Tele-Mentored Handheld Ultrasound System for General Practitioners: A Prospective, Descriptive Study in Remote and Rural Communities
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants
2.3. Patients
2.4. Training Protocol
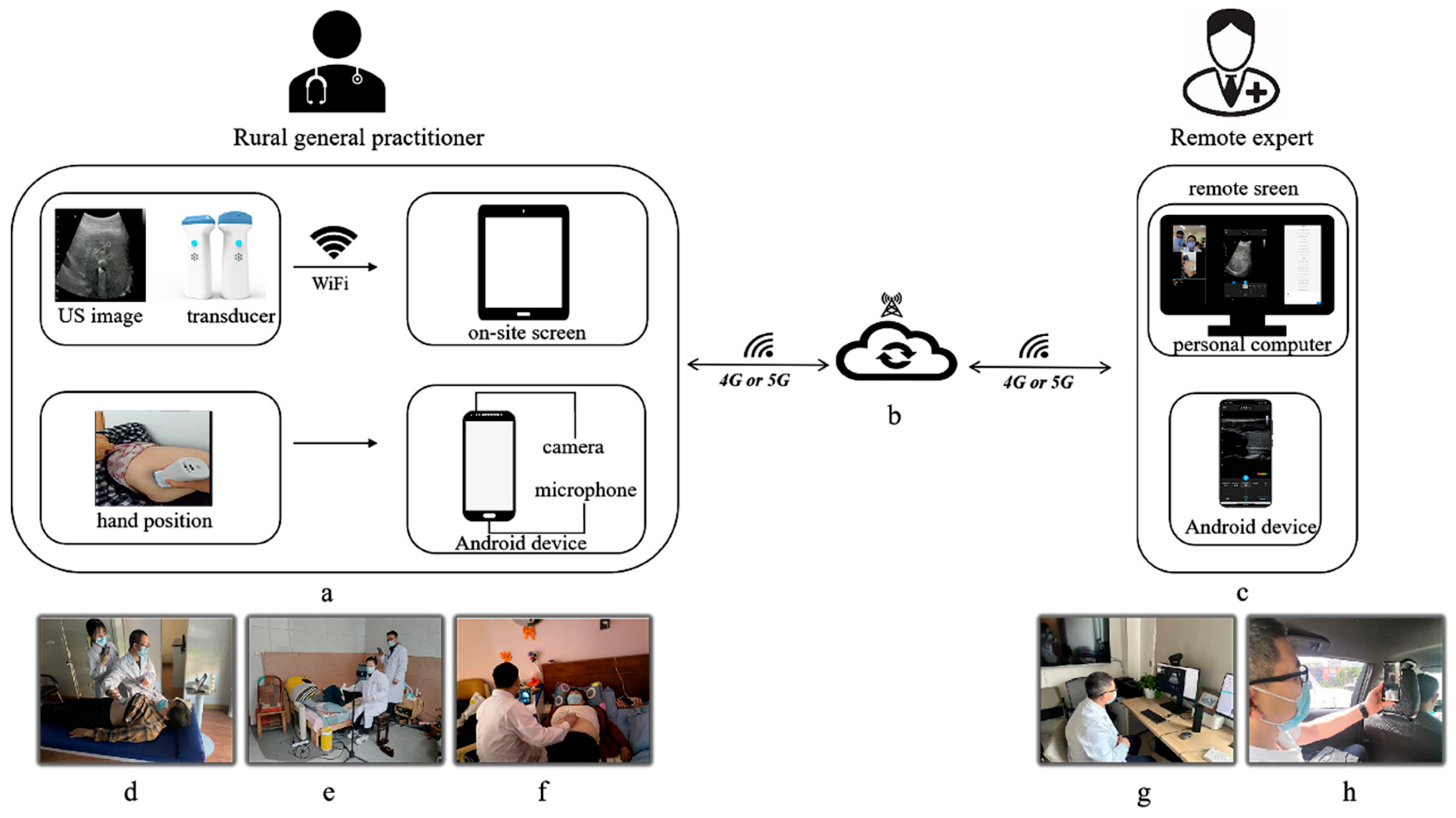
2.5. Tele-HHUS System
2.6. Scanning Procedure
2.7. Measurements and Outcomes
2.8. Statistical Analyses
3. Results
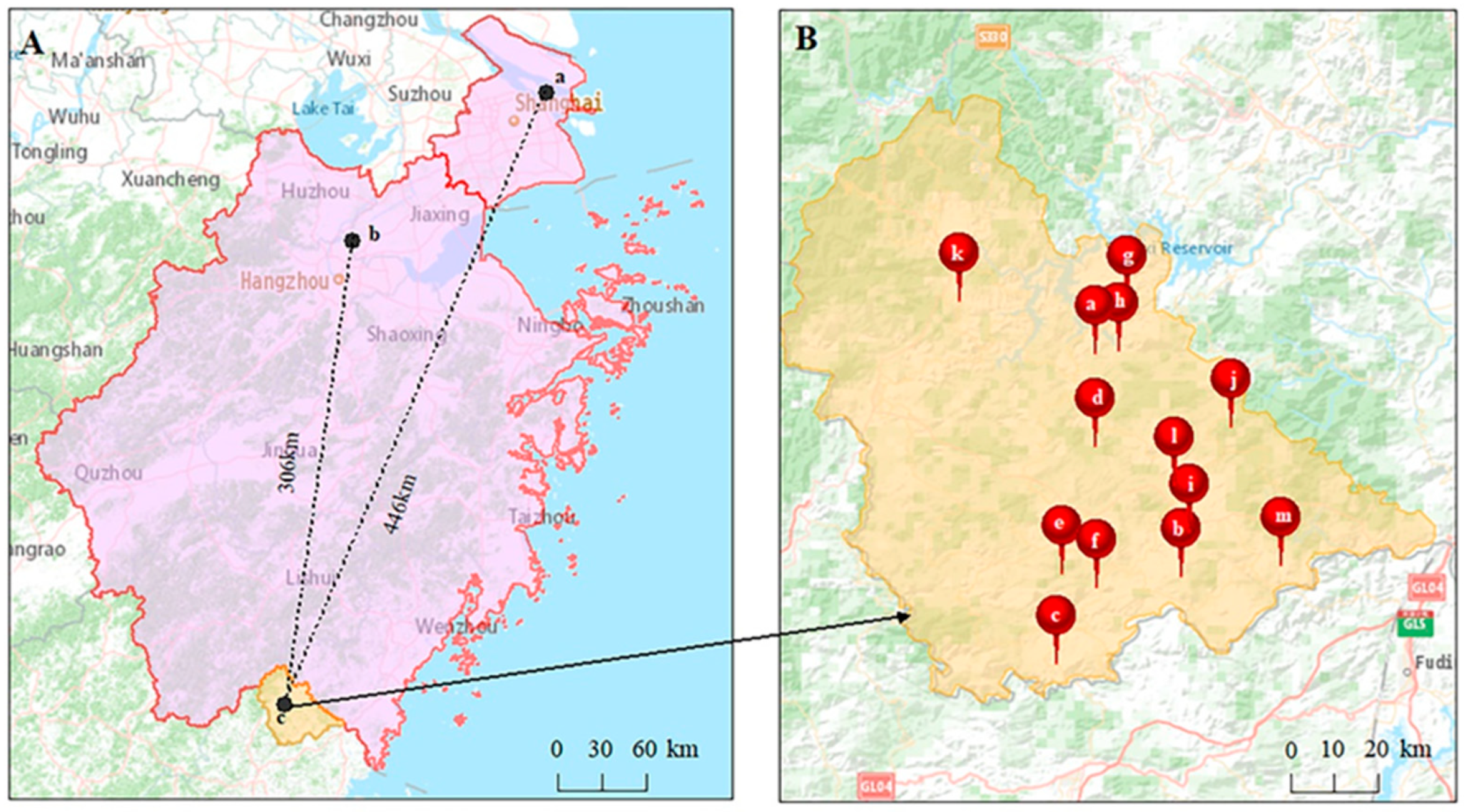
3.1. Patients and Locations of Tele-HHUS
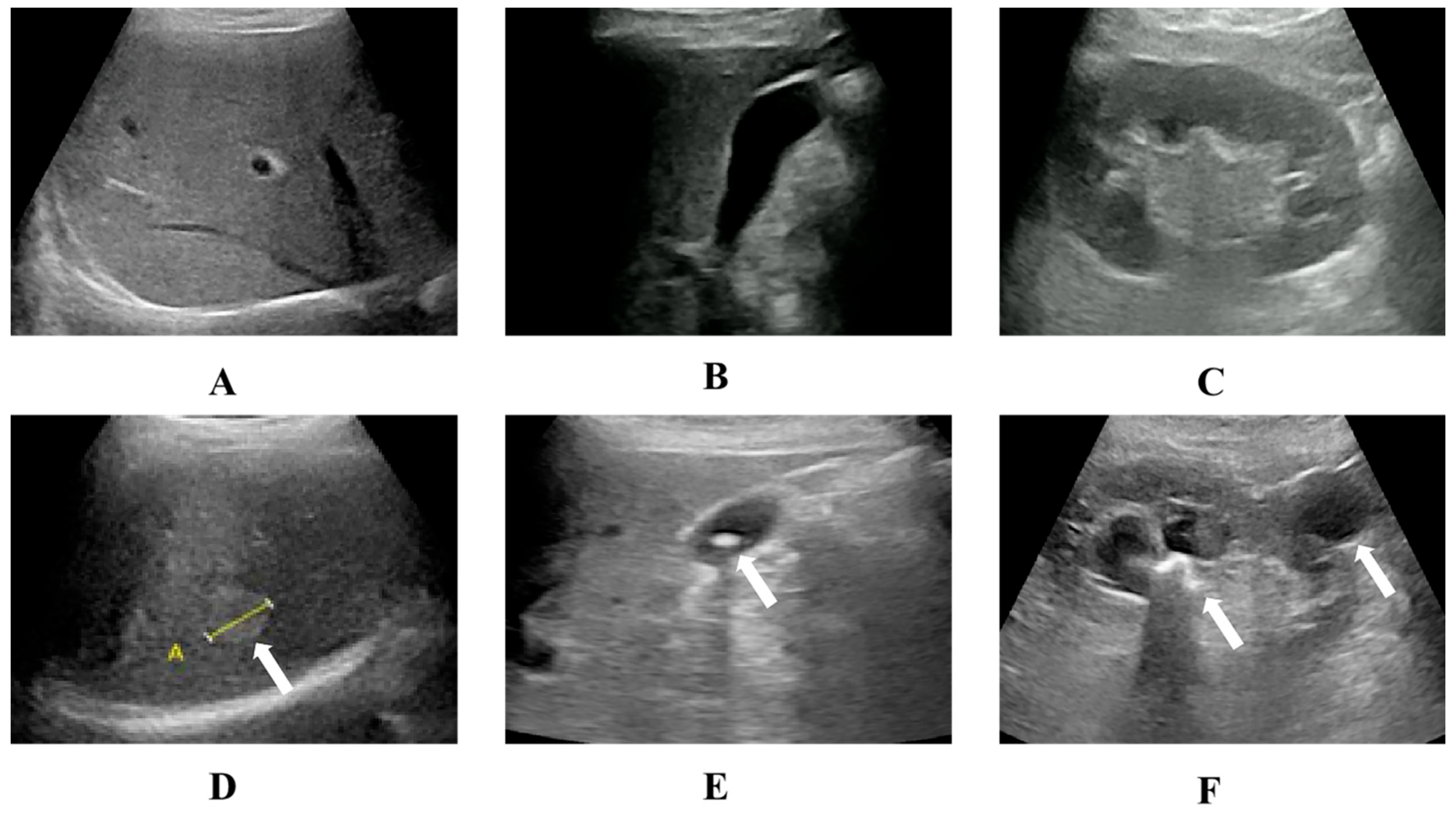
3.2. US Examinations and Results
3.3. Changes in the Treatment Plans
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Tele-HHUS | Tele-mentored handheld ultrasound; |
| HHUS | Handheld ultrasound; |
| US | Ultrasound; |
| GPs | General practitioners; |
| WHO | World Health Organization. |
