Laparoscopic Extended Left Lateral Sectionectomy for Hepatocellular Carcinoma in a Patient with Right-Sided Ligamentum Teres: A Case Report and Literature Review
Abstract
1. Introduction
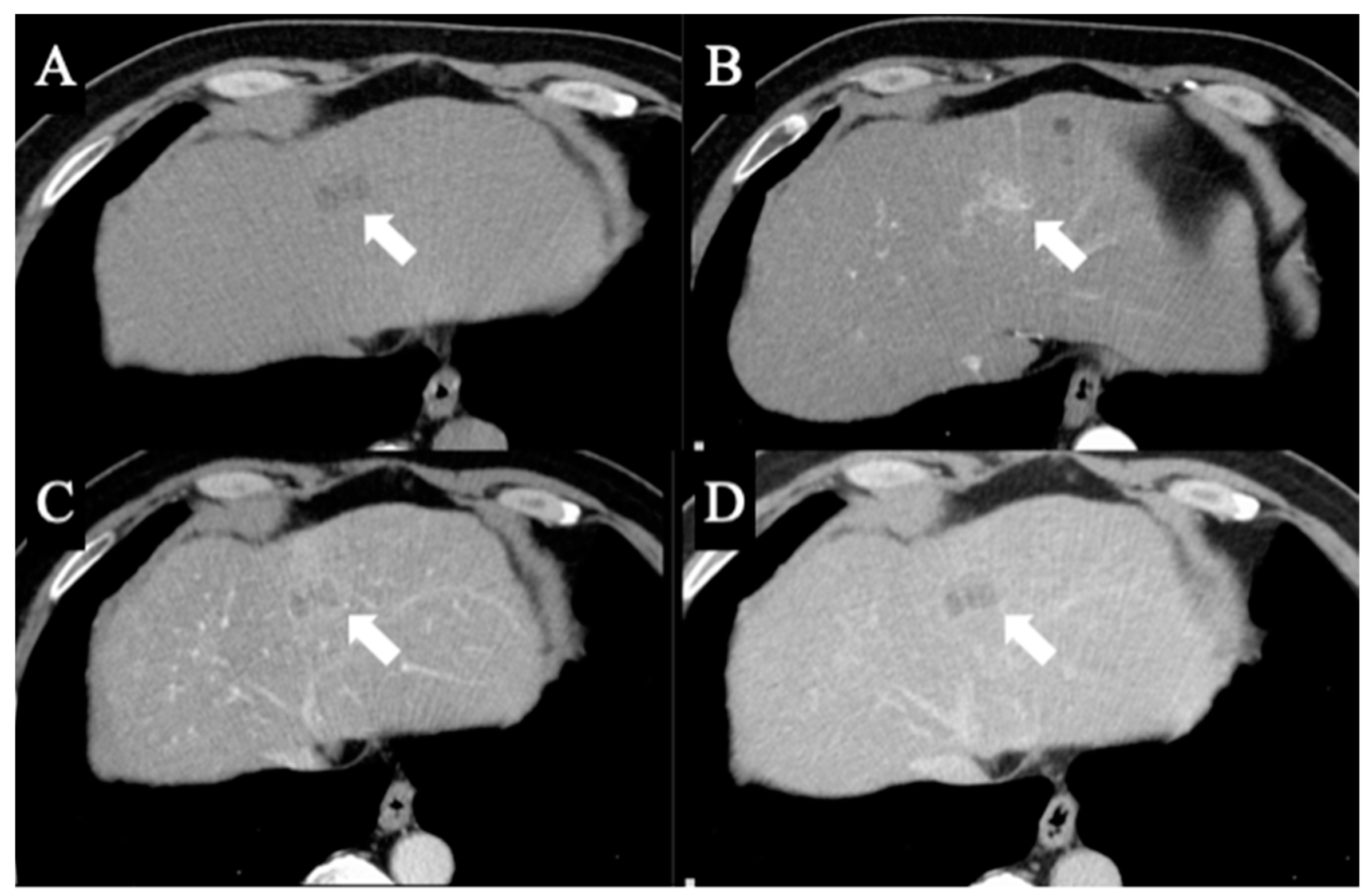
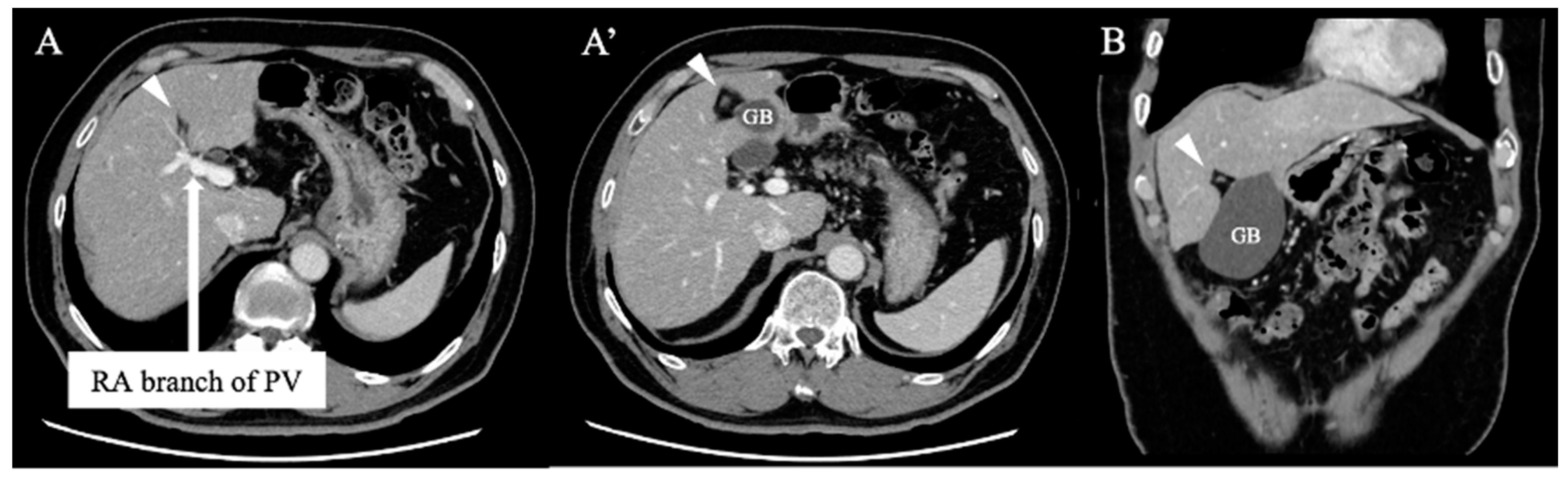
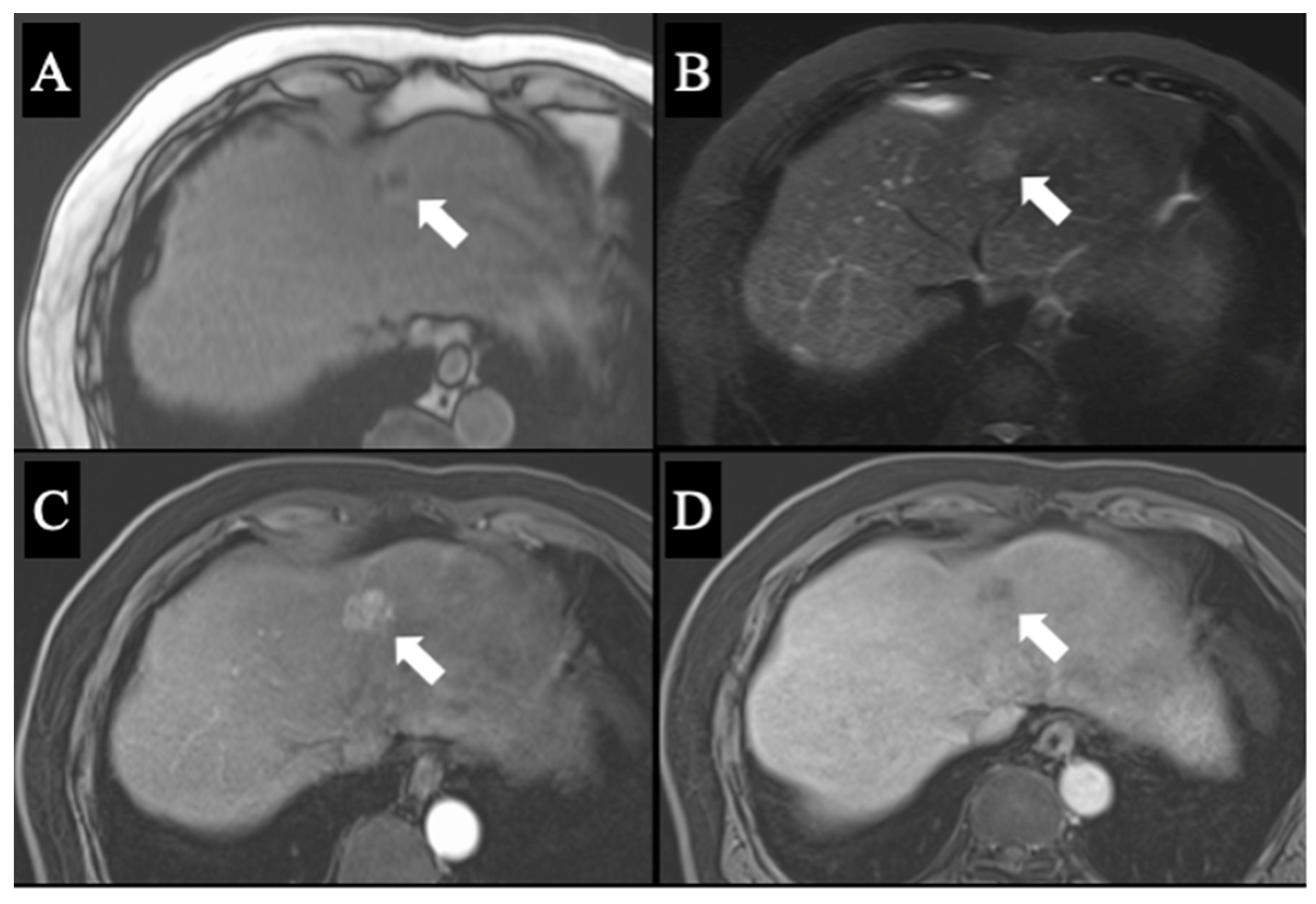
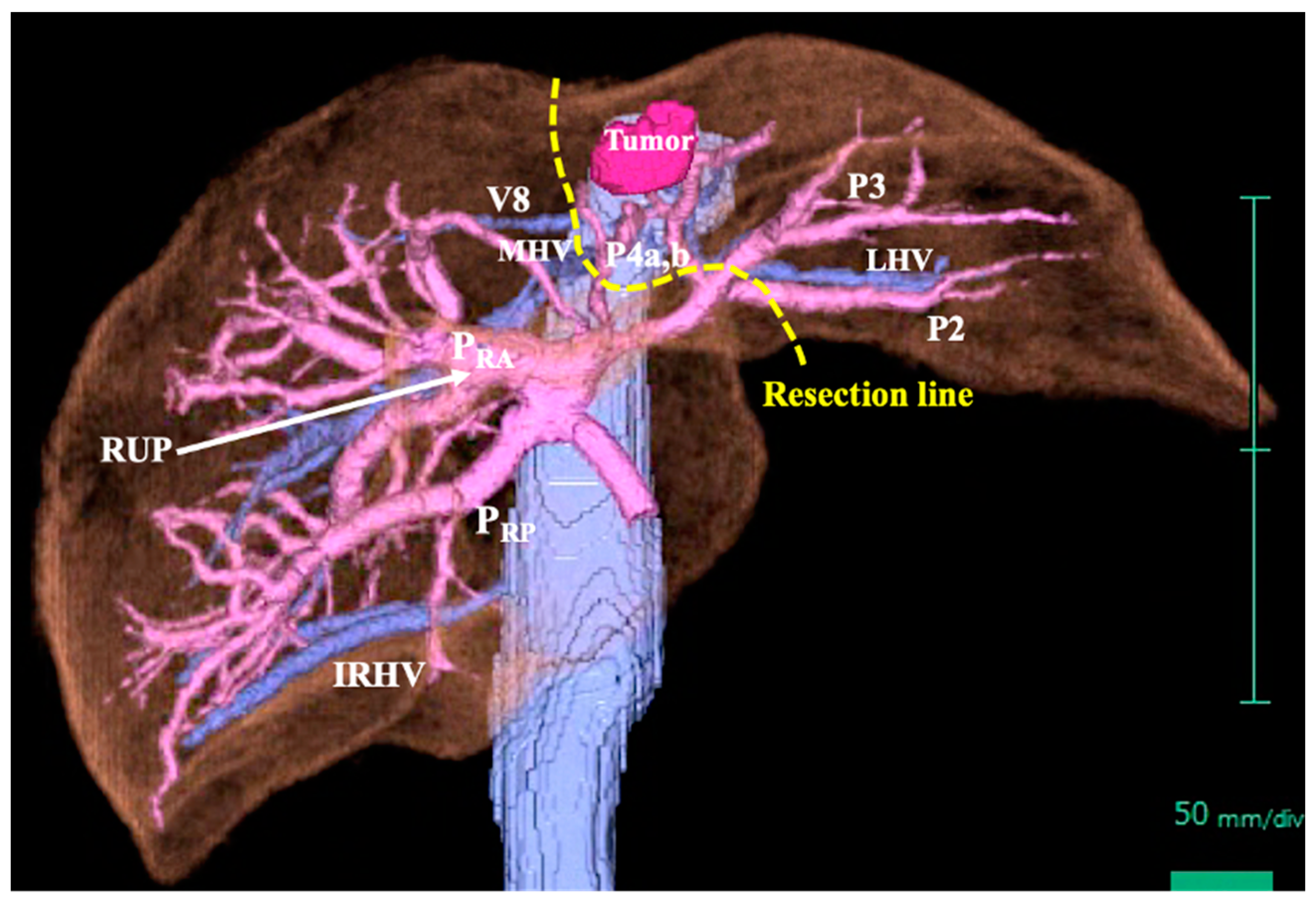
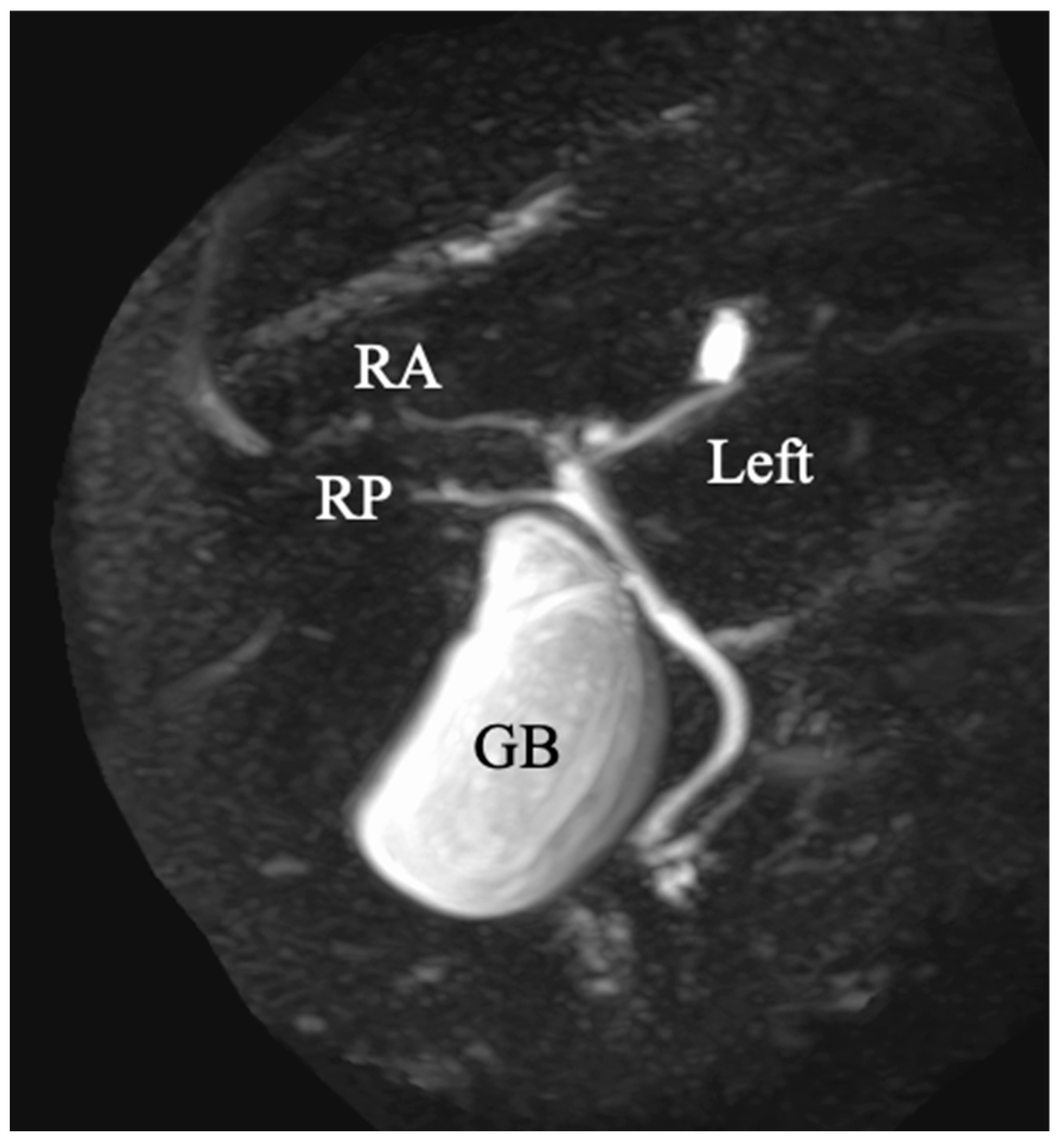
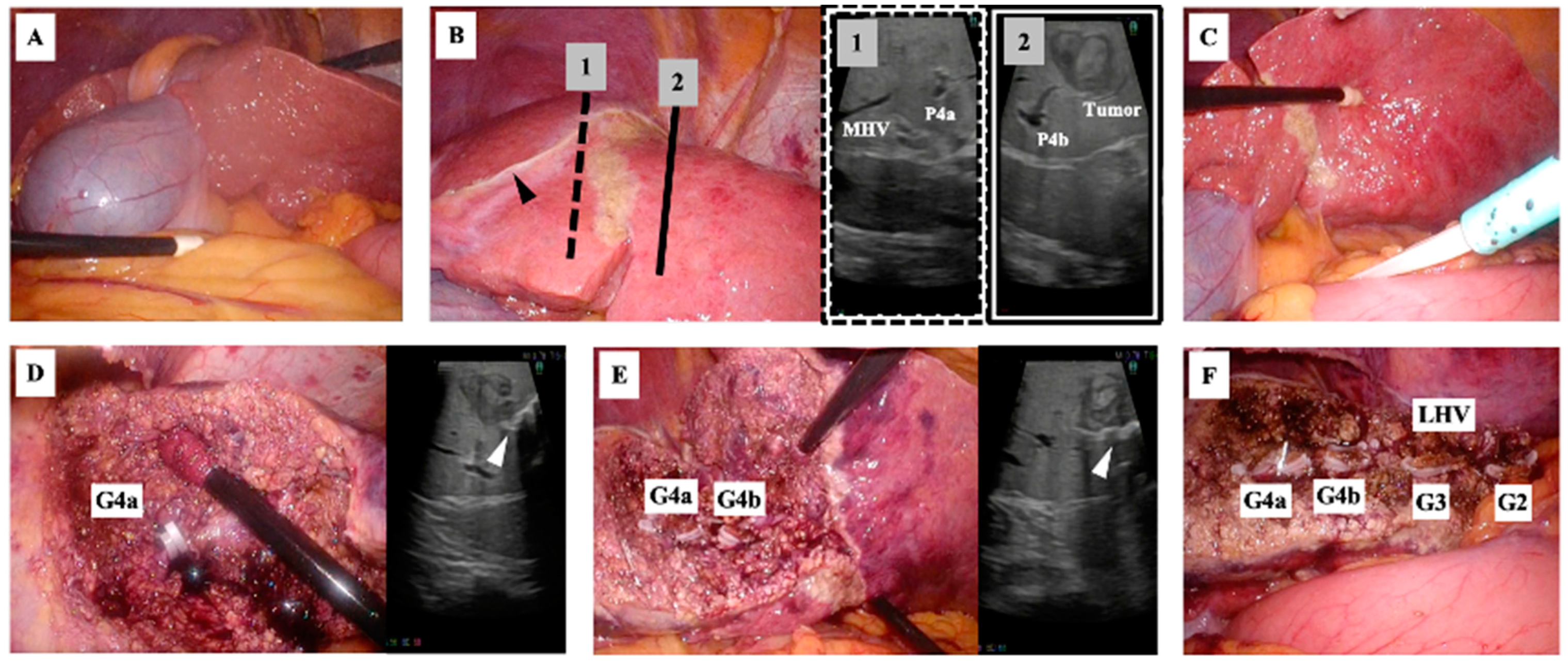
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shindoh, J.; Akahane, M.; Satou, S.; Aoki, T.; Beck, Y.; Hasegawa, K.; Sugawara, Y.; Ohtomo, K.; Kokudo, N. Vascular architecture in anomalous right-sided ligamentum teres: Three-dimensional analyses in 35 patients. HPB 2012, 14, 32–41. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Nagai, M.; Kubota, K.; Kawasaki, S.; Takayama, T.; Bandai, Y.; Makuuchi, M. Are left-sided gallbladders really located on the left side? Ann. Surg. 1997, 225, 274–280. [Google Scholar] [CrossRef] [PubMed]
