How Automated Techniques Ease Functional Assessment of the Fetal Heart: Applicability of MPI+™ for Direct Quantification of the Modified Myocardial Performance Index
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Acquisition of PW Doppler Waveform Images
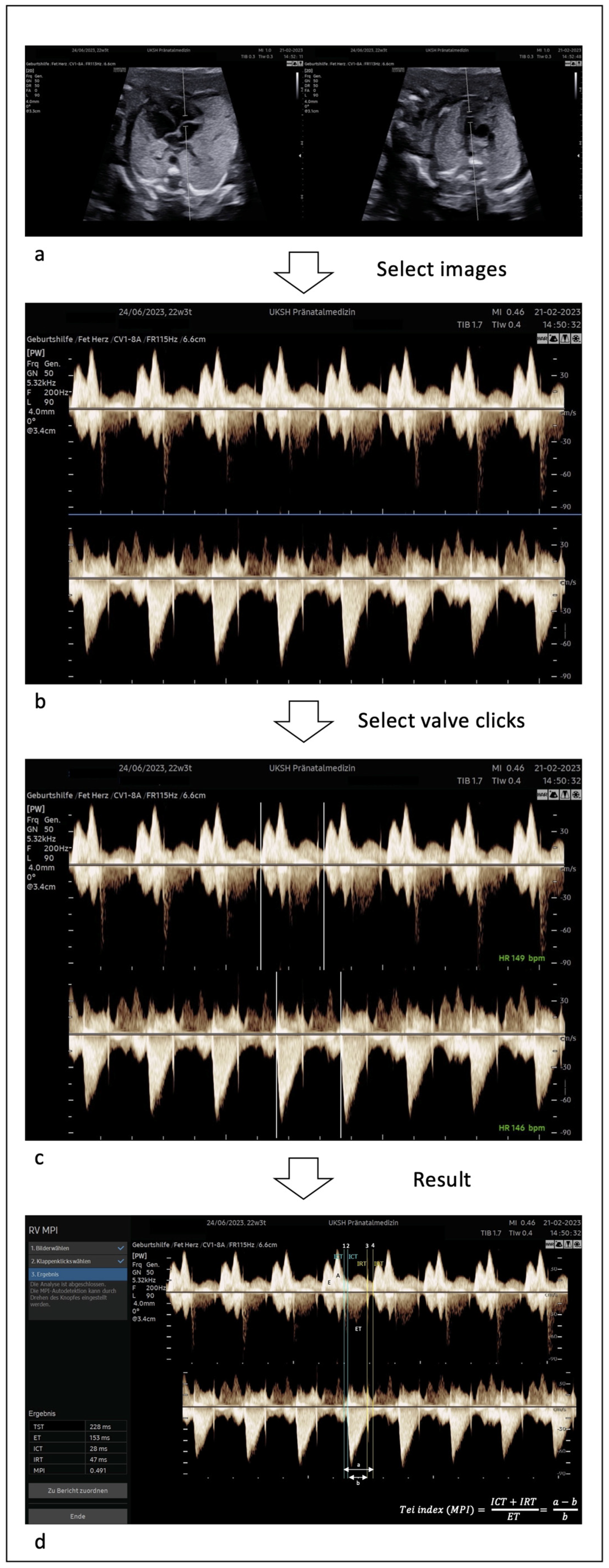
2.3. Application of MPI+™
2.4. Statistics
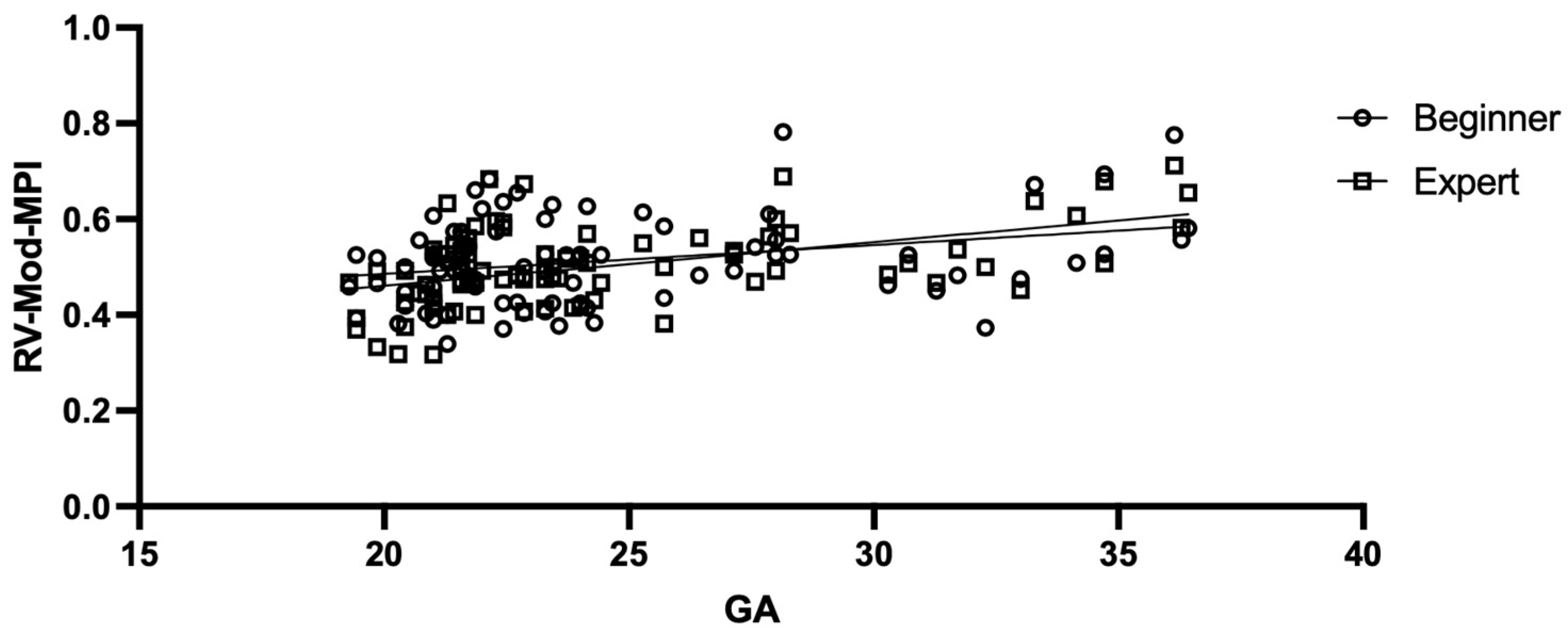
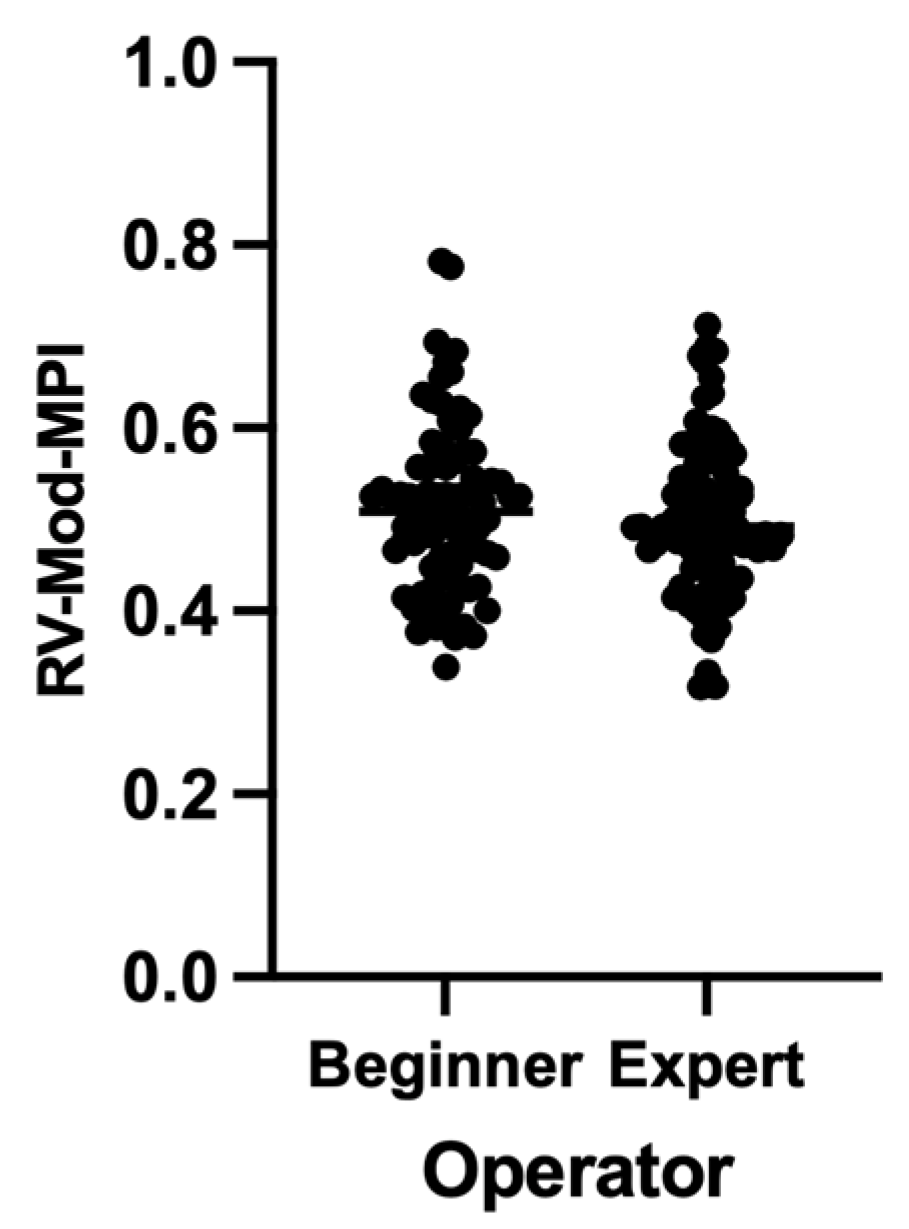
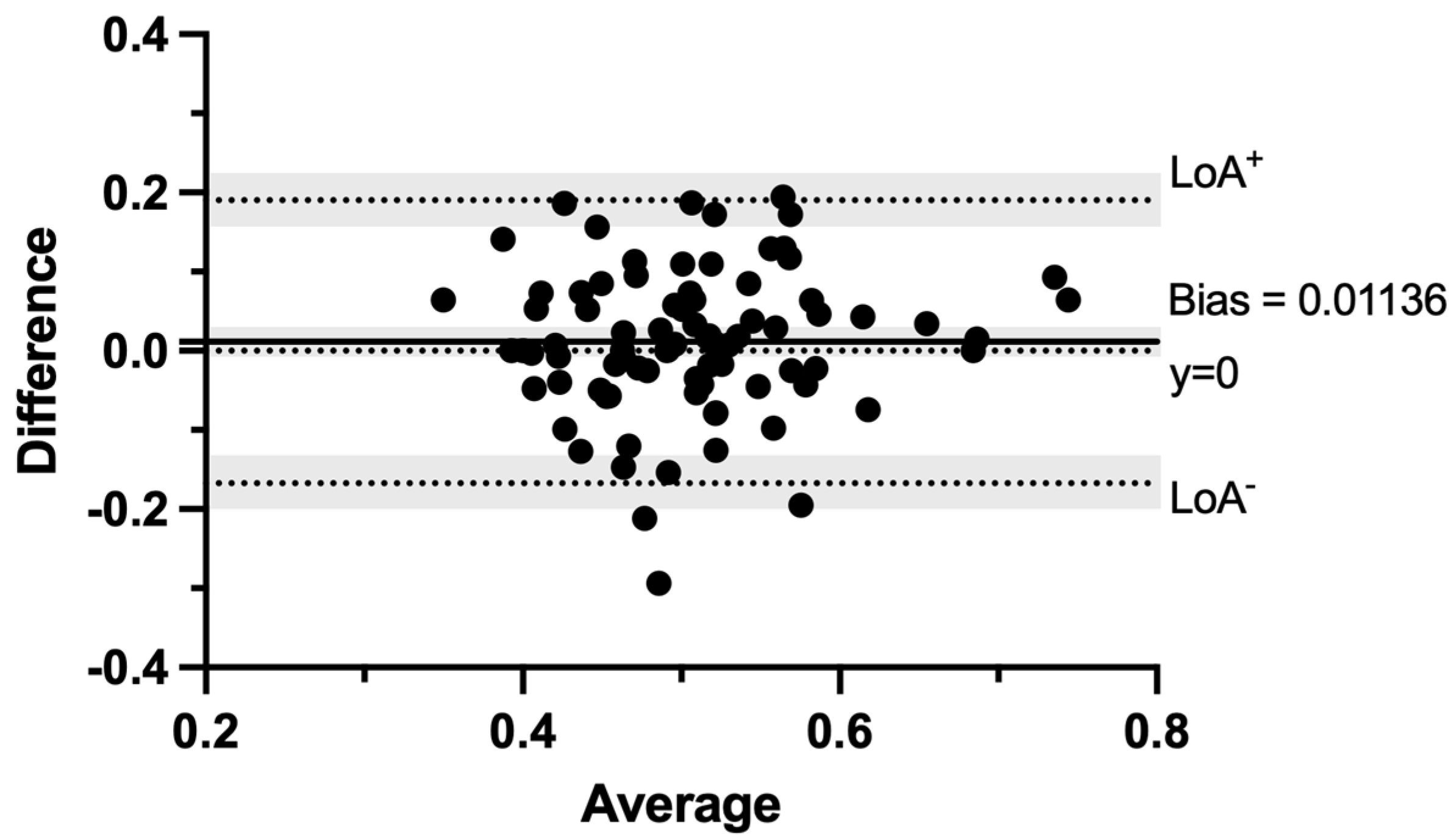
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Maheshwari, P.; Henry, A.; Welsh, A.W. The Fetal Modified Myocardial Performance Index: Is Automation the Future? BioMed Res. Int. 2015, 2015, 215910. [Google Scholar] [CrossRef]
- Graupner, O.; Enzensberger, C. Kardiale Funktionsanalyse beim Feten: Schritt für Schritt. Gynäkologe 2022, 55, 7–13. [Google Scholar] [CrossRef]
