Electronic Alert Signal for Early Detection of Tissue Injuries in Patients: An Innovative Pressure Sensor Mattress
Abstract
1. Introduction
2. Literature Review
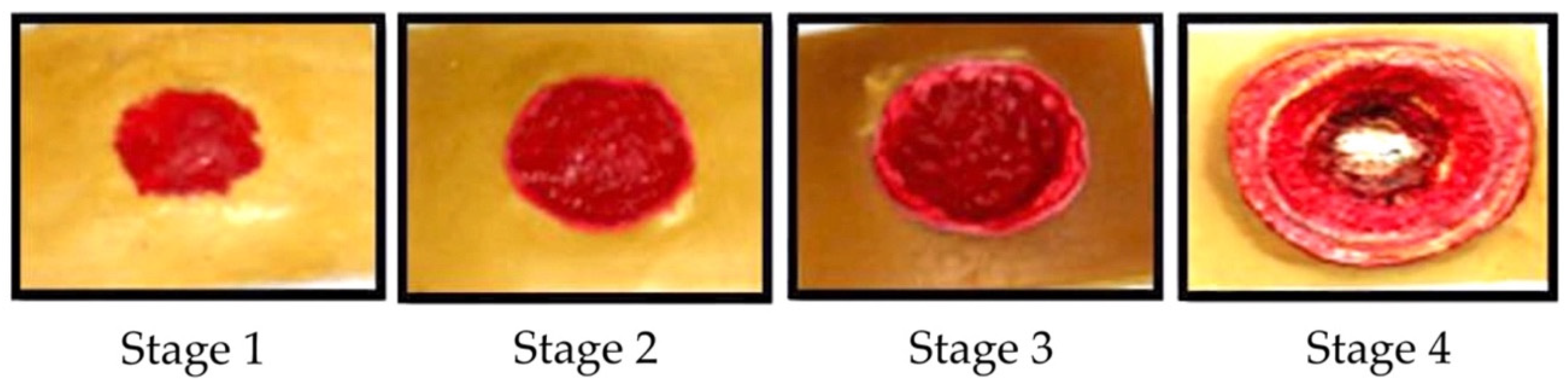
2.1. Tissue Injury Stages
- Lightly pigmented skin injuries (stage I). Such an injury is defined as the first visible change in the skin and is known as the ‘heralding sign’.
