Postoperative 30-Day Comparative Complications of Multilevel Anterior Cervical Discectomy and Fusion and Laminoplasty for Cervical Spondylotic Myelopathy: An Evidence in Reaching Consensus
Abstract
1. Introduction
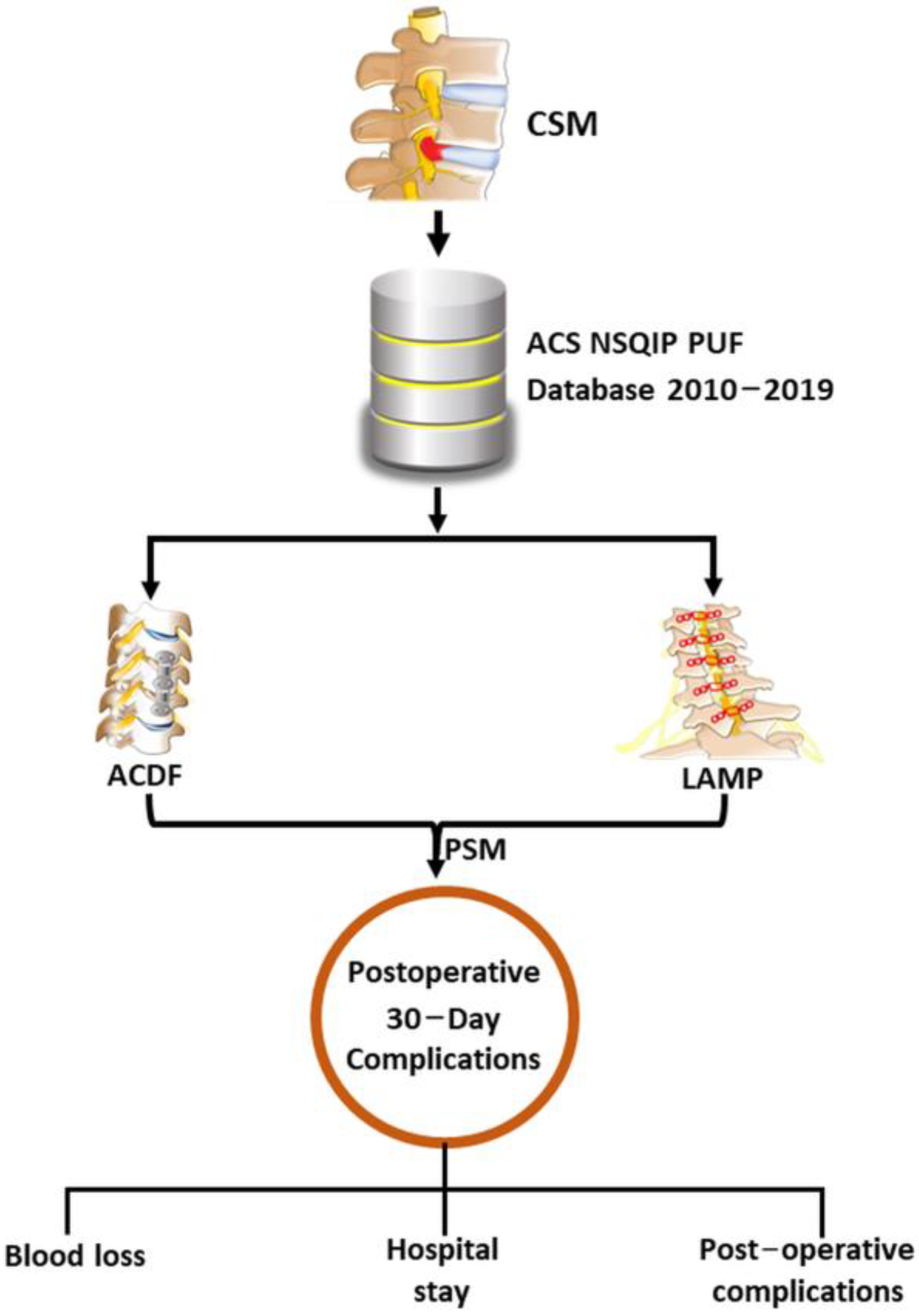
2. Materials and Methods
2.1. Database and Patient Selection
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Young, W.F. Cervical spondylotic myelopathy: A common cause of spinal cord dysfunction in older persons. Am. Fam. Physician 2000, 62, 1064–1070. [Google Scholar]
- Hartig, D.; Batke, J.; Dea, N.; Kelly, A.; Fisher, C.; Street, J. Adverse events in surgically treated cervical spondylopathic myelopathy: A prospective validated observational study. Spine 2015, 40, 292–298. [Google Scholar] [CrossRef]
- Hirai, T.; Yoshii, T.; Arai, Y.; Sakai, K.; Torigoe, I.; Maehara, H.; Tomori, M.; Taniyama, T.; Sato, H.; Okawa, A. A Comparative Study of Anterior Decompression with Fusion and Posterior Decompression with Laminoplasty for the Treatment of Cervical Spondylotic Myelopathy Patients with Large Anterior Compression of the Spinal Cord. Clin. Spine Surg. 2017, 30, E1137–E1142. [Google Scholar] [CrossRef]
- Yoshii, T.; Egawa, S.; Chikuda, H.; Wakao, N.; Furuya, T.; Kanchiku, T.; Nagoshi, N.; Fujiwara, Y.; Yoshida, M.; Taguchi, T.; et al. A systematic review and meta-analysis comparing anterior decompression with fusion and posterior laminoplasty for cervical spondylotic myelopathy. J. Orthop. Sci. 2021, 26, 116–122. [Google Scholar] [CrossRef]
- Lee, J.J.; Lee, N.; Oh, S.H.; Shin, D.A.; Yi, S.; Kim, K.N.; Yoon, D.H.; Shin, H.C.; Ha, Y. Clinical and radiological outcomes of multilevel cervical laminoplasty versus three-level anterior cervical discectomy and fusion in patients with cervical spondylotic myelopathy. Quant. Imaging Med. Surg. 2020, 10, 2112–2124. [Google Scholar] [CrossRef] [PubMed]
- Morishita, S.; Yoshii, T.; Okawa, A.; Fushimi, K.; Fujiwara, T. Comparison of Perioperative Complications Between Anterior Decompression with Fusion and Laminoplasty For Cervical Spondylotic Myelopathy: Propensity Score-matching Analysis Using Japanese Diagnosis Procedure Combination Database. Clin. Spine Surg. 2020, 33, E101–E107. [Google Scholar] [CrossRef]
- Chen, Q.; Qin, M.; Chen, F.; Ni, B.; Guo, Q.; Han, Z. Comparison of Outcomes Between Anterior Cervical Decompression and Fusion and Posterior Laminoplasty in the Treatment of 4-Level Cervical Spondylotic Myelopathy. World Neurosurg. 2019, 125, e341–e347. [Google Scholar] [CrossRef] [PubMed]
