus, J.; Hahnemann, M.; Schenkl, S.; Muggenthaler, H.; Pfeiffer, H.; Banaschak, S.; Karger, B.; et al. Fractures and skin lesions in pediatric abusive head trauma: A forensic multi-center study. Int. J. Legal Med. 2022, 136, 591–601. [Google Scholar] [CrossRef] [PubMed]
- Bhardwaj, G.; Chowdhury, V.; Jacobs, M.B.; Moran, K.T.; Martin, F.J.; Coroneo, M.T. A Systematic Review of the Diagnostic Accuracy of Ocular Signs in Pediatric Abusive Head Trauma. Ophthalmology 2010, 117, 983–992.e17. [Google Scholar] [CrossRef]
- Colombari, M.; Troakes, C.; Turrina, S.; Tagliaro, F.; De Leo, D.; Al-Sarraj, S. Spinal cord injury as an indicator of abuse in forensic assessment of abusive head trauma (AHT). Int. J. Leg. Med. 2021, 135, 1481–1498. [Google Scholar] [CrossRef] [PubMed]
- Maiese, A.; Iannaccone, F.; Scatena, A.; Del Fante, Z.; Oliva, A.; Frati, P.; Fineschi, V. Pediatric Abusive Head Trauma: A Systematic Review. Diagnostics 2021, 11, 734. [Google Scholar] [CrossRef] [PubMed]
- Messing-Jünger, M.; Alhourani, J. A suspected case of shaken baby syndrome-clinical management in Germany: A case-based overview. Childs Nerv. Syst. 2022, 38, 2375–2382. [Google Scholar] [CrossRef] [PubMed]
- Unuma, K.; Makino, Y.; Yamamoto, K.; Hattori, S.; Arai, N.; Sakai, K.; Kitagawa, M.; Uemura, K.; Kanegane, H. Fatal intracranial hemorrhage due to infantile acute lymphoblastic leukemia mimicking abusive head trauma. J. Forensic Sci. 2021, 66, 2504–2510. [Google Scholar] [CrossRef] [PubMed]
- Clauß, D.; Richter, C.; Klohs, G.; Heide, S. Strafprozessuale Folgen von Kindesmisshandlung [Legal consequences in cases of child abuse]. Klin. Padiatr. 2013, 225, 283–287. [Google Scholar] [CrossRef] [PubMed]
| Authors | Type of Study | Number of Suspected or Confirmed AHT Cases Analysed | Investigations Performed | Results |
|---|---|---|---|---|
| Hahnemann et al. [1] | Retrospective study | 56 | Neuroimaging analysis | 96.4% showed a multifocal presence of SDCs |
| Moskwa et al. [21] | Retrospective study | 133 | Ophthalmological analysis | Ophthalmologic lesions were in 70.3% |
| Yamazaki et al. [22] | Experimental study | Experimental model with a doll | Time integral of stress in shaking is 107 Pa.s, larger than that of a fall | |
| Yoshida et al. [23] | Experimental study | Experimental model with a finite element | Time integral of stress in shaking is 101 Pa.s, larger than that of a single impact | |
| Maguire et al. [24] | Systematic review | 998 | Ophthalmological analysis | Retinal hemorrhages were found in 78% of AHT. |
| Kadom et al. [26] | Retrospective study | 64 | Neuroimaging analysis | 36% of children showed cervical spine injuries. A statistically significant relationship was found between bilateral hypoxic–ischemic brain injury patterns and AHT |
| Vinchon et al. [27] | Prospective study | 1138 | Review of registry | Physicians should exclude non-traumatic bleeding and second, accidental trauma. A systematic and multidisciplinary approach is mandatory. |
| Koumellis et al. [28] | Retrospective study | 18 | Neuroimaging analysis | 44% of cases showed occult subdural collections |
| Cartocci et al. [29] | Review | - | Neuroimaging analysis | Radioimaging is mandatory in suspect of AHT. Subdural hemorrhages with bridging vein rupture and thrombosis are more commonly associated |
| Bradford et al. [30] | Retrospective study | 210 | Neuroimaging analysis | In patients with subdural hematomas, the first hypodense component due to SDH was between 0.3 and 16 days after injury, and the last hyperdense component disappeared between 2 and 40 days after injury. |