- Darkly pigmented skin injuries (stage II). This type of injury is defined as partial-thickness skin loss with an exposed dermis.
- Blanchable erythema injuries (stage III). This type of injury is defined as full-thickness skin loss, such as adipose, granulation tissue, and epibole.
- Pressure injury with oedema (stage IV). This injury is defined as full-thickness skin and tissue loss with exposure of directly palpable fascia, muscle, tendon, ligament, cartilage, and bone in the ulcer.
2.2. Tissue Injury Detection
2.3. Temperature Detection
2.4. Humidity Detection
3. Materials and Methods
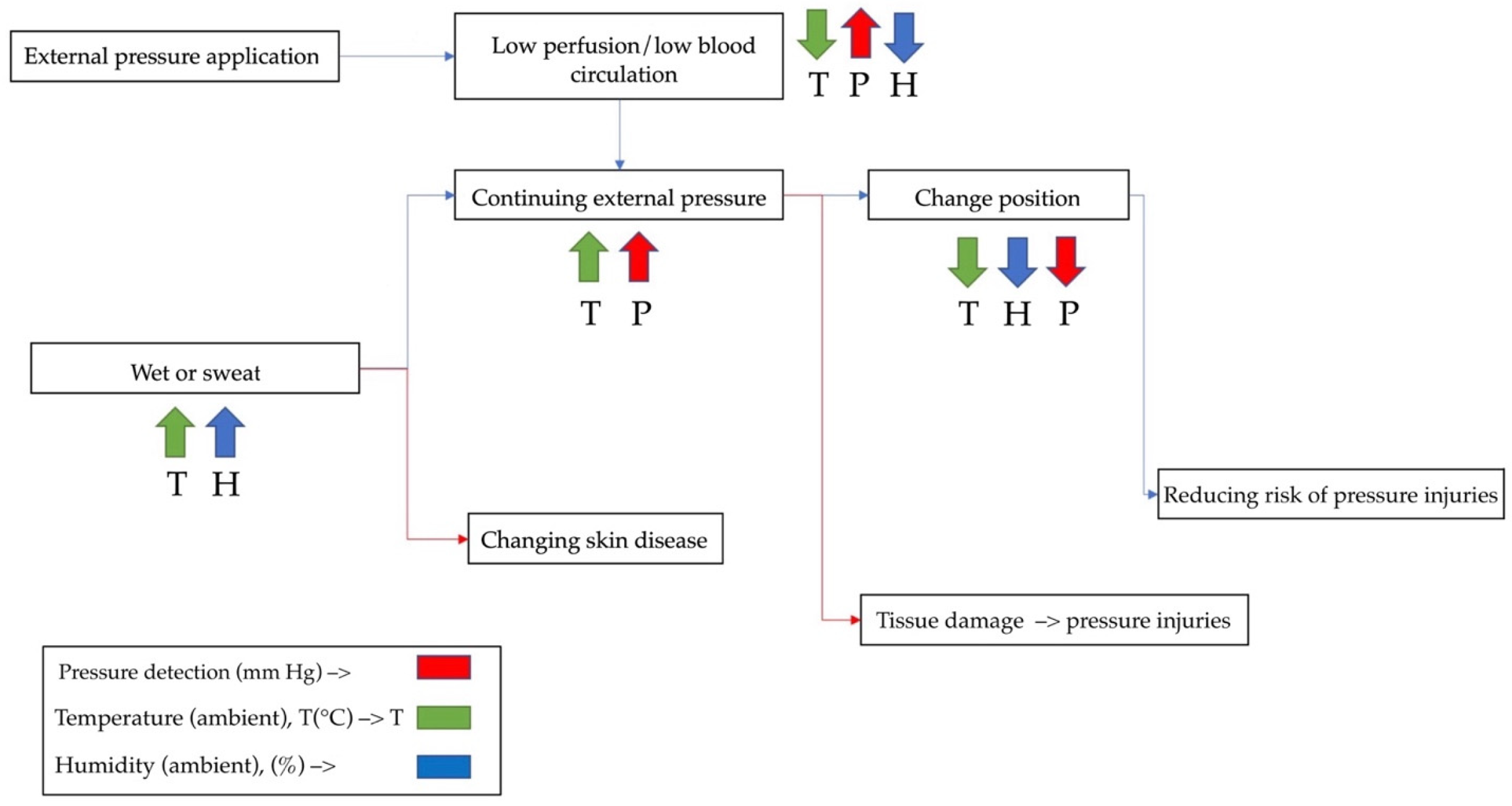
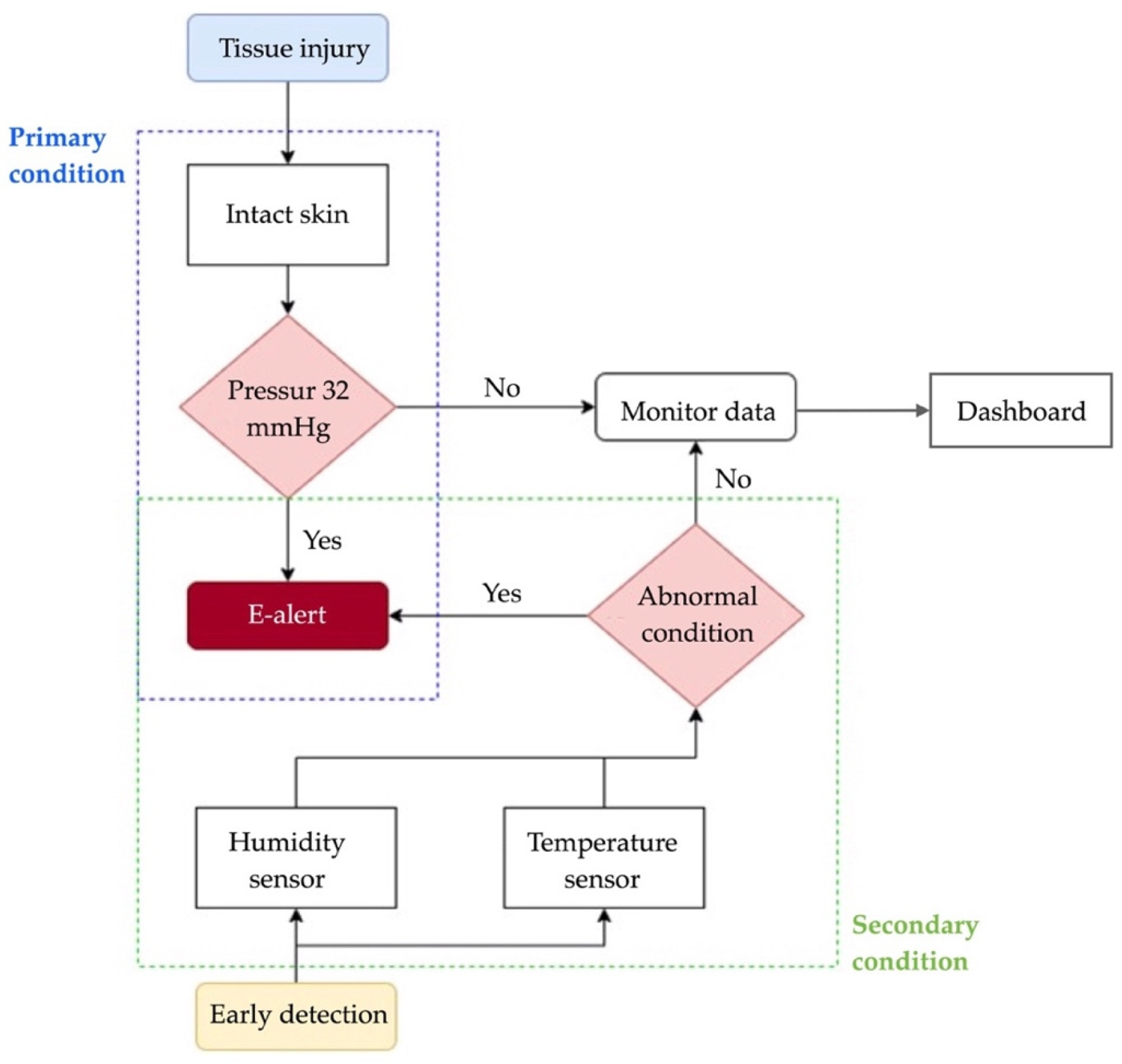
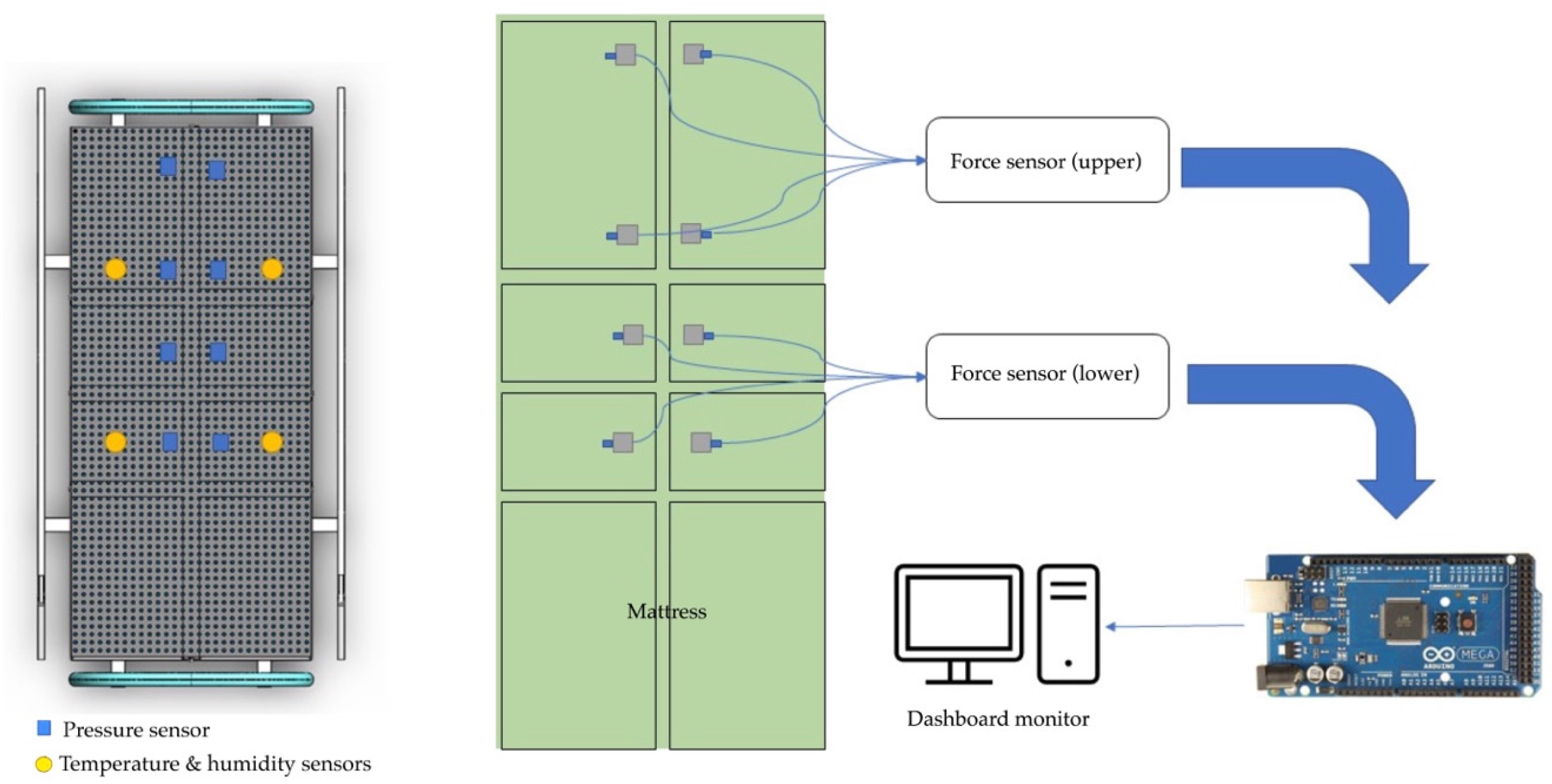
3.1. Detection Procedures
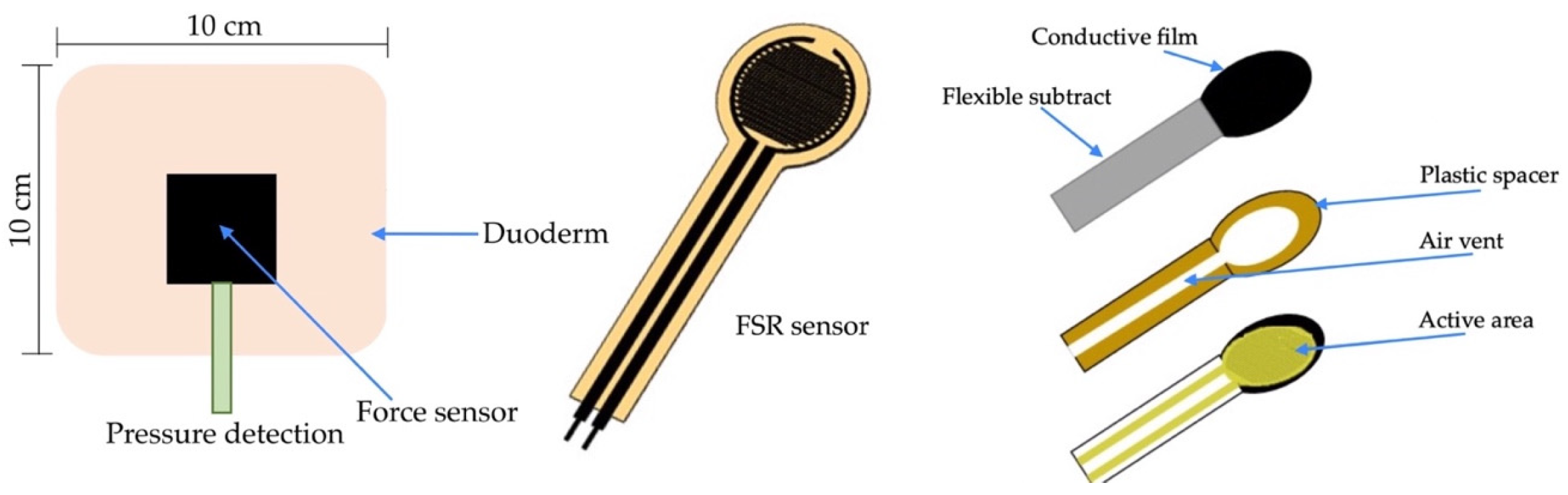
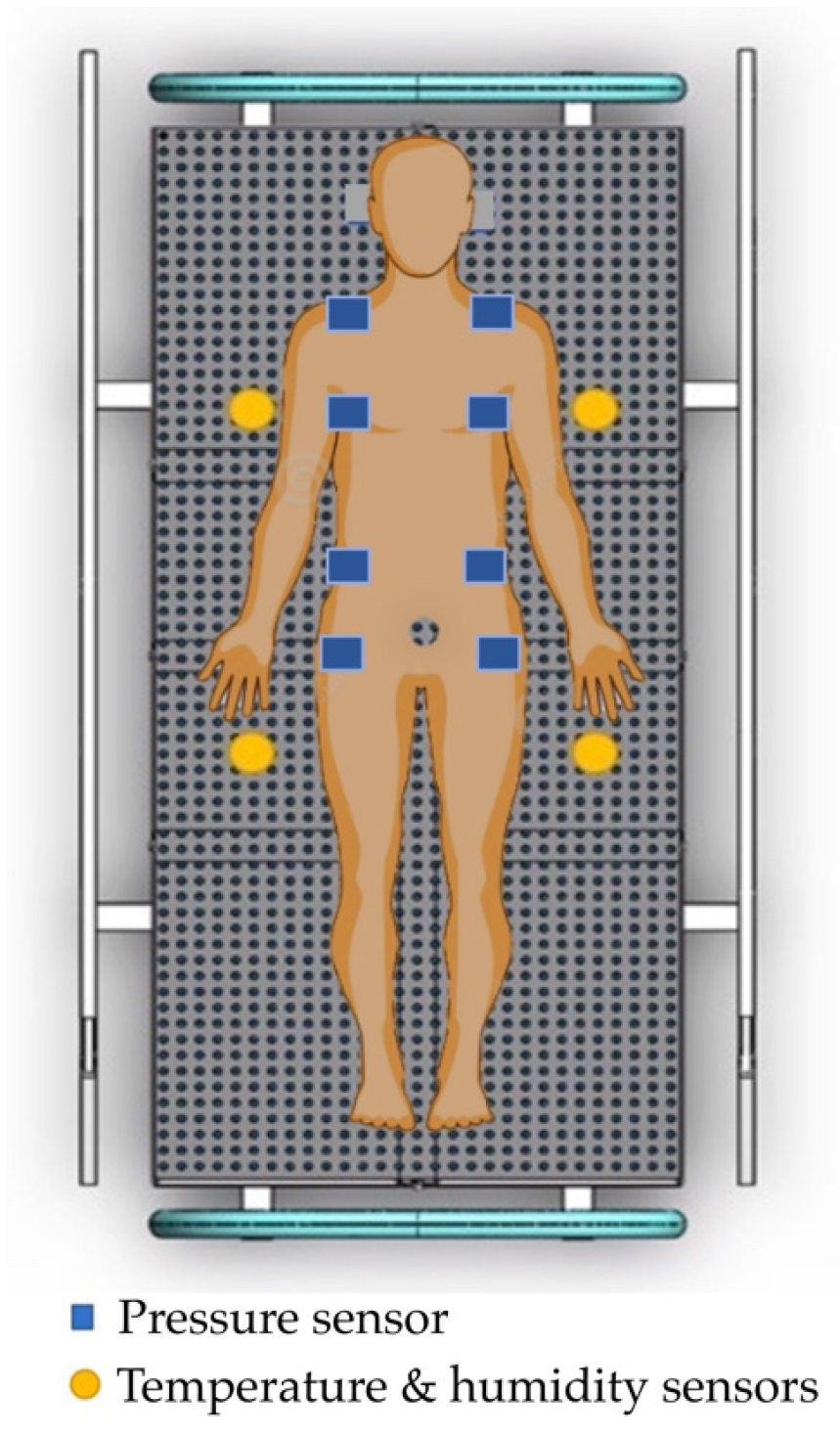
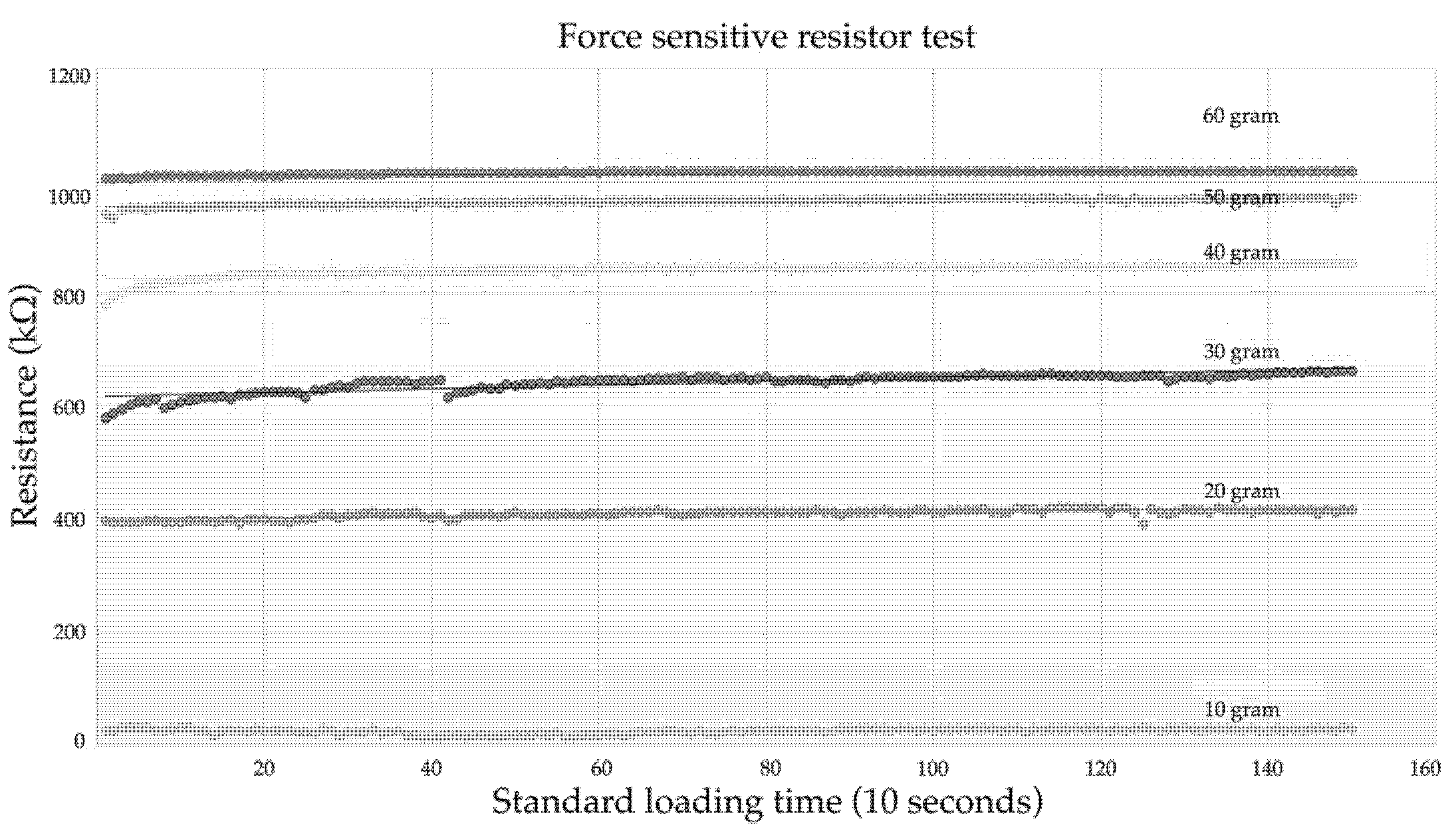
3.2. Pressure Sensors
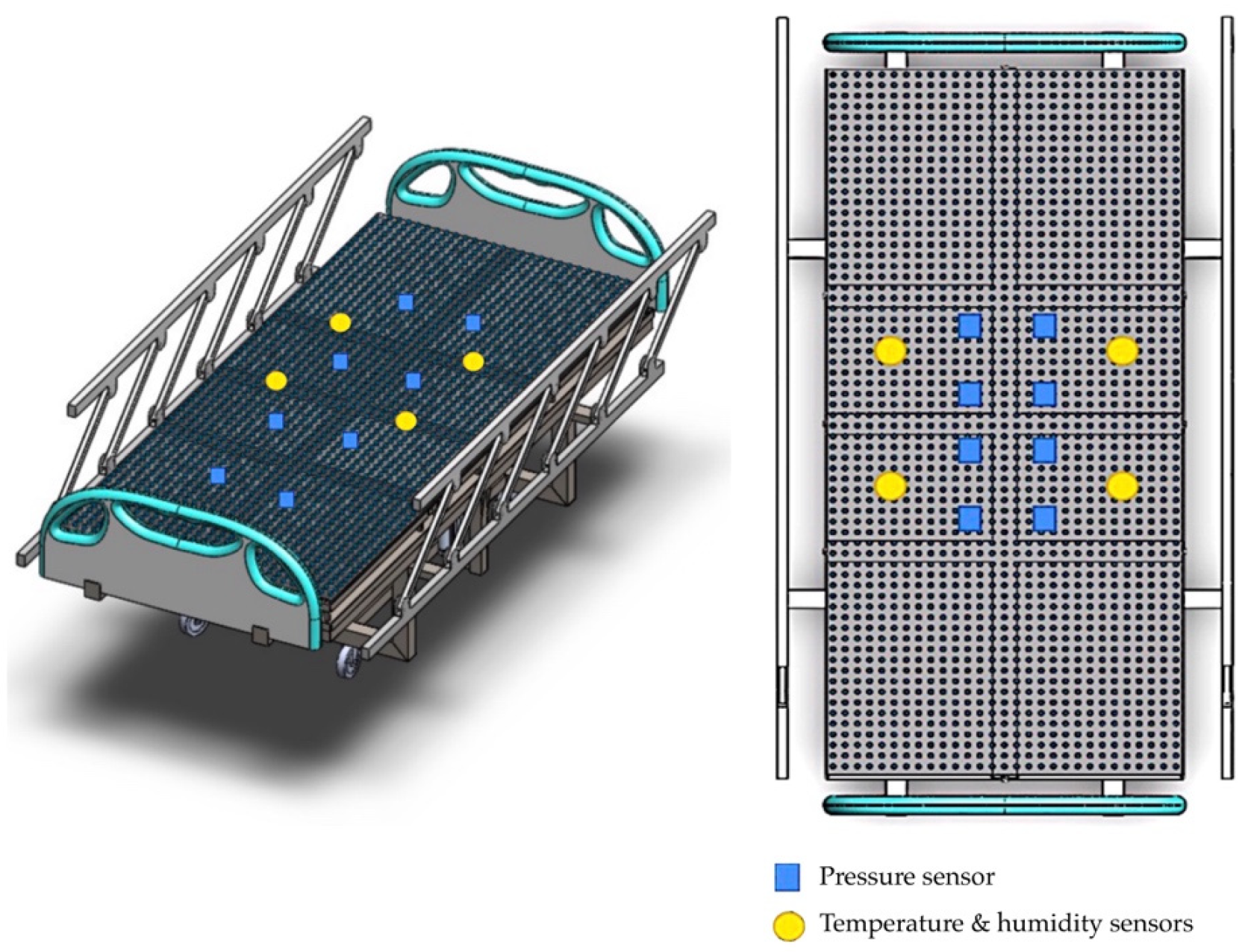