- Hirai, T.; Yoshii, T.; Sakai, K.; Inose, H.; Yamada, T.; Kato, T.; Kawabata, S.; Arai, Y.; Shinomiya, K.; Okawa, A. Long-term results of a prospective study of anterior decompression with fusion and posterior decompression with laminoplasty for treatment of cervical spondylotic myelopathy. J. Orthop. Sci. 2018, 23, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Yang, H.L.; Xu, Y.Z.; Qi, R.F.; Guan, H.Q. ACDF with the PCB cage-plate system versus laminoplasty for multilevel cervical spondylotic myelopathy. J. Spinal Disord. Tech. 2011, 24, 213–220. [Google Scholar] [CrossRef]
- Xu, L.; Sun, H.; Li, Z.; Liu, X.; Xu, G. Anterior cervical discectomy and fusion versus posterior laminoplasty for multilevel cervical myelopathy: A meta-analysis. Int. J. Surg. 2017, 48, 247–253. [Google Scholar] [CrossRef]
- Zhang, Y.; Yang, G.; Zhou, T.; Chen, Y.; Gao, Z.; Zhou, W.; Gu, Y. Efficacy and safety of anterior cervical discectomy and fusion (ACDF) through mini-incision and posterior laminoplasty (LAMP) for treatment of long-level cervical spondylosis: A retrospective cohort study. BMC Surg. 2022, 22, 115. [Google Scholar] [CrossRef] [PubMed]
- Davenport, D.L.; Holsapple, C.W.; Conigliaro, J. Assessing surgical quality using administrative and clinical data sets: A direct comparison of the University HealthSystem Consortium Clinical Database and the National Surgical Quality Improvement Program data set. Am. J. Med. Qual. 2009, 24, 395–402. [Google Scholar] [CrossRef]
- Wang, B.; Lü, G.; Kuang, L. Anterior cervical discectomy and fusion with stand-alone anchored cages versus posterior laminectomy and fusion for four-level cervical spondylotic myelopathy: A retrospective study with 2-year follow-up. BMC Musculoskelet. Disord. 2018, 19, 216. [Google Scholar] [CrossRef]
- Mitsunaga, L.K.; Klineberg, E.O.; Gupta, M.C. Laminoplasty techniques for the treatment of multilevel cervical stenosis. Adv. Orthop. 2012, 2012, 307916. [Google Scholar] [CrossRef] [PubMed]
- Montano, N.; Ricciardi, L.; Olivi, A. Comparison of Anterior Cervical Decompression and Fusion versus Laminoplasty in the Treatment of Multilevel Cervical Spondylotic Myelopathy: A Meta-Analysis of Clinical and Radiological Outcomes. World Neurosurg. 2019, 130, 530–536.e532. [Google Scholar] [CrossRef]
- Ghazwan, H.; Oscar, L.A. Dysphagia Following Anterior Cervical Spine Surgery. In Dysphagia; Monjur, A., Ed.; IntechOpen: Rijeka, Croatia, 2022; p. 4. [Google Scholar]
- Riester, M.; Taylor, J.M.; Feifer, A.; Koppie, T.; Rosenberg, J.E.; Downey, R.J.; Bochner, B.H.; Michor, F. Combination of a novel gene expression signature with a clinical nomogram improves the prediction of survival in high-risk bladder cancer. Clin. Cancer Res. 2012, 18, 1323–1333. [Google Scholar] [CrossRef] [PubMed]