Appendix A
- Full list of participants:
- Rural general practitioners:
- Fuzhuo Dong (Nanpuxi Town Lianyun Health Center);
- Shiliu Zhou (Zhuozhai Village Clinic);
- Minyun Shi (Shiyang Branch of Taishun County Hospital of Chinese Medicine);
- Shuting Zhang (Shiyang Branch of Taishun County Hospital of Chinese Medicine);
- Ningning Lei (Xiaocun Branch of Taishun County People’s Hospital);
- Yang Wang (Xiyang Town Health Center);
- Dongdong Lei (Sankui Branch of Taishun County People’s Hospital);
- Xiaoqian Jun (Sankui Branch of Taishun County People’s Hospital);
- Chenmeng Cai (Sankui Branch of Taishun County People’s Hospital);
- Qingqing Cai (Sankui Branch of Taishun County People’s Hospital);
- Hao Hong (Sankui Branch of Taishun County People’s Hospital);
- Chuanji Mei (Sankui Branch of Taishun County People’s Hospital);
- Yingxue Shu (Sankui Branch of Taishun County People’s Hospital);
- Chunyan Weng (Sankui Branch of Taishun County People’s Hospital);
- Xuejing Ye (Sankui Branch of Taishun County People’s Hospital);
- Shaobang Li (Baoyang Township Health Center);
- Zhangning Wu (Nanpuxi Town Health Center);
- Guangwu Wu (Nanpuxi Town Health Center);
- Deping Wang (Sixi Branch of Taishun County People’s Hospital);
- Xiuxiu Zeng (Pengxi Town Central Health Center);
- Limei Li (Pengxi Town Central Health Center);
- Hongzu Qiu (Pengxi Town Central Health Center);
- Jie Wang (Sixi Town Hengkeng Health Center);
- Saie Lei (Siqian Town Central Health Center);
- Li Lin (Siqian Town Central Health Center);
- Shiyong Luo (Siqian Town Central Health Center);
- Yi Wu (Siqian Town Central Health Center);
- YaTing Ji (Fengyang Branch of Taishun County People’s Hospital)
- Remote experts:
- Chengzhong Peng (Shanghai Tenth People’s Hospital);
- Huihui Chai (Shanghai Tenth People’s Hospital);
- Ruizhong Ye (Zhejiang Provincial People’s Hospital);
- Weinan Chen (Zhejiang Provincial People’s Hospital);
- Jianchun Li (Zhejiang Provincial People’s Hospital);
- Ceng Wang (Zhejiang Provincial People’s Hospital);
- Yanming Zhang (Zhejiang Provincial People’s Hospital);
- Lizhen Pan (Zhejiang Provincial People’s Hospital);
- Zezhou Song (Zhejiang Provincial People’s Hospital).
References
- World Health Organization. Aide-mémoire for Diagnostic Imaging Services. Available online: https://apps.who.int/iris/handle/10665/66695 (accessed on 17 June 2012).
