Simple Point-of-Care Nucleic Acid Amplification Test for Rapid SARS-CoV-2 Infection Diagnosis
Abstract
:1. Introduction
2. Materials and Methods
2.1. SARS-CoV-2 and Clinical Samples
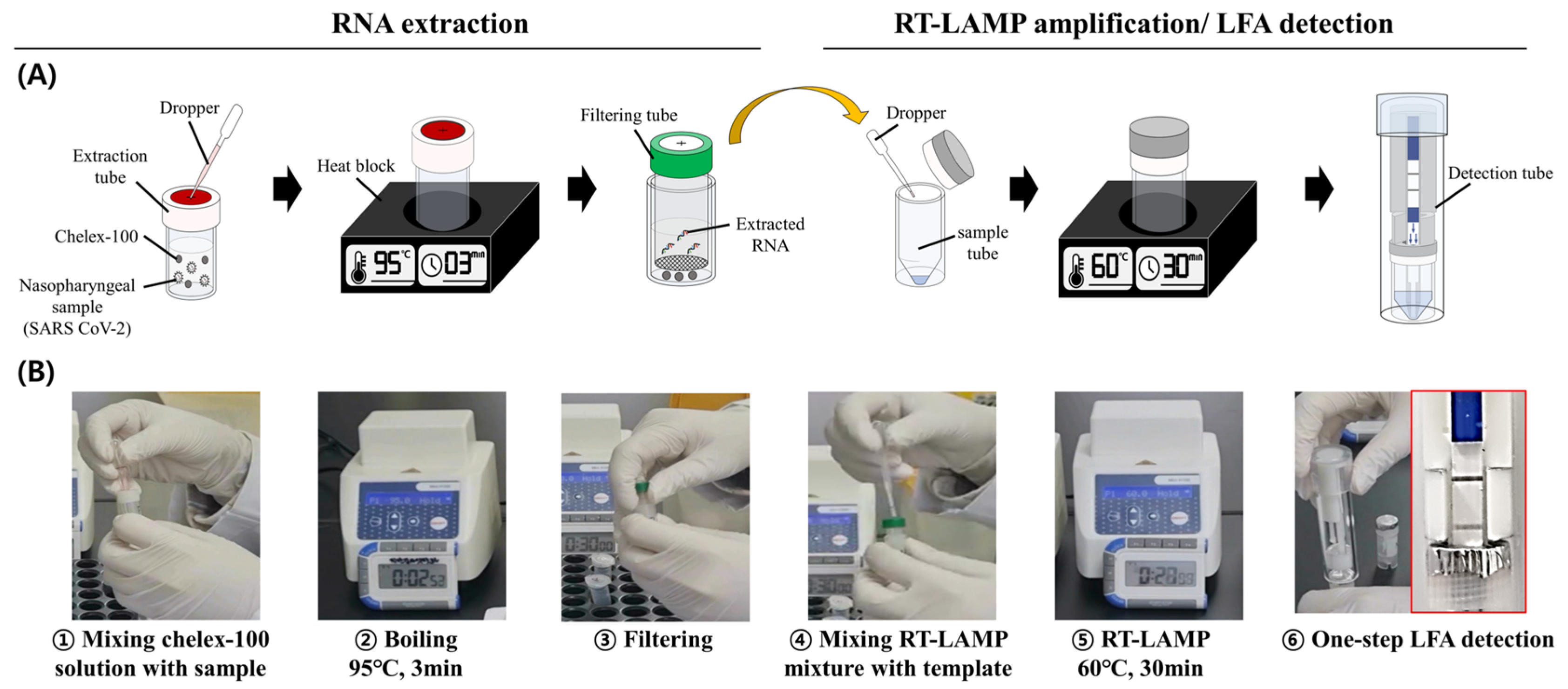
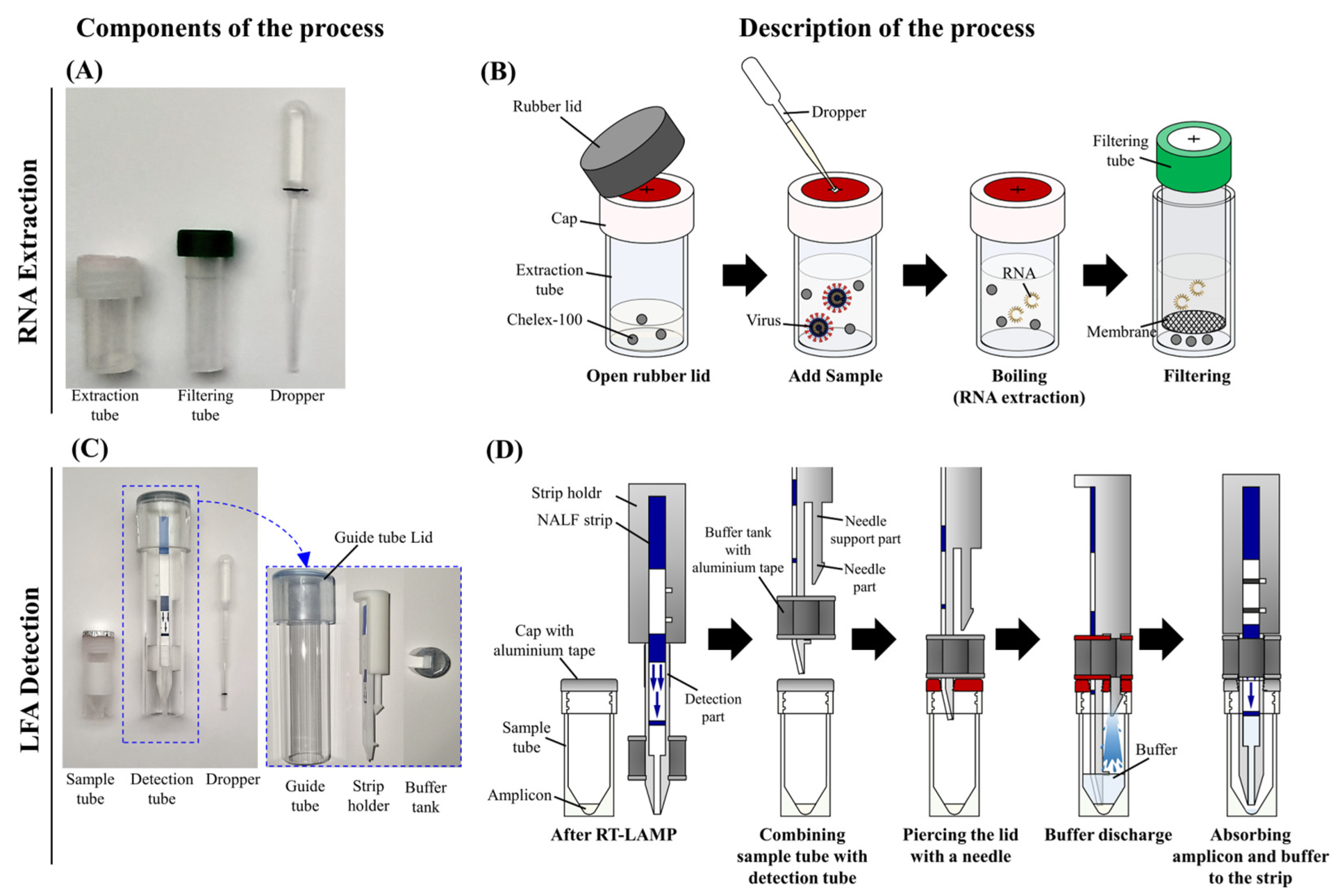
2.2. RNA Extraction
2.3. Design of a One-Step Amplification-Detection Device for the Rapid SARS-CoV-2 RT-LAMP-LFA Kit
2.4. Real-Time RT-qPCR and RT-LAMP
2.5. Limit of Detection (LOD) Tests
3. Results
3.1. Rapid SARS-CoV-2 RT-LAMP-LFA Kit
3.2. Performances of the Chelex-100/Boiling Nucleic Acid Extraction Device
3.3. Clinical Performance of the Rapid SARS-CoV-2 RT-LAMP-LFA Kit
3.4. Cross-Reactivity Test
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lu, R.; Zhao, X.; Li, J.; Niu, P.; Yang, B.; Wu, H.; Wang, W.; Song, H.; Huang, B.; Zhu, N.; et al. Genomic Characterisation and Epidemiology of 2019 Novel Coronavirus: Implications for Virus Origins and Receptor Binding. Lancet 2020, 395, 565–574. [Google Scholar] [CrossRef] [PubMed]
- Bharadwaj, M.; Bengtson, M.; Golverdingen, M.; Waling, L.; Dekker, C. Diagnosing point-of-care diagnostics for neglected tropical diseases. PLoS Negl. Trop. Dis. 2021, 15, e0009405. [Google Scholar] [CrossRef] [PubMed]
- Yan, Y.; Chang, L.; Wang, L. Laboratory Testing of SARS-CoV, MERS-CoV, and SARS-CoV-2 (2019-nCoV): Current Status, Challenges, and Countermeasures. Rev. Med. Virol. 2020, 30, e2106. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.-J.; Rai, C.-I.; Wang, S.-C.; Chen, Y.-C. Point-of-Care Testing for Infectious Diseases Based on Class 2 CRISPR/Cas Technology. Diagnostics 2023, 13, 2255. [Google Scholar] [CrossRef]
- Mak, G.C.; Cheng, P.K.; Lau, S.S.; Wong, K.K.; Lau, C.; Lam, E.T.; Chan, R.C.; Tsang, D.N. Evaluation of Rapid Antigen Test for Detection of SARS-CoV-2 Virus. J. Clin. Virol. 2020, 129, 104500. [Google Scholar] [CrossRef]