- Maetani, Y.; Itoh, K.; Kojima, N.; Tabuchi, T.; Shibata, T.; Asonuma, K.; Tanaka, K.; Konishi, J. Portal vein anomaly associated with deviation of the ligamentum teres to the right and malposition of the gallbladder. Radiology 1998, 207, 723–728. [Google Scholar] [CrossRef] [PubMed]
- Saafan, T.; Hu, J.Y.; Mahfouz, A.E.; Abdelaal, A. True left-sided gallbladder: A case report and comparison with the literature for the different techniques of laparoscopic cholecystectomy for such anomalies. Int. J. Surg. Case Rep. 2018, 42, 280–286. [Google Scholar] [CrossRef] [PubMed]
- Terasaki, F.; Yamamoto, Y.; Sugiura, T.; Okamura, Y.; Ito, T.; Ashida, R.; Ohgi, K.; Aramaki, T.; Uesaka, K. Analysis of right-sided ligamentum teres: The novel anatomical findings and classification. J. Hepatobiliary Pancreat. Sci. 2021, 28, 221–230. [Google Scholar] [CrossRef] [PubMed]
- Terasaki, F.; Yamamoto, Y.; Ohgi, K.; Sugiura, T.; Okamura, Y.; Ito, T.; Ashida, R.; Uesaka, K. Laparoscopic left lateral sectionectomy for a patient with right-sided ligamentum teres. Surg. Case Rep. 2019, 5, 43. [Google Scholar] [CrossRef] [PubMed]
