A New Classification of the Morphology of Complete Ponticulus Posticus on Cone Beam Computed Tomography
Abstract
1. Introduction
2. Materials and Methods
2.1. Searching Strategy
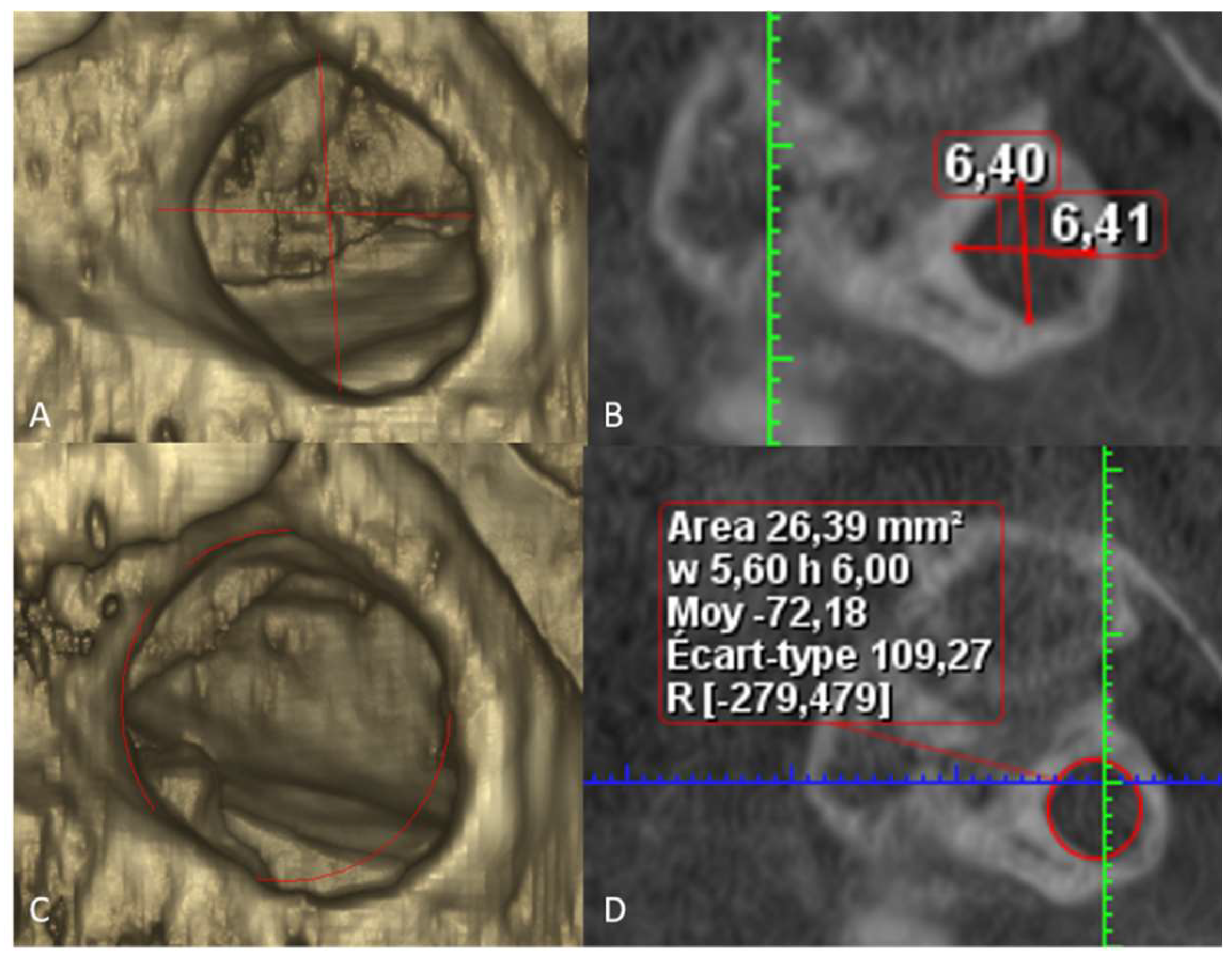
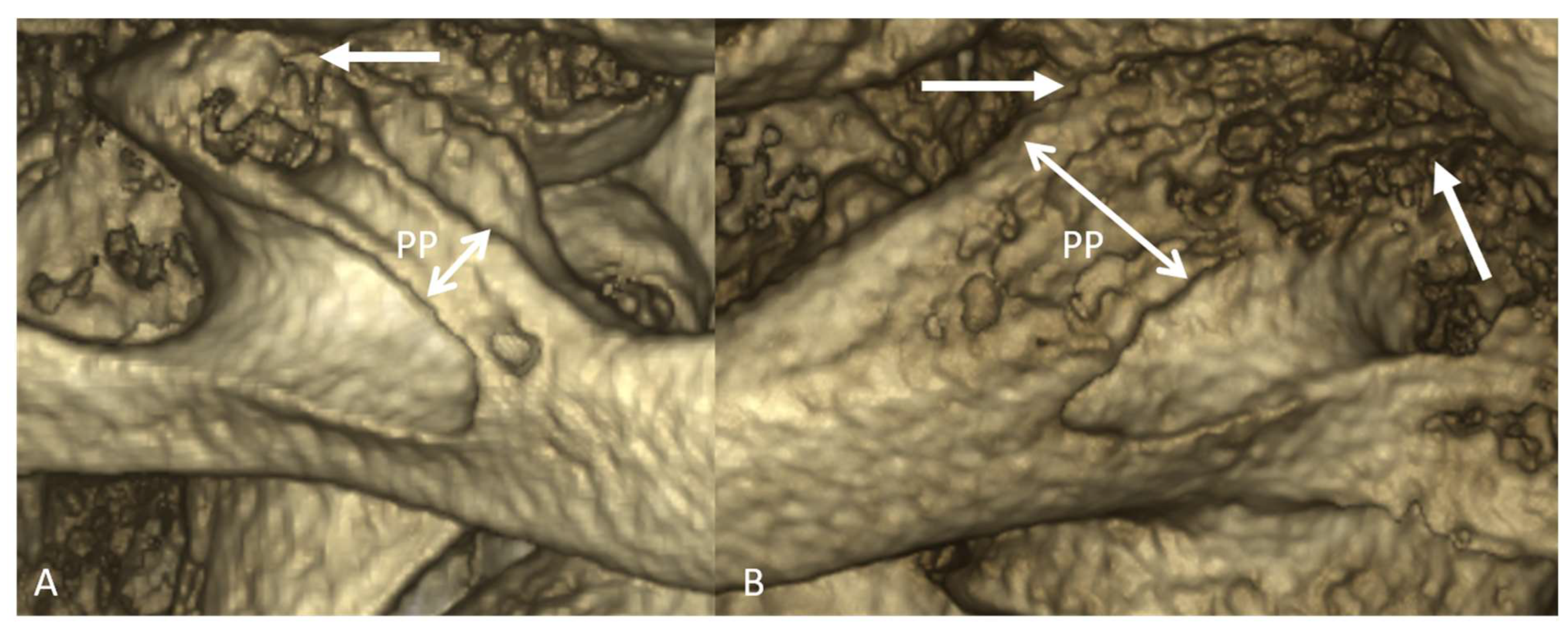
2.2. Measurement Methodology
2.3. Classification Definition
2.4. Statistics Methods
3. Results
3.1. Descriptive Statistics
3.2. Analytic Statistics
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kuhta, P.; Hart, J.; Greene-Orndorff, L.; McDowell-Reizer, B.; Rush, P. The Prevalence of Posticus Ponticus: Retrospective Analysis of Radiographs from a Chiropractic Health Center. J. Chiropr. Med. 2010, 9, 162–165. [Google Scholar] [CrossRef][Green Version]
- Evirgen, Ş.; Yüksel, H.T.; Yüksel, G.; Kaki, B.; Kamburoğlu, K. Assessment of Intravertebral Pneumatocysts, Degenerative Joint Disease, and Ponticulus Posticus in the Cervical Spine Through Cone Beam Computed Tomography Examination. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2020, 129, 531–538. [Google Scholar] [CrossRef]
- Polat, E.; Orhan, K. Examination of Incidental Intra-cranial and Extra-cranial Head and Neck Calcifications Using Cone-beam Computed Tomography. J. Stomatol. 2022, 75, 222–230. [Google Scholar] [CrossRef]
- Macrì, M.; Perrella, G.; Varvara, G.; Murmura, G.; Traini, T.; Rendina, F.; Festa, F. Assessments of Prevalence of Ponticulus Posticus, Atlas Posterior Arch Deficiency, Sella Turcica Bridging, Maxillary Canine Impaction, and Associations Among Them in 500 CBCTs of Italian Orthodontic Patients. Front. Dent. Med. 2021, 2, 708169. [Google Scholar] [CrossRef]
- Sekerci, A.E.; Soylu, E.; Arikan, M.P.; Ozcan, G.; Amuk, M.; Kocoglu, F. Prevalence and Morphologic Characteristics of Ponticulus Posticus: Analysis Using Cone-beam Computed Tomography. J. Chiropr. Med. 2015, 14, 153–161. [Google Scholar] [CrossRef]