- Shirato, K.; Yano, T.; Senba, S.; Akachi, S.; Kobayashi, T.; Nishinaka, T.; Notomi, T.; Matsuyama, S. Detection of Middle East Respiratory Syndrome Coronavirus Using Reverse Transcription Loop-Mediated Isothermal Amplification (RT-LAMP). Virol. J. 2014, 11, 139. [Google Scholar] [CrossRef]
- Yan, C.; Cui, J.; Huang, L.; Du, B.; Chen, L.; Xue, G.; Li, S.; Zhang, W.; Zhao, L.; Sun, Y.; et al. Rapid and Visual Detection of 2019 Novel Coronavirus (SARS-CoV-2) by a Reverse Transcription Loop-Mediated Isothermal Amplification Assay. Clin. Microbiol. Infect. 2020, 26, 773–779. [Google Scholar] [CrossRef]
- Park, G.-S.; Ku, K.; Baek, S.-H.; Kim, S.-J.; Kim, S.I.; Kim, B.-T.; Maeng, J.-S. Development of Reverse Transcription Loop-Mediated Isothermal Amplification Assays Targeting Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). J. Mol. Diagn. 2020, 22, 729–735. [Google Scholar] [CrossRef]
- Walker, G.T.; Fraiser, M.S.; Schram, J.L.; Little, M.C.; Nadeau, J.G.; Malinowski, D.P. Strand Displacement Amplification—An Isothermal, in Vitro DNA Amplification Technique. Nucleic Acids Res. 1992, 20, 1691–1696. [Google Scholar] [CrossRef]
- Vincent, M.; Xu, Y.; Kong, H. Helicase-Dependent Isothermal DNA Amplification. EMBO Rep. 2004, 5, 795–800. [Google Scholar] [CrossRef]
- Piepenburg, O.; Williams, C.H.; Stemple, D.L.; Armes, N.A. DNA Detection Using Recombination Proteins. PLoS Biol. 2006, 4, e204. [Google Scholar] [CrossRef] [PubMed]
- Notomi, T. Loop-Mediated Isothermal Amplification of DNA. Nucleic Acids Res. 2000, 28, e63. [Google Scholar] [CrossRef] [PubMed]
- Mori, Y.; Notomi, T. Loop-Mediated Isothermal Amplification (LAMP): A Rapid, Accurate, and Cost-Effective Diagnostic Method for Infectious Diseases. J. Infect. Chemother. 2009, 15, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Gill, P.; Ghaemi, A. Nucleic Acid Isothermal Amplification Technologies—A Review. Nucleosides Nucleotides Nucleic Acids 2008, 27, 224–243. [Google Scholar] [CrossRef]
