Stereomicroscopic Aspects of Non-Carious Cervical Lesions
Abstract
1. Introduction
2. Materials and Methods
2.1. Sampling and Preparation of Teeth
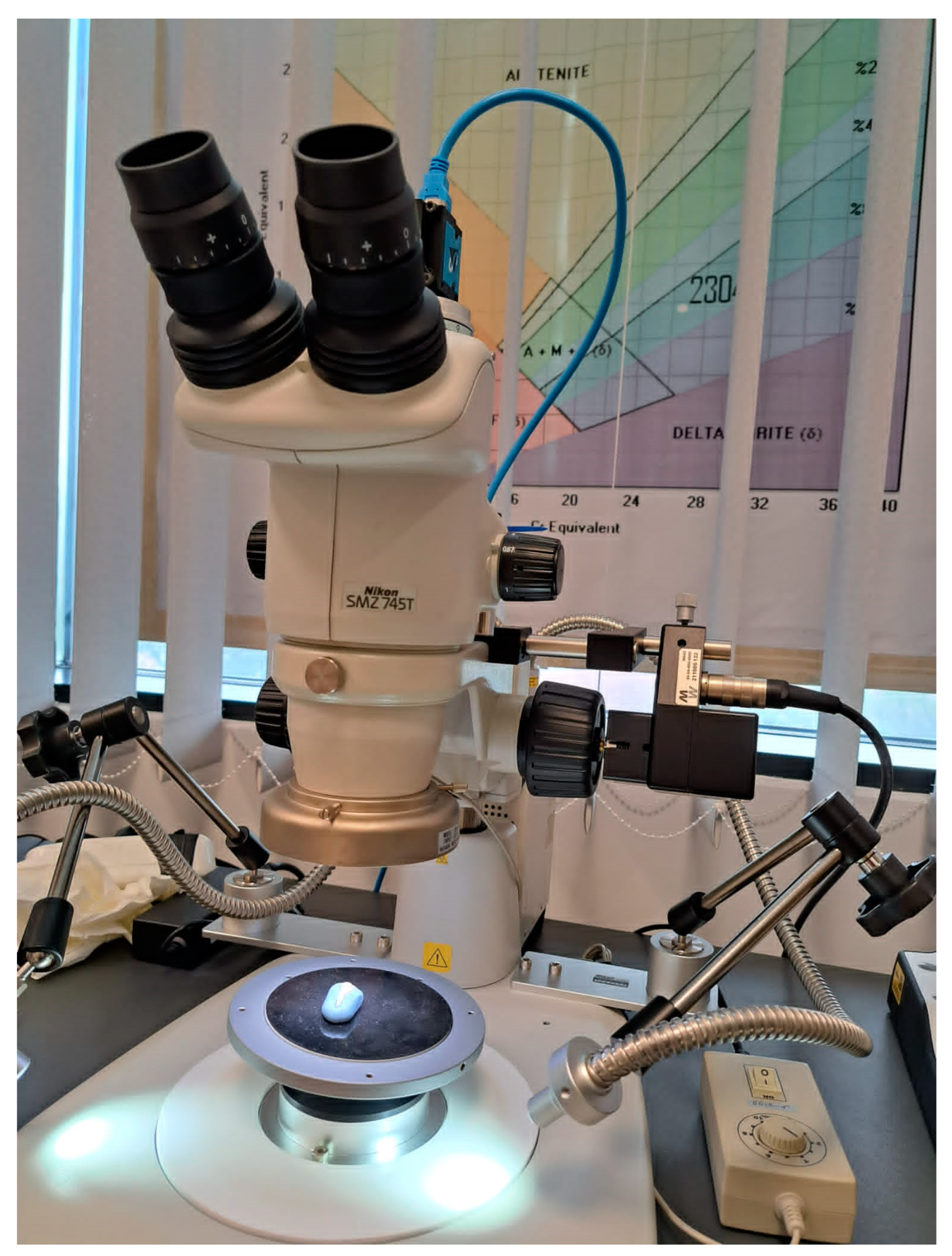
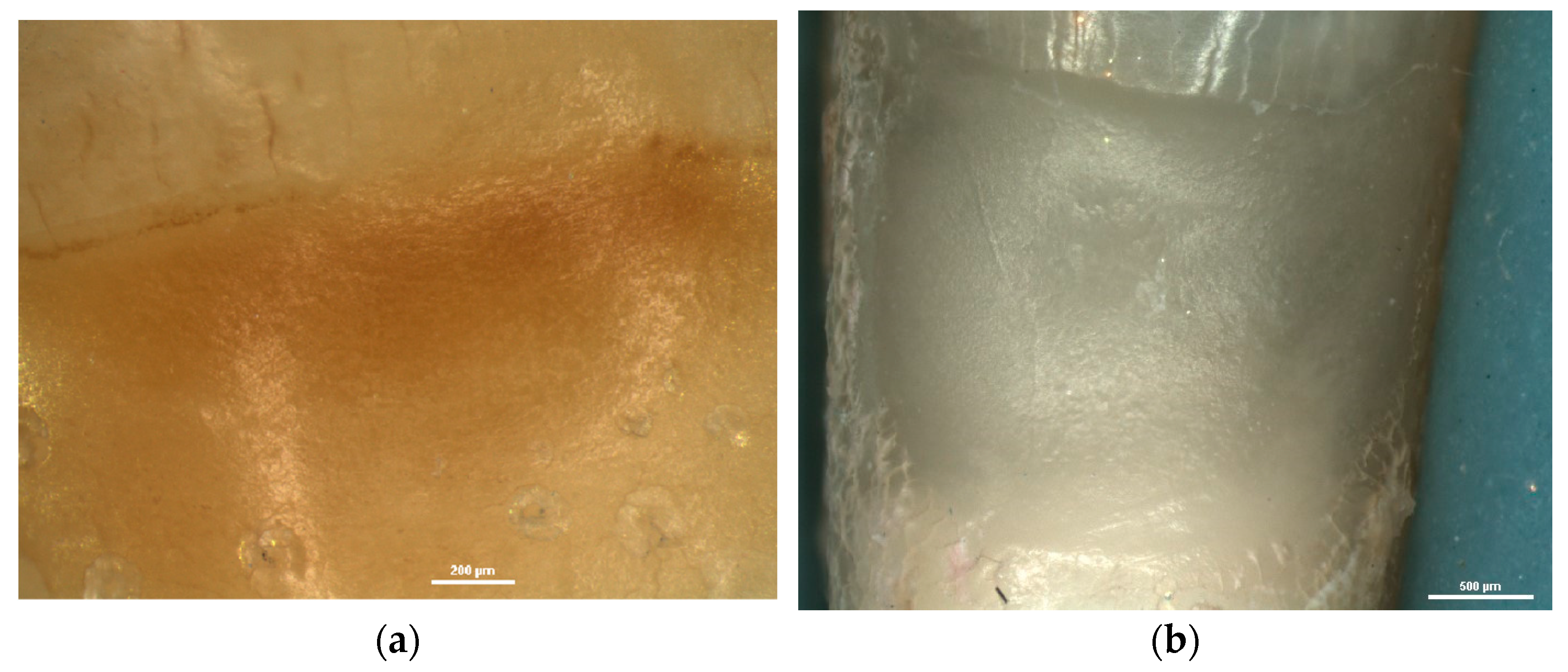
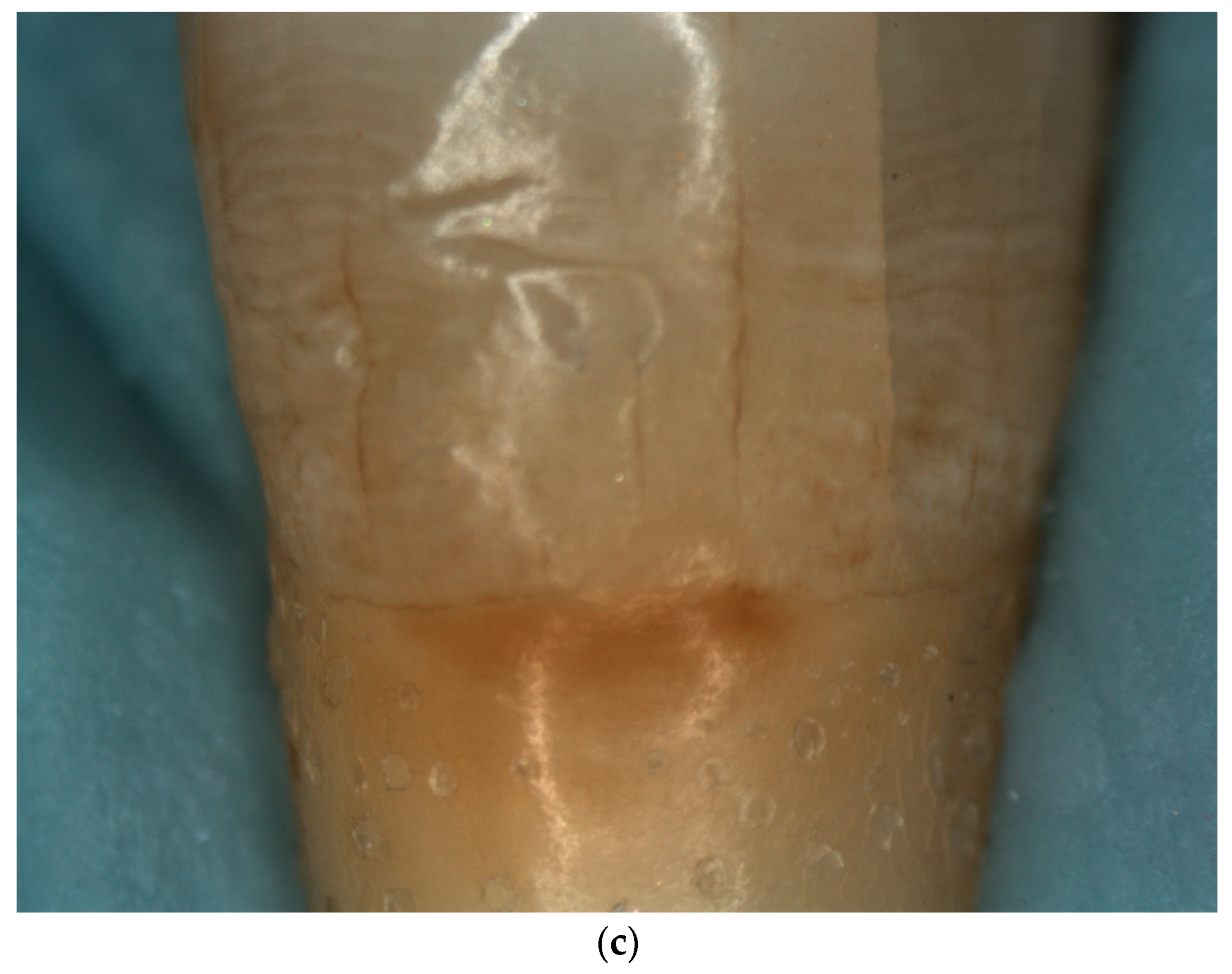
2.2. Stereomicroscopic Examination of NCCL
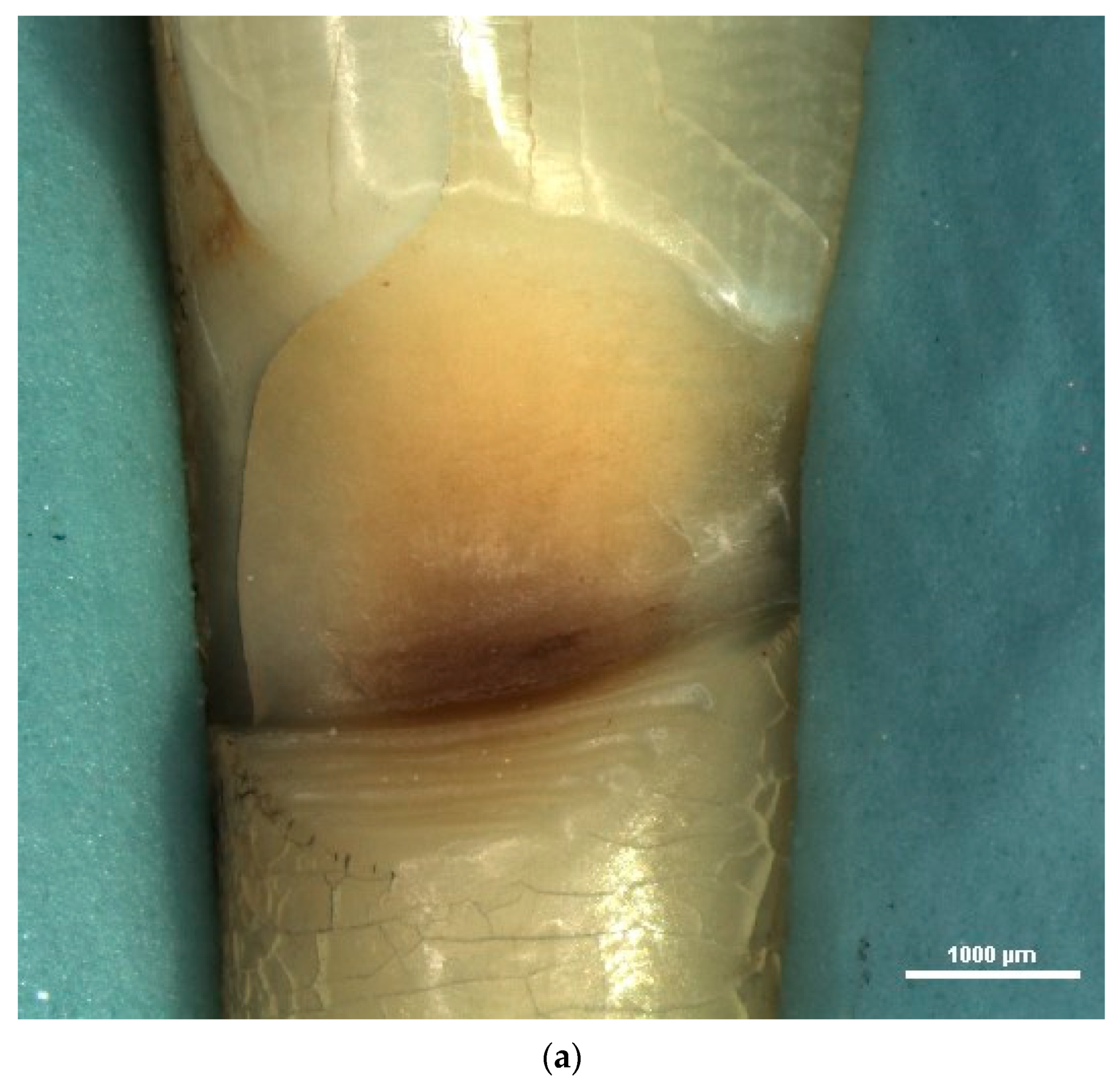
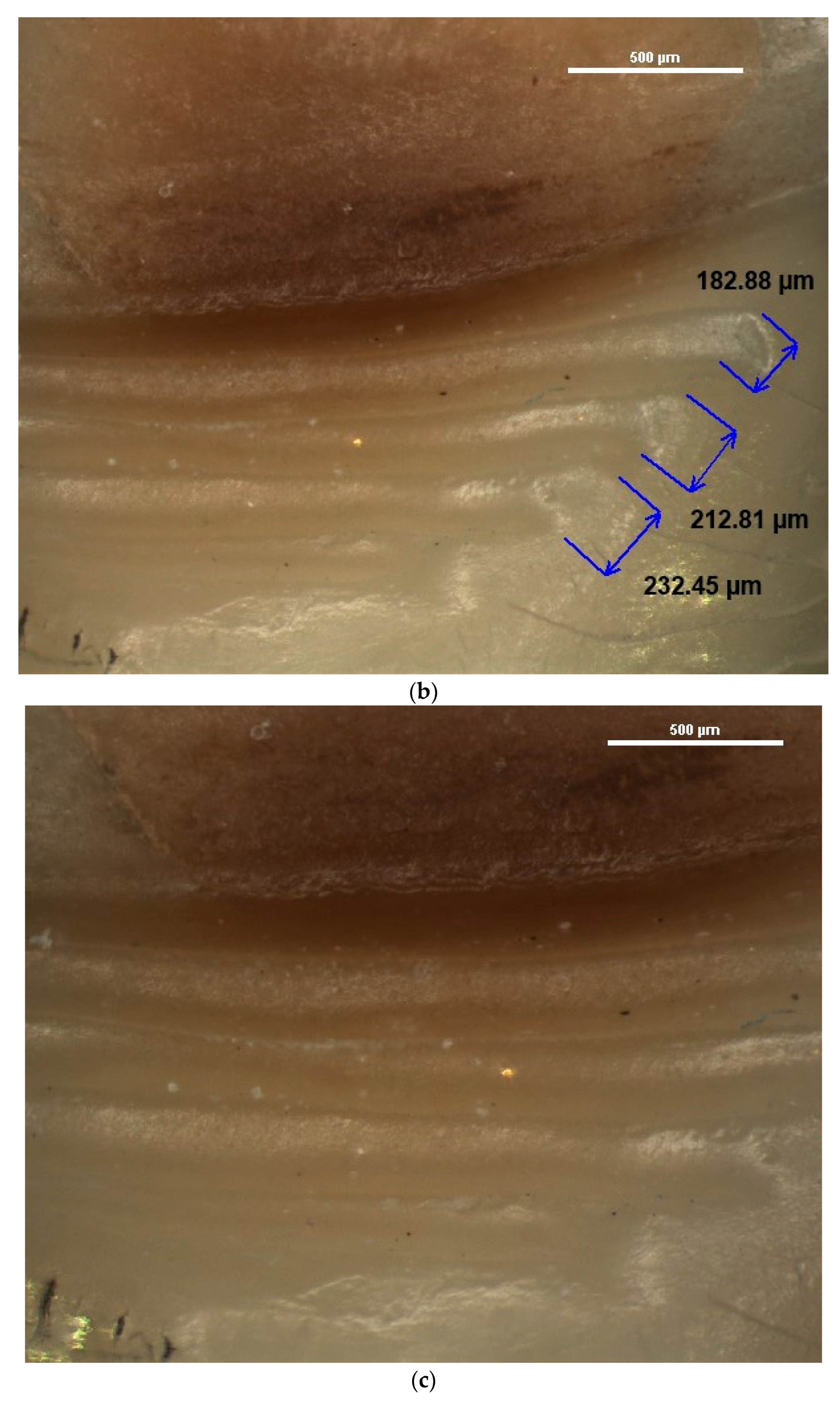
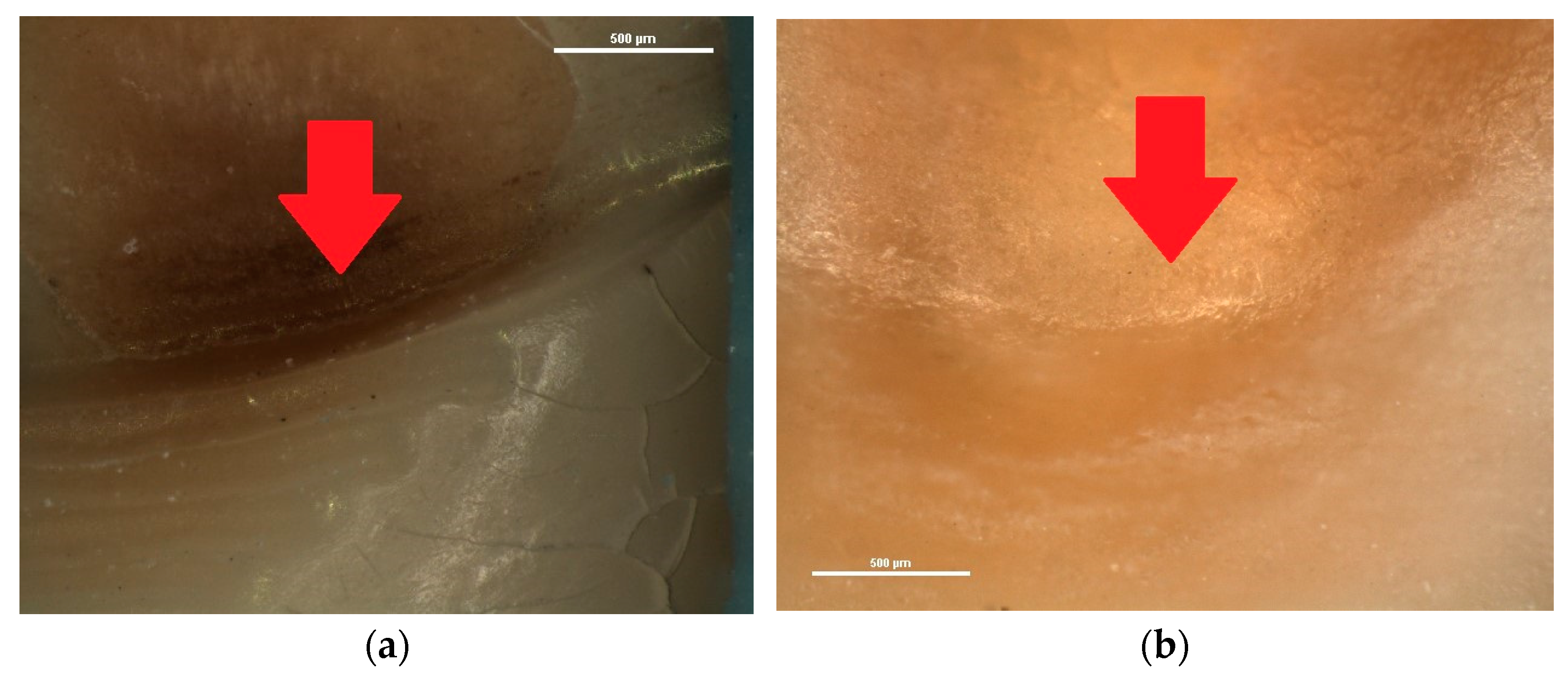
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Quinchiguano Caraguay, M.A.; Amoroso Calle, E.E.; Idrovo Tinta, T.S.; Gil Pozo, J.A. Non-carious cervical lesions (NCCL): A review of the literature. Res. Soc. Dev. 2023, 12, e26612541876. [Google Scholar] [CrossRef]
- Demarco, F.F.; Cademartori, M.G.; Hartwig, A.D.; Lund, R.G.; Azevedo, M.S.; Horta, B.L.; Corrêa, M.B.; Huysmans, M.-C. Non-carious cervical lesions (NCCLs) and associated factors: A multilevel analysis in a cohort study in southern Brazil. J. Clin. Periodontol. 2022, 49, 48–58. [Google Scholar] [CrossRef] [PubMed]
- Goodacre, C.J.; Eugene Roberts, W.; Munoz, C.A. Noncarious cervical lesions: Morphology and progression, prevalence, etiology, pathophysiology, and clinical guidelines for restoration. J. Prosthodont. 2023, 32, e1–e18. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, D.N.R.; Thomas, R.Z.; Soares, P.V.; Cune, M.S.; Gresnigt, M.M.M.; Slot, D.E. Prevalence of noncarious cervical lesions among adults: A systematic review. J. Dent. 2020, 95, 103285. [Google Scholar] [CrossRef]
- Koc Vural, U.; Meral, E.; Ergin, E.; Gürgan, S. Twenty-four-month clinical performance of a glass hybrid restorative in non-carious cervical lesions of patients with bruxism: A split-mouth, randomized clinical trial. Clin. Oral Investig. 2019, 24, 1229–1238. [Google Scholar] [CrossRef] [PubMed]
- Patano, A.; Malcangi, G.; De Santis, M.; Morolla, R.; Settanni, V.; Piras, F.; Inchingolo, A.D.; Mancini, A.; Inchingolo, F.; Dipalma, G.; et al. Conservative Treatment of Dental Non-Carious Cervical Lesions: A Scoping Review. Biomedicines 2023, 11, 1530. [Google Scholar] [CrossRef]
- Hayashi, M.; Kubo, S.; Pereira, P.N.R.; Ikeda, M.; Takagaki, T.; Nikaido, T.; Tagami, J. Progression of non-carious cervical lesions: 3D morphological analysis. Clin. Oral Investig. 2022, 26, 575–583. [Google Scholar] [CrossRef] [PubMed]
- Hamouda, Y.; Elsayed, H.; Etman, W. Biomimetic Mineralization Approach of Dentin Hypersensitivity in Patients with Early Non-Carious Cervical Lesions. Egypt. Dent. J. 2021, 67, 3693–3710. [Google Scholar] [CrossRef]
