Hepatic Venous Pressure Gradient Predicts Further Decompensation in Cirrhosis Patients with Acute Esophageal Variceal Bleeding
Abstract
1. Introduction
2. Materials and Methods
2.1. Management of Acute Variceal Bleeding
Primary and Secondary Outcomes
2.2. Statistical Analysis
3. Results
3.1. Baseline Characteristics
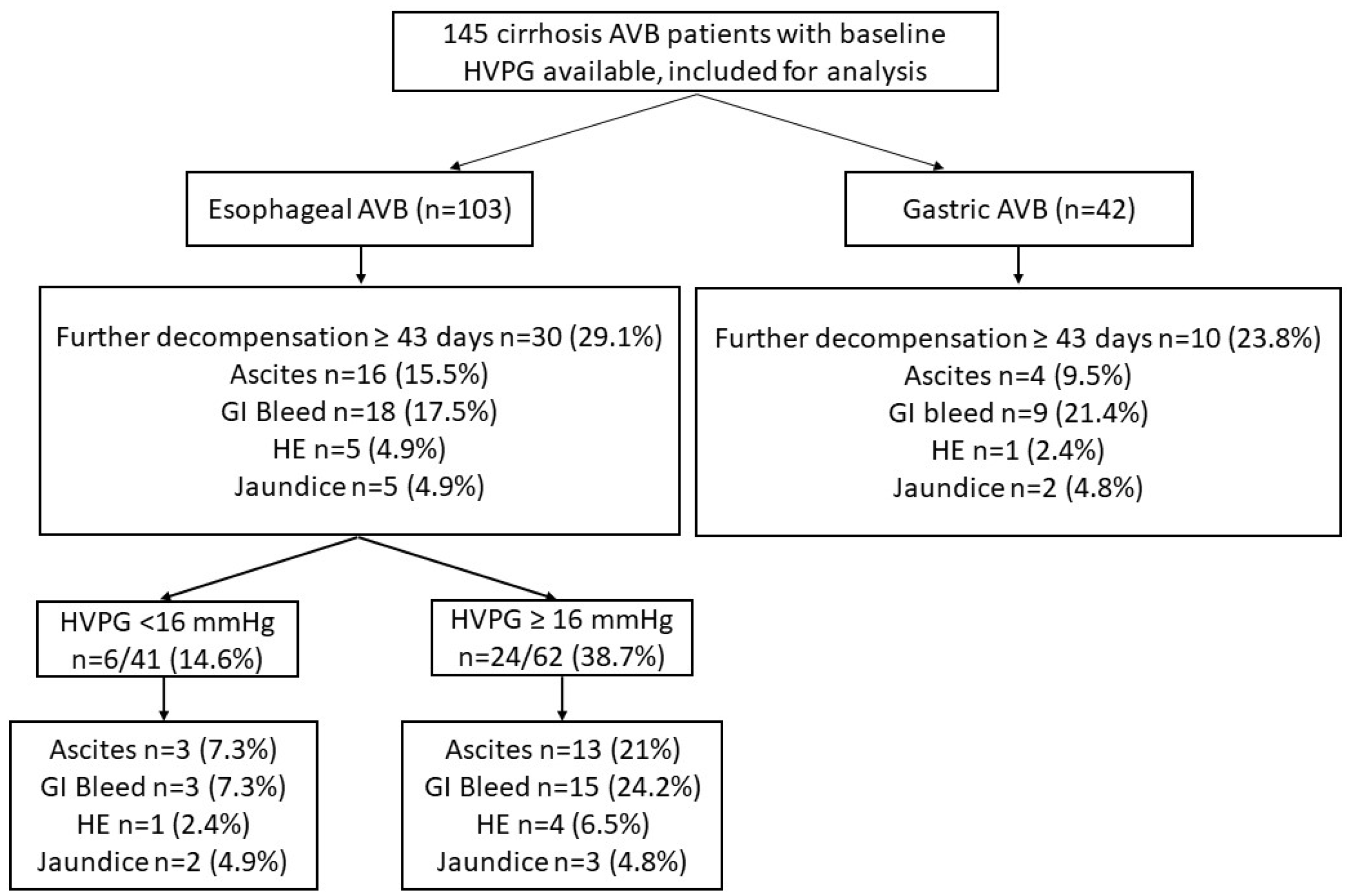
3.2. Further Decompensation in Esophageal and Gastric AVB Cohort
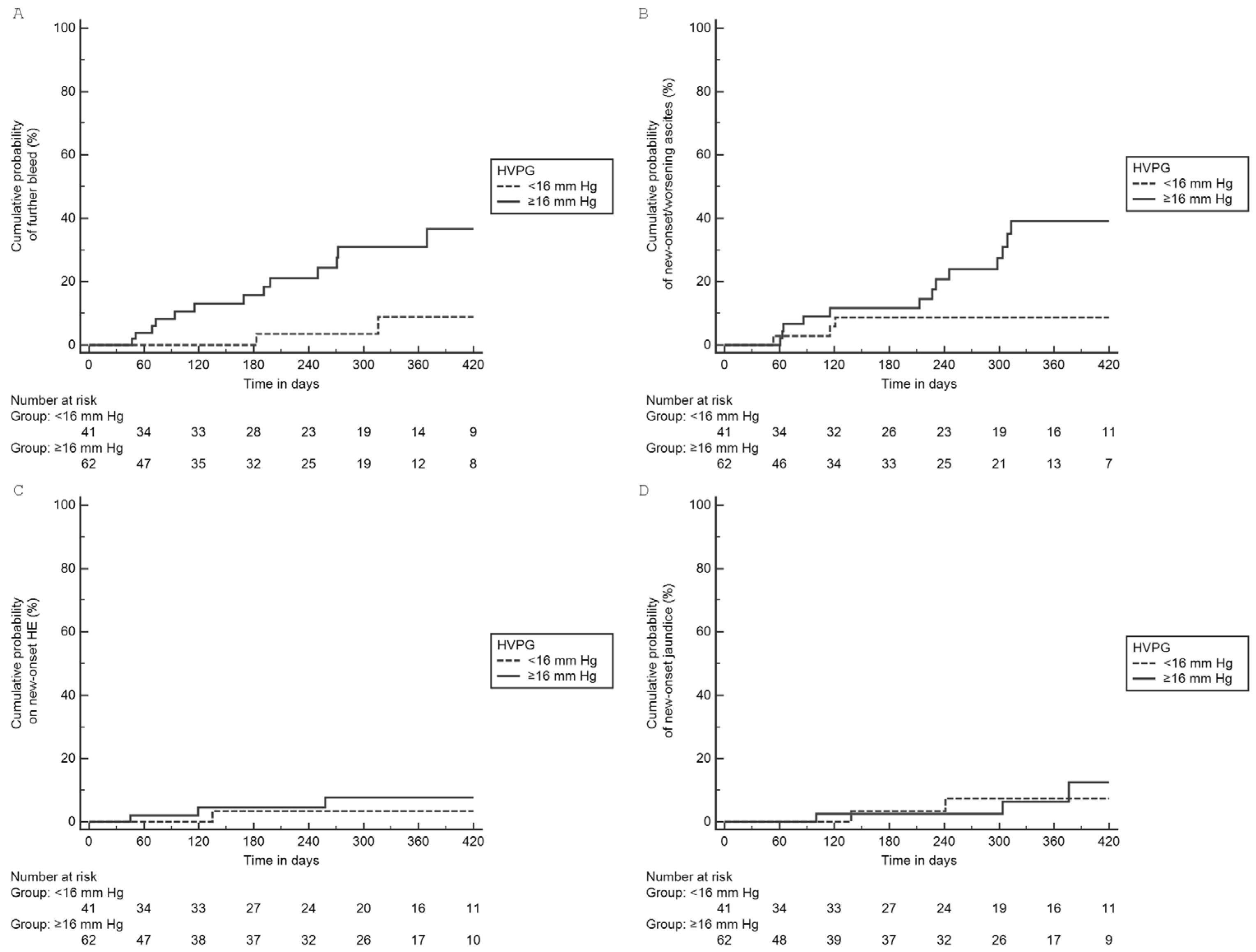
3.3. HVPG as a Predictor of Further Decompensation
3.4. Comparison of Esophageal AVB Based on HVPG Cutoff Value of 16 mmHg
3.5. Causes of Mortality
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ripoll, C.; Groszmann, R.J.; Garcia-Tsao, G.; Bosch, J.; Grace, N.; Burroughs, A.; Planas, R.; Escorsell, A.; Garcia-Pagan, J.C.; Makuch, R.; et al. Hepatic venous pressure gradient predicts development of hepatocellular carci-noma independently of severity of cirrhosis. J. Hepatol. 2009, 50, 923–928. [Google Scholar] [CrossRef]
- Reverter, E.; Cirera, I.; Albillos, A.; Debernardi-Venon, W.; Abraldes, J.G.; Llop, E.; Flores, A.; Martínez-Palli, G.; Blasi, A.; Martínez, J.; et al. The prognostic role of hepatic venous pressure gradient in cirrhotic patients undergoing elective extrahepatic surgery. J. Hepatol. 2019, 71, 942–950. [Google Scholar] [CrossRef] [PubMed]
- Ripoll, C.; Groszmann, R.; Garcia-Tsao, G.; Grace, N.; Burroughs, A.; Planas, R.; Escorsell, A.; Garcia-Pagan, J.C.; Makuch, R.; Patch, D.; et al. Hepatic Venous Pressure Gradient Predicts Clinical Decompensation in Patients with Compensated Cirrhosis. Gastroenterology 2007, 133, 481–488. [Google Scholar] [CrossRef] [PubMed]
- Groszmann, R.J.; Garcia-Tsao, G.; Bosch, J.; Grace, N.D.; Burroughs, A.K.; Planas, R.; Escorsell, A.; Garcia-Pagan, J.C.; Patch, D.; Matloff, D.S.; et al. Beta-Blockers to Prevent Gastroesophageal Varices in Patients with Cirrhosis. N. Engl. J. Med. 2005, 353, 2254–2261. [Google Scholar] [CrossRef] [PubMed]