- Crispi, F.; Gratacós, E. Fetal Cardiac Function: Technical Considerations and Potential Research and Clinical Applications. Fetal Diagn. Ther. 2012, 32, 47–64. [Google Scholar] [CrossRef] [PubMed]
- Tei, C.; Ling, L.H.; Hodge, D.O.; Bailey, K.R.; Oh, J.K.; Rodeheffer, R.J.; Tajik, A.J.; Seward, J.B. New index of combined systolic and diastolic myocardial performance: A simple and repro-ducible measure of cardiac function—A study in normals and dilated cardiomyopathy. J. Cardiol. 1995, 26, 357–366. [Google Scholar] [PubMed]
- Tsutsumi, T.; Ishii, M.; Eto, G.; Hota, M.; Kato, H. Serial evaluation for myocardial performance in fetuses and neonates using a new Doppler index. Pediatr. Int. 1999, 41, 722–727. [Google Scholar] [CrossRef] [PubMed]
- Mori, Y.; Rice, M.J.; McDonald, R.W.; Reller, M.D.; Wanitkun, S.; Harada, K.; Sahn, D.J. Evaluation of systolic and diastolic ventricular performance of the right ventricle in fetuses with ductal constriction using the Doppler Tei index. Am. J. Cardiol. 2001, 88, 1173–1178. [Google Scholar] [CrossRef]
