Laser-Based 3D Body Scanning Reveals a Higher Prevalence of Abdominal Obesity than Tape Measurements: Results from a Population-Based Sample
Abstract
1. Introduction
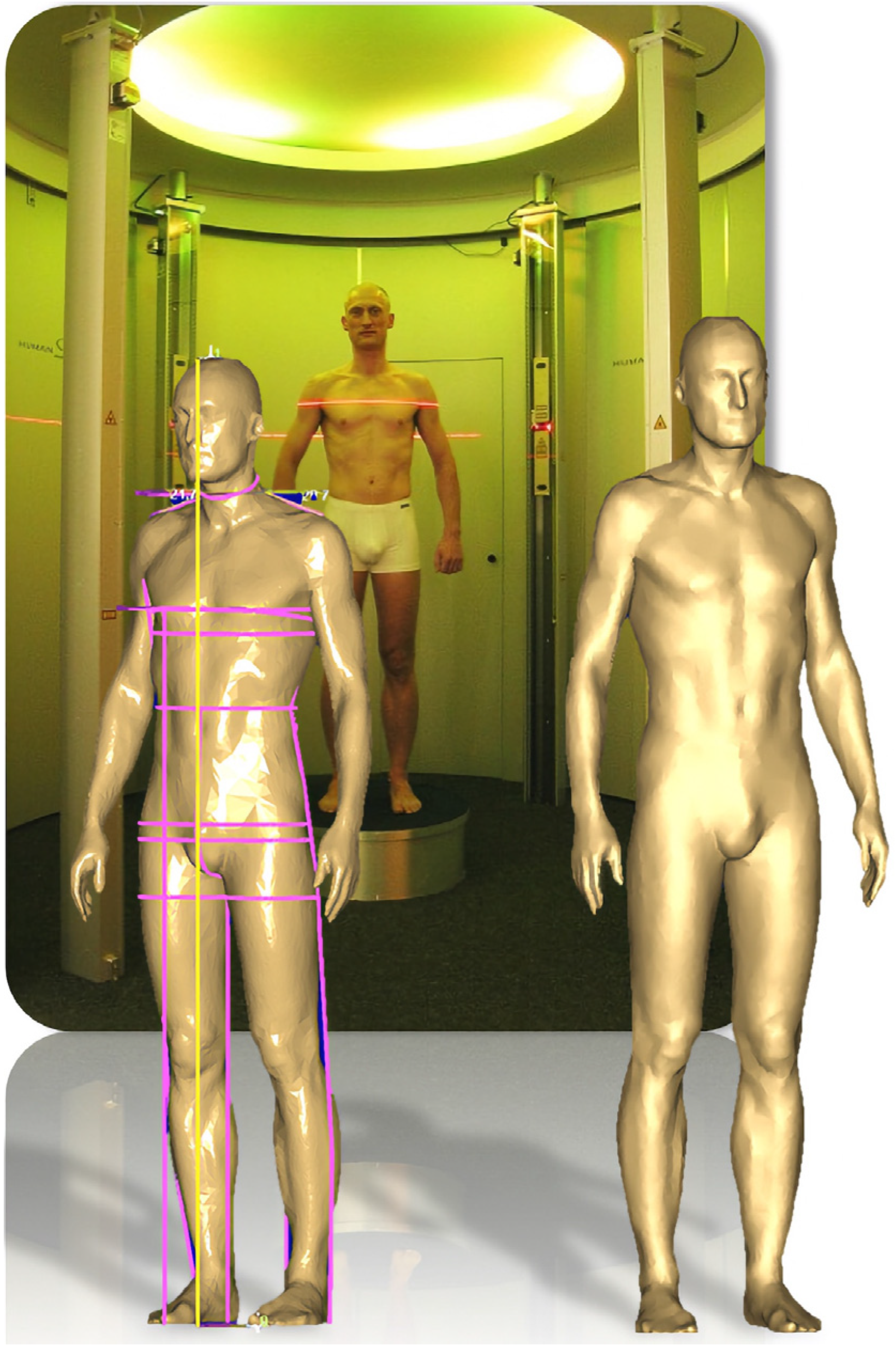
2. Methods
2.1. Study Design and Population
2.2. Data
2.3. Metabolic Syndrome Classification
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Agreement of Manual and Automatic Measurements
3.3. Practical Implications
3.4. Anthropometric Measurements
3.5. Metabolic Syndrome
4. Discussion
4.1. Body Scan and Manual Tape Measurements Show Excellent Agreement
4.2. Body Scanning Reveals a Higher Prevalence of Abdominal Obesity
4.3. Other Literature
4.4. Risk Assessment
4.5. Strengths and Limitations
4.6. Perspectives
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alberti, K.G.; Zimmet, P.; Shaw, J.; Grundy, S.M. The IDF Consensus Worldwide Definition of the Metabolic Syndrome; International Diabetes Federation: Brussels, Belgium, 2006. [Google Scholar]
- Alberti, K.G.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.; Loria, C.M.; Smith, S.C., Jr. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef] [PubMed]
- Kaur, J. A comprehensive review on metabolic syndrome. Cardiol. Res. Pr. 2014, 2014, 943162. [Google Scholar] [CrossRef] [PubMed]
- Fosbol, M.O.; Zerahn, B. Contemporary methods of body composition measurement. Clin. Physiol. Funct. Imaging 2015, 35, 81–97. [Google Scholar] [CrossRef] [PubMed]
- Muller, M.J.; Braun, W.; Pourhassan, M.; Geisler, C.; Bosy-Westphal, A. Application of standards and models in body composition analysis. Proc. Nutr. Soc. 2016, 75, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Treleaven, P.; Wells, J. 3D Body Scanning and Healthcare Applications. Computer 2007, 40, 28–34. [Google Scholar] [CrossRef]
- Wells, J.C.; Ruto, A.; Treleaven, P. Whole-body three-dimensional photonic scanning: A new technique for obesity research and clinical practice. Int. J. Obes. 2008, 32, 232–238. [Google Scholar] [CrossRef]
- Wang, J.; Gallagher, D.; Thornton, J.C.; Yu, W.; Horlick, M.; Pi-Sunyer, F.X. Validation of a 3-dimensional photonic scanner for the measurement of body volumes, dimensions, and percentage body fat. Am. J. Clin. Nutr. 2006, 83, 809–816. [Google Scholar] [CrossRef] [PubMed]
- Heuberger, R.; Domina, T.; MacGillivray, M. Body scanning as a new anthropometric measurement tool for health-risk assessment. Int. J. Consum. Stud. 2008, 32, 34–40. [Google Scholar] [CrossRef]
- Bretschneider, T.; Koop, U.; Schreiner, V.; Wenck, H.; Jaspers, S. Validation of the body scanner as a measuring tool for a rapid quantification of body shape. Ski. Res. Technol. 2009, 15, 364–369. [Google Scholar] [CrossRef] [PubMed]