- Terasaki, F.; Yamamoto, Y.; Sugiura, T.; Okamura, Y.; Ito, T.; Ashida, R.; Ohgi, K.; Akamoto, S.; Uesaka, K. A case of perihilar cholangiocarcinoma with bilateral ligamentum teres hepatis treated with hepatopancreatoduodenectomy. Surg. Case Rep. 2020, 6, 32. [Google Scholar] [CrossRef] [PubMed]
- Nishitai, R.; Shindoh, J.; Yamaoka, T.; Akahane, M.; Kokudo, N.; Manaka, D. Biliary architecture of livers exhibiting right-sided ligamentum teres: An indication for preoperative cholangiography prior to major hepatectomy. HPB 2016, 18, 929–935. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Uesaka, K.; Yasui, K.; Morimoto, T.; Torii, A.; Kodera, Y.; Hirai, T.; Yamamura, Y.; Kato, T.; Kito, T. Left-Sided gallbladder with intrahepatic portal venous anomalies. J. Hepato-Biliary-Pancreat. Surg. 1995, 2, 425–430. [Google Scholar] [CrossRef]
- Kaneoka, Y.; Yamaguchi, A.; Isogai, M.; Harada, T. Hepatectomy for cholangiocarcinoma complicated with right umbilical portion: Anomalous configuration of the intrahepatic biliary tree. J. Hepatobiliary Pancreat. Surg. 2000, 7, 321–326. [Google Scholar] [CrossRef]
