Assessment of the Tumor–Stroma Ratio and Tumor-Infiltrating Lymphocytes in Colorectal Cancer: Inter-Observer Agreement Evaluation
Abstract
1. Introduction
2. Material and Methods
2.1. Patients
2.2. Tumor–Stroma Ratio Estimation
2.3. Statistical Analysis
3. Results
3.1. Intratumoral Stromal TILs
3.2. TILs in the Tumor Front
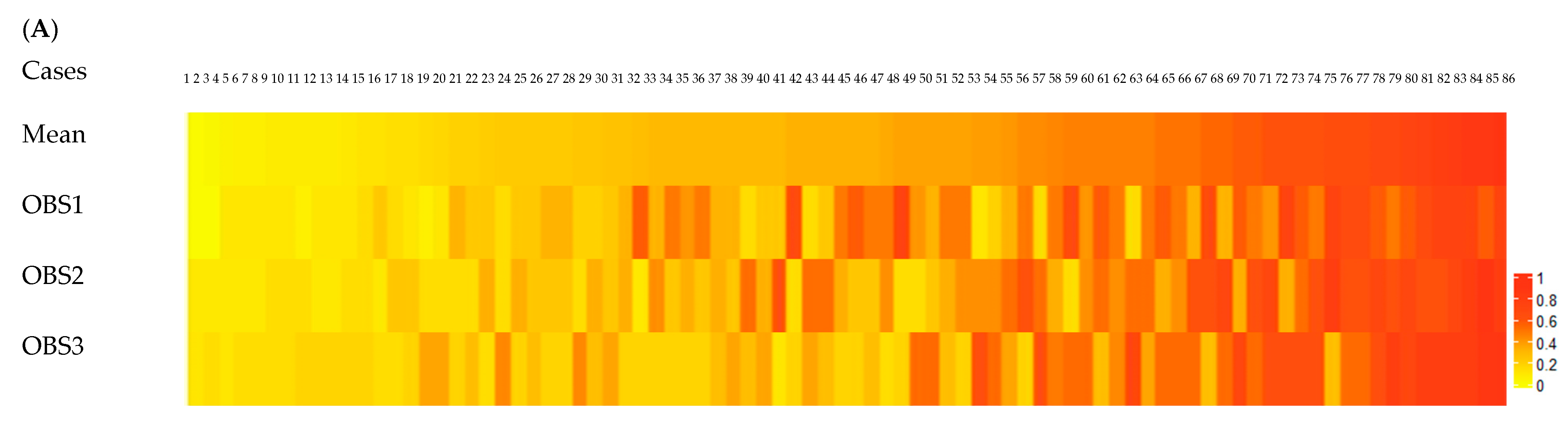
3.3. Tumor–Stroma Ratio
3.4. Correlation between Scored Biomarkers and Patient Data
4. Discussion
4.1. Intratumoral Stromal TILs
4.2. TILs in the Tumor Front
4.3. Tumor–Stroma Ratio
4.4. Correlation between Scored Biomarkers and Patient Data
4.5. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bychkov, D.; Linder, N.; Turkki, R.; Nordling, S.; Kovanen, P.E.; Verrill, C.; Walliander, M.; Lundin, M.; Haglund, C.; Lundin, J. Deep learning based tissue analysis predicts outcome in colorectal cancer. Sci. Rep. 2018, 8, 3395. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.C.S.; Huang, J.; Lok, V.; Wang, J.; Fung, F.; Ding, H.; Zheng, Z.J. Differences in Incidence and Mortality Trends of Colorectal Cancer Worldwide Based on Sex, Age, and Anatomic Location. Clin. Gastroenterol. Hepatol. 2021, 19, 955–966. [Google Scholar] [CrossRef]
- Cardoso, R.; Guo, F.; Heisser, T.; Hackl, M.; Ihle, P.; De Schutter, H.; Van Damme, N.; Valerianova, Z.; Atanasov, T.; Majek, O.; et al. Colorectal cancer incidence, mortality, and stage distribution in European countries in the colorectal cancer screening era: An international population-based study. Lancet Oncol. 2021, 22, 1002–1013. [Google Scholar] [CrossRef] [PubMed]
- Favoriti, P.; Carbone, G.; Greco, M.; Pirozzi, F.; Pirozzi, R.E.; Corcione, F. Worldwide burden of colorectal cancer: A review. Updates Surg. 2016, 68, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Denkert, C.; von Minckwitz, G.; Darb-Esfahani, S.; Lederer, B.; Heppner, B.I.; Weber, K.E.; Budczies, J.; Huober, J.; Klauschen, F.; Furlanetto, J.; et al. Tumour-infiltrating lymphocytes and prognosis in different subtypes of breast cancer: A pooled analysis of 3771 patients treated with neoadjuvant therapy. Lancet Oncol. 2018, 19, 40–50. [Google Scholar] [CrossRef] [PubMed]
- Maibach, F.; Sadozai, H.; Seyed Jafari, S.M.; Hunger, R.E.; Schenk, M. Tumor-Infiltrating Lymphocytes and Their Prognostic Value in Cutaneous Melanoma. Front. Immunol. 2020, 11, 2105. [Google Scholar] [CrossRef]
- Paijens, S.T.; Vledder, A.; de Bruyn, M.; Nijman, H.W. Tumor-infiltrating lymphocytes in the immunotherapy era. Cell Mol. Immunol. 2021, 18, 842–859. [Google Scholar] [CrossRef]
- Zakhartseva, L.M.; Yanovytska, M.A. Prognostic Value of Tumor Stroma Ratio in Triple Negative Breast Cancer. Wiad. Lek. 2021, 74, 565–571. [Google Scholar] [CrossRef]
- Kang, J.; Su, M.; Xu, Q.; Wang, C.; Yuan, X.; Han, Z. Tumour-stroma ratio is a valuable prognostic factor for oral tongue squamous cell carcinoma. Oral. Dis. 2023, 29, 628–638. [Google Scholar] [CrossRef]
- Galon, J.; Mlecnik, B.; Bindea, G.; Angell, H.K.; Berger, A.; Lagorce, C.; Lugli, A.; Zlobec, I.; Hartmann, A.; Bifulco, C.; et al. Towards the introduction of the 'Immunoscore' in the classification of malignant tumours. J. Pathol. 2014, 232, 199–209. [Google Scholar] [CrossRef]