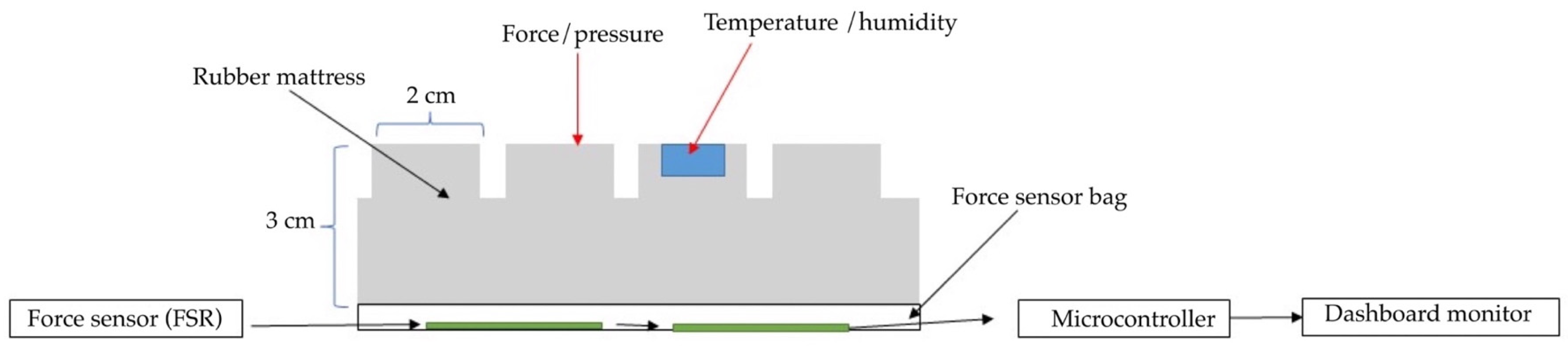
3.3. Developing an Innovative Pressure Sensor Mattress
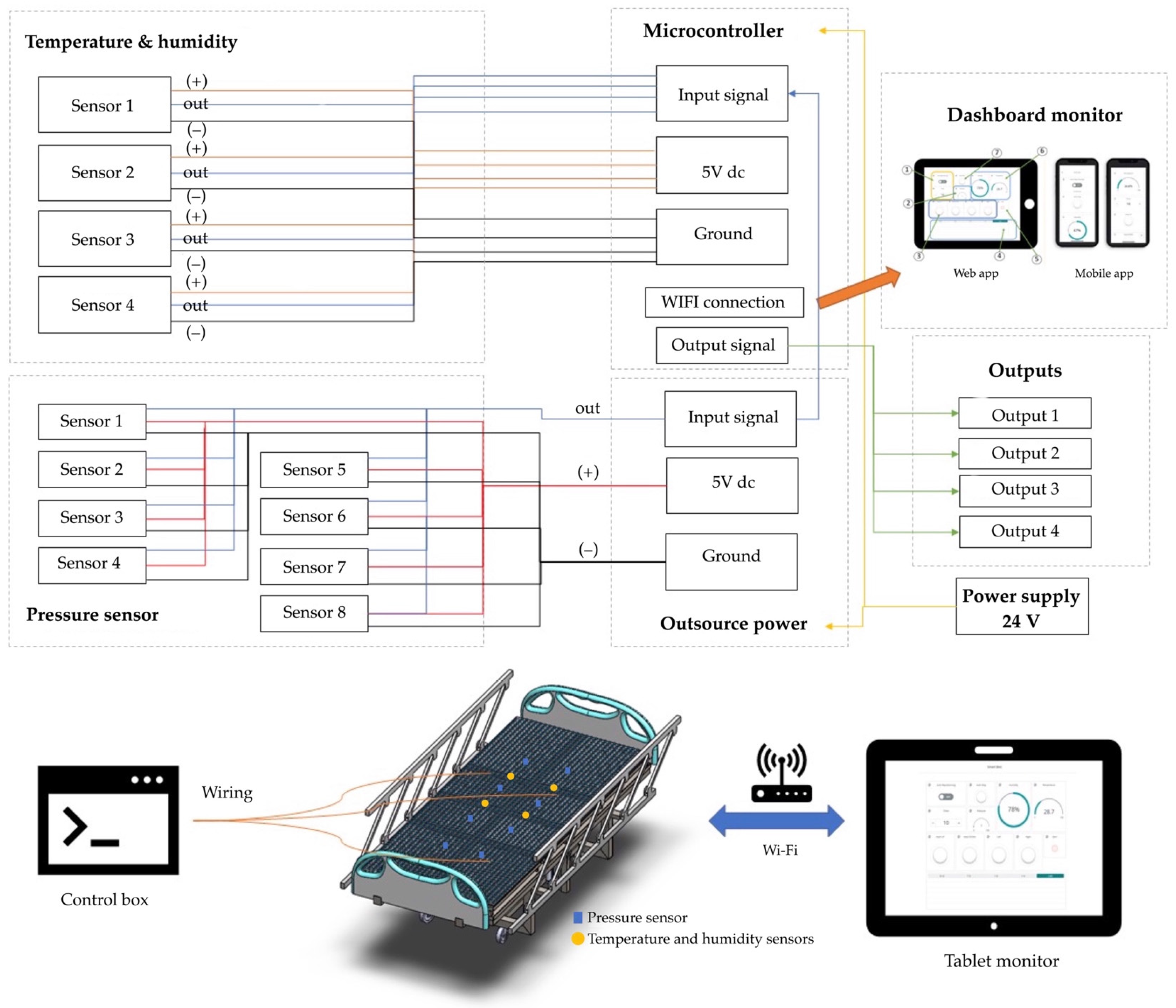
3.4. The Functional Sensing System
- The sensor is mounted on a hard surface;
- The contact pad is smaller than the sensitive area;
- The contact pad is mounted in the central array;
- Permanent loads are not applied to the sensor to avoid drift;
- The sensor is bent in the active area.