- Maeda, H.; Kokeguchi, S.; Fujimoto, C.; Tanimoto, I.; Yoshizumi, W.; Nishimura, F.; Takashiba, S. Detection of Periodontal Pathogen Porphyromonas Gingivalis by Loop-Mediated Isothermal Amplification Method. FEMS Immunol. Med. Microbiol. 2005, 43, 233–239. [Google Scholar] [CrossRef]
- Fischbach, J.; Xander, N.C.; Frohme, M.; Glökler, J.F. Shining a Light on LAMP Assays’ A Comparison of LAMP Visualization Methods Including the Novel Use of Berberine. Biotechniques 2015, 58, 189–194. [Google Scholar] [CrossRef]
- Goto, M.; Honda, E.; Ogura, A.; Nomoto, A.; Hanaki, K.-I. Colorimetric Detection of Loop-Mediated Isothermal Amplification Reaction by Using Hydroxy Naphthol Blue. Biotechniques 2009, 46, 167–172. [Google Scholar] [CrossRef]
- Kiatpathomchai, W.; Jaroenram, W.; Arunrut, N.; Jitrapakdee, S.; Flegel, T.W. Shrimp Taura Syndrome Virus Detection by Reverse Transcription Loop-Mediated Isothermal Amplification Combined with a Lateral Flow Dipstick. J. Virol. Methods 2008, 153, 214–217. [Google Scholar] [CrossRef]
- Donato, L.J.; Myhre, N.K.; Murray, M.A.; McDonah, M.R.; Myers, J.F.; Maxson, J.A.; Meek, A.M.; Espy, M.J.; Furst, J.W.; Karon, B.S.; et al. Assessment of Test Performance and Potential for Environmental Contamination Associated with a Point-of-Care Molecular Assay for Group A Streptococcus in an End User Setting. J. Clin. Microbiol. 2019, 57, 10-1128. [Google Scholar] [CrossRef]
- Binnicker, M.J.; Espy, M.J.; Irish, C.L.; Vetter, E.A. Direct Detection of Influenza A and B Viruses in Less Than 20 Minutes Using a Commercially Available Rapid PCR Assay. J. Clin. Microbiol. 2015, 53, 2353–2354. [Google Scholar] [CrossRef]
- Odiwuor, N.; Xiong, J.; Ogolla, F.; Hong, W.; Li, X.; Khan, F.M.; Wang, N.; Yu, J.; Wei, H. A Point-of-Care SARS-CoV-2 Test Based on Reverse Transcription Loop-Mediated Isothermal Amplification without RNA Extraction with Diagnostic Performance Same as RT-PCR. Anal. Chim. Acta 2022, 1200, 339590. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Zheng, T.; Wang, H.; Chen, W.; Huang, X.; Liang, J.; Qiu, L.; Han, D.; Tan, W. Rapid One-Pot Detection of SARS-CoV-2 Based on a Lateral Flow Assay in Clinical Samples. Anal. Chem. 2021, 93, 3325–3330. