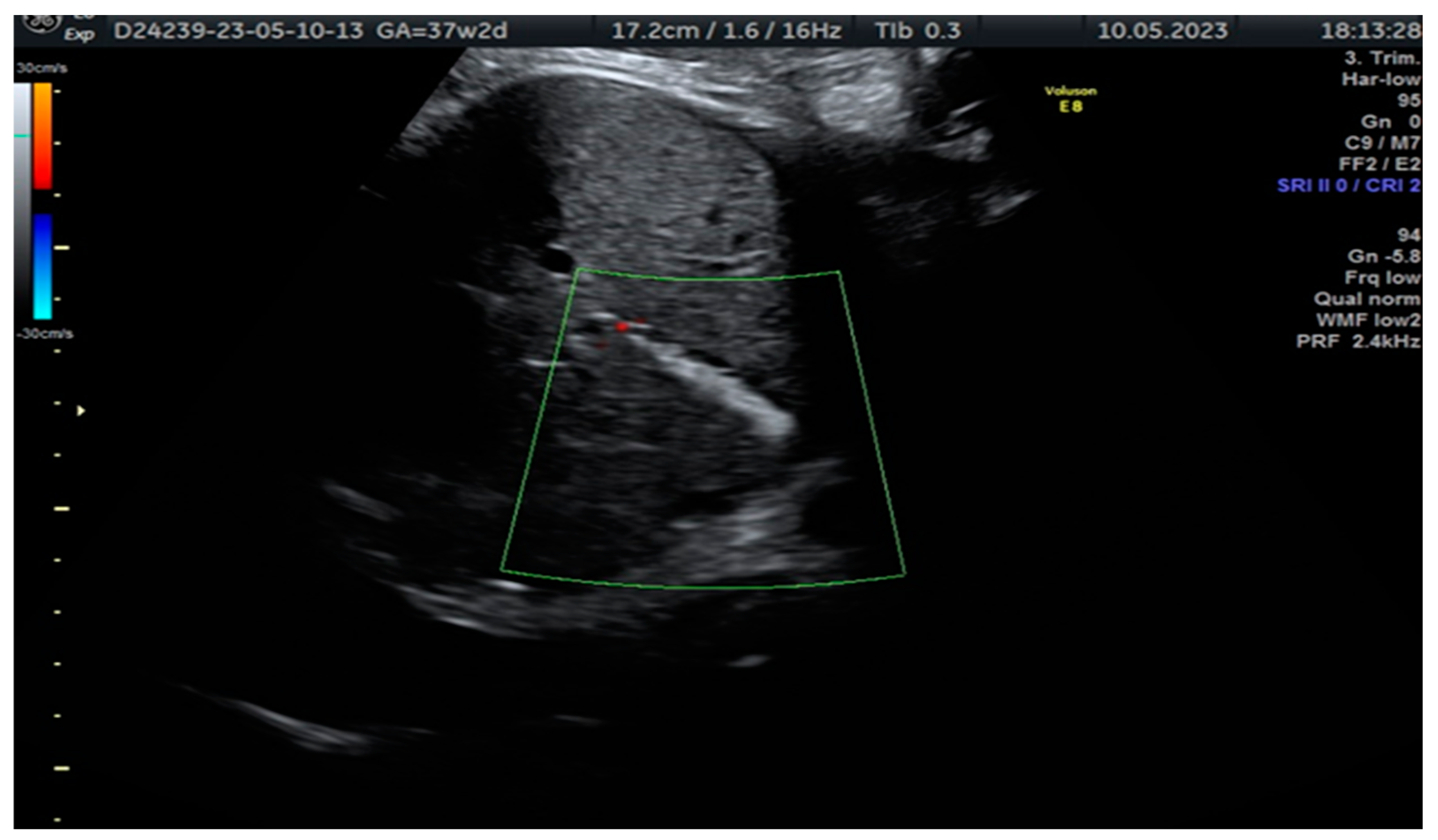
Sonographic Detection of Fetal Cholelithiasis
Abstract
:
Author Contributions
Funding
Informed Consent Statement
Conflicts of Interest
References
- Triunfo, S.; Rosati, P.; Ferrara, P.; Gatto, A.; Scambia, G. Fetal cholelithiasis: A diagnostic update and a literature review. Clin. Med. Insights Case Rep. 2013, 6, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Iroh Tam, P.Y.; Angelides, A. Perinatal detection of gallstones in siblings. Am. J. Perinatol. 2010, 27, 771–774. [Google Scholar] [PubMed]
- Agnifili, A.; Verzaro, R.; Carducci, G.; Mancini, E.; Gola, P.; Marino, M.; Tollis, G.; Rizzo, F.M.; Criscione, S. Fetal cholelithiasis: A prospective study of incidence, predisposing factors, and ultrasonographic and clinical features. Clin. Pediatr. 1999, 38, 371–373. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.L.; Teele, R.L.; Doubilet, P.M.; DiSalvo, D.N.; Benson, C.B.; Van Alstyne, G.A. Echogenic material in the fetal gallbladder: Sonographic and clinical observations. Radiology 1992, 182, 73–76. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gică, N.; Radoi, A.; Gică, C.; Panaitescu, A.M.; Peltecu, G.; Huluță, I. Sonographic Detection of Fetal Cholelithiasis. Diagnostics 2023, 13, 2900. https://doi.org/10.3390/diagnostics13182900
Gică N, Radoi A, Gică C, Panaitescu AM, Peltecu G, Huluță I. Sonographic Detection of Fetal Cholelithiasis. Diagnostics. 2023; 13(18):2900. https://doi.org/10.3390/diagnostics13182900
Chicago/Turabian StyleGică, Nicolae, Andra Radoi, Corina Gică, Anca Maria Panaitescu, Gheorghe Peltecu, and Iulia Huluță. 2023. "Sonographic Detection of Fetal Cholelithiasis" Diagnostics 13, no. 18: 2900. https://doi.org/10.3390/diagnostics13182900
APA StyleGică, N., Radoi, A., Gică, C., Panaitescu, A. M., Peltecu, G., & Huluță, I. (2023). Sonographic Detection of Fetal Cholelithiasis. Diagnostics, 13(18), 2900. https://doi.org/10.3390/diagnostics13182900