- Xu, R.; Bydon, M.; Sciubba, D.M.; Witham, T.F.; Wolinsky, J.P.; Gokaslan, Z.L.; Bydon, A. Safety and efficacy of rhBMP2 in posterior cervical spinal fusion for subaxial degenerative spine disease: Analysis of outcomes in 204 patients. Surg. Neurol. Int. 2011, 2, 109. [Google Scholar] [CrossRef]
- Ghobrial, G.M.; Harrop, J.S.; Sasso, R.C.; Tannoury, C.A.; Tannoury, T.; Smith, Z.A.; Hsu, W.K.; Arnold, P.M.; Fehlings, M.G.; Mroz, T.E.; et al. Anterior Cervical Infection: Presentation and Incidence of an Uncommon Postoperative Complication. Glob. Spine J. 2017, 7, 12S–16S. [Google Scholar] [CrossRef]
- Sebastian, A.; Huddleston, P., 3rd; Kakar, S.; Habermann, E.; Wagie, A.; Nassr, A. Risk factors for surgical site infection after posterior cervical spine surgery: An analysis of 5,441 patients from the ACS NSQIP 2005–2012. Spine J. 2016, 16, 504–509. [Google Scholar] [CrossRef]
- Cha, Y.H.; Ha, Y.C.; Ryu, H.J.; Lee, Y.K.; Park, S.H.; Lee, K.J.; Koo, K.H. Effect of heart failure on postoperative short and long-term mortality in elderly patients with hip fracture. Injury 2020, 51, 694–698. [Google Scholar] [CrossRef]
- Lerman, B.J.; Popat, R.A.; Assimes, T.L.; Heidenreich, P.A.; Wren, S.M. Association between Heart Failure and Postoperative Mortality Among Patients Undergoing Ambulatory Noncardiac Surgery. JAMA Surg. 2019, 154, 907–914. [Google Scholar] [CrossRef] [PubMed]
- Hammill, B.G.; Curtis, L.H.; Bennett-Guerrero, E.; O’Connor, C.M.; Jollis, J.G.; Schulman, K.A.; Hernandez, A.F. Impact of heart failure on patients undergoing major noncardiac surgery. Anesthesiology 2008, 108, 559–567. [Google Scholar] [CrossRef] [PubMed]
- Turrentine, F.E.; Sohn, M.W.; Jones, R.S. Congestive Heart Failure and Noncardiac Operations: Risk of Serious Morbidity, Readmission, Reoperation, and Mortality. J. Am. Coll. Surg. 2016, 222, 1220–1229. [Google Scholar] [CrossRef]
- Pradeep, A.; Rajagopalam, S.; Kolli, H.K.; Patel, N.; Venuto, R.; Lohr, J.; Nader, N.D. High volumes of intravenous fluid during cardiac surgery are associated with increased mortality. HSR Proc. Intensive Care Cardiovasc. Anesth. 2010, 2, 287–296. [Google Scholar]
- Yee, T.J.; Swong, K.; Park, P. Complications of anterior cervical spine surgery: A systematic review of the literature. J. Spine Surg. 2020, 6, 302–322. [Google Scholar] [CrossRef]
- Weinberg, D.S.; Rhee, J.M. Cervical laminoplasty: Indication, technique, complications. J. Spine Surg. 2020, 6, 290–301. [Google Scholar] [CrossRef] [PubMed]

| Before PSM | After 1:1 PSM | |||||
|---|---|---|---|---|---|---|
| Preoperative Characteristics | Multilevel ACDF (Group A) | LAMP (Group B) | p-Value | Multilevel ACDF (Group A) | Laminoplasty (Group B) | p-Value |
