Fluid-Attenuated Inversion Recovery Sequence with Fat Suppression for Assessment of Ankle Synovitis without Contrast Enhancement: Comparison with Contrast-Enhanced MRI
Abstract
1. Introduction
2. Materials and Methods
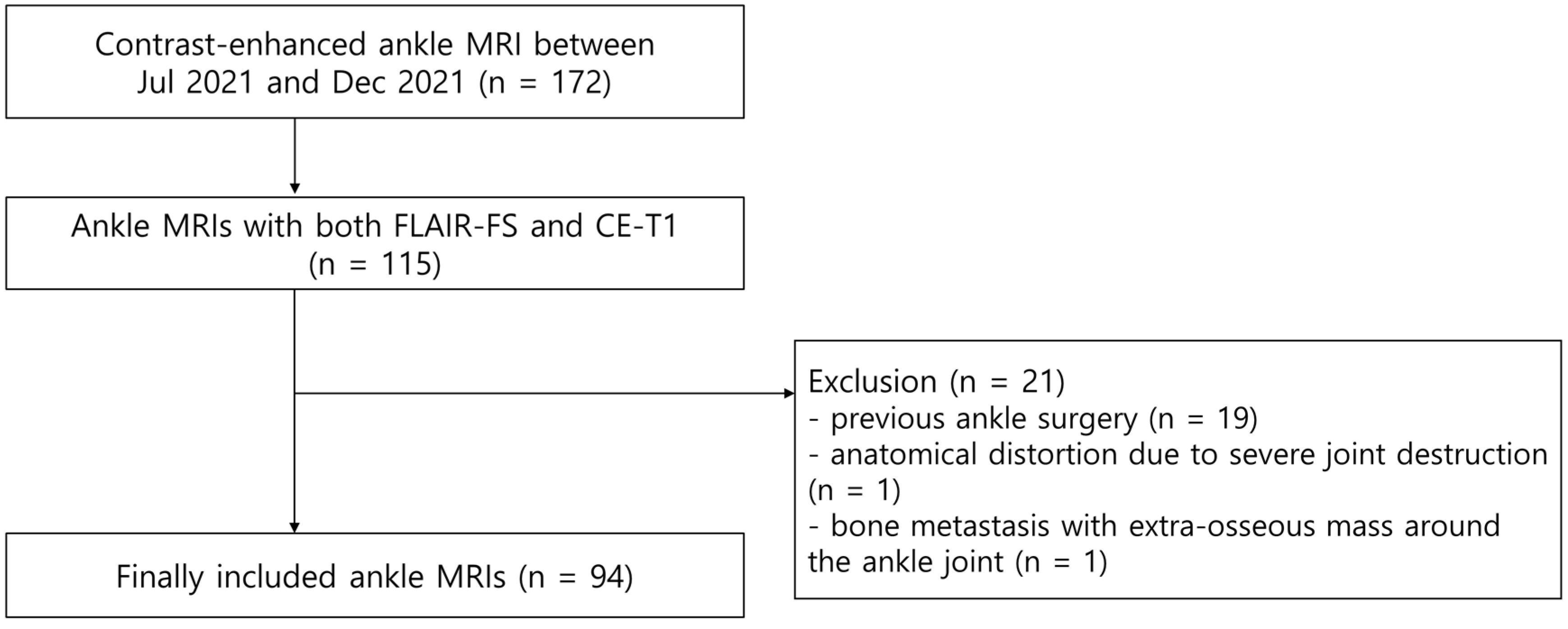
2.1. Patients
2.2. Magnetic Resonance Imaging Protocol
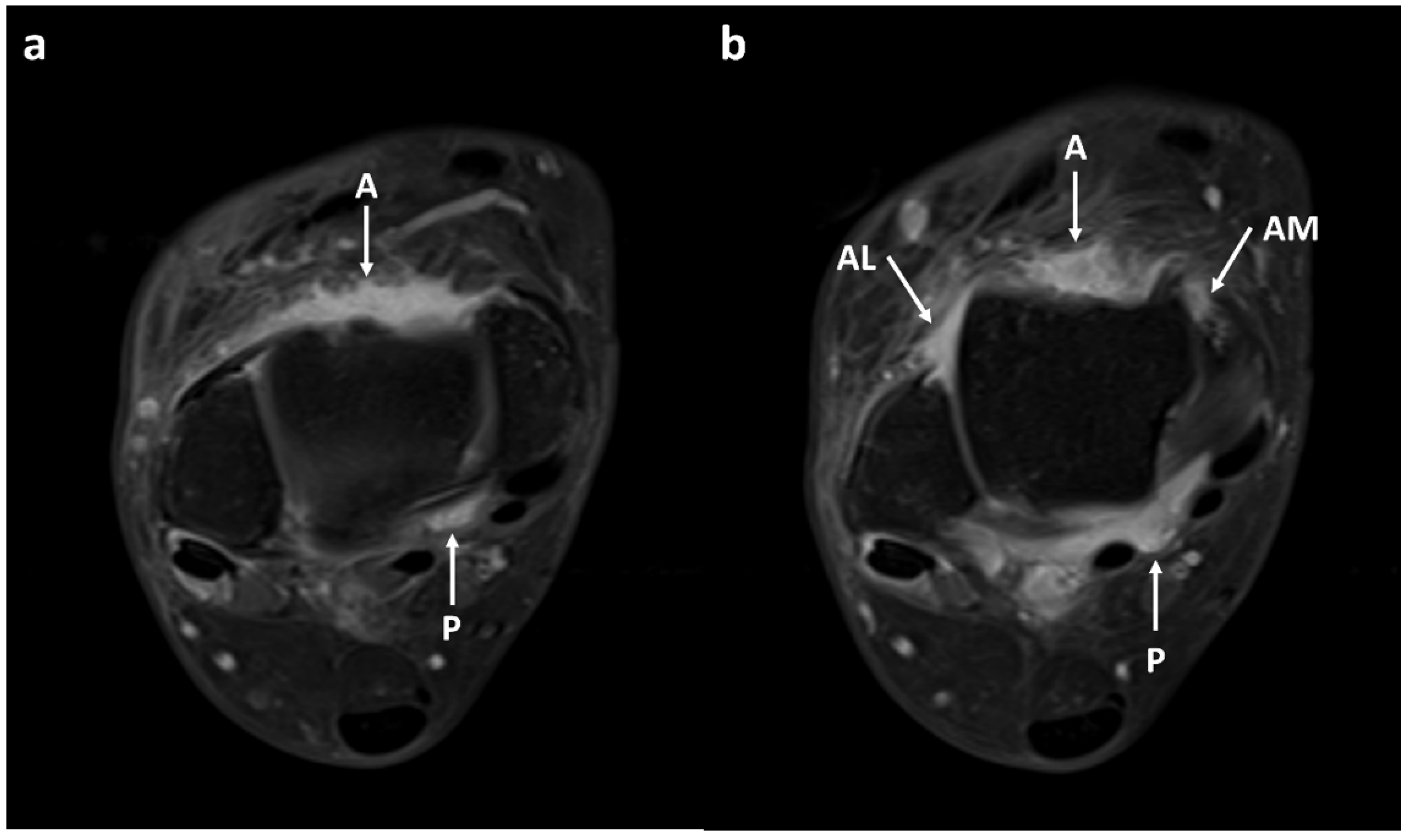
2.3. Image Analysis
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Synovial Visibility on FLAIR-FS and CE-T1 Images
3.3. Comparison of Synovial Thickness on FLAIR-FS and CE-T1 Images
3.4. Interobserver and Intraobserver Reliability in the Assessment of Synovium
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hayashi, D.; Roemer, F.W.; Katur, A.; Felson, D.T.; Yang, S.-O.; Alomran, F.; Guermazi, A. Imaging of synovitis in osteoarthritis: Current status and outlook. Semin. Arthritis Rheum. 2011, 41, 116–130. [Google Scholar] [CrossRef]
- Burke, C.J.; Alizai, H.; Beltran, L.S.; Regatte, R.R. MRI of synovitis and joint fluid. J. Magn. Reson. Imaging 2019, 49, 1512–1527. [Google Scholar] [CrossRef]
- Prieto-Potin, I.; Largo, R.; Roman-Blas, J.A.; Herrero-Beaumont, G.; Walsh, D. Characterization of multinucleated giant cells in synovium and subchondral bone in knee osteoarthritis and rheumatoid arthritis. BMC Musculoskelet. Disord. 2015, 16, 226. [Google Scholar] [CrossRef]
- Baker, K.; Grainger, A.; Niu, J.; Clancy, M.; Guermazi, A.; Crema, M.; Hughes, L.; Buckwalter, J.; Wooley, A.; Nevitt, M.; et al. Relation of synovitis to knee pain using contrast-enhanced MRIs. Ann. Rheum. Dis. 2010, 69, 1779–1783. [Google Scholar] [CrossRef]