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.; Lin, H.; Feng, X.; Lui, G.C.Y.; Hsing, I.-M. Disposable and Low-Cost Pen-like Sensor Incorporating Nucleic-Acid Amplification Based Lateral-Flow Assay for at-Home Tests of Communicable Pathogens. Biosens. Bioelectron. X 2022, 12, 100248. [Google Scholar] [CrossRef]
- Lim, D.H.; Jee, H.; Moon, K.C.; Lim, C.S.; Jang, W.S. Development of a Simple DNA Extraction Method and Candida Pan Loop-Mediated Isothermal Amplification Assay for Diagnosis of Candidemia. Pathogens 2022, 11, 111. [Google Scholar] [CrossRef] [PubMed]
- Jang, W.S.; Lim, D.H.; Yoon, J.; Kim, A.; Lim, M.; Nam, J.; Yanagihara, R.; Ryu, S.W.; Jung, B.K.; Ryoo, N.H.; et al. Development of a Multiplex Loop-Mediated Isothermal Amplification (LAMP) Assay for Onsite Diagnosis of SARS-CoV-2. PLoS ONE 2021, 16, e0248042. [Google Scholar] [CrossRef] [PubMed]
- Perry, D.J.; Fitzmaurice, D.A.; Kitchen, S.; Mackie, I.J.; Mallett, S. Point-of-Care Testing in Haemostasis. Br. J. Haematol. 2010, 150, 501–514. [Google Scholar] [CrossRef] [PubMed]
- Pai, N.P.; Vadnais, C.; Denkinger, C.; Engel, N.; Pai, M. Point-of-Care Testing for Infectious Diseases: Diversity, Complexity, and Barriers in Low- And Middle-Income Countries. PLoS Med. 2012, 9, e1001306. [Google Scholar] [CrossRef]
- Zhu, C.; Hu, A.; Cui, J.; Yang, K.; Zhu, X.; Liu, Y.; Deng, G.; Zhu, L. A Lab-on-a-Chip Device Integrated DNA Extraction and Solid Phase PCR Array for the Genotyping of High-Risk HPV in Clinical Samples. Micromachines 2019, 10, 537. [Google Scholar] [CrossRef]
- Yin, K.; Ding, X.; Xu, Z.; Li, Z.; Wang, X.; Zhao, H.; Otis, C.; Li, B.; Liu, C. Multiplexed Colorimetric Detection of SARS-CoV-2 and Other Pathogens in Wastewater on a 3D Printed Integrated Microfluidic Chip. Sens. Actuators B Chem. 2021, 344, 130242. [Google Scholar] [CrossRef]