- Falkensammer, C.B.; Paul, J.; Huhta, J.C. Fetal congestive heart failure: Correlation of Tei-Index and Cardiovascular-Score. J. Perinat. Med. 2001, 29, 390–398. [Google Scholar] [CrossRef]
- Eidem, B.W.; Edwards, J.M.; Cetta, F. Quantitative Assessment of Fetal Ventricular Function: Establishing Normal Values of the Myocardial Performance Index in the Fetus. Echocardiography 2001, 18, 9–13. [Google Scholar] [CrossRef]
- Ichizuka, K.; Matsuoka, R.; Hasegawa, J.; Shirato, N.; Jimbo, M.; Otsuki, K.; Sekizawa, A.; Farina, A.; Okai, T. The Tei index for evaluation of fetal myocardial performance in sick fetuses. Early Hum. Dev. 2005, 81, 273–279. [Google Scholar] [CrossRef]
- Inamura, N.; Taketazu, M.; Smallhorn, J.F.; Hornberger, L.K. Left Ventricular Myocardial Performance in the Fetus with Severe Tricuspid Valve Disease and Tricuspid Insufficiency. Am. J. Perinatol. 2005, 22, 91–97. [Google Scholar] [CrossRef]
- Hernandez-Andrade, E.; López-Tenorio, J.; Figueroa-Diesel, H.; Sanin-Blair, J.; Carreras, E.; Cabero, L.; Gratacos, E. A modified myocardial performance (Tei) index based on the use of valve clicks improves reproducibility of fetal left cardiac function assessment: Reproducibility of a modified fetal myo-cardial performance index. Ultrasound Obstet. Gynecol. 2005, 26, 227–232. [Google Scholar] [CrossRef] [PubMed]
- Friedman, D.; Buyon, J.; Kim, M.; Glickstein, J.S. Fetal cardiac function assessed by Doppler myocardial performance index (Tei Index): The fetal Tei Index. Ultrasound Obstet. Gynecol. 2003, 21, 33–36. [Google Scholar] [CrossRef] [PubMed]
- Raboisson, M.-J.; Bourdages, M.; Fouron, J.-C. Measuring left ventricular myocardial performance index in fetuses. Am. J. Cardiol. 2003, 91, 919–921. [Google Scholar] [CrossRef] [PubMed]
- Meriki, N.; Izurieta, A.; Welsh, A.W. Fetal left modified myocardial performance index: Technical refinements in obtaining pulsed-Doppler waveforms: The fetal left MPI: Technical refinements. Ultrasound Obstet. Gynecol. 2011, 39, 421–429. [Google Scholar] [CrossRef]
- Ghawi, H.; Gendi, S.; Mallula, K.; Zghouzi, M.; Faza, N.; Awad, S. Fetal Left and Right Ventricle Myocardial Performance Index: Defining Normal Values for the Second and Third Trimesters—Single Tertiary Center Experience. Pediatr. Cardiol. 2013, 34, 1808–1815. [Google Scholar] [CrossRef]
- Lee, M.Y.; Kim, S.Y.; Won, H.S. White Paper: MPI+, an Automatic Tool for Measurement of Fetal Right Ventricular Myocardial Per-Formance Index. Published online 9 December 2021. Available online: https://www.samsunghealthcare.com/en/products/UltrasoundSystem (accessed on 19 October 2022).