- Villanueva, C.; Torres, F.; Sarin, S.K.; Shah, H.A.; Tripathi, D.; Brujats, A.; Rodrigues, S.G.; Bhardwaj, A.; Azam, Z.; Hayes, P.C.; et al. Carvedilol reduces the risk of decompensation and mortality in patients with compensated cirrhosis in a competing-risk meta-analysis. J. Hepatol. 2022, 77, 1014–1025. [Google Scholar] [CrossRef]
- Mandorfer, M.; Kozbial, K.; Schwabl, P.; Chromy, D.; Semmler, G.; Stättermayer, A.F.; Pinter, M.; Hernández-Gea, V.; Fritzer-Szekeres, M.; Steindl-Munda, P.; et al. Changes in Hepatic Venous Pressure Gradient Predict Hepatic Decompensation in Patients Who Achieved Sustained Virologic Response to Interferon-Free Therapy. Hepatology 2020, 71, 1023–1036. [Google Scholar] [CrossRef]
- Jindal, A.; Bhardwaj, A.; Kumar, G.; Sarin, S.K. Clinical Decompensation and Outcomes in Patients with Compensated Cirrhosis and a Hepatic Venous Pressure Gradient ≥20 mm Hg. Am. J. Gastroenterol. 2020, 115, 1624–1633. [Google Scholar] [CrossRef]
- Moitinho, E.; Escorsell, À.; Bandi, J.; Salmerón, J.; García-Pagán, J.; Rodés, J.; Bosch, J. Prognostic value of early measurements of portal pressure in acute variceal bleeding. Gastroenterology 1999, 117, 626–631. [Google Scholar] [CrossRef]
- Sarin, S.K.; Lahoti, D.; Saxena, S.P.; Murthy, N.S.; Makwana, U.K. Prevalence, classification and natural history of gastric varices: A long-term follow-up study in 568 portal hypertension patients. Hepatology 1992, 16, 1343–1349. [Google Scholar] [CrossRef]
- Garcia-Tsao, G.; Abraldes, J.G.; Berzigotti, A.; Bosch, J. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology 2017, 65, 310–335. [Google Scholar] [CrossRef]
- de Franchis, R.; Bosch, J.; Garcia-Tsao, G.; Reiberger, T.; Ripoll, C.; Abraldes, J.G.; Albillos, A.; Baiges, A.; Bajaj, J.; Bañares, R.; et al. Baveno VII—Renewing consensus in portal hypertension. J. Hepatol. 2022, 76, 959–974. [Google Scholar] [CrossRef] [PubMed]
- Bosch, J. Carvedilol for portal hypertension in patients with cirrhosis. Hepatology 2010, 51, 2214–2218. [Google Scholar] [CrossRef] [PubMed]
- Heimbach, J.K.; Kulik, L.M.; Finn, R.S.; Sirlin, C.B.; Abecassis, M.M.; Roberts, L.R.; Zhu, A.X.; Murad, M.H.; Marrero, J.A. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology 2018, 67, 358–380. [Google Scholar] [CrossRef] [PubMed]