| n | 4236 | 661 | X | 621 | 621 | X |
| Mean age (std) | 59.00 (10.80) | 62.85 (10.93) | <0.0001 * | 60.69 (10.65) | 61.86 (10.37) | 0.0496 * |
| Gender, male (%) | 2141 (50.54) | 431 (65.20) | <0.0001 * | 302 (48.63) | 412 (66.34) | <0.0001 * |
| Mean BMI (std) | 30.51 (6.73) | 29.46 (6.46) | 0.0002 * | 30.72 (6.98) | 29.57 (6.46) | 0.0027 * |
| Diabetes mellitus with oral agents or insulin (%) | 0 = No: 3417 (80.67) | 0 = No: 520 (78.67) | 0.4830 | 0 = No: 489 (78.74) | 0 = No: 493 (79.39) | 0.9607 |
| 1 = non-insulin: 537 (12.68) | 1 = non-insulin: 93 (14.07) | 1 = non-insulin: 87 (14.01) | 1 = non-insulin: 84 (13.53) | |||
| 2 = insulin: 282 (6.66) | 2 = insulin: 48 (7.26) | 2 = insulin: 45 (7.25) | 2 = insulin: 44 (7.09) | |||
| Open wound/wound infection (%) | 13 (0.31) | 5 (0.76) | 0.0842 | 3 (0.48) | 5 (0.81) | 0.7257 |
| Steroid use for chronic condition (%) | 174 (4.11) | 29 (4.39) | 0.7373 | 20 (3.22) | 21 (3.38) | 0.8738 |
| Bleeding disorders (%) | 64 (1.51) | 12 (1.82) | 0.5557 | 10 (1.61) | 9 (1.45) | 0.8172 |
| Preop transfusion of ≥1 unit of whole/packed RBCs in 72 h prior to surgery (%) | 0 (0) | 0 (0) | X | 0 (0) | 0 (0) | X |
| Systemic sepsis (%) | 0 = none: 4226 (99.76) | 0 = none: 660 (99.85) | 1.0000 | 0 = none: 620 (99.84) | 0 = none: 620 (99.84) | 1.0000 |
| 1 = SIRS: 10 (0.24) | 1 = SIRS: 1 (0.15) | 1 = SIRS: 1 (0.16) | 1 = SIRS: 1 (0.16) | |||
| 2 = sepsis: 0 (0) | 2 = sepsis: 0 (0) | 2 = sepsis: 0 (0) | 2 = sepsis: 0 (0) | |||
| 3 = septic shock: 0 (0) | 3 = septic shock: 0 (0) | 3 = septic shock: 0 (0) | 3 = septic shock: 0 (0) | |||
| Mean preoperative WBC (std) | 7.40 (2.41) | 7.15 (2.09) | 0.0043 * | 7.34 (2.70) | 7.15 (2.12) | 0.1708 |
| Mean preoperative hematocrit (std) | 41.56 (4.22) | 41.48 (4.39) | 0.6569 | 40.79 (3.94) | 41.86 (4.06) | <0.0001 |
| Hypertension requiring medication (%) | 2368 (55.90) | 408 (61.72) | 0.0050 * | 369 (59.42) | 376 (60.55) | 0.6852 |
| CHF in 30 days before surgery (%) | 14 (0.33) | 4 (0.61) | 0.2909 | 2 (0.32) | 4 (0.64) | 0.6867 |
| Mean preoperative serum creatinine (std) | 0.94 (0.53) | 0.99 (0.58) | 0.0433 * | 0.92 (0.33) | 0.97 (0.52) | 0.0656 |
| Acute renal failure (preop) (%) | 1 (0.02) | 0 (0) | 1.0000 | 0 (0) | 0 (0) | X |
| Currently on dialysis (preop) (%) | 16 (0.38) | 4 (0.61) | 0.3349 | 1 (0.16) | 1 (0.16) | 1.0000 |
| Dyspnea (%) | 0 = no: 3949 (93.22) | 0 = no: 643 (97.28) | 0.0003 * | 0 = no: 576 (92.75) | 0 = no: 604 (97.26) | 0.0004 * |
| 1 = moderate exertion: 272 (6.42) | 1 = moderate exertion: 18 (2.72) | 1 = moderate exertion: 43 (6.92) | 1 = moderate exertion: 17 (2.74) | |||