- Meriki, N.; Welsh, A.W. Fetal cardiac function: Feasibility in obtaining the right modified myocardial performance index in a single Doppler waveform. Australas. J. Ultrasound Med. 2017, 20, 18–25. [Google Scholar] [CrossRef]
- Ali, S.; Okasha, A.; Elsirgany, S.; Abdel-Rasheed, M.; Khalil, A.; El-Anwary, S.; Elsheikhah, A. Normal reference ranges for fetal cardiac function: Assessed by modified Doppler myocardial performance index (Mod MPI) in the Egyptian population. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 251, 66–72. [Google Scholar] [CrossRef]
- Kim, S.-M.; Ye, S.-Y. Evaluation of the Fetal Left Ventricular Myocardial Performance Index (MPI) by Using an Automated Measurement of Doppler Signals in Normal Pregnancies. Diagnostics 2021, 11, 358. [Google Scholar] [CrossRef] [PubMed]
- Mahajan, A.; Henry, A.; Meriki, N.; Hernandez-Andrade, E.; Crispi, F.; Wu, L.; Welsh, A.W. The (Pulsed-Wave) Doppler Fetal Myocardial Performance Index: Technical Challenges, Clinical Applications and Future Research. Fetal Diagn. Ther. 2015, 38, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Ozel, A.; Davutoglu, E.A.; Ozdemir, M.E.; Oztunc, F.; Madazli, R. Assessment of fetal left ventricular modified myocardial performance index and its prognostic significance for adverse perinatal outcome in intrahepatic cholestasis of pregnancy. J. Matern. Neonatal Med. 2018, 33, 2000–2005. [Google Scholar] [CrossRef]
- Tutschek, B.; Schmidt, K.G. Techniques for assessing cardiac output and fetal cardiac function. Semin. Fetal Neonatal Med. 2011, 16, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Kang, O.; Kim, S.Y.; Lee, M.; Won, H.; Choi, K.; Lee, J.; Kim, M. Novel Technique for the Measurement of Fetal Right Modified Myocardial Performance Index Using Synchronized Images of Right Ventricular Inflow and Outflow and Clinical Application to Twin-to-Twin Transfusion Syndrome. J. Ultrasound Med. 2021, 40, 2467–2475. [Google Scholar] [CrossRef]
- Lee, M.-Y.; Won, H.-S.; Shim, J.-Y.; Lee, P.-R.; Kim, A.; Kil, E.-M.; Kim, M.-J. Novel Technique for Measurement of Fetal Right Myocardial Performance Index Using Dual Gate Pulsed-Wave Doppler: Fetal Cardiac Function. J. Ultrasound Med. 2017, 36, 1585–1594. [Google Scholar] [CrossRef]
- Harada, K.; Tamura, M.; Toyono, M.; Yasuoka, K. Comparison of the right ventricular Tei index by tissue Doppler imaging to that obtained by pulsed Doppler in children without heart disease. Am. J. Cardiol. 2002, 90, 566–569. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Wang, J.; Su, X.; Chen, X.; Zhou, Y.; Zhang, X.; Lu, H.; Niu, J.; Yu, L.; Sun, C.; et al. Reference ranges of fetal heart function using a Modified Myocardial Performance Index: A prospective multicentre, cross-sectional study. BMJ Open 2021, 11, e049640. [Google Scholar] [CrossRef] [PubMed]
- Comas, M.; Crispi, F.; Gómez, O.; Puerto, B.; Figueras, F.; Gratacós, E. Gestational age- and estimated fetal weight-adjusted reference ranges for myocardial tissue Doppler indices at 24–41 weeks’ gestation. Ultrasound Obstet. Gynecol. 2010, 37, 57–64. [Google Scholar] [CrossRef]
- Cruz-Martínez, R.; Figueras, F.; Bennasar, M.; García-Posadas, R.; Crispi, F.; Hernández-Andrade, E.; Gratacós, E. Normal Reference Ranges from 11 to 41 Weeks’ Gestation of Fetal Left Modified Myocardial Performance Index by Conventional Doppler with the Use of Stringent Criteria for Delimitation of the Time Periods. Fetal Diagn. Ther. 2012, 32, 79–86. [Google Scholar] [CrossRef]