- Dharel, N.; Bajaj, J.S. Definition and Nomenclature of Hepatic Encephalopathy. J. Clin. Exp. Hepatol. 2015, 5, S37–S41. [Google Scholar] [CrossRef] [PubMed]
- de Franchis, R. Evolving consensus in portal hypertension. Report of the Baveno IV consensus workshop on methodology of diagnosis and therapy in portal hypertension. J. Hepatol. 2005, 43, 167–176. [Google Scholar] [CrossRef] [PubMed]
- D’Amico, G.; Bernardi, M.; Angeli, P. Towards a new definition of decompensated cirrhosis. J. Hepatol. 2022, 76, 202–207. [Google Scholar] [CrossRef]
- Trebicka, J.; Fernandez, J.; Papp, M.; Caraceni, P.; Laleman, W.; Gambino, C.; Giovo, I.; Uschner, F.E.; Jimenez, C.; Mookerjee, R.; et al. The PREDICT study uncovers three clinical courses of acutely decompensated cirrhosis that have distinct pathophysiology. J. Hepatol. 2020, 73, 842–854. [Google Scholar] [CrossRef]
- Kim, T.; Shijo, H.; Kokawa, H.; Tokumitsu, H.; Kubara, K.; Ota, K.; Akiyoshi, N.; Iida, T.; Yokoyama, M.; Okumura, M. Risk factors for hemorrhage from gastric fundal varices. Hepatology 1997, 25, 307–312. [Google Scholar] [CrossRef]
- Zaman, A.; Becker, T.; Lapidus, J.; Benner, K. Risk Factors for the Presence of Varices in Cirrhotic Patients without a History of Variceal Hemorrhage. Arch. Intern. Med. 2001, 161, 2564–2570. [Google Scholar] [CrossRef]
- Lee, C.H.; Lee, J.H.; Choi, Y.S.; Paik, S.W.; Sinn, D.H.; Lee, C.Y.; Koh, K.C.; Gwak, G.Y.; Choi, M.S.; Yoo, B.C. Natural history of gastric varices and risk factors for bleeding. Korean J. Hepatol. 2008, 14, 331–341. [Google Scholar] [CrossRef]
- Luo, X.; Hernández-Gea, V. Update on the management of gastric varices. Liver Int. 2022, 42, 1250–1258. [Google Scholar] [CrossRef] [PubMed]
- De Franchis, R. (Ed.) Portal Hypertension VII: Proceedings of the 7th Baveno Consensus Workshop: Personalized Care in Portal Hypertension; Springer Nature: Berlin/Heidelberg, Germany, 2022. [Google Scholar]