| 2 = at rest: 15 (0.35) | 2 = at rest: 0 (0) | 2 = at rest: 2 (0.32) | 2 = at rest: 0 (0) | |||
| History of severe COPD (%) | 243 (5.74) | 33 (4.99) | 0.4404 | 43 (6.92) | 30 (4.83) | 0.1168 |
| Ventilator dependence (%) | 0 (0) | 0 (0) | X | 0 (0) | 0 (0) | X |
| Disseminated cancer (%) | 6 (0.14) | 3 (0.45) | 0.1101 | 0 (0) | 0 (0) | X |
| Current smoker within 1 year (%) | 1104 (26.06) | 147 (22.24) | 0.0361 * | 136 (21.90) | 145 (23.35) | 0.5416 |
| Wound classification (%) | 1 = clean: 4222 (99.67) | 1 = clean: 656 (99.24) | 0.2079 | 1 = clean: 620 (99.84) | 1 = clean: 616 (99.19) | 0.2176 |
| 2 = clean/contaminated: 13 (0.31) | 2 = clean/contaminated: 5 (0.76) | 2 = clean/contaminated: 1 (0.16) | 2 = clean/contaminated: 5 (0.81) | |||
| 3 = contaminated: 0 (0) | 3 = contaminated: 0 (0) | 3 = contaminated: 0 (0) | 3 = contaminated: 0 (0) | |||
| 4 = dirty/infected: 1 (0.02) | 4 = dirty/infected: 0 (0) | 4 = dirty/infected: 0 (0) | 4 = dirty/infected: 0 (0) | |||
| ASA classification (%) | 1 = no disturb: 86 (2.03) | 1 = no disturb: 7 (1.06) | 0.0852 | 1 = no disturb: 5 (0.81) | 1 = no disturb: 7 (1.13) | 0.3877 |
| 2 = mild disturb: 1890 (44.62) | 2 = mild disturb: 272 (41.15) | 2 = mild disturb: 254 (40.90) | 2 = mild disturb: 267 (43.00) | |||
| 3 = severe disturb: 2150 (50.76) | 3 = severe disturb: 365 (55.22) | 3 = severe disturb: 340 (54.75) | 3 = severe disturb: 234 (53.78) | |||
| 4 = life threat: 110 (2.60) | 4 = life threat: 17 (2.57) | 4 = life threat: 22 (3.54) | 4 = life threat: 13 (2.09) | |||
| 5 = moribund: 0 (0) | 5 = moribund: 0 (0) | 5 = moribund: 0 (0) | 5 = moribund: 0 (0) | |||
| Before PSM | After 1:1 PSM | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Postoperation Occurrence | Multilevel ACDF (Group A) | LAMP (Group B) | p-Value | B versus AOR (95% CI) | p-Value of OR | Multilevel ACDF (Group A) | LAMP (Group B) | p-Value | B versus AOR (95% CI) | p-Value of OR |
| n | 4236 | 661 | X | X | X | 621 | 621 | X | X | X |
| Mean total operation time (std) | 159.32 (68.93) | 149.96 (58.02) | 0.0002 * | 0.835 (0.724, 0.962) | 0.0128 * | 158.60 (69.40) | 149.51 (57.64) | 0.0122 * | 0.837 (0.690, 1.015) | 0.0712 |
| Superficial surgical site infection (%) | 5 (0.12) | 7 (1.06) | 0.0003 * | 9.057 (2.866, 28.621) | 0.0002 * | 0 (0) | 7 (1.13) | 0.0154 * | >999.999 (<0.001, >999.999) | 0.9531 |
| Deep incisional SSI (%) | 3 (0.07) | 6 (0.91) | 0.0003 * | 12.925 (3.225, 51.807) | 0.0003 * | 0 (0) | 6 (0.97) | 0.0309 * | >999.999 (<0.001, >999.999) | 0.9341 |
| Organ space SSI (%) | 5 (0.12) | 0 (0) | 1.0000 | <0.001 (<0.001, >999.999) | 0.9702 | 0 (0) | 0 (0) | X | X | X |