- Pepper, M.R.; Freeland-Graves, J.H.; Yu, W.; Stanforth, P.R.; Cahill, J.M.; Mahometa, M.; Xu, B. Validation of a 3-dimensional laser body scanner for assessment of waist and hip circumference. J. Am. Coll. Nutr. 2010, 29, 179–188. [Google Scholar] [CrossRef] [PubMed]
- Tomkinson, G.R.; Shaw, L.G. Quantification of the postural and technical errors in asymptomatic adults using direct 3D whole body scan measurements of standing posture. Gait Posture 2013, 37, 172–177. [Google Scholar] [CrossRef] [PubMed]
- Jaeschke, L.; Steinbrecher, A.; Pischon, T. Measurement of waist and hip circumference with a body surface scanner: Feasibility, validity, reliability, and correlations with markers of the metabolic syndrome. PLoS ONE 2015, 10, e0119430. [Google Scholar] [CrossRef] [PubMed]
- Kuehnapfel, A.; Ahnert, P.; Loeffler, M.; Broda, A.; Scholz, M. Reliability of 3D laser-based anthropometry and comparison with classical anthropometry. Sci. Rep. 2016, 6, 26672. [Google Scholar] [CrossRef] [PubMed]
- Koepke, N.; Zwahlen, M.; Wells, J.C.; Bender, N.; Henneberg, M.; Ruhli, F.J.; Staub, K. Comparison of 3D laser-based photonic scans and manual anthropometric measurements of body size and shape in a validation study of 123 young Swiss men. PeerJ 2017, 5, e2980. [Google Scholar] [CrossRef] [PubMed]
- John, U.; Greiner, B.; Hensel, E.; Ludemann, J.; Piek, M.; Sauer, S.; Adam, C.; Born, G.; Alte, D.; Greiser, E.; et al. Study of Health In Pomerania (SHIP): A health examination survey in an east German region: Objectives and design. Soz. Praventivmed. 2001, 46, 186–194. [Google Scholar] [CrossRef] [PubMed]
- Volzke, H.; Alte, D.; Schmidt, C.O.; Radke, D.; Lorbeer, R.; Friedrich, N.; Aumann, N.; Lau, K.; Piontek, M.; Born, G.; et al. Cohort profile: The study of health in Pomerania. Int. J. Epidemiol. 2011, 40, 294–307. [Google Scholar] [CrossRef] [PubMed]
- Volzke, H.; Schossow, J.; Schmidt, C.O.; Jurgens, C.; Richter, A.; Werner, A.; Werner, N.; Radke, D.; Teumer, A.; Ittermann, T.; et al. Cohort Profile Update: The Study of Health in Pomerania (SHIP). Int. J. Epidemiol. 2022, 51, e372–e383. [Google Scholar] [CrossRef]
- Ludemann, J.; Piek, M.; Wood, W.G.; Meyer, S.; Greiner, B.; John, U.; Hense, H.W. [Methods for quality assurance of medical examination in epidemiological field studies: The “Study of Health in Pomerania” (SHIP)]. Gesundheitswesen 2000, 62, 234–243. [Google Scholar] [CrossRef]
- Universitätsmedizin-Greifswald. Transferstelle für Daten- und Biomaterialienmanagement. Available online: https://transfer.ship-med.uni-greifswald.de/FAIRequest (accessed on 20 March 2023).