- Tashiro, H.; Itamoto, T.; Nakahara, H.; Ohdan, H.; Kobayashi, T.; Asahara, T. Resection of hepatocellular carcinoma in a patient with congenital anomaly of the portal system. Dig. Surg. 2003, 20, 163–165. [Google Scholar] [CrossRef]
- Sakaguchi, T.; Suzuki, S.; Morita, Y.; Oishi, K.; Suzuki, A.; Fukumoto, K.; Inaba, K.; Takehara, Y.; Baba, S.; Nakamura, S.; et al. Hepatectomy for metastatic liver tumors complicated with right umbilical portion. Hepatogastroenterology 2011, 58, 984–987. [Google Scholar]
- Abe, T.; Kajiyama, K.; Harimoto, N.; Gion, T.; Shirabe, K.; Nagaie, T. Resection of metastatic liver cancer in a patient with a left-sided gallbladder and intrahepatic portal vein and bile duct anomalies: A case report. Int. J. Surg. Case Rep. 2012, 3, 147–150. [Google Scholar] [CrossRef][Green Version]
- Almodhaiberi, H.; Hwang, S.; Cho, Y.J.; Kwon, Y.; Jung, B.H.; Kim, M.H. Customized left-sided hepatectomy and bile duct resection for perihilar cholangiocarcinoma in a patient with left-sided gallbladder and multiple combined anomalies. Korean J. Hepatobiliary Pancreat. Surg. 2015, 19, 30–34. [Google Scholar] [CrossRef] [PubMed]