- Epstein, D.; Petersiel, N.; Klein, E.; Marcusohn, E.; Aviran, E.; Harel, R.; Azzam, Z.S.; Neuberger, A.; Fuchs, L. Pocket-size point-of-care ultrasound in rural Uganda—A unique opportunity “to see”, where no imaging facilities are available. Travel Med. Infect. Dis. 2018, 23, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Burleson, S.L.; Swanson, J.F.; Shufflebarger, E.F.; Wallace, D.W.; Heimann, M.A.; Crosby, J.C.; Pigott, D.C.; Gullett, J.P.; Thompson, M.A.; Greene, C.J. Evaluation of a novel handheld point-of-care ultrasound device in an African emergency department. Ultrasound J. 2020, 12, 53. [Google Scholar] [CrossRef] [PubMed]
- Baribeau, Y.; Sharkey, A.; Chaudhary, O.; Krumm, S.; Fatima, H.; Mahmood, F.; Matyal, R. Handheld Point-of-Care Ultrasound Probes: The New Generation of POCUS. J. Cardiothorac. Vasc. Anesth. 2020, 34, 3139–3145. [Google Scholar] [CrossRef] [PubMed]
- Prager, R.; Sedgwick, C.; Lund, A.; Kim, D.; Ho, B.; Stachura, M.; Gutman, S. Prospective Evaluation of Point-of-Care Ultrasound at a Remote, Multi-Day Music Festival. Prehospital Disaster Med. 2018, 33, 484–489. [Google Scholar] [CrossRef] [PubMed]
- Cardim, N.; Dalen, H.; Voigt, J.U.; Ionescu, A.; Price, S.; Neskovic, A.N.; Edvardsen, T.; Galderisi, M.; Sicari, R.; Donal, E.; et al. The use of handheld ultrasound devices: A position statement of the European Association of Cardiovascular Imaging (2018 update). Eur. Heart J.-Cardiovasc. Imaging 2019, 20, 245–252. [Google Scholar] [CrossRef]
- Lo, H.; Frauendorf, V.; Wischke, S.; Schimmath-Deutrich, C.; Kersten, M.; Nuernberg, M.; Nuernberg, D.; Jenssen, C. Ambulatory Use of Handheld Point-of-Care Ultrasound (HH-POCUS) in Rural Brandenburg—A Pilot Study. Ultraschall Der Med.-Eur. J. Ultrasound 2022, 43, 584–591. [Google Scholar] [CrossRef]
- Sun, Y.K.; Li, X.L.; Wang, Q.; Zhou, B.Y.; Zhu, A.Q.; Qin, C.; Guo, L.H.; Xu, H.X. Improving the quality of breast ultrasound examination performed by inexperienced ultrasound doctors with synchronous tele-ultrasound: A prospective, parallel controlled trial. Ultrasonography 2022, 41, 307–316. [Google Scholar] [CrossRef]
- Li, X.L.; Sun, Y.K.; Wang, Q.; Chen, Z.T.; Qian, Z.B.; Guo, L.H.; Xu, H.X. Synchronous tele-ultrasonography is helpful for a naive operator to perform high-quality thyroid ultrasound examinations. Ultrasonography 2022, 41, 650–660. [Google Scholar] [CrossRef]
- Kaneko, T.; Kagiyama, N.; Nakamura, Y.; Hirasawa, T.; Murata, A.; Morimoto, R.; Miyazaki, S.; Minamino, T. Effectiveness of real-time tele-ultrasound for echocardiography in resource-limited medical teams. J. Echocardiogr. 2022, 20, 16–23. [Google Scholar] [CrossRef]
- Robertson, T.E.; Levine, A.R.; Verceles, A.C.; Buchner, J.A.; Lantry, J.H.; Papali, A.; Zubrow, M.T.; Colas, L.N.; Augustin, M.E.; McCurdy, M.T. Remote tele-mentored ultrasound for non-physician learners using FaceTime: A feasibility study in a low-income country. J. Crit. Care 2017, 40, 145–148. [Google Scholar] [CrossRef]