- Francini, E.; Ou, F.S.; Lazzi, S.; Petrioli, R.; Multari, A.G.; Pesola, G.; Messuti, L.; Colombo, E.; Livellara, V.; Bazzurri, S.; et al. The prognostic value of CD3+ tumor-infiltrating lymphocytes for stage II colon cancer according to use of adjuvant chemotherapy: A large single-institution cohort study. Transl. Oncol. 2021, 14, 100973. [Google Scholar] [CrossRef]
- Eriksen, A.C.; Sorensen, F.B.; Lindebjerg, J.; Hager, H.; dePont Christensen, R.; Kjaer-Frifeldt, S.; Hansen, T.F. The Prognostic Value of Tumor-Infiltrating lymphocytes in Stage II Colon Cancer. A Nationwide Population-Based Study. Transl. Oncol. 2018, 11, 979–987. [Google Scholar] [CrossRef] [PubMed]
- Ye, L.; Zhang, T.; Kang, Z.; Guo, G.; Sun, Y.; Lin, K.; Huang, Q.; Shi, X.; Ni, Z.; Ding, N.; et al. Tumor-Infiltrating Immune Cells Act as a Marker for Prognosis in Colorectal Cancer. Front. Immunol. 2019, 10, 2368. [Google Scholar] [CrossRef] [PubMed]
- Salgado, R.; Denkert, C.; Demaria, S.; Sirtaine, N.; Klauschen, F.; Pruneri, G.; Wienert, S.; Van den Eynden, G.; Baehner, F.L.; Penault-Llorca, F.; et al. The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: Recommendations by an International TILs Working Group 2014. Ann. Oncol. 2015, 26, 259–271. [Google Scholar] [CrossRef] [PubMed]
- Van Bockstal, M.R.; Francois, A.; Altinay, S.; Arnould, L.; Balkenhol, M.; Broeckx, G.; Burgues, O.; Colpaert, C.; Dedeurwaerdere, F.; Dessauvagie, B.; et al. Interobserver variability in the assessment of stromal tumor-infiltrating lymphocytes (sTILs) in triple-negative invasive breast carcinoma influences the association with pathological complete response: The IVITA study. Mod. Pathol. 2021, 34, 2130–2140. [Google Scholar] [CrossRef] [PubMed]
- Hendry, S.; Salgado, R.; Gevaert, T.; Russell, P.A.; John, T.; Thapa, B.; Christie, M.; Van De Vijver, K.; Estrada, M.V.; Gonzalez-Ericsson, P.I. Assessing tumor infiltrating lymphocytes in solid tumors: A practical review for pathologists and proposal for a standardized method from the International Immuno-Oncology Biomarkers Working Group: Part 1: Assessing the host immune response, TILs in invasive breast carcinoma and ductal carcinoma in situ, metastatic tumor deposits and areas for further research. Adv. Anat. Pathol. 2017, 24, 235. [Google Scholar]
- Iseki, Y.; Shibutani, M.; Maeda, K.; Nagahara, H.; Fukuoka, T.; Matsutani, S.; Kashiwagi, S.; Tanaka, H.; Hirakawa, K.; Ohira, M. A new method for evaluating tumor-infiltrating lymphocytes (TILs) in colorectal cancer using hematoxylin and eosin (H-E)-stained tumor sections. PLoS ONE 2018, 13, e0192744. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, T.L.; Sioson, L.; Sheen, A.; Jafari-Nejad, K.; Renaud, C.J.; Andrici, J.; Ahadi, M.; Chou, A.; Gill, A.J. Assessment of Tumor-infiltrating Lymphocytes Using International TILs Working Group (ITWG) System Is a Strong Predictor of Overall Survival in Colorectal Carcinoma: A Study of 1034 Patients. Am. J. Surg. Pathol. 2020, 44, 536–544. [Google Scholar] [CrossRef]