- Peumans, M.; Politano, G.; Van Meerbeek, B. Treatment of noncarious cervical lesions: When, why, and how. Int. J. Esthet. Dent. 2020, 15, 16–42. [Google Scholar]
- Paradowska-Stolarz, A.; Wieckiewicz, M.; Owczarek, A.; Wezgowiec, J. Natural Polymers for the Maintenance of Oral Health: Review of Recent Advances and Perspectives. Int. J. Mol. Sci. 2021, 22, 10337. [Google Scholar] [CrossRef]
- Mazur, M.; Ndokaj, A.; Bietolini, S.; Nisii, V.; Duś-Ilnicka, I.; Ottolenghi, L. Green dentistry: Organic toothpaste formulations. A literature review. Dent. Med. Probl. 2022, 59, 461–474. [Google Scholar] [CrossRef] [PubMed]
- El-Dhuwaib, B. The diagnosis & management of non-carious cervical lesions by dental practitioners from the South Yorkshire and Bassetlaw regions of England. Open Access J. Dent. Sci. 2022, 7, 000321. [Google Scholar] [CrossRef]
- Nascimento, M.; Dilbone, D.; Pereira, P.; Geraldeli, S.; Delgado, A.; Duarte, W. Abfraction lesions: Etiology, diagnosis, and treatment options. Clin. Cosmet. Investig. Dent. 2016, 8, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Modena, R.A.; Tannure, P.N.; Pessoa, V.A.; Cavalcante, L.M.; Schneider, L.F.J. Diagnosis attitudes and restorative practices of noncarious cervical lesions by a group of Brazilian dentists from the state of Rio de Janeiro. Adhes. Sci. 2018, 6, 11. [Google Scholar] [CrossRef]
- Sawlani, K.; Lawson, N.C.; Burgess, J.O.; Lemons, J.E.; Kinderknecht, K.E.; Givan, D.A.; Ramp, L. Factors influencing the progression of noncarious cervical lesions: A 5-year prospective clinical evaluation. J. Prosthet. Dent. 2016, 115, 571–577. [Google Scholar] [CrossRef]
- Santos, M.J.; Ari, N.; Steele, S.; Costella, J.; Banting, D. Retention of tooth-colored restorations in non-carious cervical lesions—A systematic review. Clin. Oral Investig. 2014, 18, 1369–1381. [Google Scholar] [CrossRef]
- Soares, P.V.; Grippo, J.O. Noncarious Cervical Lesions and Cervical Dentin Hypersensitivity–Etiology, Diagnosis and Treatment; Quintessesnce Publishing: Batavia, IL, USA, 2017. [Google Scholar]
- Skośkiewicz-Malinowska, K.; Mysior, M.; Rusak, A.; Kuropka, P.; Kozakiewicz, M.; Jurczyszyn, K. Application of Texture and Fractal Dimension Analysis to Evaluate Subgingival Cement Surfaces in Terms of Biocompatibility. Materials 2021, 14, 5857. [Google Scholar] [CrossRef]
- Biniraj, K.R.; Sagir, M.; Sunil, M.M.; Janardhanan, M. Clinical attachment level gain and bone regeneration around a glass ionomer restoration on root surface wall of periodontal pocket. J. Indian Soc. Periodontol. 2012, 16, 442–445. [Google Scholar] [CrossRef]