3.5. Control System
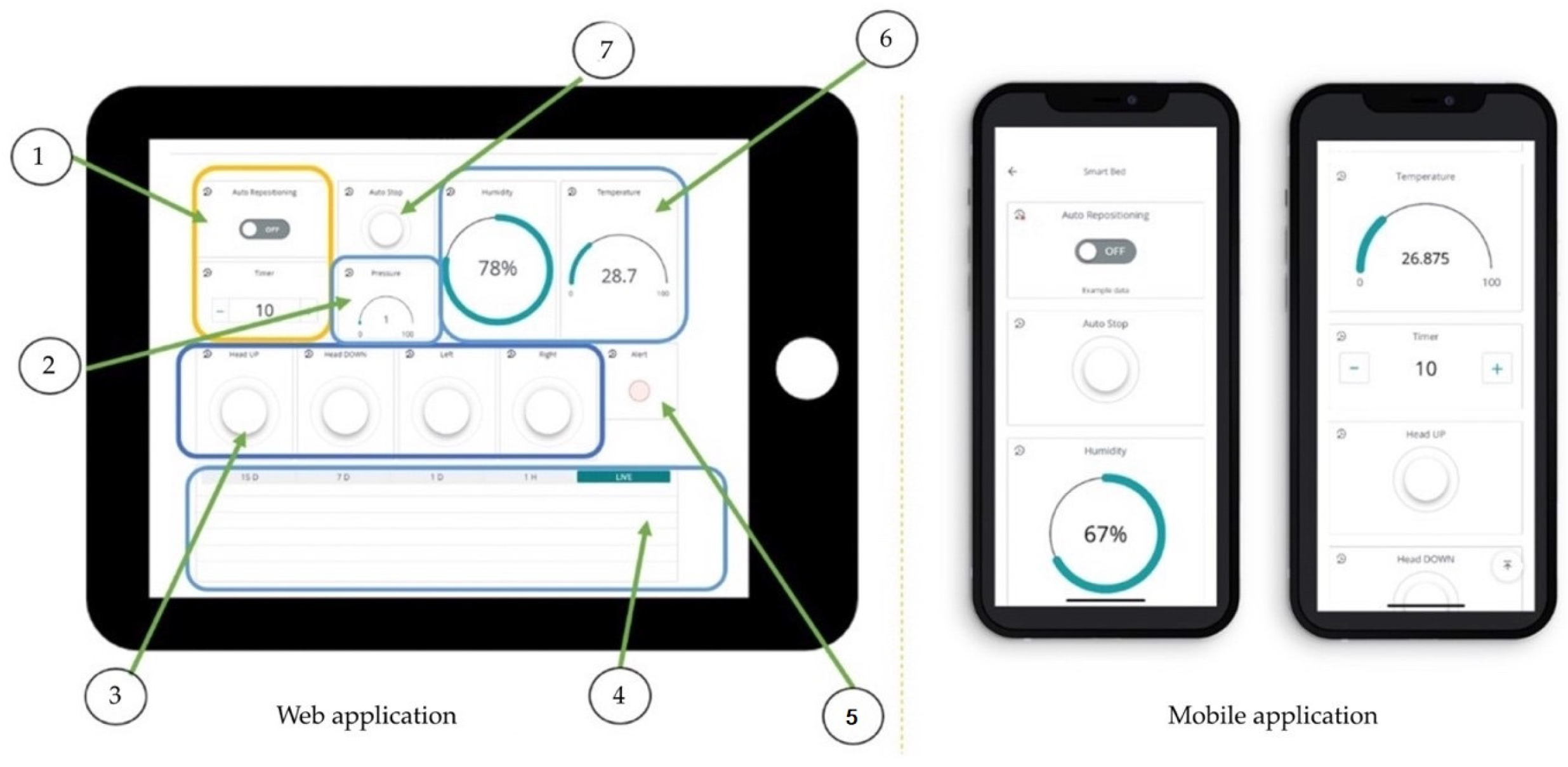
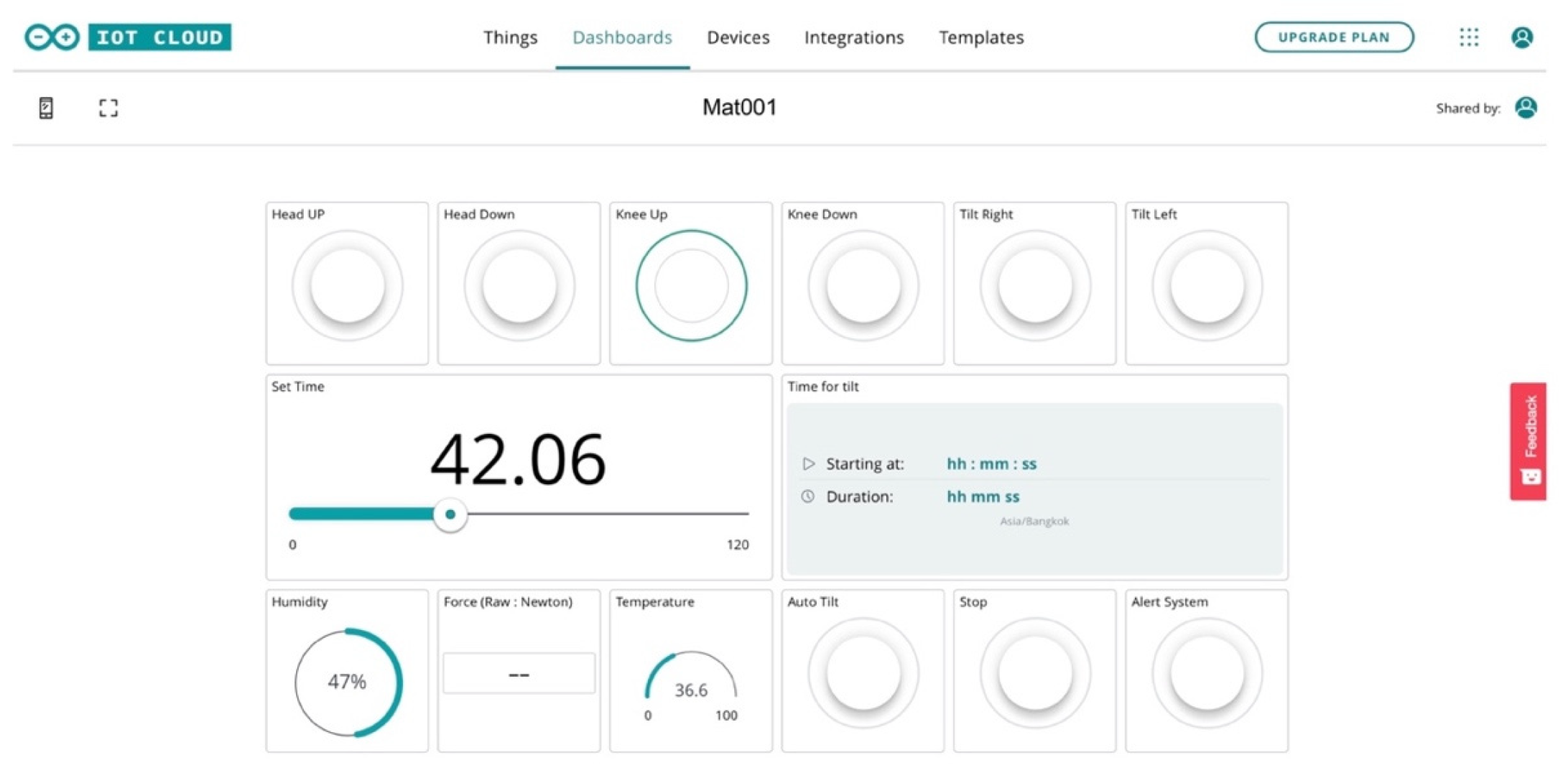
3.6. Dashboard Monitor
- ➀
- Real-time displays and reporting with command keypads ‘on’ the left and right after a specification time;
- ➁
- A display of the patient’s weight and surveillance alerts;
- ➂
- A flip command to control the screen;
- ➃
- A display of the real-time temperature and view in period;
- ➄
- A display of the magnitude of the force-sensor hazard when the pressure is over 32 mm Hg, with a red alert warning;
- ➅
- A display of the temperature and humidity values;
- ➆
- Keypad command (autos and manual control).