- Boregowda, U.; Umapathy, C.; Halim, N.; Desai, M.; Nanjappa, A.; Arekapudi, S.; Theethira, T.; Wong, H.; Roytman, M.; Saligram, S. Update on the management of gastrointestinal varices. World J. Gastrointest. Pharmacol. Ther. 2019, 10, 1–21. [Google Scholar] [CrossRef] [PubMed]
- La Mura, V.; Garcia-Guix, M.; Berzigotti, A.; Abraldes, J.G.; García-Pagán, J.C.; Villanueva, C.; Bosch, J. A Prognostic Strategy Based on Stage of Cirrhosis and HVPG to Improve Risk Stratification after Variceal Bleeding. Hepatology 2020, 72, 1353–1365. [Google Scholar] [CrossRef] [PubMed]
- D’Amico, G.; Garcia-Tsao, G.; Pagliaro, L. Natural history and prognostic indicators of survival in cirrhosis: A systematic review of 118 studies. J. Hepatol. 2006, 44, 217–231. [Google Scholar] [CrossRef] [PubMed]
- Zipprich, A.; Garcia-Tsao, G.; Rogowski, S.; Fleig, W.E.; Seufferlein, T.; Dollinger, M.M. Prognostic indicators of survival in patients with compensated and decompensated cirrhosis. Liver Int. 2012, 32, 1407–1414. [Google Scholar] [CrossRef]
- Urrunaga, N.H.; Mindikoglu, A.L.; Rockey, D.C. Renal dysfunction in cirrhosis. Curr. Opin. Gastroenterol. 2015, 31, 215–223. [Google Scholar] [CrossRef]
- Bucsics, T.; Krones, E. Renal dysfunction in cirrhosis: Acute kidney injury and the hepatorenal syndrome. Gastroenterol. Rep. 2017, 5, 127–137. [Google Scholar] [CrossRef]
- Jalan, R.; Fernandez, J.; Wiest, R.; Schnabl, B.; Moreau, R.; Angeli, P.; Stadlbauer, V.; Gustot, T.; Bernardi, M.; Canton, R.; et al. Bacterial infections in cirrhosis: A position statement based on the EASL Special Conference 2013. J. Hepatol. 2014, 60, 1310–1324. [Google Scholar] [CrossRef]
- Villanueva, C.; Albillos, A.; Genescà, J.; Garcia-Pagan, J.C.; Calleja, J.L.; Aracil, C.; Bañares, R.; Morillas, R.M.; Poca, M.; Peñas, B.; et al. β blockers to prevent decompensation of cirrhosis in patients with clinically significant portal hypertension (PREDESCI): A randomised, double-blind, placebo-controlled, multicentre trial. Lancet 2019, 393, 1597–1608. [Google Scholar] [CrossRef]
- Raines, D.L.; Dupont, A.W.; Arguedas, M.R. Cost-effectiveness of hepatic venous pressure gradient measurements for prophylaxis of variceal re-bleeding. Aliment. Pharmacol. Ther. 2004, 19, 571–581. [Google Scholar] [CrossRef]