- Lim, J.; Lee, W.; Judex, S.; Mahdian, M. Optical Coherence Tomography for the Detection and Characterization of Subgingival Root Caries Lesions and Noncarious Cervical Lesions: A Quantitative Analysis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2021, 132, e118–e119. [Google Scholar] [CrossRef]
- Wada, I.; Shimada, Y.; Ikeda, M.; Sadr, A.; Nakashima, S.; Tagami, J.; Sumi, Y. Clinical assessment of non carious cervical lesion using swept-source optical coherence tomography. J. Biophotonics 2015, 8, 846–854. [Google Scholar] [CrossRef]
- Marcauteanu, C.; Stoica, E.; Dorin, B.; Sinescu, C.; Negrutiu, M.L.; Topala, F.; Goguta, L.; Hughes, M.; Bradu, A.; Dobre, G.; et al. Microstructural characterization of non-carious cervical lesions by en face optical coherence tomography. Timis. Med. J. 2010, 60, 60–63. [Google Scholar]
- Lim, G.E.; Son, S.A.; Hur, B.; Park, J.K. Evaluation of the relationship between non-caries cervical lesions and the tooth and periodontal tissue: An ex-vivo study using micro-computed tomography. PLoS ONE 2020, 15, e0240979. [Google Scholar] [CrossRef] [PubMed]
- Hur, B.; Kim, H.C.; Park, J.K.; Versluis, A. Characteristics of non-carious cervical lesions—An ex vivo study using micro computed tomography. J. Oral Rehabil. 2010, 38, 469–474. [Google Scholar] [CrossRef]
- Worawongvasu, R. Scanning electron microscope characterization of noncarious cervical lesions in human teeth. J. Oral Maxillofac. Pathol. 2021, 25, 202. [Google Scholar] [CrossRef]
- Levrini, L.; Di Benedetto, G.; Raspanti, M. Dental Wear: A Scanning Electron Microscope Study. BioMed Res. Int. 2014, 2014, 340425. [Google Scholar] [CrossRef] [PubMed]
- Daley, T.; Harbrow, D.; Kahler, B.; Young, W. The cervical wedge-shaped lesion in teeth: A light and electron microscopic study. Aust. Dent. J. 2009, 54, 212–219. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, C.; Ranjitkar, S.; Kaidonis, J.A.; Townsend, G.C. A qualitative assessment of non-carious cervical lesions in extracted human teeth. Aust. Dent. J. 2008, 53, 46–51. [Google Scholar] [CrossRef]
- Stanusi, A.; Iacov-Craitoiu, M.M.; Scrieciu, M.; Mitrut, I.; Firulescu, B.C.; Botila, M.R.; Vladutu, D.E.; Stanusi, A.S.; Mercut, V.; Osiac, E. Morphological and Optical Coherence Tomography Aspects of Non-Carious Cervical Lesions. J. Pers. Med. 2023, 13, 772. [Google Scholar] [CrossRef]
- Stănuși, A.; Ionescu, M.; Cerbulescu, C.; Popescu, S.M.; Osiac, E.; Mercuț, R.; Scrieciu, M.; Pascu, R.M.; Stănuși, A.Ş.; Mercuț, V. Modifications of the Dental Hard Tissues in the Cervical Area of Occlusally Overloaded Teeth Identified Using Optical Coherence Tomography. Medicina 2022, 58, 702. [Google Scholar] [CrossRef]