4. Results
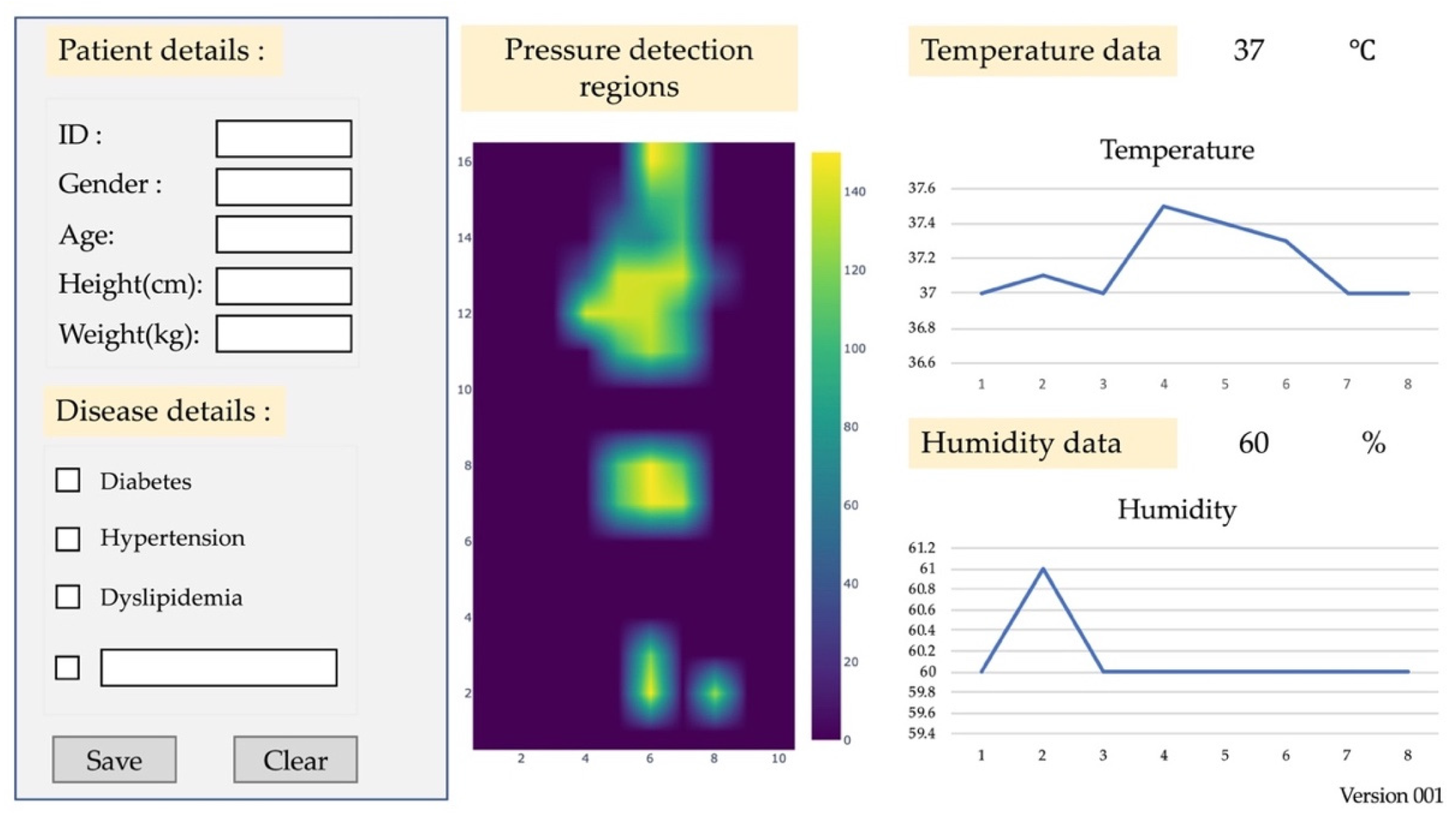
4.1. Patients with Tissue Injuries
4.2. Platform of Mattress
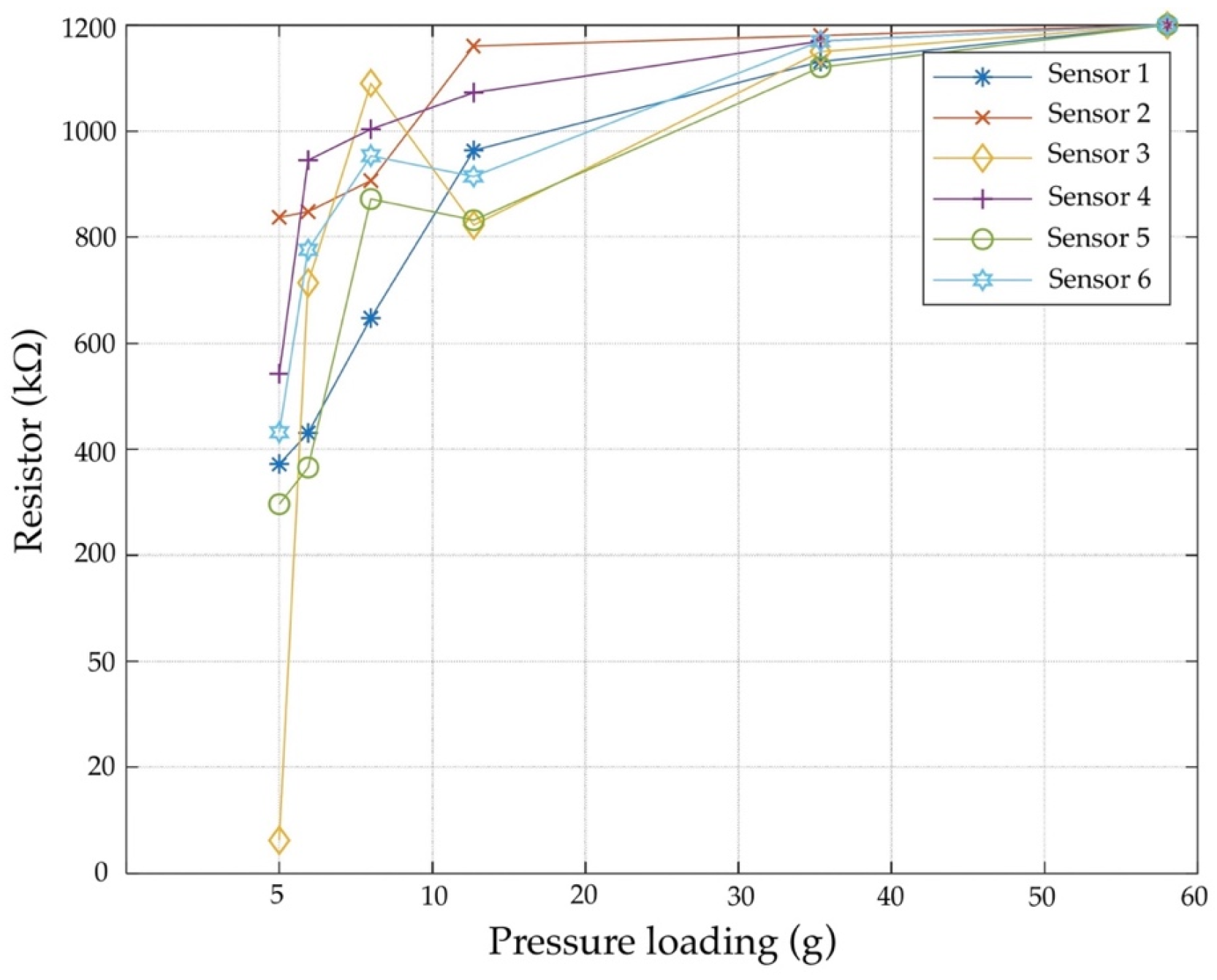