| Snelling et al. [31] | Retrospective study | 20 | Clinical and radiological analysis | SDH was associated with maternal drug use, delayed presentation in ED, seizures, altered level of consciousness; fractures, skin injuries or retinal hemorrhages; radiological findings of bilateral and inter-hemispheric blood |
| Dashti et al. [32] | Retrospective study | 38 | Clinical and radiological analysis | SDH was in 69% of cases, retinal hemorrhages were in 53% of cases. Low socioeconomic status was associated with SDH. |
| Vinchon et al. [33] | Retrospective study | 45 | Clinical and radiological analysis | SDH, severe RH, and absence of signs of impact were associated with AHT |
| Keenan et al. [34] | Retrospective study | 80 | Clinical and radiological analysis | RH, fractures, and SDH were more associated with AHT |
| Wiskott et al. [35] | Experimental study | 7 | Proteomic analysis | 165 circulating serum proteins display differences in AHT cases versus controls |
| Feld et al. [36] | Retrospective study | 72 | Clinical and radiological analysis | Fractures were found in 32% of cases; skin injuries were found in 53% of cases |
| Bhardwaj et al. [37] | Systematic review | 20 studies | Ophthalmological analysis | Bilateral, extensive, and intraocular hemorrhages are highly specific for AHT |
| Colombari et al. [38] | Review | - | Radiological and neuropathological spinal cord examination | Spinal blood collection is the most indicative finding in AHT. |
| Maiese et al. [39] | Systematic review | 49 studies | Clinical and forensic investigations | circumstantial data, post-mortem radiological examinations, autopsy, and histological examination of the eye and brain play an important role |
| Oruç et al. [20] | Retrospective study | 8 | Clinical and radiological analysis | The main associated findings were: male sex, trauma perpetrated by the father, bilateral retinal hemorrhage |
| Messing-Jünger et al. [40] | Case report | 1 | Clinical and radiological analysis | massive bilateral retinal bleedings, fracture of the femur, left SDH |
| Unuma et al. [41] | Case report | 1 | Autopsy and post-mortem histological examination | Subdural hematoma, retinal hemorrhage, and encephalopathy without fractures were present but post-mortem examination revealed acute lymphoblastic leukemia |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sacco, M.A.; Gualtieri, S.; Tarda, L.; Ricci, P.; Aquila, I. Clinical and Forensic Investigation Protocols for Diagnosing Abusive Head Trauma: A Literature Review. Diagnostics 2023, 13, 3093. https://doi.org/10.3390/diagnostics13193093
Sacco MA, Gualtieri S, Tarda L, Ricci P, Aquila I. Clinical and Forensic Investigation Protocols for Diagnosing Abusive Head Trauma: A Literature Review. Diagnostics. 2023; 13(19):3093. https://doi.org/10.3390/diagnostics13193093
Chicago/Turabian StyleSacco, Matteo Antonio, Saverio Gualtieri, Lucia Tarda, Pietrantonio Ricci, and Isabella Aquila. 2023. "Clinical and Forensic Investigation Protocols for Diagnosing Abusive Head Trauma: A Literature Review" Diagnostics 13, no. 19: 3093. https://doi.org/10.3390/diagnostics13193093
APA StyleSacco, M. A., Gualtieri, S., Tarda, L., Ricci, P., & Aquila, I. (2023). Clinical and Forensic Investigation Protocols for Diagnosing Abusive Head Trauma: A Literature Review. Diagnostics, 13(19), 3093. https://doi.org/10.3390/diagnostics13193093