- Hamela-Olkowska, A.; Szymkiewicz-Dangel, J. Quantitative assessment of the right and the left ventricular function using pulsed Doppler myocardial performance index in normal fetuses at 18 to 40 weeks of gestation. Ginekol. Pol. 2011, 82, 108–113. [Google Scholar] [PubMed]
- Lee, M.-Y.; Won, H.-S.; Park, J.E.; Shim, J.-Y.; Lee, P.-R.; Kim, A.; Lee, J.B. Fetal left modified myocardial performance index measured by the Auto Mod-MPI system: Development of reference values and application to recipients of twin-to-twin transfusion syndrome: Mod-MPI reference values. Prenat. Diagn. 2016, 36, 424–431. [Google Scholar] [CrossRef] [PubMed]
- Parasuraman, R.; Osmond, C.; Howe, D.T. Gestation-specific reference intervals for fetal cardiac Doppler indices from 12 to 40 weeks of gestation. Open J. Obstet. Gynecol. 2013, 3, 97–104. [Google Scholar] [CrossRef]
- Bhorat, I.; Bagratee, J.; Reddy, T. Gestational age-adjusted trends and reference intervals of the Modified Myocardial Performance Index (Mod-MPI) and its components, with its interpretation in the context of established cardiac physiological principles: Reference intervals of the Mod-MPI and its components in pregnanc. Prenat. Diagn. 2014, 34, 1031–1036. [Google Scholar] [CrossRef] [PubMed]
- Meriki, N.; Henry, A.; Sanderson, J.; Majajan, A.; Wu, L.; Welsh, A.W. Development of Normal Gestational Ranges for the Right Myocardial Performance Index in the Australian Population with Three Alternative Caliper Placements. Fetal Diagn. Ther. 2014, 36, 272–281. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Martinez, R.; Figueras, F.; Jaramillo, J.J.; Meler, E.; Méndez, A.; Hernandez-Andrade, E.; Gratacos, E. Learning curve for Doppler measurement of fetal modified myocardial performance index. Ultrasound Obstet. Gynecol. 2011, 37, 158–162. [Google Scholar] [CrossRef] [PubMed]
- Tegnander, E.; Eik-Nes, S.H. The examiner’s ultrasound experience has a significant impact on the detection rate of congenital heart defects at the second-trimester fetal examination. Ultrasound Obstet. Gynecol. 2006, 28, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Yeo, L.; Romero, R. Optical ultrasound simulation-based training in obstetric sonography. J. Matern. Neonatal Med. 2020, 35, 2469–2484. [Google Scholar] [CrossRef] [PubMed]
- Weichert, J.; Welp, A.; Scharf, J.L.; Dracopoulos, C.; Rody, A.; Gembicki, M. Künstliche Intelligenz in der pränatalen kardialen Diagnostik. Gynäkologe 2021, 55, 22–31. [Google Scholar] [CrossRef]
- Ahn, K.H.; Lee, K.-S. Artificial intelligence in obstetrics. Obstet. Gynecol. Sci. 2022, 65, 113–124. [Google Scholar] [CrossRef]
- Chen, Z.; Liu, Z.; Du, M.; Wang, Z. Artificial Intelligence in Obstetric Ultrasound: An Update and Future Applications. Front. Med. 2021, 8, 733468. [Google Scholar] [CrossRef]
- Edwards, C.; Chamunyonga, C.; Searle, B.; Reddan, T. The application of artificial intelligence in the sonography profession: Professional and educational considerations. Ultrasound 2022, 30, 273–282. [Google Scholar] [CrossRef]
- Steinhard, J.; Freundt, P.; Janzing, P.; Popov, V.; Menkhaus, R.; Ross, L. Künstliche Intelligenz und Simulation in der Pränatalmedizin–was wir von Maschinen lernen können. Gynäkologie 2022, 55, 746–758. [Google Scholar] [CrossRef]
- Yoon, H.; Lee, H.; Jeon, K.-W.; Jung, H.-K.; Lee, M.-Y.; Won, H.-S.; Jeon, E.-J.; Yang, E.-H.; Choi, J.-Y.; Hong, S.-J. Automated measurement of fetal myocardial performance index in ultrasound Doppler waveforms. Proc. SPIE 2014, 9040, 90401E. [Google Scholar] [CrossRef]