- Mandorfer, M.; Hernández-Gea, V.; Reiberger, T.; García-Pagán, J.C. Hepatic Venous Pressure Gradient Response in Non-Selective Beta-Blocker Treatment—Is It Worth Measuring? Curr. Hepatol. Rep. 2019, 18, 174–186. [Google Scholar] [CrossRef]
- Paternostro, R.; Becker, J.; Hofer, B.S.; Panagl, V.; Schiffke, H.; Simbrunner, B.; Semmler, G.; Schwabl, P.; Scheiner, B.; Bucsics, T.; et al. The prognostic value of HVPG-response to non-selective beta-blockers in patients with NASH cirrhosis and varices. Dig. Liver Dis. 2022, 54, 500–508. [Google Scholar] [CrossRef] [PubMed]
- Baffy, G.; Bosch, J. Overlooked subclinical portal hypertension in non-cirrhotic NAFLD: Is it real and how to measure it? J. Hepatol. 2022, 76, 458–463. [Google Scholar] [CrossRef] [PubMed]
- Miao, L.; Targher, G.; Byrne, C.D.; Valenti, L.; Qi, X.; Zheng, M. Portal hypertension in nonalcoholic fatty liver disease: Challenges and perspectives. Portal Hypertens. Cirrhosis 2022, 1, 57–65. [Google Scholar] [CrossRef]
- Bochnakova, T. Hepatic venous pressure gradient. Clin. Liver Dis. 2021, 17, 144. [Google Scholar] [CrossRef]
| Parameters | Overall Cohort (n = 145) | Esophageal AVB (n = 103) | Gastric AVB (n = 42) | p Value |
|---|---|---|---|---|
| Age (years) | 44 (37–52) | 43 (37–49) | 50 (38–56) | 0.033 |
| Sex (Male) | 128 (88.3%) | 94 (91.3%) | 34 (81%) | 0.080 |
| Etiology | 0.935 | |||
| Alcohol | 67 (46.2%) | 49 (47.6%) | 18 (42.9%) | |
| Hepatitis B virus | 24 (16.6%) | 17 (16.6%) | 7 (16.7%) | |
| Hepatitis C virus | 13 (9%) | 10 (9.7%) | 3 (7.1%) | |
| Autoimmune hepatitis | 3 (2.1%) | 2 (1.9%) | 1 (2.4%) | |
| NAFLD | 15 (10.3%) | 9 (8.7%) | 6 (14.3%) | |
| Cryptogenic/Others | 23 (15.9%) | 16 (15.5%) | 7 (16.7%) | |
| Hemoglobin (g/dL) | 7.9 ± 2.7 | 7.5 ± 2.6 | 8.9 ± 2.8 | 0.004 |
| Platelets (×103/mm3) | 89 (59–120) | 83 (57–120) | 92 (62–135) | 0.283 |
| Creatinine (mg/dL) | 0.8 (0.7–1.1) | 0.8 (0.7–1.0) | 1 (0.7–1.3) | 0.082 |
| Total bilirubin (mg/dL) | 1.7 (1–2.7) | 1.8 (1.0–2.8) | 1.5 (0.9–2.5) | 0.495 |