- Tramm, T.; Di Caterino, T.; Jylling, A.B.; Lelkaitis, G.; Laenkholm, A.V.; Rago, P.; Tabor, T.P.; Talman, M.M.; Vouza, E.; Scientific Committee of Pathology, D.B.C.G. Standardized assessment of tumor-infiltrating lymphocytes in breast cancer: An evaluation of inter-observer agreement between pathologists. Acta Oncol. 2018, 57, 90–94. [Google Scholar] [CrossRef]
- Sari, C.T.; Gunduz-Demir, C. Unsupervised Feature Extraction via Deep Learning for Histopathological Classification of Colon Tissue Images. IEEE Trans. Med. Imaging 2019, 38, 1139–1149. [Google Scholar] [CrossRef]
- Ao, T.; Kajiwara, Y.; Yonemura, K.; Shinto, E.; Mochizuki, S.; Okamoto, K.; Kishi, Y.; Ueno, H. Morphological consistency of desmoplastic reactions between the primary colorectal cancer lesion and associated metastatic lesions. Virchows Arch. 2020, 477, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Jin, Z.; Qian, Y.; Shen, Y.; Wang, Z. Prognostic Value of Tumor-Stroma Ratio in Rectal Cancer: A Systematic Review and Meta-analysis. Front. Oncol. 2021, 11, 685570. [Google Scholar] [CrossRef] [PubMed]
- Souza da Silva, R.M.; Queiroga, E.M.; Paz, A.R.; Neves, F.F.P.; Cunha, K.S.; Dias, E.P. Standardized Assessment of the Tumor-Stroma Ratio in Colorectal Cancer: Interobserver Validation and Reproducibility of a Potential Prognostic Factor. Clin. Pathol. 2021, 14, 2632010X21989686. [Google Scholar] [CrossRef]
- Bani, N.; Moetamani-Ahmadi, M.; Alidoust, M.; ShahidSales, S.; Khazaei, M.; Esmaily, H.; Joudi-Mashhad, M.; Ferns, G.A.; Gharib, M.; Avan, A. Association between the 308 G>A variant of the TNF-α gene and risk of colorectal cancer. Meta Gene 2021, 28, 100878. [Google Scholar] [CrossRef]
- Sullivan, L.; Pacheco, R.R.; Kmeid, M.; Chen, A.; Lee, H. Tumor Stroma Ratio and Its Significance in Locally Advanced Colorectal Cancer. Curr. Oncol. 2022, 29, 3232–3241. [Google Scholar] [CrossRef]
- Gisev, N.; Bell, J.S.; Chen, T.F. Interrater agreement and interrater reliability: Key concepts, approaches, and applications. Res. Social. Adm. Pharm. 2013, 9, 330–338. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Denkert, C.; Wienert, S.; Poterie, A.; Loibl, S.; Budczies, J.; Badve, S.; Bago-Horvath, Z.; Bane, A.; Bedri, S.; Brock, J.; et al. Standardized evaluation of tumor-infiltrating lymphocytes in breast cancer: Results of the ring studies of the international immuno-oncology biomarker working group. Mod. Pathol. 2016, 29, 1155–1164. [Google Scholar] [CrossRef]
- Swisher, S.K.; Wu, Y.; Castaneda, C.A.; Lyons, G.R.; Yang, F.; Tapia, C.; Wang, X.; Casavilca, S.A.; Bassett, R.; Castillo, M.; et al. Interobserver Agreement Between Pathologists Assessing Tumor-Infiltrating Lymphocytes (TILs) in Breast Cancer Using Methodology Proposed by the International TILs Working Group. Ann. Surg. Oncol. 2016, 23, 2242–2248. [Google Scholar] [CrossRef]
- Dang, H.A.-O.; van Pelt, G.W.; Haasnoot, K.J.; Backes, Y.; Elias, S.G.; Seerden, T.C.; Schwartz, M.P.; Spanier, B.W.; de Vos Tot Nederveen Cappel, W.H.; van Bergeijk, J.D.; et al. Tumour-stroma ratio has poor prognostic value in non-pedunculated T1 colorectal cancer: A multi-centre case-cohort study. United Eur. Gastroenterol. J. 2021, 9, 478–485. [Google Scholar] [CrossRef] [PubMed]