- Mautner, L.; Baillie, C.-K.; Herold, H.M.; Volkwein, W.; Guertler, P.; Eberle, U.; Ackermann, N.; Sing, A.; Pavlovic, M.; Goerlich, O.; et al. Rapid Point-of-Care Detection of SARS-CoV-2 Using Reverse Transcription Loop-Mediated Isothermal Amplification (RT-LAMP). Virol. J. 2020, 17, 160. [Google Scholar] [CrossRef]
- World Health Organization. COVID-19 Target Product Profiles for Priority Diagnostics to Support Response to the COVID-19 Pandemic v.1.0; World Health Organization: Geneva, Switzerland, 2020.
- Freire-Paspuel, B.; Garcia-Bereguiain, M.A. Analytical and Clinical Evaluation of “AccuPower SARS-CoV-2 Multiplex RT-PCR Kit (Bioneer, Republic of Korea)” and “Allplex 2019-NCoV Assay (Seegene, Republic of Korea)” for SARS-CoV-2 RT-PCR Diagnosis: Korean CDC EUA as a Quality Control Proxy for Developing Countries. Front. Cell Infect. Microbiol. 2021, 11, 630552. [Google Scholar] [CrossRef]
- Pickering, S.; Batra, R.; Merrick, B.; Snell, L.B.; Nebbia, G.; Douthwaite, S.; Reid, F.; Patel, A.; Kia Ik, M.T.; Patel, B.; et al. Comparative Performance of SARS-CoV-2 Lateral Flow Antigen Tests and Association with Detection of Infectious Virus in Clinical Specimens: A Single-Centre Laboratory Evaluation Study. Lancet Microbe 2021, 2, e461–e471. [Google Scholar] [CrossRef] [PubMed]

| PFU mL−1 | Advansure TM E3 System | Chlex-100/Boiling Nucleic Acid Extraction | ||||
|---|---|---|---|---|---|---|
| Allplex ™ SARS-CoV-2 Assay | RT-LAMP Assay | RT-LAMP -LFA Kit | Allplex ™ SARS-CoV-2 Assay | RT-LAMP Assay | RT-LAMP -LFA Kit | |
| Ct 1 (SD 4) | Ct (SD) | Results | Ct (SD) | Ct (SD) | Results | |
| 1 × 103 | 22.57 ± 0.11 | 8.73 ± 1.27 | P 2 | 24.45 ± 0.40 | 11.29 ± 1.61 | P |
| 1 × 102 | 27.03 ± 0.69 | 9.91 ± 1.25 | P | 28.22 ± 0.71 | 11.92 ± 1.66 | P |
| 1 × 101 | 30.44 ± 0.29 | 10.85 ± 1.58 | P | 31.42 ± 0.52 | 13.50 ± 2.48 | P |
| 1 × 100 | 34.54 ± 0.60 | 13.09 ± 1.73 | P | 35.03 ± 0.84 | 18.38 ± 5.62 | P |
| 1 × 10−1 | 37.84 ± 0.52 | 21.27 ± 2.70 | P | N/A | N/A | N/A |
| 1 × 10−2 | N/A 3 | N/A | N/A | N/A | N/A | N/A |