- Swanson, J.O.; Nathan, R.O.; Swanson, D.L.; Perez, K.M.; Bresnahan, B.W.; Mirza, W.; Goldenberg, R.L. Use of ultrasound and mHealth to improve perinatal outcomes in low and middle income countries. Semin. Perinatol. 2019, 43, 267–272. [Google Scholar] [CrossRef]
- Jemal, K.; Ayana, D.; Tadesse, F.; Adefris, M.; Awol, M.; Tesema, M.; Dagne, B.; Abeje, S.; Bantie, A.; Butler, M.; et al. Implementation and evaluation of a pilot antenatal ultrasound imaging programme using tele-ultrasound in Ethiopia. J. Telemed. Telecare 2022, 0, 1357633X221115746. [Google Scholar] [CrossRef]
- Frohlich, E.; Beller, K.; Muller, R.; Herrmann, M.; Debove, I.; Klinger, C.; Pauluschke-Frohlich, J.; Hoffmann, T.; Kreppenhofer, S.; Dietrich, C.F. Point of Care Ultrasound in Geriatric Patients: Prospective Evaluation of a Portable Handheld Ultrasound Device. Ultraschall Med.-Eur. J. Ultrasound 2020, 41, 308–316. [Google Scholar] [CrossRef]
- Britton, N.; Miller, M.A.; Safadi, S.; Siegel, A.; Levine, A.R.; McCurdy, M.T. Tele-Ultrasound in Resource-Limited Settings: A Systematic Review. Front. Public Health 2019, 7, 244. [Google Scholar] [CrossRef] [PubMed]
- Bhavnani, S.P.; Sola, S.; Adams, D.; Venkateshvaran, A.; Dash, P.K.; Sengupta, P.P.; Investigators, A.-V. A Randomized Trial of Pocket-Echocardiography Integrated Mobile Health Device Assessments in Modern Structural Heart Disease Clinics. JACC Cardiovasc. Imaging 2018, 11, 546–557. [Google Scholar] [CrossRef]
- Costantino, A.; Piagnani, A.; Nandi, N.; Sciola, V.; Maggioni, M.; Donato, F.; Vecchi, M.; Lampertico, P.; Casazza, G.; Fraquelli, M. Reproducibility and diagnostic accuracy of pocket-sized ultrasound devices in ruling out compensated cirrhosis of mixed etiology. Eur. Radiol. 2022, 32, 4609–4615. [Google Scholar] [CrossRef]
- Haji-Hassan, M.; Dutu, B.; Bolboaca, S.D. Handheld Echocardiography Measurements Concordance and Findings Agreement: An Exploratory Study. Diagnostics 2023, 13, 853. [Google Scholar] [CrossRef]
- Wastl, D.; Lowe, A.; Dietrich, C.F. Echoscopy in scanning cardiac diseases in critical care medicine. Med. Klin.-Intensivmed. Notfallmedizin 2023, 118, 293–300. [Google Scholar] [CrossRef]
- Wastl, D.; Lowe, A.; Dietrich, C.F. Echoscopy in scanning abdominal diseases in a critical care setting. Med. Klin.-Intensivmed. Notfallmedizin 2023, 118, 228–235. [Google Scholar] [CrossRef]
- Bhavnani, S.P.; Narula, J.; Sengupta, P.P. Mobile technology and the digitization of healthcare. Eur. Heart J. 2016, 37, 1428–1438. [Google Scholar] [CrossRef]
- Sim, I. Mobile Devices and Health. N. Engl. J. Med. 2019, 381, 956–968. [Google Scholar] [CrossRef]