| INR | 1.6 ± 0.5 | 1.6 ± 0.4 | 1.7 ± 0.6 | 0.357 |
| Albumin (g/dL) | 2.9 ± 0.7 | 2.9 ± 0.6 | 3 ± 0.8 | 0.226 |
| Sodium (meq/L) | 136.9 ± 4.3 | 136.3 ± 4.1 | 138.3 ± 4.4 | 0.007 |
| CTP Score | 7 (6–9) | 8 (6–9) | 7 (7–9) | 0.769 |
| Child Class | 0.289 | |||
| Child A | 36 (24.8%) | 29 (28.2%) | 7 (16.7%) | |
| Child B | 90 (62.1%) | 60 (58.2%) | 30 (71.4%) | |
| Child C | 19 (13.1%) | 14 (13.6%) | 5 (11.9%) | |
| MELD Score | 14 (11.0–17.0) | 13 (11.0–16) | 15 (11–20) | 0.130 |
| Diabetes | 27 (18.6%) | 20 (19.4%) | 7 (16.7%) | 0.700 |
| Ascites | 69 (47.6%) | 49 (47.6%) | 20 (47.6%) | 0.996 |
| Hepatic Encephalopathy | 3 (2.1%) | 0 | 3 (7.1%) | 0.006 |
| HVPG (mmHg) | 16 (13–19) | 16 (14–19) | 13 (11–16) | <0.001 |
| Median duration of follow up, days | 296 (92–410) | 271 (77–406) | 349 (196–431) | 0.263 |
| Death | 17 (11.7%) | 8 (7.8%) | 9 (21.4%) | 0.042 |
| Parameters | Whole Cohort (n = 145) | Esophageal AVB (n = 103) | Esophageal AVB HVPG < 16 mmHg (n = 41) | Esophageal AVB HVPG ≥ 16 mmHg (n = 62) | p Value * | Gastric Variceal Bleeding (n = 42) | p-Value ** |
|---|---|---|---|---|---|---|---|
| Any further decompensation | 40 (27.6%) | 30 (29.1%) | 6 (14.6%) | 24 (38.7%) | 0.008 | 10 (23.8%) | 0.516 |
| Median duration (days) | 213 (73–365) | 187 (83–305) | 152 (99–444) | 194 (76–296) | 0.815 | 285 (100–381) | 0.212 |
| Types of further decompensation | |||||||
| New onset Ascites/Worsening | 20 (13.8%) | 16 (15.5%) | 3 (7.3%) | 13 (21%) | 0.061 | 4 (9.5%) | 0.341 |
| GI Bleed | 27 (18.6%) | 18 (17.5%) | 3 (7.3%) | 15 (24.2%) | 0.027 | 9 (21.4%) | 0.640 |
| Hepatic encephalopathy | 6 (4.1%) | 5 (4.9%) | 1 (2.4%) | 4 (6.5%) | 0.646 | 1 (2.4%) | 0.673 |
| Jaundice | 7 (4.8%) | 5 (4.9%) | 2 (4.9%) | 3 (4.8%) | 1.000 | 2 (4.8%) | 1.000 |
| Death | 7 (4.8%) | 5 (4.9%) | 1 (2.4%) | 4 (6.5%) | 0.646 | 2 (4.8%) | 1.000 |
| Univariate Model | Multivariate Model-1 | Multivariate Model-2 (Includes MELD) | Multivariate Model-3 (Includes CTP Score) | |||||
|---|---|---|---|---|---|---|---|---|
| Parameters | HR | p | HR | p | HR | p | HR | p |