4.3. Pressure Sensor Test
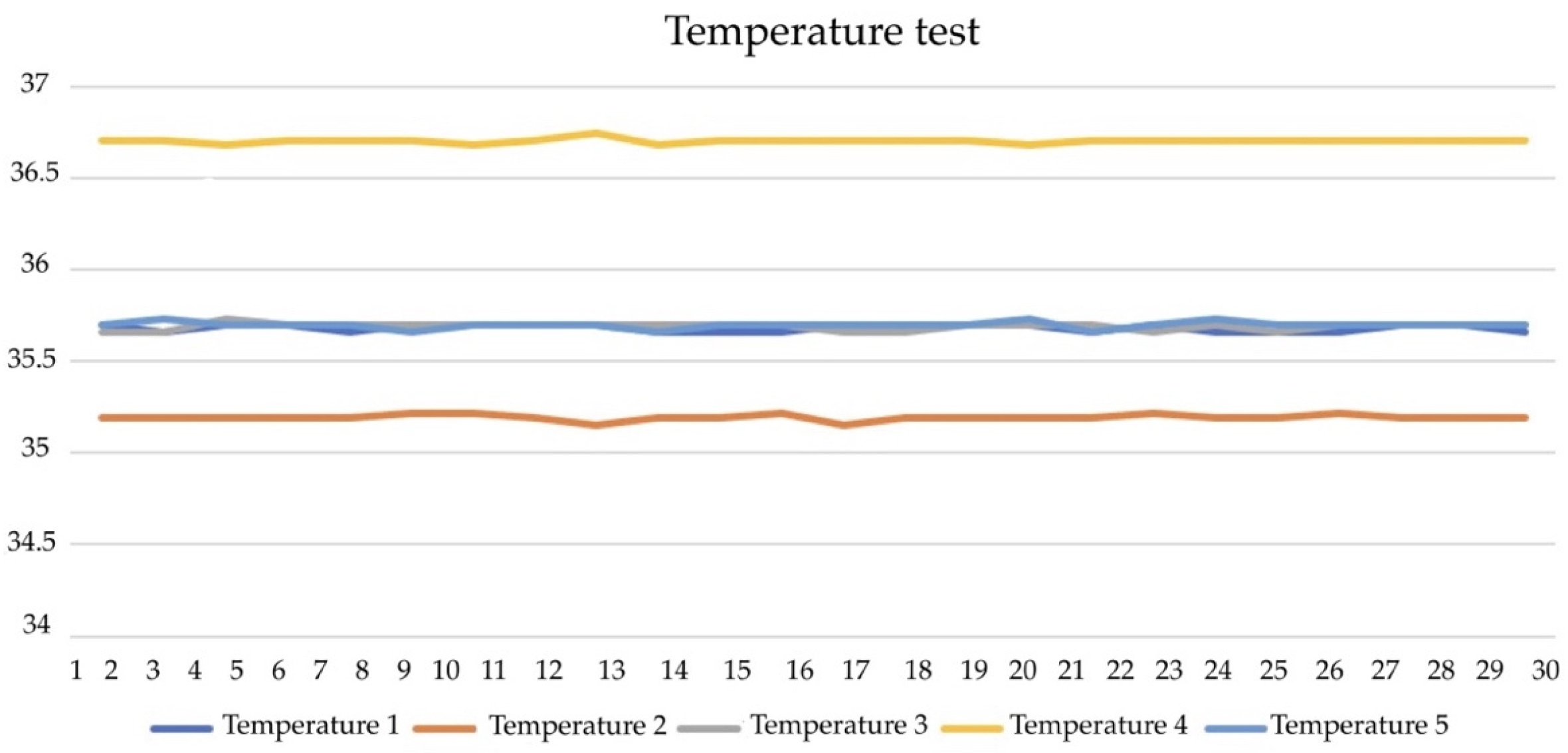
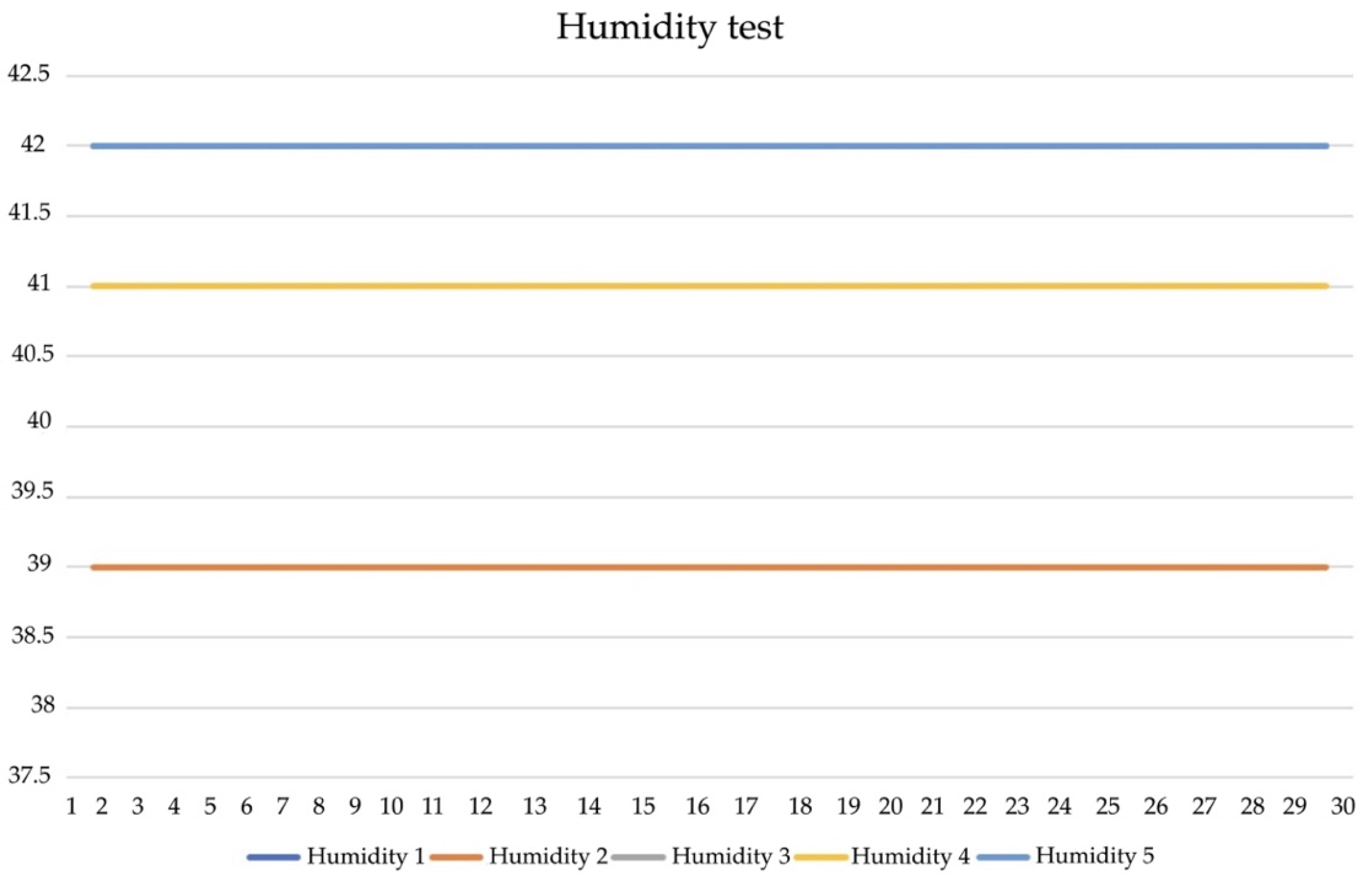