- Evangelista, A.; Galuppo, V.; Mendez, J.; Evangelista, L.; Arpal, L.; Rubio, C.; Vergara, M.; Liceran, M.; Lopez, F.; Sales, C.; et al. Hand-held cardiac ultrasound screening performed by family doctors with remote expert support interpretation. Heart 2016, 102, 376–382. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Bansal, M.; Maheshwari, P.; Adams, D.; Sengupta, S.P.; Price, R.; Dantin, L.; Smith, M.; Kasliwal, R.R.; Pellikka, P.A.; et al. American Society of Echocardiography: Remote Echocardiography with Web-Based Assessments for Referrals at a Distance (ASE-REWARD) Study. J. Am. Soc. Echocardiogr. 2013, 26, 221–233. [Google Scholar] [CrossRef] [PubMed]
- Duan, S.; Liu, L.; Chen, Y.; Yang, L.; Zhang, Y.; Wang, S.; Hao, L.; Zhang, L. A 5G-powered robot-assisted teleultrasound diagnostic system in an intensive care unit. Crit. Care 2021, 25, 134. [Google Scholar] [CrossRef] [PubMed]
- Adams, S.J.; Burbridge, B.; Chatterson, L.; McKinney, V.; Babyn, P.; Mendez, I. Telerobotic ultrasound to provide obstetrical ultrasound services remotely during the COVID-19 pandemic. J. Telemed. Telecare 2022, 28, 568–576. [Google Scholar] [CrossRef]
- Zhang, Y.Q.; Yin, H.H.; He, T.; Guo, L.H.; Zhao, C.K.; Xu, H.X. Clinical application of a 5G-based telerobotic ultrasound system for thyroid examination on a rural island: A prospective study. Endocrine 2022, 76, 620–634. [Google Scholar] [CrossRef]
- Ye, R.; Zhou, X.; Shao, F.; Xiong, L.; Hong, J.; Huang, H.; Tong, W.; Wang, J.; Chen, S.; Cui, A.; et al. Feasibility of a 5G-Based Robot-Assisted Remote Ultrasound System for Cardiopulmonary Assessment of Patients with Coronavirus Disease 2019. Chest 2021, 159, 270–281. [Google Scholar] [CrossRef]
- Galusko, V.; Khanji, M.Y.; Bodger, O.; Weston, C.; Chambers, J.; Ionescu, A. Hand-held Ultrasound Scanners in Medical Education: A Systematic Review. J. Cardiovasc. Ultrasound 2017, 25, 75–83. [Google Scholar] [CrossRef]
| Setting | Number of Patients (%) | Mean Age, Years (Range) a | Patients’ Gender Distribution (%) | Main Complaints (%) |
|---|---|---|---|---|
| In-hospital | 642 (90.6%) | 59 ± 14.1 (21–93) | Male 273 (42.5%) Female 369(57.4%) | Physical examination 164 (25.5%) Flank pain 91(14.2%) |
| Out-of-hospital | 66 (9.4%) | 75 ± 10 (51–101) | Male 37 (56%) Female 29 (43.9%) | Physical examination 29 (43.9%) Chest distress 8 (12.1%) Flank discomfort 8 (12.1%) |
| Scans Performed for Specific Organs | Number of Tele-HHUS Scans (%) | |
|---|---|---|
| Digestive system | Liver | 352 (35.7%) |
| Gallbladder | 78 (7.9%) | |
| Spleen | 49 (5.0%) | |
| Pancreas | 45 (4.5%) | |
| Urinary system | Kidney | 378 (38.5%) |
| Ureter | 17 (1.7%) | |
| Prostate | 16 (1.6%) | |
| Bladder | 8 (0.8%) | |
| Adrenal gland | 2 (0.2%) | |
| Gynecology and obstetrics | Uterus | 27 (2.7%) |
| Ovary | 5 (0.5%) | |
| Pelvic cavity | 4 (0.4%) | |
| Circulatory system | Heart | 4 (0.4%) |
| Other | Pericardial cavity Abdominal cavity Thoracic cavity | 1 (0.1%) 1 (0.1%) 1 (0.1%) |
| Total | 987 (100.0%) |
| Tele-HHUS Findings | Number (%) |
|---|---|
| Fatty liver | 173 (23.0%) |
| Kidney stones | 152 (20.2%) |
| Renal cyst | 112 (14.9%) |
| Renal crystallization | 66 (8.8%) |
| Hepatic cyst | 57 (7.6%) |
| Gallstone | 37 (4.9%) |