- Microscope Systems for Life Science Research & Healthcare|Nikon. Available online: https://www.microscope.healthcare.nikon.com/products/stereomicroscopes-macroscopes/smz745-745t (accessed on 7 July 2023).
- Mercut, V.; Popescu, S.M.; Scrieciu, M.; Amarascu, M.O.; Vatu, M.; Diaconu, O.A. Optical coherence tomography applications in tooth wear diagnosis. Rom. J. Morphol. Embryol. 2017, 58, 99–106. [Google Scholar]
- Popescu, S.M.; Mercut, V.; Scrieciu, M.; Mercut, R.; Popescu, F.D.; Chiriac, A.M.; Craitoiu, M.M.; Osiac, E. Radiological and optical coherence tomography aspects in external root resorption. Rom. J. Morphol. Embryol. 2017, 58, 131–137. [Google Scholar]
- Microscope Systems for Life Science Research & Healthcare|Nikon. Available online: https://www.microscope.healthcare.nikon.com/products/stereomicroscopes-macroscopes/smz745-745t/specifications (accessed on 7 July 2023).
- Swift, E.J., Jr.; Perdigão, J.; Heymann, H.O.; Wilder, A.D., Jr.; Bayne, S.C.; May, K.N., Jr.; Sturdevant, J.R.; Roberson, T.M. Eighteen-month clinical evaluation of a filled and unfilled dentin adhesive. J. Dent. 2001, 29, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, D.F.M.; Shinohara, M.S.; Carvalho, P.R.M.A.; Ramos, F.S.E.S.; Oliveira, L.C.; Omoto, É.M.; Fagundes, T.C. Three-year evaluation of different adhesion strategies in non-carious cervical lesion restorations: A randomized clinical trial. J. Appl. Oral Sci. 2021, 29, e20210192. [Google Scholar] [CrossRef]
- Schwendicke, F.; Müller, A.; Seifert, T.; Jeggle-Engbert, L.M.; Paris, S.; Göstemeyer, G. Glass hybrid versus composite for non-carious cervical lesions: Survival, restoration quality and costs in randomized controlled trial after 3 years. J. Dent. 2021, 110, 103689. [Google Scholar] [CrossRef] [PubMed]
- Cairo, F.; Cortellini, P.; Nieri, M.; Pilloni, A.; Barbato, L.; Pagavino, G.; Tonetti, M. Coronally advanced flap and composite restoration of the enamel with or without connective tissue graft for the treatment of single maxillary gingival recession with non-carious cervical lesion. A randomized controlled clinical trial. J. Clin. Periodontol. 2020, 47, 362–371. [Google Scholar] [CrossRef] [PubMed]
- Hunter, J. The Natural History of Human Teeth: Explaining Their Structure, Use, Formation, Growth, and Diseases; J. Johnson: London, UK, 1778; pp. 98–100. [Google Scholar]