- Ome, Y.; Kawamoto, K.; Park, T.B.; Ito, T. Major hepatectomy using the glissonean approach in cases of right umbilical portion. World J. Hepatol. 2016, 8, 1535–1540. [Google Scholar] [CrossRef]
- Hai, S.; Hatano, E.; Hirano, T.; Asano, Y.; Suzumura, K.; Sueoka, H.; Fujimoto, J. Hepatectomy for Hilar Cholangiocarcinoma with Right-Sided Ligamentum Teres Using a Hepatectomy Simulation System. Case Rep. Gastroenterol. 2017, 11, 576–583. [Google Scholar] [CrossRef]
- Goto, T.; Terajima, H.; Yamamoto, T.; Uchida, Y. Hepatectomy for gallbladder-cancer with unclassified anomaly of right-sided ligamentum teres: A case report and review of the literature. World J. Hepatol. 2018, 10, 523–529. [Google Scholar] [CrossRef]
| No | Author | Year | Age | Sex | Disease | Operation | Open/Lap | Complication | Portal Vein Branching Type |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Uesaka et al. [9] | 1995 | 53 | M | Liver metastasis of CC | Right hemihepatectomy | Open | - | Independent right lateral |
| 2 | Nagai et al. [2] | 1997 | 67 | M | HCC | Segmentectomy 8, and partial resection of segment 1 | Open | - | Independent right lateral |
| 3 | Nagai et al. [2] | 67 | M | Hilar CC | HPD | Open | - | Independent right lateral | |
| 4 | Kaneoka et al. [10] | 2000 | 53 | M | Hilar CC | Extended left hemihepatectomy with extrahepatic bile duct resection | Open | - | Independent right lateral |
| 5 | Kaneoka et al. [10] | 61 | M | Extrahepatic CC | HPD | Open | - | Independent right lateral | |
| 6 | Tashiro et al. [11] | 2003 | 53 | M | HCC | Partial hepatectomy | Open | - | Independent right lateral |
| 7 | Sakaguchi et al. [12] | 2011 | 76 | M | CRLM | Extended right posterior sectionectomy | Open | - | Independent right lateral |
| 8 | Abe et al. [13] | 2012 | 70 | F | CRLM | Right hemihepatectomy | Open | - | Bifurcation |
| 9 | Almodhaiberi et al. [14] | 2015 | 67 | M | Hilar CC | Extended left lateral sectionectomy with extrahepatic bile duct resection | Open | - | Trifurcation |