| Wound disruption (%) | 2 (0.05) | 5 (0.76) | 0.0007 * | 16.136 (3.124, 83.339) | 0.0009 * | 0 (0) | 5 (0.81) | 0.0620 | >999.999 (<0.001, >999.999) | 0.9398 |
| Pneumonia (%) | 38 (0.90) | 7 (1.06) | 0.6606 | 1.183 (0.526, 2.659) | 0.6851 | 8 (1.29) | 7 (1.13) | 0.7950 | 0.874 (0.315, 2.424) | 0.7952 |
| Unplanned intubation (%) | 34 (0.80) | 1 (0.15) | 0.0783 | 0.187 (0.026, 1.370) | 0.0990 | 7 (1.13) | 1 (0.16) | 0.0694 | 0.141 (0.017, 1.153) | 0.0677 |
| Ventilator > 48 h (%) | 26 (0.61) | 1 (0.15) | 0.1652 | 0.245 (0.033, 1.811) | 0.1683 | 5 (0.81) | 1 (0.16) | 0.2176 | 0.199 (0.023, 1.706) | 0.1407 |
| Progressive renal insufficiency (%) | 1 (0.02) | 0 (0) | 1.0000 | <0.001 (<0.001, >999.999) | 0.9702 | 0 (0) | 0 (0) | X | X | X |
| Acute renal failure (%) | 4 (0.09) | 1 (0.15) | 0.5158 | 1.603 (0.179, 14.364) | 0.6732 | 0 (0) | 0 (0) | X | X | X |
| Urinary tract infection (%) | 24 (0.57) | 11 (1.66) | 0.0048 * | 2.970 (1.448, 6.098) | 0.0030 * | 5 (0.81) | 10 (1.61) | 0.1940 | 2.016 (0.685, 5.934) | 0.2028 |
| Pulmonary embolism (%) | 18 (0.42) | 6 (0.91) | 0.1247 | 2.147 (0.849, 5.429) | 0.1063 | 2 (0.32) | 6 (0.97) | 0.2875 | 3.019 (0.607, 15.015) | 0.1770 |
| Cardiac arrest requiring CPR (%) | 4 (0.09) | 2 (0.30) | 0.1887 | 3.211 (0.587, 17.565) | 0.1785 | 0 (0) | 2 (0.32) | 0.4996 | >999.999 (<0.001, >999.999) | 0.9426 |
| Myocardial infarction (%) | 9 (0.21) | 1 (0.15) | 1.0000 | 0.712 (0.090, 5.626) | 0.7476 | 4 (0.64) | 1 (0.16) | 0.3740 | 0.249 (0.028, 2.232) | 0.2140 |
| Return to OR (%) | 60 (1.42) | 14 (2.12) | 0.1691 | 1.506 (0.837, 2.710) | 0.1720 | 9 (1.45) | 13 (2.09) | 0.3895 | 1.454 (0.617, 3.426) | 0.3922 |
| DVT/thrombophlebitis (%) | 11 (0.26) | 4 (0.61) | 0.1333 | 2.338 (0.742, 7.366) | 0.1467 | 2 (0.32) | 3 (0.48) | 1.0000 | 1.502 (0.250, 9.020) | 0.6563 |
| Bleeding transfusions (%) | 15 (0.35) | 14 (2.12) | <0.0001 * | 6.089 (2.926, 12.674) | <0.0001* | 5 (0.81) | 10 (1.61) | 0.1940 | 2.016 (0.685, 5.934) | 0.2028 |
| Sepsis (%) | 16 (0.38) | 2 (0.30) | 1.0000 | 0.801 (0.184, 3.489) | 0.7671 | 1 (0.16) | 2 (0.32) | 1.0000 | 2.003 (0.181, 22.149) | 0.5709 |
| Septic shock (%) | 7 (0.17) | 2 (0.30) | 0.3480 | 1.834 (0.380, 8.845) | 0.4502 | 1 (0.16) | 1 (0.16) | 1.0000 | 1.000 (0.062, 16.023) | 1.0000 |
| Mean length of total hospital stay (std) | 2.03 (2.83) | 3.22 (2.40) | <0.0001 * | 5.005 (4.300, 5.825) | <0.0001 * | 2.25 (3.86) | 3.11 (2.23) | <0.0001 * | 5.215 (4.190, 6.491) | <0.0001 * |
| Mean days from operation to discharge (std) | 1.96 (2.39) | 3.18 (2.35) | <0.0001 * | 5.127 (4.403, 5.969) | <0.0001 * | 2.12 (2.94) | 3.08 (2.22) | <0.0001 * | 5.328 (4.278, 6.635) | <0.0001 * |