- Guermazi, A.; Hayashi, D.; Roemer, F.W.; Zhu, Y.; Niu, J.; Crema, M.D.; Javaid, M.K.; Marra, M.D.; Lynch, J.A.; El-Khoury, G.Y.; et al. Synovitis in knee osteoarthritis assessed by contrast-enhanced magnetic resonance imaging (MRI) is associated with radiographic tibiofemoral osteoarthritis and MRI-detected widespread cartilage damage: The MOST study. J. Rheumatol. 2014, 41, 501–508. [Google Scholar] [CrossRef]
- Østergaard, M.; Gideon, P.; Henriksen, O.; Lorenzen, I. Synovial volume—A marker of disease severity in rheumatoid arthritis? Quantification by MRI. Scand. J. Rheumatol. 1994, 23, 197–202. [Google Scholar] [CrossRef]
- Huh, Y.M.; Suh, J.S.; Lee, J.W.; Song, H.T. Synovitis and soft tissue impingement of the ankle: Assessment with enhanced three-dimensional FSPGR MR imaging. J. Magn. Reson. Imaging 2004, 19, 108–116. [Google Scholar] [CrossRef]
- Acevedo, J.I.; Busch, M.T.; Ganey, T.M.; Hutton, W.C.; Ogden, J.A. Coaxial portals for posterior ankle arthroscopy: An anatomic study with clinical correlation on 29 patients. Arthroscopy 2000, 16, 836–842. [Google Scholar] [CrossRef]
- Do, C.; DeAguero, J.; Brearley, A.; Trejo, X.; Howard, T.; Escobar, G.P.; Wagner, B. Gadolinium-based contrast agent use, their safety, and practice evolution. Kidney360 2020, 1, 561–568. [Google Scholar] [CrossRef]
- Yoo, H.J.; Hong, S.H.; Oh, H.Y.; Choi, J.-Y.; Chae, H.D.; Ahn, J.M.; Kang, H.S. Diagnostic accuracy of a fluid-attenuated inversion-recovery sequence with fat suppression for assessment of peripatellar synovitis: Preliminary results and comparison with contrast-enhanced MR imaging. Radiology 2017, 283, 769–778. [Google Scholar] [CrossRef]
- Huang, Z.-G.; Chen, X.-L.; Shi, K.-N.; Yan, R.; Chen, H.; Yang, M.-X.; Gao, B.-X.; Chan, Q.; Wang, G.-C. The application of T2W SPIR-FLAIR in the diagnosis of hip synovitis in patients with spondyloarthritis. Br. J. Radiol. 2016, 89, 20160566. [Google Scholar] [CrossRef]