| 10 | Ome et al. [15] | 2016 | 70 | M | ICC | Right anterior sectionectomy | Open | - | Trifurcation |
| 11 | Ome et al. [15] | 70 | F | Hilar CC | Left trisectionectomy with extrahepatic bile duct resection | Open | - | Trifurcation | |
| 12 | Hai et al. [16] | 2017 | 78 | M | Hilar CC | Extended left hemihepatectomy | Open | Bile leakage | Independent right lateral |
| 13 | Goto et al. [17] | 2018 | 70s | M | GC | Right hemihepatectomy | Open | - | other |
| 14 | Terasaki et al. [6] | 2019 | 63 | M | CRLM | Left lateral sectionectomy | Lap | - | Bifurcation |
| 15 | Terasaki et al. [8] | 2020 | 72 | M | Hilar CC | HDP | Open | - | Bilateral |
| 16 | Our case | 2021 | 69 | M | HCC | Extended left lateral sectionectomy | Lap | - | Independent right lateral |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adachi, Y.; Takahashi, H.; Yamamoto, T.; Hagiwara, M.; Imai, K.; Yokoo, H. Laparoscopic Extended Left Lateral Sectionectomy for Hepatocellular Carcinoma in a Patient with Right-Sided Ligamentum Teres: A Case Report and Literature Review. Diagnostics 2023, 13, 2529. https://doi.org/10.3390/diagnostics13152529