- Mander, A. Available online: http://fmwww.bc.edu/RePEc/bocode/b/batplot.html (accessed on 25 September 2017).
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Measuring agreement in method comparison studies. Stat. Methods Med. Res. 1999, 8, 135–160. [Google Scholar] [CrossRef]
- Petrescu, L.; Strungaru, C.A.; Mihailescu, D.; Salistean, A.; Niculescu, C.; Ionescu-Tirgoviste, C. 3D Body Scanning Technology, a Method for Assessing Early Risk of Diabetes. Proc. Rom. Acad. Ser. B 2012, 1, 3–8. [Google Scholar]
- Lin, J.D.; Chiou, W.K.; Weng, H.F.; Tsai, Y.H.; Liu, T.H. Comparison of three-dimensional anthropometric body surface scanning to waist-hip ratio and body mass index in correlation with metabolic risk factors. J. Clin. Epidemiol. 2002, 55, 757–766. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.D.; Chiou, W.K.; Weng, H.F.; Fang, J.T.; Liu, T.H. Application of three-dimensional body scanner: Observation of prevalence of metabolic syndrome. Clin. Nutr. 2004, 23, 1313–1323. [Google Scholar] [CrossRef] [PubMed]
- Chiou, W.K.; Lin, J.D.; Weng, H.F.; Ou, Y.C.; Liu, T.H.; Fang, J.T. Correlation of the dysmetabolic risk factors with different anthropometric measurements. Endocr. J. 2005, 52, 139–148. [Google Scholar] [CrossRef]
- Wells, J.C.; Cole, T.J.; Bruner, D.; Treleaven, P. Body shape in American and British adults: Between-country and inter-ethnic comparisons. Int. J. Obes. 2008, 32, 152–159. [Google Scholar] [CrossRef]
- Wells, J.C.; Treleaven, P.; Charoensiriwath, S. Body shape by 3-D photonic scanning in Thai and UK adults: Comparison of national sizing surveys. Int. J. Obes. 2012, 36, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Lamb, M.J.; Byrne, C.D.; Wilson, J.F.; Wild, S.H. Evaluation of bioelectrical impedance analysis for identifying overweight individuals at increased cardiometabolic risk: A cross-sectional study. PLoS ONE 2014, 9, e106134. [Google Scholar] [CrossRef] [PubMed]
- Schneider, H.J.; Friedrich, N.; Klotsche, J.; Pieper, L.; Nauck, M.; John, U.; Dorr, M.; Felix, S.; Lehnert, H.; Pittrow, D.; et al. The predictive value of different measures of obesity for incident cardiovascular events and mortality. J. Clin. Endocrinol. Metab. 2010, 95, 1777–1785. [Google Scholar] [CrossRef]
- Marks, G.C.; Habicht, J.P.; Mueller, W.H. Reliability, dependability, and precision of anthropometric measurements. The Second National Health and Nutrition Examination Survey 1976–1980. Am. J. Epidemiol. 1989, 130, 578–587. [Google Scholar] [CrossRef]
- Kouchi, M.; Mochimaru, M.; Tsuzuki, K.; Yokoi, T. Random errors in anthropometry. J. Hum. Ergol. 1996, 25, 155–166. [Google Scholar]
- Klipstein-Grobusch, K.; Georg, T.; Boeing, H. Interviewer variability in anthropometric measurements and estimates of body composition. Int. J. Epidemiol. 1997, 26 (Suppl. 1), S174–S180. [Google Scholar] [CrossRef] [PubMed]
- Kouchi, M.; Mochimaru, M.; Tsuzuki, K.; Yokoi, T. Interobserver errors in anthropometry. J. Hum. Ergol. 1999, 28, 15–24. [Google Scholar]
- Ulijaszek, S.J.; Kerr, D.A. Anthropometric measurement error and the assessment of nutritional status. Br. J. Nutr. 1999, 82, 165–177. [Google Scholar] [CrossRef] [PubMed]