- Joshi, V.; Matsuda, Y.; Kimura, Y.; Araki, K.; Ishida, H. Evaluation of Prevalence and Characteristics of Ponticulus Posticus among Japanese Adults: A Comparative Study Between CBCT Imaging and Lateral Cephalogram. Orthod. Waves 2018, 77, 134–141. [Google Scholar] [CrossRef]
- Bayrakdar, S.; Miloğlu, Ö.; Yeşiltepe, S.; Yılmaz, A.B. Ponticulus Posticus in a Cohort of Orthodontic Children and Adolescent Patients with Different Sagittal Skeletal Anomalies: A Comparative Cone Beam Computed Tomography Investigation. Folia Morphol. 2017, 77, 65–71. [Google Scholar] [CrossRef]
- Hasani, M.; Shahidi, S.; Rashedi, V.; Hasani, M.; Hajiyan, K. Cone beam CT Study of Ponticulus Posticus: Prevalence, Characterictics. Biomed. Pharmacol. J. 2016, 9, 1067–1072. [Google Scholar] [CrossRef]
- Afsharpour, S.; Hoiriis, K.T.; Fox, R.B.; Demons, S. An Anatomical Study of Arcuate Foramen and its Clinical Implications: A Case Report. Chiropr. Man. Ther. 2016, 24, 4. [Google Scholar] [CrossRef] [PubMed]
- Sekerci, A.E.; Soylu, E.; Arikan, M.P.; Aglarci, O.S. Is There a Relationship Between the Presence of Ponticulus Posticus and Elongated Styloid Process? Clin. Imaging 2015, 39, 220–224. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.H.; Chen, Y.K.; Wang, C.K. Prevalence of Ponticuli Posticus among Patients Referred for Dental Examinations by Cone-beam CT. Spine J. 2015, 15, 1270–1276. [Google Scholar] [CrossRef]
- Tripodi, D.; Tieri, M.; Demartis, P.; Pero, G.; Marzo, G.; D’Ercole, S. Ponticulus Posticus: Clinical and CBCT Analysis in a Young Italian Population. Eur. J. Paediatr. Dent. 2019, 20, 219–223. [Google Scholar]
- Sabir, H.; Kumbhare, S.; Rout, P. Evaluation of Ponticulus Posticus on Digital Lateral Cephalograms and Cone Beam Computed Tomography in Patients with Migraine and Healthy Individuals: A Comparative Study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2014, 118, 348–354. [Google Scholar] [CrossRef]