- Treutlein, C.; Bäuerle, T.; Nagel, A.M.; Guermazi, A.; Kleyer, A.; Simon, D.; Schett, G.; Hepp, T.; Uder, M.; Roemer, F.W. Comprehensive assessment of knee joint synovitis at 7 T MRI using contrast-enhanced and non-enhanced sequences. BMC Musculoskelet. Disord. 2020, 21, 116. [Google Scholar] [CrossRef]
- Berman, Z.; Tafur, M.; Ahmed, S.S.; Huang, B.K.; Chang, E.Y. Ankle impingement syndromes: An imaging review. Br. J. Radiol. 2017, 90, 20160735. [Google Scholar] [CrossRef]
- Guermazi, A.; Roemer, F.W.; Hayashi, D.; Crema, M.D.; Niu, J.; Zhang, Y.; Marra, M.D.; Katur, A.; Lynch, J.A.; El-Khoury, G.Y.; et al. Assessment of synovitis with contrast-enhanced MRI using a whole-joint semiquantitative scoring system in people with, or at high risk of, knee osteoarthritis: The MOST study. Ann. Rheum. Dis. 2011, 70, 805–811. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Sauer, A.; Li, M.; Holl-Wieden, A.; Pabst, T.; Neubauer, H. Readout-segmented multi-shot diffusion-weighted MRI of the knee joint in patients with juvenile idiopathic arthritis. Pediatr. Rheumatol. Online J. 2017, 15, 73. [Google Scholar] [CrossRef]
- Barendregt, A.M.; van Gulik, E.C.; Lavini, C.; Nusman, C.M.; van den Berg, J.M.; Schonenberg-Meinema, D.; Dolman, K.M.; Kuijpers, T.W.; Hemke, R.; Maas, M. Diffusion-weighted imaging for assessment of synovial inflammation in juvenile idiopathic arthritis: A promising imaging biomarker as an alternative to gadolinium-based contrast agents. Eur. Radiol. 2017, 27, 4889–4899. [Google Scholar] [CrossRef]
- Barendregt, A.M.; Mazzoli, V.; van Gulik, E.C.; Schonenberg-Meinema, D.; Nassar-Sheikh al Rashid, A.; Nusman, C.M.; Dolman, K.M.; van den Berg, J.M.; Kuijpers, T.W.; Nederveen, A.J.; et al. Juvenile idiopathic arthritis: Diffusion-weighted MRI in the assessment of arthritis in the knee. Radiology 2020, 295, 373–380. [Google Scholar] [CrossRef]