- Sebo, P.; Beer-Borst, S.; Haller, D.M.; Bovier, P.A. Reliability of doctors’ anthropometric measurements to detect obesity. Prev. Med. 2008, 47, 389–393. [Google Scholar] [CrossRef] [PubMed]
- Loffler-Wirth, H.; Willscher, E.; Ahnert, P.; Wirkner, K.; Engel, C.; Loeffler, M.; Binder, H. Novel Anthropometry Based on 3D-Bodyscans Applied to a Large Population Based Cohort. PLoS ONE 2016, 11, e0159887. [Google Scholar] [CrossRef] [PubMed]

| Males (n = 160; 45.2%) | Females (n = 194; 54.8%) | |||||
|---|---|---|---|---|---|---|
| Variable | Median/IQR or %/n | |||||
| Age (years) | 44.5 | / | 22.0 | 45.0 | / | 19.0 |
| BMI (kg/m2) | 27.5 | / | 5.11 | 25.1 | / | 6.94 |
| BMI < 25 kg/m2 | 21.9% | / | 35 | 49.5% | / | 96 |
| BMI 25–29.9 kg/m2 | 50.6% | / | 81 | 29.9% | / | 58 |
| BMI 30–34.9 kg/m2 | 21.9% | / | 35 | 16.0% | / | 31 |
| BMI ≥ 35 kg/m2 | 5.6% | / | 9 | 4.6% | / | 9 |
| Waist circumference (cm) | 95.5 | / | 14.7 | 80.1 | / | 16.9 |
| Abdominal obesity 1 | 56.3% | / | 90 | 50.0% | / | 97 |
| WHtR | 0.54 | / | 0.09 | 0.49 | / | 0.11 |
| Body fat percentage | 23.4 | / | 6.60 | 32.7 | / | 10.7 |
| Metabolic syndrome 1 | 44.4% | / | 71 | 20.1% | / | 39 |
| Tape Measurements | 3D Body Scan Measurements | Delta 1 | Correlation 2 | ||
|---|---|---|---|---|---|
| Height | M | 179.0/8.0 | 179.3/9.0 | 0.3/1.8 | 0.990 |
| F | 165.0/9.0 | 165.2/8.3 | 0.6/1.1 | 0.990 | |
| Right upper arm circ. | M | 31.0/4.0 | 31.7/3.2 | 0.9/2.2 | 0.801 |
| F | 28.0/4.6 | 28.7/3.8 | 1.0/2.0 | 0.896 | |
| Waist circumference | M | 95.5/14.7 | 98.4/15.6 | 2.8/3.4 | 0.968 |
| F | 80.1/16.9 | 82.6/17.6 | 3.1/3.4 | 0.975 | |
| Hip circumference | M | 99.1/9.3 | 100.0/13.3 | 2.1/6.3 | 0.888 |
| F | 98.5/13.9 | 98.2/15.5 | 1.0/4.2 | 0.946 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kosilek, R.P.; Ittermann, T.; Radke, D.; Schipf, S.; Nauck, M.; Friedrich, N.; Völzke, H. Laser-Based 3D Body Scanning Reveals a Higher Prevalence of Abdominal Obesity than Tape Measurements: Results from a Population-Based Sample. Diagnostics 2023, 13, 2594. https://doi.org/10.3390/diagnostics13152594
Kosilek RP, Ittermann T, Radke D, Schipf S, Nauck M, Friedrich N, Völzke H. Laser-Based 3D Body Scanning Reveals a Higher Prevalence of Abdominal Obesity than Tape Measurements: Results from a Population-Based Sample. Diagnostics. 2023; 13(15):2594. https://doi.org/10.3390/diagnostics13152594
Chicago/Turabian StyleKosilek, Robert P., Till Ittermann, Dörte Radke, Sabine Schipf, Matthias Nauck, Nele Friedrich, and Henry Völzke. 2023. "Laser-Based 3D Body Scanning Reveals a Higher Prevalence of Abdominal Obesity than Tape Measurements: Results from a Population-Based Sample" Diagnostics 13, no. 15: 2594. https://doi.org/10.3390/diagnostics13152594
APA StyleKosilek, R. P., Ittermann, T., Radke, D., Schipf, S., Nauck, M., Friedrich, N., & Völzke, H. (2023). Laser-Based 3D Body Scanning Reveals a Higher Prevalence of Abdominal Obesity than Tape Measurements: Results from a Population-Based Sample. Diagnostics, 13(15), 2594. https://doi.org/10.3390/diagnostics13152594