| 1 × 10−3 | N/A | N/A | N/A | N/A | N/A | N/A |
| Assay | Infected (n = 92) | Non-Infected (n = 100) | PPV ** | NPV ** | ||
|---|---|---|---|---|---|---|
| P/N * | Sensitivity | P/N | Specificity | |||
| Allplex™ SARS-CoV-2 assay | 92/0 | 100% | 0/100 | 100% | 100% | 100% |
| SARS-CoV-2 RT-LAMP assay | 90/2 | 97.8% | 0/100 | 100% | 100% | 93.7% |
| Rapid SARS-CoV-2 RT-LAMP-LFA kit | 90/2 | 97.8% | 0/100 | 100% | 100% | 93.7% |
| Virus | Allplex™ SARS-CoV-2 Assay | SARS-CoV-2 RT-LAMP Assay | Rapid SARS-CoV-2 RT-LAMP-LFA Kit |
|---|---|---|---|
| P/N * | P/N | P/N | |
| CoV 229E | 0/3 | 0/3 | 0/3 |
| CoV NL63 | 0/3 | 0/3 | 0/3 |
| CoV OC43 | 0/3 | 0/3 | 0/3 |
| Inf A/H1N1 | 0/3 | 0/3 | 0/3 |
| Inf A/H3N2 | 0/3 | 0/3 | 0/3 |
| Inf B | 0/3 | 0/3 | 0/3 |
| RSV A | 0/3 | 0/3 | 0/3 |
| RSV B | 0/3 | 0/3 | 0/3 |
| PIV | 0/3 | 0/3 | 0/3 |
| AdV | 0/3 | 0/3 | 0/3 |
| HboV | 0/3 | 0/3 | 0/3 |
| HEV | 0/3 | 0/3 | 0/3 |
| HRV | 0/3 | 0/3 | 0/3 |
| MPV | 0/3 | 0/3 | 0/3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jee, H.; Choi, M.; Park, I.S.; Lee, J.; Jang, W.S.; Lim, C.S. Simple Point-of-Care Nucleic Acid Amplification Test for Rapid SARS-CoV-2 Infection Diagnosis. Diagnostics 2023, 13, 3001. https://doi.org/10.3390/diagnostics13183001
Jee H, Choi M, Park IS, Lee J, Jang WS, Lim CS. Simple Point-of-Care Nucleic Acid Amplification Test for Rapid SARS-CoV-2 Infection Diagnosis. Diagnostics. 2023; 13(18):3001. https://doi.org/10.3390/diagnostics13183001
Chicago/Turabian StyleJee, Hyunseul, Minkyeong Choi, In Su Park, Junmin Lee, Woong Sik Jang, and Chae Seung Lim. 2023. "Simple Point-of-Care Nucleic Acid Amplification Test for Rapid SARS-CoV-2 Infection Diagnosis" Diagnostics 13, no. 18: 3001. https://doi.org/10.3390/diagnostics13183001
APA StyleJee, H., Choi, M., Park, I. S., Lee, J., Jang, W. S., & Lim, C. S. (2023). Simple Point-of-Care Nucleic Acid Amplification Test for Rapid SARS-CoV-2 Infection Diagnosis. Diagnostics, 13(18), 3001. https://doi.org/10.3390/diagnostics13183001