- Bayrakdar, İ.Ş.; Yasa, Y.; Duman, Ş.B.; Karaturgut, U.E.; Ocak, A.; Günen Yılmaz, S. Cone Beam Computed Tomography Evaluation of Ponticulus Posticus in Patients with Cleft Lip and Palate: A Retrospective Radio-anatomic Study. Folia Morphol. 2018, 77, 72–78. [Google Scholar] [CrossRef]
- Bayrakdar, I.S.; Miloglu, O.; Altun, O.; Gumussoy, I.; Durna, D.; Yilmaz, A.B. Cone beam Computed Tomography Imaging of Ponticulus Posticus: Prevalence, Characteristics, and a Review of the Literature. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2014, 118, e210–e219. [Google Scholar] [CrossRef]
- Buyuk, S.K.; Sekerci, A.E.; Benkli, Y.A.; Ekizer, A. A survey of ponticulus posticus: Radiological Analysis of Atlas in an Orthodontic Population Based on Cone-beam Computed Tomography. Niger. J. Clin. Pract. 2017, 20, 106–110. [Google Scholar] [CrossRef]
- Geist, J.R.; Geist, S.M.; Lin, L.M. A Cone beam CT Investigation of Ponticulus Posticus and Lateralis in Children and Adolescents. Dentomaxillofac. Radiol. 2014, 43, 20130451. [Google Scholar] [CrossRef]
- Elliott, R.E.; Tanweer, O. The Prevalence of the Ponticulus Posticus (Arcuate Foramen) and its Importance in the Goel-Harms Procedure: Meta-analysis and Review of the Literature. World Neurosurg. 2014, 82, 335–343. [Google Scholar] [CrossRef]
- Pękala, P.A.; Henry, B.M.; Pękala, J.R.; Hsieh, W.C.; Vikse, J.; Sanna, B.; Walocha, J.A.; Tubbs, R.S.; Tomaszewski, K.A. Prevalence of Foramen Arcuale and its Clinical Significance: A Meta-analysis of 55,985 Subjects. J. Neurosurg. 2017, 27, 276–290. [Google Scholar] [CrossRef]
- Mitchell, J. The Incidence and Dimensions of the Retroarticular Canal of the Atlas Vertebra. Acta Anat. 1998, 163, 113–120. [Google Scholar] [CrossRef]
- Padovan, L.; Ulbricht, V.; Groppo, F.C.; Sarmento Pereira Neto, J.; Moreira Andrade, V.; Francesquini Júnior, L. Sexual Dimorphism Through the Study of Atlas Vertebra in the Brazilian Population. J. Forensic Dent. Sci. 2019, 11, 158–162. [Google Scholar] [PubMed]