- de Vries, B.A.; Breda, S.J.; Sveinsson, B.; McWalter, E.J.; Meuffels, D.E.; Krestin, G.P.; Hargreaves, B.A.; Gold, G.E.; Oei, E.H. Detection of knee synovitis using non-contrast-enhanced qDESS compared with contrast-enhanced MRI. Arthritis Res. Ther. 2021, 23, 55. [Google Scholar] [CrossRef]
- Son, Y.N.; Jin, W.; Jahng, G.-H.; Cha, J.G.; Park, Y.S.; Yun, S.J.; Park, S.Y.; Park, J.S.; Ryu, K.N. Efficacy of double inversion recovery magnetic resonance imaging for the evaluation of the synovium in the femoro-patellar joint without contrast enhancement. Eur. Radiol. 2018, 28, 459–467. [Google Scholar] [CrossRef]
- Jahng, G.H.; Jin, W.; Yang, D.M.; Ryu, K.N. Optimization of a double inversion recovery sequence for noninvasive synovium imaging of joint effusion in the knee. Med. Phys. 2011, 38, 2579–2585. [Google Scholar] [CrossRef]
- Østergaard, M.; Klarlund, M. Importance of timing of post-contrast MRI in rheumatoid arthritis: What happens during the first 60 minutes after IV gadolinium-DTPA? Ann. Rheum. Dis. 2001, 60, 1050–1054. [Google Scholar] [CrossRef]
- Loeuille, D.; Rat, A.-C.; Goebel, J.-C.; Champigneulle, J.; Blum, A.; Netter, P.; Gillet, P.; Chary-Valckenaere, I. Magnetic resonance imaging in osteoarthritis: Which method best reflects synovial membrane inflammation?: Correlations with clinical, macroscopic and microscopic features. Osteoarthritis Cartilage 2009, 17, 1186–1192. [Google Scholar] [CrossRef]
- Steinbach, L.S.; Palmer, W.E.; Schweitzer, M.E. Special focus session: MR arthrography. Radiographics 2002, 22, 1223–1246. [Google Scholar] [CrossRef]
- American College of Radiology. ACR Manual on Contrast Media. 2023. Available online: https://www.acr.org/Clinical-Resources/Contrast-Manual (accessed on 25 May 2023).