| Hydronephrosis | 30 (4.0%) |
| Hepatic hemangioma | 18 (2.4%) |
| Hepatolith | 17 (2.3%) |
| Gallbladder polyps | 13 (1.7%) |
| Intrahepatic calcification | 12 (1.6%) |
| Liver lesion | 8 (1.1%) |
| Hysteromyoma | 8 (1.1%) |
| Benign prostatic Hyperplasia | 7 (0.9%) |
| Nephrarctia | 5 (0.7%) |
| Liver solid mass | 4 (0.5%) |
| Ovarian cyst | 4 (0.5%) |
| Pericardial effusion | 4 (0.5%) |
| Ureteral calculus | 3 (0.4%) |
| Hydroureter | 3 (0.4%) |
| Splenomegaly | 2 (0.3%) |
| Dilated intrahepatic bile ducts | 2 (0.3%) |
| Pregnancy | 2 (0.3%) |
| IUD location | 2 (0.3%) |
| Predominant left ventricular systolic dysfunction | 2 (0.3%) |
| Adrenal occupying lesion | 2 (0.3%) |
| Other a | 7 (0.7%) |
| Total | 752 (100%) |
| Based on Tele-HHUS Findings | |||
|---|---|---|---|
| Based on Clinical Experience Alone | No Referral | Referral | Total |
| No referral | 620 (87.5%) | 46 (6.5%) | 666 (94.0%) |
| Referral | 29 (4.1%) | 13 (1.8%) | 42 (5.9%) |
| Total | 649 (91.6%) | 59 (8.3%) | 708 (99.9%) |
| Real-Time or Asynchronous | Data Transfer Platform | Network | US Type | Portable | Cost | Application Fields | |
|---|---|---|---|---|---|---|---|
| Tele-HHUS system | Real-time | Custom software | Private 4G or 5G network | HHUS | Yes | Low | Wide |
| Tele-US system | Both | Data collector device | Private network | Conventional US system | No | High | Wide |
| Telerobotic US system | Real-time | Two subsystems | 5G network | Telerobotic US system | No | Very high | Narrow |
| HHUS system alone | None | None | None | HHUS | Yes | Low | Wide |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, Y.-J.; Guo, L.-H.; Bo, X.-W.; Sun, L.-P.; Zhang, Y.-F.; Chai, H.-H.; Ye, R.-Z.; Peng, C.-Z.; Qin, C.; Xu, H.-X. Tele-Mentored Handheld Ultrasound System for General Practitioners: A Prospective, Descriptive Study in Remote and Rural Communities. Diagnostics 2023, 13, 2932. https://doi.org/10.3390/diagnostics13182932
Zhou Y-J, Guo L-H, Bo X-W, Sun L-P, Zhang Y-F, Chai H-H, Ye R-Z, Peng C-Z, Qin C, Xu H-X. Tele-Mentored Handheld Ultrasound System for General Practitioners: A Prospective, Descriptive Study in Remote and Rural Communities. Diagnostics. 2023; 13(18):2932. https://doi.org/10.3390/diagnostics13182932
Chicago/Turabian StyleZhou, Yu-Jing, Le-Hang Guo, Xiao-Wan Bo, Li-Ping Sun, Yi-Feng Zhang, Hui-Hui Chai, Rui-Zhong Ye, Cheng-Zhong Peng, Chuan Qin, and Hui-Xiong Xu. 2023. "Tele-Mentored Handheld Ultrasound System for General Practitioners: A Prospective, Descriptive Study in Remote and Rural Communities" Diagnostics 13, no. 18: 2932. https://doi.org/10.3390/diagnostics13182932
APA StyleZhou, Y.-J., Guo, L.-H., Bo, X.-W., Sun, L.-P., Zhang, Y.-F., Chai, H.-H., Ye, R.-Z., Peng, C.-Z., Qin, C., & Xu, H.-X. (2023). Tele-Mentored Handheld Ultrasound System for General Practitioners: A Prospective, Descriptive Study in Remote and Rural Communities. Diagnostics, 13(18), 2932. https://doi.org/10.3390/diagnostics13182932