- Grippo, J.O. Abfractions: A new classification of hard tissue lesions of teeth. J. Esthet. Dent. 1991, 3, 14–19. [Google Scholar] [CrossRef]
- Grippo, J.O.; Simring, M.; Schreiner, S. Attrition, abrasion, corrosion and abfraction revisited: A new perspective on tooth surface lesions. J. Am. Dent. Assoc. 2004, 135, 1109–1118. [Google Scholar] [CrossRef]
- Schlueter, N.; Amaechi, B.T.; Bartlett, D. Terminology of erosive tooth wear: Consensus report of a workshop organized by the ORCA and the Cariology Research Group of the IADR. Caries Res. 2020, 54, 2–6. [Google Scholar] [CrossRef]
- Mi-Kyoung, J.; Seok-Woo, P.; Eun-Song, L.; Bo-Ra, K.; Baek-Il, K. Diagnosis and management of cracked tooth by quantitative light-induced fluorescence technology. Photodiagnosis Photodyn. Ther. 2019, 26, 324–326. [Google Scholar] [CrossRef]
- Mi-Kyoung, J.; Hye-Min, K.; Euiseong, K.; Hee-Eun, K.; Ho-Keun, K.; Baek-Il, K. Detection and Analysis of Enamel Cracks by Quantitative Light-induced Fluorescence Technology. J. Endod. 2016, 42, 500–504. [Google Scholar] [CrossRef]
- Mukhatar, A.J.; Mohasin, A.K.; Razan, M.A.; Muna, J.A.; Thamra, M.A.; Mohamed, K.A. Spectrophotometric Analysis of Dental Enamel Staining to Antiseptic and Dietary Agents: In Vitro Study. Int. J. Dent. 2020, 2020, 5429725. [Google Scholar] [CrossRef]
- Olczak-Kowalczyk, D.; Krämer, N.; Gozdowski, D. Developmental enamel defects and their relationship with caries in adolescents aged 18 years. Sci. Rep. 2023, 13, 4932. [Google Scholar] [CrossRef] [PubMed]
- Bud, M.; Jitaru, S.; Lucaciu, O.; Korkut, B.; Dumitrascu-Timis, L.; Ionescu, C.; Cimpean, S.; Delean, A. The advantages of the dental operative microscope in restorative dentistry. Med. Pharm. Rep. 2021, 94, 22–27. [Google Scholar] [CrossRef]
- Tulkki, M.J.; Weissman, M. Advantages of advanced magnification. Decis. Dent. 2023, 9, 10,13–14,16. [Google Scholar]
- Simon-Stickley, A. Image and Imagination. The Stereomicroscope on the Cusp of Modern Biology. NTM J. Hist. Sci. Technol. Med. 2019, 27, 109–144. [Google Scholar] [CrossRef]
- Singh, S. Microscopes in conservative dentistry and endodontics research. J. Conserv. Dent. 2022, 25, 333–337. [Google Scholar] [CrossRef]
- Femiano, F.; Sorice, R.; Femiano, R.; Femiano, L.; Nucci, L.; Grassia, V.; Annunziata, M.; Baldi, A.; Scotti, N.; Nastri, L. Clinical Behavior of the Gingival Margin following Conservative “Coronally Dynamic” Restorations in the Presence of Non-Carious Cervical Lesions Associated with Gingival Recession: A Pilot Study. Dent. J. 2022, 10, 132. [Google Scholar] [CrossRef]