- Carter, L.; Farman, A.G.; Geist, J.; Scarfe, W.C.; Angelopoulos, C.; Nair, M.K.; Hildebolt, C.F.; Tyndall, D.; Shrout, M. American Academy of Oral and Maxillofacial Radiology Executive Opinion Statement on Performing and Interpreting Diagnostic Cone Beam Computed Tomography. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2008, 106, 561–562. [Google Scholar] [CrossRef] [PubMed]
- Horner, K.; Islam, M.; Flygare, L.; Tsiklakis, K.; Whaites, E. Basic Principles for Use of Dental Cone Beam Computed Tomography: Consensus Guidelines of the European Academy of Dental and Maxillofacial Radiology. Dentomaxillofac. Radiol. 2009, 38, 187–195. [Google Scholar] [CrossRef] [PubMed]
- Scarfe, W.C.; Li, Z.; Aboelmaaty, W.; Scott, S.A.; Farman, A.G. Maxillofacial Cone Beam Computed Tomography: Essence, Elements and Steps to Interpretation. Aust. Dent. J. 2012, 57 (Suppl. S1), 46–60. [Google Scholar] [CrossRef] [PubMed]
| Thin | Thick | p-Value | |
|---|---|---|---|
| Age in years (mean ± SD) | 50.5 ± 21.6 | 45.4 ± 21.2 | 0.0633 |
| Gender (F/M) | 63/46 | 57/85 | 0.0054 * |
| Side (L/R) | 58/51 | 72/70 | 0.07 |
| Hight in mm (mean ± SD) | 6.7 ± 1.1 | 6.5 ± 1.0 | 0.15 |
| Width in mm (mean ± SD) | 7.5 ± 1.1 | 7.3 ± 0.9 | 0.24 |
| Area in mm2 | 32.8 ± 7.9 | 31.5 ± 7.1 | 0.18 |
| Unilateral | Bilateral | p-Value | |
|---|---|---|---|
| Age in years (mean ± SD) | 47.1 ± 21.2 | 47.8 ± 22.0 | 0.83 |
| Gender (F/M) | 68/63 | 26/35 | 0.23 |
| Morphology (Thin/Thick) | 68/63 | 41/79 | 0.0045 * |
| Hight in mm (mean ± SD) | 6.5 ± 1.1 | 6.7 ± 1.0 | 0.17 |
| Width in mm (mean ± SD) | 7.4 ± 1.0 | 7.4 ± 1.0 | 0.72 |
| Area in mm2 | 32.0 ± 7.9 | 32.1 ± 7.0 | 0.84 |
| Author, Year of Publication | Country | CBCT Scans | Number of Complete PP in the Study | Prevalence (%) of Complete PP | Unilateral/Bilateral |
|---|---|---|---|---|---|
| Geist et al., 2014 [17] | USA | 576 | 60 | 10.41 | No information |
| Bayrakdar et al., 2014 [15] | Turkey | 730 | 70 | 9.58 | 48/79 |
| Sabir et al., 2014 [13] | India | 200 | 17 | 8.5 | 13/4 |