- Lee, M.-Y.; Won, H.-S.; Jeon, E.-J.; Yoon, H.C.; Choi, J.Y.; Hong, S.J.; Kim, M.-J. Feasibility of using Auto Mod-MPI system, a novel technique for automated measurement of fetal modified myocardial performance index. Ultrasound Obstet. Gynecol. 2013, 43, 640–645. [Google Scholar] [CrossRef] [PubMed]
- Suresh, R.; Sivanandan, S.; Singhal, N.; Lee, M.-Y.; Won, H.-S.; Lee, J. Automated measurement of fetal right-myocardial performance index from pulsed wave Doppler spectrum. In Medical Imaging 2019: Computer-Aided Diagnosis; Hahn, H.K., Mori, K., Eds.; SPIE: Bellingham, WA, USA, 2019; Volume 20. [Google Scholar] [CrossRef]
- Lobmaier, S.M.; Cruz-Lemini, M.; Valenzuela-Alcaraz, B.; Ortiz, J.U.; Martinez, J.M.; Gratacos, E.; Crispi, F. Influence of equipment and settings on myocardial performance index repeatability and definition of settings to achieve optimal reproducibility. Ultrasound Obstet. Gynecol. 2014, 43, 632–639. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.Y.; Msc, J.A.P.; McCandless, R.T. Prenatal detection of critical cardiac outflow tract anomalies remains suboptimal despite revised obstetrical imaging guidelines. Congenit. Heart Dis. 2018, 13, 748–756. [Google Scholar] [CrossRef]
- Carvalho, J.; Allan, L.; Chaoui, R.; Copel, J.; DeVore, G.; Hecher, K.; Lee, W.; Munoz, H.; Paladini, D.; Tutschek, B.; et al. ISUOG Practice Guidelines (updated): Sonographic screening examination of the fetal heart: ISUOG Guidelines. Ultrasound Obstet. Gynecol. 2013, 41, 348–359. [Google Scholar] [CrossRef]
- Crino, J.P.; Finberg, H.J.; Frieden, F.; Kuller, J.; Odibo, A.; Robichaux, A.; Bohm-Velez, M.; Pretorius, D.H.; Sheth, S.; Angtuaco, T.L.; et al. AIUM Practice Guideline for the Performance of Obstetric Ultrasound Examinations. J. Ultrasound Med. 2013, 32, 1083–1101. [Google Scholar] [CrossRef]
| Characteristics | Mean (Range) |
|---|---|
| Maternal age, years | 32.86 (19–42) |
| Nulliparous, % | 43.53 |
| Primiparity, % | 32.94 |
| BMI prior to pregnancy, kg/m2 | 24.85 (17.11–44.08) |
| GA at targeted ultrasound, weeks of gestation | 24.44 (19+2–36+3) |
| Fetal cephalic presentation, % | 61.18 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scharf, J.L.; Dracopoulos, C.; Gembicki, M.; Welp, A.; Weichert, J. How Automated Techniques Ease Functional Assessment of the Fetal Heart: Applicability of MPI+™ for Direct Quantification of the Modified Myocardial Performance Index. Diagnostics 2023, 13, 1705. https://doi.org/10.3390/diagnostics13101705
Scharf JL, Dracopoulos C, Gembicki M, Welp A, Weichert J. How Automated Techniques Ease Functional Assessment of the Fetal Heart: Applicability of MPI+™ for Direct Quantification of the Modified Myocardial Performance Index. Diagnostics. 2023; 13(10):1705. https://doi.org/10.3390/diagnostics13101705
Chicago/Turabian StyleScharf, Jann Lennard, Christoph Dracopoulos, Michael Gembicki, Amrei Welp, and Jan Weichert. 2023. "How Automated Techniques Ease Functional Assessment of the Fetal Heart: Applicability of MPI+™ for Direct Quantification of the Modified Myocardial Performance Index" Diagnostics 13, no. 10: 1705. https://doi.org/10.3390/diagnostics13101705
APA StyleScharf, J. L., Dracopoulos, C., Gembicki, M., Welp, A., & Weichert, J. (2023). How Automated Techniques Ease Functional Assessment of the Fetal Heart: Applicability of MPI+™ for Direct Quantification of the Modified Myocardial Performance Index. Diagnostics, 13(10), 1705. https://doi.org/10.3390/diagnostics13101705