- Sugita, I.; Nakashima, S.; Ikeda, A.; Burrow, M.F.; Nikaido, T.; Kubo, S.; Tagami, J.; Sumi, Y. A pilot study to assess the morphology and progression of non-carious cervical lesions. J. Dent. 2017, 57, 51–56. [Google Scholar] [CrossRef]
- Luo, X.; Rong, Q.; Luan, Q.; Yu, X. Effect of partial restorative treatment on stress distributions in non-carious cervical lesions: A three-dimensional finite element analysis. BMC Oral Health 2022, 22, 607. [Google Scholar] [CrossRef]
- Abdalla, R.; Mitchell, R.J.; Ren, Y. Non-carious cervical lesions imaged by focus variation microscopy. J. Dent. 2017, 63, 14–20. [Google Scholar] [CrossRef]
- Igarashi, Y.; Yoshida, S.; Kanazawa, E. The prevalence and morphological types of non-carious cervical lesions (NCCL) in a contemporary sample of people. Odontology 2017, 105, 443–452. [Google Scholar] [CrossRef] [PubMed]
- Lai, Z.Y.; Zhi, Q.H.; Zhou, Y.; Lin, H.C. Prevalence of non-carious cervical lesions and associated risk indicators in middle-aged and elderly populations in Southern China. Chin. J. Dent. Res. 2015, 18, 41–50. [Google Scholar] [PubMed]
- Senna, P.; Del Bel Cury, A.; Rösing, C. Non-carious cervical lesions and occlusion: A systematic review of clinical studies. J. Oral Rehabil. 2012, 39, 450–462. [Google Scholar] [CrossRef] [PubMed]
- Bernhardt, O.; Gesch, D.; Schwahn, C.; Mack, F.; Meyer, G.; John, U.; Kocher, T. Epidemiological evaluation of the multifactorial aetiology of abfractions. J. Oral Rehabil. 2006, 33, 17–25. [Google Scholar] [CrossRef]
- Faye, B.; Sarr, M.; Kane, A.W.; Toure, B.; Leye, F.; Gaye, F.; Dieng, M.B. Prévalence et facteurs etiologiques des lésions cervicales non carieuses. Etude dans une population sénégalaise [Prevalence and etiologic factors of non-carious cervical lesions. A study in a Senegalese population]. Odontostomatol. Trop. 2005, 28, 15–18. [Google Scholar]
- Piotrowski, B.T.; Gillette, W.B.; Hancock, E.B. Examining the prevalence and characteristics of abfractionlike cervical lesions in a population of U.S. veterans. J. Am. Dent. Assoc. 2001, 132, 1694–1701. [Google Scholar] [CrossRef]
- Jomaa, K.; Abdul-Hak, M.; Almahdi, W.H.; Al Namly, M.R.; Hanafi, L. Efficacy of 810 nm and 650 nm Diode Laser Alone and in Combination With Sodium Fluoride Gel in Treating Dentin Hypersensitivity: A Split-Mouth Randomized Clinical Study. Cureus 2023, 15, e33489. [Google Scholar] [CrossRef]
- Moraschini, V.; da Costa, L.S.; dos Santos, G.O. Effectiveness for dentin hypersensitivity treatment of non-carious cervical lesions: A meta-analysis. Clin. Oral Investig. 2018, 22, 617–631. [Google Scholar] [CrossRef]