| Age (years) | 0.987 (0.949–1.026) | 0.503 | ||||||
| Sex (Female) | 1.285 (0.385–4.284) | 0.683 | ||||||
| Hemoglobin (g/dL) | 0.916 (0.779–1.079) | 0.294 | ||||||
| Platelets (×103/mm3) | 0.999 (0.992–1.006) | 0.813 | ||||||
| Creatinine (mg/dL) | 3.005 (1.029–8.778) | 0.044 | 2.220 (0.692–7.121) | 0.180 | 3.471 (1.144–10.531) | 0.028 | ||
| INR | 3.994 (2.149–7.420) | <0.001 | 1.875 (0.773–4.546) | 0.164 | ||||
| Bilirubin (mg/dL) | 1.180 (1.043–1.334) | 0.009 | 1.076 (0.899–1.287) | 0.424 | ||||
| Albumin (g/dL) | 0.294 (0.143–0.607) | <0.001 | 0.436 (0.192–0.987) | 0.046 | 0.485 (0.209–1.128) | 0.093 | ||
| Sodium (mEq/L) | 0.937 (0.856–1.063) | 0.395 | ||||||
| CTP Score | 1.700 (1.341–2.154) | <0.001 | 1.631 (1.279–2.082) | <0.001 | ||||
| MELD score | 1.191 (1.114–1.1273) | <0.001 | 1.152 (1.071–1.239) | <0.001 | ||||
| Ascites | 1.602 (0.772–3.324) | 0.206 | ||||||
| Diabetes | 1.115 (0.449–2.767) | 0.815 | ||||||
| HVPG (mm Hg) | 1.136 (1.066–1.209) | <0.001 | 1.109 (1.036–1.187) | 0.003 | 1.111 (1.038–1.189) | 0.002 | 1.115 (1.044–1.189) | 0.001 |
| Esophageal AVB (n = 103) | p Value | ||
|---|---|---|---|
| HVPG < 16 mmHg (n = 41) | HVPG ≥ 16 mmHg (n = 62) | ||
| Age (years) | 41 (36–48) | 44 (37–50) | 0.566 |
| Sex (Male) | 38 (92.7%) | 56 (90.3%) | 0.678 |
| Etiology | 0.247 | ||
| Alcohol | 16 (39%) | 33 (53.2%) | |
| Hepatitis B virus | 9 (22%) | 8 (12.9%) | |
| Hepatitis C virus | 3 (7.3%) | 7 (11.3%) | |
| Autoimmune hepatitis | 2 (4.9%) | 0 (0%) | |
| NAFLD | 5 (12.2%) | 4 (6.5%) | |
| Cryptogenic | 6 (14.6%) | 10 (16.1%) | |
| Hemoglobin (g/dL) | 7.8 ± 2.7 | 7.3 ± 2.5 | 0.362 |
| Platelets (×103/mm3) | 77 (48–111) | 90 (60–128) | 0.263 |
| Creatinine (mg/dL) | 0.8 (0.7–1.0) | 0.8 (0.6–1.1) | 0.867 |
| Total Bilirubin (mg/dL) | 1.6 (1.0–2.9) | 2.0 (1.0–2.8) | 0.381 |
| INR | 1.5 ± 0.3 | 1.6 ± 0.5 | 0.171 |
| Albumin (g/dL) | 3.2 ± 0.7 | 2.7 ± 0.5 | <0.001 |
| Sodium (mEq/L) | 137.1 ± 3.5 | 135.7 ± 4.3 | 0.085 |
| CTP Score | 7 (6–8) | 8 (7–9) | 0.036 |
| MELD Score | 12.7 (9.0–16.2) | 14.3 (11.5–16.5) | 0.119 |
| Diabetes mellitus | 7 (17.1%) | 13 (21.0%) | 0.800 |