| Chen et al., 2015 [11] | Taiwan | 500 | 23 | 4.60 | 20/3 |
| Sekerci et al., 2015 [5] | Turkey | 698 | 112 | 16.04 | 68/44 |
| Sekerci et al., 2015 [10] | Turkey | 542 | 70 | 12.91 | 34/36 |
| Hasani et al., 2016 [8] | Iran | 260 | 21 | 8.07 | 15/6 |
| Buyuk et al., 2017 [16] | Turkey | 374 | 40 | 10.69 | 21/19 |
| Bayrakdar et al., 2017 [7] | Turkey | 181 | 16 | 8.83 | 9/7 |
| Joshi et al., 2018 [6] | Japan | 30 | No information | No information | 10/unknown |
| Bayrakdar et al., 2018 [14] | Turkey | 54 (CLP) *, 108 (control group) | 4 (CLP), 4 (control group) | 7.40 (CLP), 3.70 (control group) | 2/2 CLP, 2/2 control group |
| Tripodi et at., 2019 [12] | Italy | 524 | 24 | 4.58 | 7/17 |
| Evigren et al., 2020 [2] | Turkey | 440 | 55 (left), 63 (right) | 12.5 (left), 14.30 (right) | 118/unknown |
| Macri et al., 2021 [4] | Italy | 500 | 42 | 8.4 | 18/24 |
| Polat et al., 2022 [3] | Turkey | 171 | 15 | 8.77 | No information |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Olszewski, R.; Issa, J.; Odri, G.-A. A New Classification of the Morphology of Complete Ponticulus Posticus on Cone Beam Computed Tomography. Diagnostics 2023, 13, 3009. https://doi.org/10.3390/diagnostics13183009
Olszewski R, Issa J, Odri G-A. A New Classification of the Morphology of Complete Ponticulus Posticus on Cone Beam Computed Tomography. Diagnostics. 2023; 13(18):3009. https://doi.org/10.3390/diagnostics13183009
Chicago/Turabian StyleOlszewski, Raphael, Julien Issa, and Guillaume-Anthony Odri. 2023. "A New Classification of the Morphology of Complete Ponticulus Posticus on Cone Beam Computed Tomography" Diagnostics 13, no. 18: 3009. https://doi.org/10.3390/diagnostics13183009
APA StyleOlszewski, R., Issa, J., & Odri, G.-A. (2023). A New Classification of the Morphology of Complete Ponticulus Posticus on Cone Beam Computed Tomography. Diagnostics, 13(18), 3009. https://doi.org/10.3390/diagnostics13183009