- Loomba, K.; Bains, R.; Bains, V.K.; Loomba, A. Proposal for clinical classification of multifactorial noncarious cervical lesions. Gen. Dent. 2014, 62, 39–44. [Google Scholar]
- Walter, C.; Kress, E.; Götz, H.; Taylor, K.; Willershausen, I.; Zampelis, A. The anatomy of non-carious cervical lesions. Clin. Oral Investig. 2014, 18, 139–146. [Google Scholar] [CrossRef]
- Stanusi, A.; Mercuţ, V.; Scrieciu, M.; Popescu, S.M.; Craitoiu-Iacov, M.M.; Daguci, L.; Castravete, S.; Vintila, D.D.; Vatu, M. Effects of occlusal loads in the genesis of non-carious cervical lesions—A finite element study. Rom. J. Oral Rehabil. 2019, 11, 73–81. [Google Scholar]
- Vandana, K.; Deepti, M.; Shaimaa, M.; Naveen, K.; Rajendra, D. A finite element study to determine the occurrence of abfraction and displacement due to various occlusal factors and with different alveolar bone height. J. Indian Soc. Periodontol. 2016, 20, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Jakupovic, S.; Cerjakovic, E.; Topcic, A.; Ajanovic, M.; Konjhodzicprcic, A.; Vukovic, A. Analysis of the abfraction lesions formation mechanism by the finite element method. Acta Inf. Med. 2014, 22, 241–245. [Google Scholar] [CrossRef] [PubMed]
- Borcic, J.; Anic, I.; Smojver, I.; Catic, A.; Miletic, I.; Ribaric, S.P. 3D finite element model and cervical lesion formation in normal occlusion and in malocclusion. J. Oral Rehabil. 2005, 32, 504–510. [Google Scholar] [CrossRef]
- Tanaka, M.; Naito, T.; Yokota, M.; Kohno, M. Finite element analysis of the possible mechanism of cervical lesion formation by occlusal force. J. Oral Rehabil. 2003, 30, 60–67. [Google Scholar] [CrossRef]
- Machado, A.C.; Soares, C.J.; Reis, B.R.; Bicalho, A.A.; Raposo, L.; Soares, P.V. Stress-strain analysis of premolars with non-carious cervical lesions: Influence of restorative material, loading direction and mechanical fatigue. Oper. Dent. 2017, 42, 253–265. [Google Scholar] [CrossRef]
- Vlăduțu, D.E.; Ionescu, M.; Noveri, L.; Manolea, H.O.; Scrieciu, M.; Popescu, S.M.; Turcu, A.A.; Ştefârță, A.; Lăzărescu, G.; Mercuț, V. Aspects of Dental Occlusion Assessed with the T-Scan System among a Group of Romanian Dental Students in a Cross-Sectional Study. Int. J. Environ. Res. Public Health 2023, 20, 4877. [Google Scholar] [CrossRef]
- Nascimento, B.L.; Vieira, A.R.; Bezamat, M. Occlusal problems, mental health issues and non-carious cervical lesions. Odontology 2022, 110, 349–355. [Google Scholar] [CrossRef]