- Kuo, P.H.; Kanal, E.; Abu-Alfa, A.K.; Cowper, S.E. Gadolinium-based MR contrast agents and nephrogenic systemic fibrosis. Radiology 2007, 242, 647–649. [Google Scholar] [CrossRef]
- Pezeshk, P.; Alian, A.; Chhabra, A. Role of chemical shift and Dixon based techniques in musculoskeletal MR imaging. Eur. J. Radiol. 2017, 94, 93–100. [Google Scholar] [CrossRef]
- Del Grande, F.; Santini, F.; Herzka, D.A.; Aro, M.R.; Dean, C.W.; Gold, G.E.; Carrino, J.A. Fat-suppression techniques for 3-T MR imaging of the musculoskeletal system. Radiographics 2014, 34, 217–233. [Google Scholar] [CrossRef]



| Parameters | FLAIR-FS | CE-T1 |
|---|---|---|
| TR/TE (ms) | 9000/93 | 306–871/10 |
| Inversion time (ms) | 2100 | N/A |
| Flip angle (°) | 150 | 120 |
| Echo train length | 22 | 3 |
| Bandwidth (kHz/pixel) | 269 | 265 |
| Field of view (mm) | 140 | 140 |
| Matrix size | 320 × 154 | 320 × 182 |
| Pixel size (mm) | 0.44 × 0.91 | 0.44 × 0.77 |
| Slice thickness/gap (mm) | 3/0 | 3/0 |
| Number of signals acquired | 1 | 2 |
| Number of sections | 36 | 36 |
| Fat suppression | Chemically selective | Chemically selective |
| Acquisition time (min) | 2:42 | 3:17 |
| Synovial Visibility Grade | Synovial Thickness Score | |||||
|---|---|---|---|---|---|---|
| FLAIR-FS | CE-T1 | p Value | FLAIR-FS | CE-T1 | p Value | |
| Reader 1 | ||||||
| Anterior | 3.89 ± 0.34 | 3.97 ± 0.18 | 0.052 | 0.59 ± 0.72 | 0.88 ± 0.81 | <0.001 * |
| Anteromedial | 3.87 ± 0.37 | 3.90 ± 0.33 | 0.491 | 0.32 ± 0.61 | 0.40 ± 0.64 | 0.046 * |
| Anterolateral | 3.98 ± 0.15 | 3.99 ± 0.10 | 0.564 | 0.50 ± 0.67 | 0.69 ± 0.73 | 0.001 * |
| Posterior | 3.78 ± 0.42 | 3.88 ± 0.32 | 0.041 * | 0.57 ± 0.74 | 0.79 ± 0.80 | <0.001 * |
| Whole joint | 3.88 ± 0.34 | 3.93 ± 0.26 | 0.016 * | 1.98 ± 2.19 | 2.77 ± 2.42 | <0.001 * |
| Reader 2 | ||||||
| Anterior | 3.96 ± 0.25 | 3.98 ± 0.21 | 0.577 | 0.52 ± 0.68 | 0.94 ± 0.87 | <0.001 * |
| Anteromedial | 3.86 ± 0.43 | 3.96 ± 0.29 | 0.050 | 0.32 ± 0.63 | 0.57 ± 0.78 | <0.001 * |
| Anterolateral | 3.95 ± 0.27 | 3.99 ± 0.10 | 0.157 | 0.32 ± 0.63 | 0.67 ± 0.79 | <0.001 * |
| Posterior | 3.91 ± 0.28 | 3.97 ± 0.18 | 0.132 | 0.47 ± 0.71 | 0.88 ± 0.88 | <0.001 * |