Adachi Y, Takahashi H, Yamamoto T, Hagiwara M, Imai K, Yokoo H. Laparoscopic Extended Left Lateral Sectionectomy for Hepatocellular Carcinoma in a Patient with Right-Sided Ligamentum Teres: A Case Report and Literature Review. Diagnostics. 2023; 13(15):2529. https://doi.org/10.3390/diagnostics13152529
Chicago/Turabian StyleAdachi, Yuki, Hiroyuki Takahashi, Tomohiro Yamamoto, Masahiro Hagiwara, Koji Imai, and Hideki Yokoo. 2023. "Laparoscopic Extended Left Lateral Sectionectomy for Hepatocellular Carcinoma in a Patient with Right-Sided Ligamentum Teres: A Case Report and Literature Review" Diagnostics 13, no. 15: 2529. https://doi.org/10.3390/diagnostics13152529
APA StyleAdachi, Y., Takahashi, H., Yamamoto, T., Hagiwara, M., Imai, K., & Yokoo, H. (2023). Laparoscopic Extended Left Lateral Sectionectomy for Hepatocellular Carcinoma in a Patient with Right-Sided Ligamentum Teres: A Case Report and Literature Review. Diagnostics, 13(15), 2529. https://doi.org/10.3390/diagnostics13152529