- Hussainy, S.N.; Nasim, I.; Thomas, T.; Ranjan, M. Clinical performance of resin-modified glass ionomer cement, flowable composite, and polyacid-modified resin composite in non-carious cervical lesions: One-year follow-up. J. Conserv. Dent. 2018, 21, 510–515. [Google Scholar] [CrossRef]
- Turssi, C.P.; Kelly, A.B.; Hara, A.T. Toothbrush bristle configuration and brushing load: Effect on the development of simulated non-carious cervical lesions. J. Dent. 2019, 86, 75–80. [Google Scholar] [CrossRef]
- Michael, J.A.; Kaidonis, J.A.; Townsend, G.C. Non-carious cervical lesions on permanent anterior teeth: A new morphological classification. Aust. Dent. J. 2010, 55, 134–137. [Google Scholar] [CrossRef] [PubMed]
- Dzakovich, J.J.; Oslak, R.R. In vitro reproduction of noncarious cervical lesions. J. Prosthet. Dent. 2008, 100, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Hughes, C.V.; Dean, J.A. Mechanical and Chemotherapeutic Home Oral Hygiene. In McDonald and Avery’s Dentistry for the Child and Adolescent; Jeffrey, A., Ed.; Mosby: Maryland Heights, MO, USA; pp. 120–137.
- Lührs, A.; Jacker-Guhr, S.; Günay, H.; Herrmann, P. Composite restorations placed in non-carious cervical lesions—Which cavity preparation is clinically reliable? Clin. Exp. Dent. Res. 2020, 6, 558–567. [Google Scholar] [CrossRef]
- Aw, T.C.; Lepe, X.; Johnson, G.H.; Mancl, L. Characteristics of noncarious cervical lesions: A clinical investigation. J. Am. Dent. Assoc. 2002, 133, 725–733. [Google Scholar] [CrossRef]
- Rocha, A.C.; Da Rosa, W.; Cocco, A.R.; Da Silva, A.F.; Piva, E.; Lund, R.G. Influence of Surface Treatment on Composite Adhesion in Noncarious Cervical Lesions: Systematic Review and Meta-analysis. Oper. Dent. 2018, 43, 508–519. [Google Scholar] [CrossRef]






Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stănuşi, A.; Stănuşi, A.Ş.; Gîngu, O.; Mercuţ, V.; Osiac, E. Stereomicroscopic Aspects of Non-Carious Cervical Lesions. Diagnostics 2023, 13, 2590. https://doi.org/10.3390/diagnostics13152590
Stănuşi A, Stănuşi AŞ, Gîngu O, Mercuţ V, Osiac E. Stereomicroscopic Aspects of Non-Carious Cervical Lesions. Diagnostics. 2023; 13(15):2590. https://doi.org/10.3390/diagnostics13152590
Chicago/Turabian StyleStănuşi, Andreea, Adrian Ştefan Stănuşi, Oana Gîngu, Veronica Mercuţ, and Eugen Osiac. 2023. "Stereomicroscopic Aspects of Non-Carious Cervical Lesions" Diagnostics 13, no. 15: 2590. https://doi.org/10.3390/diagnostics13152590
APA StyleStănuşi, A., Stănuşi, A. Ş., Gîngu, O., Mercuţ, V., & Osiac, E. (2023). Stereomicroscopic Aspects of Non-Carious Cervical Lesions. Diagnostics, 13(15), 2590. https://doi.org/10.3390/diagnostics13152590