| Intraclass coefficient (ICC) | 0.51 (CI *: 0.35–0.64) |
| Fleiss’ kappa values (p-value) | |
| System 1 (<10%, 10–50%, >50%) | 0.32 (<0.001) |
| System 2 (<10%, 11–39%, ≥40%) | 0.21 (<0.001) |
| System 3 (≤20%, 21–49%, ≥50%) | 0.27 (<0.001) |
| System 4 (<42%, ≥42%) | 0.38 (<0.001) |
| Concordance rates | |
| System 1 | 0.70 (range: 0.63–0.77) |
| System 2 | 0.61 (range: 0.56–0.71) |
| System 3 | 0.62 (range: 0.60–0.69) |
| System 4 | 0.72 (range: 0.69–0.78) |
| Spearman Correlation (rho) | |||
|---|---|---|---|
| Pathologists | Intra-Tumoral Stromal TILs Estimation | Tumor Front Stromal TILs Estimation | TSR Estimation |
| OBS1-OBS2 * | 0.55 | 0.54 | 0.56 |
| OBS1-OBS3 | 0.48 | 0.60 | 0.36 |
| OBS2-OBS3 | 0.64 | 0.66 | 0.39 |
| Intraclass coefficient (ICC) | 0.52 (CI *: 0.32–0.67) |
| Fleiss’ kappa values (p-value) | |
| System 1 (<10%, 10–50%, >50%) | 0.26 (<0.001) |
| System 2 (<10%, 11–39%, ≥40%) | 0.24 (<0.001) |
| System 3 (≤20%, 21–49%, ≥50%) | 0.29 (<0.001) |
| System 4 (<42%, ≥42%) | 0.30 (<0.001) |
| Concordance rates | |
| System 1 | 0.71 (range: 0.53–0.77) |
| System 2 | 0.68 (range: 0.58–0.7) |
| System 3 | 0.66 (range: 0.58–0.67) |
| System 4 | 0.72 (range: 0.63–0.76) |
| Intraclass coefficient (ICC) | 0.48 (CI *: 0.35–0.60) |
| Fleiss’ kappa values (p-value) | |
| ≤50%, >50% | 0.49 (<0.001) |
| Concordance rates | |
| ≤50%, >50% | 0.76 (range: 0.72–0.78) |
| Variable | Intratumoral TILs | TILs in Tumor Front | TSR |
|---|---|---|---|
| Sex | −0.06 (CI *: −0.27–0.16) p # = 0.61 | −0.08 (CI: −0.29–0.14) p = 0.47 | 0.03 (CI: −0.19–0.24) p = 0.82 |
| Age | 0.07 (CI: −0.15–0.28) p = 0.54 | 0.21 (CI: −0.01–0.40); p = 0.06 | 0.14 (CI: −0.08–0.34) p = 0.21 |
| Grade | 0.05 (CI: −0.22–0.30) p = 0.74 | 0.08 (CI: −0.19–0.33); p = 0.57 | 0.29 (CI: 0.03–0.51) p = 0.03 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kazemi, A.; Gharib, M.; Mohamadian Roshan, N.; Taraz Jamshidi, S.; Stögbauer, F.; Eslami, S.; Schüffler, P.J. Assessment of the Tumor–Stroma Ratio and Tumor-Infiltrating Lymphocytes in Colorectal Cancer: Inter-Observer Agreement Evaluation. Diagnostics 2023, 13, 2339. https://doi.org/10.3390/diagnostics13142339
Kazemi A, Gharib M, Mohamadian Roshan N, Taraz Jamshidi S, Stögbauer F, Eslami S, Schüffler PJ. Assessment of the Tumor–Stroma Ratio and Tumor-Infiltrating Lymphocytes in Colorectal Cancer: Inter-Observer Agreement Evaluation. Diagnostics. 2023; 13(14):2339. https://doi.org/10.3390/diagnostics13142339
Chicago/Turabian StyleKazemi, Azar, Masoumeh Gharib, Nema Mohamadian Roshan, Shirin Taraz Jamshidi, Fabian Stögbauer, Saeid Eslami, and Peter J. Schüffler. 2023. "Assessment of the Tumor–Stroma Ratio and Tumor-Infiltrating Lymphocytes in Colorectal Cancer: Inter-Observer Agreement Evaluation" Diagnostics 13, no. 14: 2339. https://doi.org/10.3390/diagnostics13142339
APA StyleKazemi, A., Gharib, M., Mohamadian Roshan, N., Taraz Jamshidi, S., Stögbauer, F., Eslami, S., & Schüffler, P. J. (2023). Assessment of the Tumor–Stroma Ratio and Tumor-Infiltrating Lymphocytes in Colorectal Cancer: Inter-Observer Agreement Evaluation. Diagnostics, 13(14), 2339. https://doi.org/10.3390/diagnostics13142339