| Whole joint | 3.92 ± 0.32 | 3.97 ± 0.20 | 0.009 * | 1.63 ± 1.97 | 3.06 ± 2.65 | <0.001 * |
| Synovial Visibility | Partially Visible | Fully Visible | p Value | ||
|---|---|---|---|---|---|
| Grade 1 | Grade 2 | Grade 3 | Grade 4 | ||
| Reader 1 | |||||
| FLAIR-FS | 0 (0.0%) | 2 (0.5%) | 41 (10.9%) | 333 (88.6%) | 1.000 |
| CE-T1 | 0 (0.0%) | 1 (0.3%) | 22 (5.9%) | 353 (93.9%) | |
| Reader 2 | |||||
| FLAIR-FS | 0 (0.0%) | 5 (1.3%) | 20 (5.3%) | 351 (93.4%) | 0.688 |
| CE-T1 | 0 (0.0%) | 3 (0.8%) | 4 (1.1%) | 369 (98.1%) | |
| Synovial Thickness | Score 0 (<2 mm) | Score 1 (2–4 mm) | Score 2 (≥4 mm) | κ Value |
|---|---|---|---|---|
| Reader 1 | ||||
| FLAIR-FS | 233 (62.0%) | 100 (26.6%) | 43 (11.4%) | 0.65 [0.56, 0.71] |
| CE-T1 | 187 (49.7%) | 118 (31.4%) | 71 (18.9%) | |
| Reader 2 | ||||
| FLAIR-FS | 261 (69.4%) | 77 (20.5%) | 38 (10.1%) | 0.41 [0.34, 0.49] |
| CE-T1 | 187 (49.7%) | 90 (23.9%) | 99 (26.3%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, J.H.; Moon, S.G.; Jung, H.-G.; Kwon, E.Y. Fluid-Attenuated Inversion Recovery Sequence with Fat Suppression for Assessment of Ankle Synovitis without Contrast Enhancement: Comparison with Contrast-Enhanced MRI. Diagnostics 2023, 13, 1960. https://doi.org/10.3390/diagnostics13111960
Kang JH, Moon SG, Jung H-G, Kwon EY. Fluid-Attenuated Inversion Recovery Sequence with Fat Suppression for Assessment of Ankle Synovitis without Contrast Enhancement: Comparison with Contrast-Enhanced MRI. Diagnostics. 2023; 13(11):1960. https://doi.org/10.3390/diagnostics13111960
Chicago/Turabian StyleKang, Ji Hee, Sung Gyu Moon, Hong-Geun Jung, and Eun Young Kwon. 2023. "Fluid-Attenuated Inversion Recovery Sequence with Fat Suppression for Assessment of Ankle Synovitis without Contrast Enhancement: Comparison with Contrast-Enhanced MRI" Diagnostics 13, no. 11: 1960. https://doi.org/10.3390/diagnostics13111960
APA StyleKang, J. H., Moon, S. G., Jung, H.-G., & Kwon, E. Y. (2023). Fluid-Attenuated Inversion Recovery Sequence with Fat Suppression for Assessment of Ankle Synovitis without Contrast Enhancement: Comparison with Contrast-Enhanced MRI. Diagnostics, 13(11), 1960. https://doi.org/10.3390/diagnostics13111960