| Baseline Ascites | 19 (46.3%) | 30 (48.4%) | 0.839 |
| Baseline Hepatic Encephalopathy | 0 | 0 | NA |
| Duration of follow up, days | 296 (130–458) | 248 (66–379) | 0.172 |
| Parameters | Esophageal AVB HVPG < 20 mm Hg (n = 79) | Esophageal AVB HVPG ≥ 20 mm Hg (n = 24) | p Value |
|---|---|---|---|
| Any further decompensation | 19 (24.1%) | 11 (45.8%) | 0.040 |
| Type of further decompensation | |||
| Ascites (new or worsening) | 9 (11.4%) | 7 (29.2%) | 0.052 |
| GI Bleed | 12 (15.2%) | 6 (25%) | 0.356 |
| HE | 2 (2.5%) | 3 (12.5%) | 0.081 |
| Jaundice | 5 (6.3%) | 0 | 0.588 |
| Death | 2 (2.5%) | 3 (12.5%) | 0.081 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vaishnav, M.; Biswas, S.; Anand, A.; Pathak, P.; Swaroop, S.; Aggarwal, A.; Arora, U.; Elhence, A.; Gamanagatti, S.; Goel, A.; et al. Hepatic Venous Pressure Gradient Predicts Further Decompensation in Cirrhosis Patients with Acute Esophageal Variceal Bleeding. Diagnostics 2023, 13, 2385. https://doi.org/10.3390/diagnostics13142385
Vaishnav M, Biswas S, Anand A, Pathak P, Swaroop S, Aggarwal A, Arora U, Elhence A, Gamanagatti S, Goel A, et al. Hepatic Venous Pressure Gradient Predicts Further Decompensation in Cirrhosis Patients with Acute Esophageal Variceal Bleeding. Diagnostics. 2023; 13(14):2385. https://doi.org/10.3390/diagnostics13142385
Chicago/Turabian StyleVaishnav, Manas, Sagnik Biswas, Abhinav Anand, Piyush Pathak, Shekhar Swaroop, Arnav Aggarwal, Umang Arora, Anshuman Elhence, Shivanand Gamanagatti, Amit Goel, and et al. 2023. "Hepatic Venous Pressure Gradient Predicts Further Decompensation in Cirrhosis Patients with Acute Esophageal Variceal Bleeding" Diagnostics 13, no. 14: 2385. https://doi.org/10.3390/diagnostics13142385
APA StyleVaishnav, M., Biswas, S., Anand, A., Pathak, P., Swaroop, S., Aggarwal, A., Arora, U., Elhence, A., Gamanagatti, S., Goel, A., Kumar, R., & Shalimar. (2023). Hepatic Venous Pressure Gradient Predicts Further Decompensation in Cirrhosis Patients with Acute Esophageal Variceal Bleeding. Diagnostics, 13(14), 2385. https://doi.org/10.3390/diagnostics13142385