| Still in hospital > 30 days (%) | 217 (5.12) | 49 (7.41) | 0.0157 * | 1.483 (1.075, 2.045) | 0.0163 * | 29 (4.67) | 46 (7.41) | 0.0429 * | 1.633 (1.012, 2.636) | 0.0446 * |
| Unplanned reoperation (%) | 275 (6.49) | 62 (9.38) | 0.0064 * | 1.491 (1.117, 1.990) | 0.0067 * | 38 (6.12) | 58 (9.34) | 0.0336 * | 1.581 (1.033, 2.418) | 0.0348 * |
| Death (%) | 13 (0.31) | 3 (0.45) | 0.4672 | 1.481 (0.421, 5.211) | 0.5406 | 0 (0) | 3 (0.48) | 0.2494 | >999.999 (<0.001, >999.999) | 0.9533 |
| Before PSM | ||||
| Parameter | Adjusted OR | 95% CI | p-Value | |
| Age | 1.11 | 1.049 | 1.174 | 0.0003 * |
| Preoperative hematocrit | 0.873 | 0.803 | 0.949 | 0.0014 * |
| Preoperative serum creatinine | 0.36 | 0.12 | 1.083 | 0.0690 |
| Steroid use for chronic condition | 4.74 | 1.315 | 17.086 | 0.0174 * |
| CHF in 30 days before surgery | 15.267 | 0.92 | 253.327 | 0.0572 |
| Currently on dialysis (preop) | 191.335 | 12.017 | >999.999 | 0.0002 * |
| Dyspnea: moderate exertion vs. no | 0.362 | 0.021 | 6.325 | 0.4863 |
| Dyspnea: at rest vs. no | 26.253 | 2.45 | 281.345 | 0.0069 * |
| Disseminated cancer | 16.523 | 2.333 | 117.02 | 0.0050 * |
| After PSM | ||||
| CHF in 30 days before surgery | 123.402 | 9.577 | >999.999 | 0.0002 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chan, R.W.-Y.; Chiang, Y.-H.; Lin, H.-C.; Chang, C.-Y.; Tsou, Y.-S. Postoperative 30-Day Comparative Complications of Multilevel Anterior Cervical Discectomy and Fusion and Laminoplasty for Cervical Spondylotic Myelopathy: An Evidence in Reaching Consensus. Diagnostics 2023, 13, 2024. https://doi.org/10.3390/diagnostics13122024
Chan RW-Y, Chiang Y-H, Lin H-C, Chang C-Y, Tsou Y-S. Postoperative 30-Day Comparative Complications of Multilevel Anterior Cervical Discectomy and Fusion and Laminoplasty for Cervical Spondylotic Myelopathy: An Evidence in Reaching Consensus. Diagnostics. 2023; 13(12):2024. https://doi.org/10.3390/diagnostics13122024
Chicago/Turabian StyleChan, Ryan Wing-Yuk, Yung-Hsiao Chiang, Hsiu-Chen Lin, Chih-Yau Chang, and Yi-Syue Tsou. 2023. "Postoperative 30-Day Comparative Complications of Multilevel Anterior Cervical Discectomy and Fusion and Laminoplasty for Cervical Spondylotic Myelopathy: An Evidence in Reaching Consensus" Diagnostics 13, no. 12: 2024. https://doi.org/10.3390/diagnostics13122024
APA StyleChan, R. W.-Y., Chiang, Y.-H., Lin, H.-C., Chang, C.-Y., & Tsou, Y.-S. (2023). Postoperative 30-Day Comparative Complications of Multilevel Anterior Cervical Discectomy and Fusion and Laminoplasty for Cervical Spondylotic Myelopathy: An Evidence in Reaching Consensus. Diagnostics, 13(12), 2024. https://doi.org/10.3390/diagnostics13122024