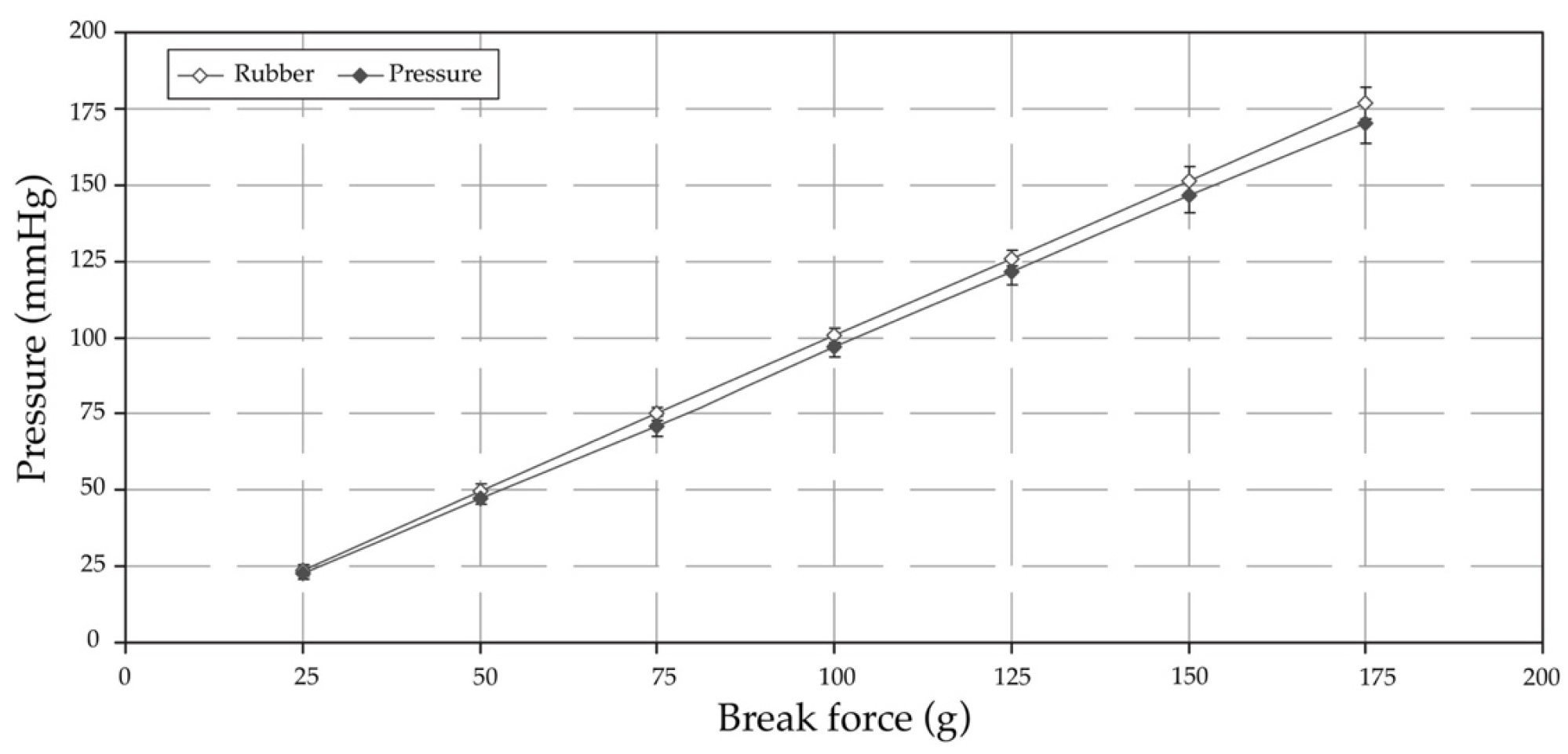
4.4. Temperture and Humdity Sensor Tests
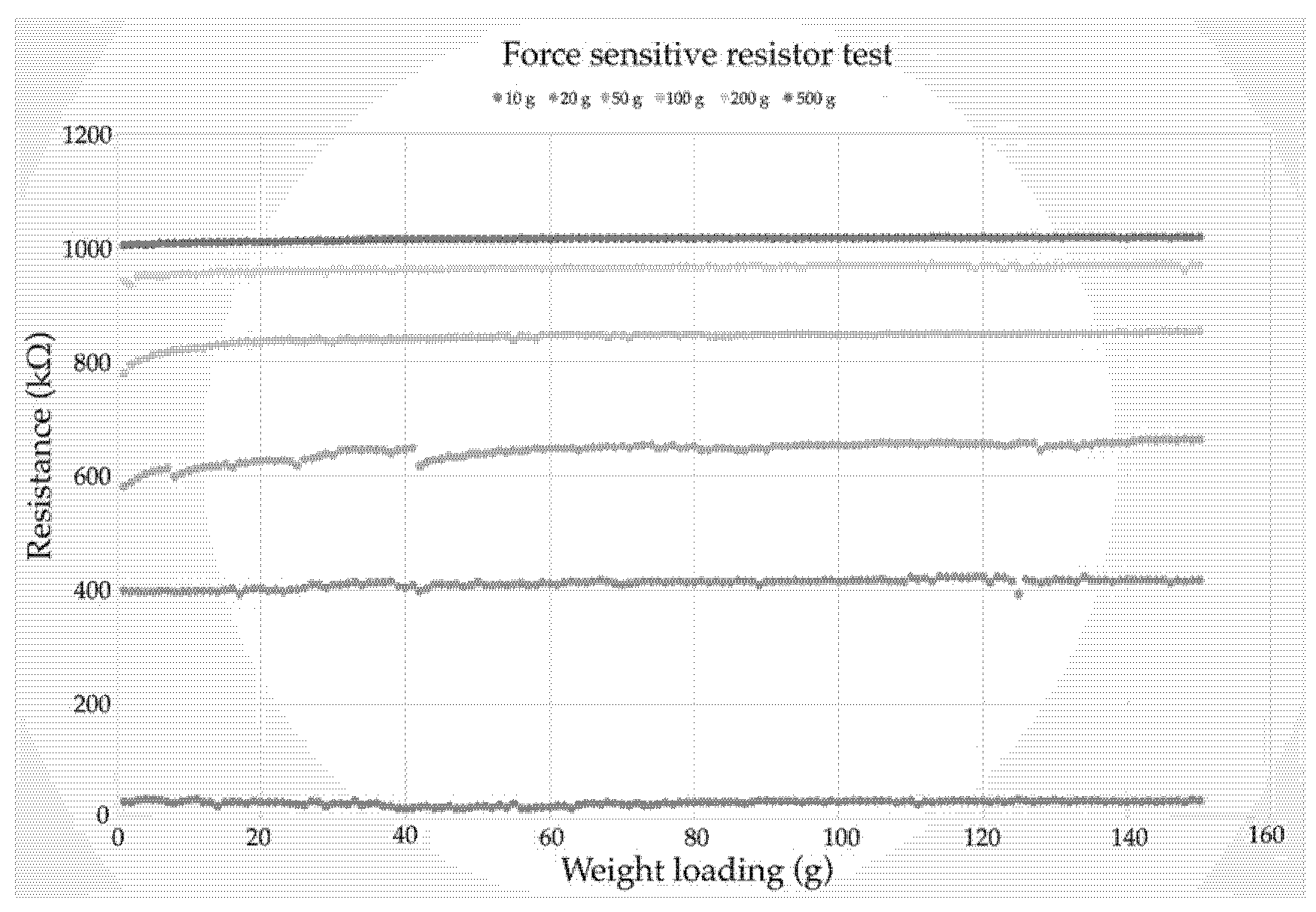
4.5. Force Sensor Test
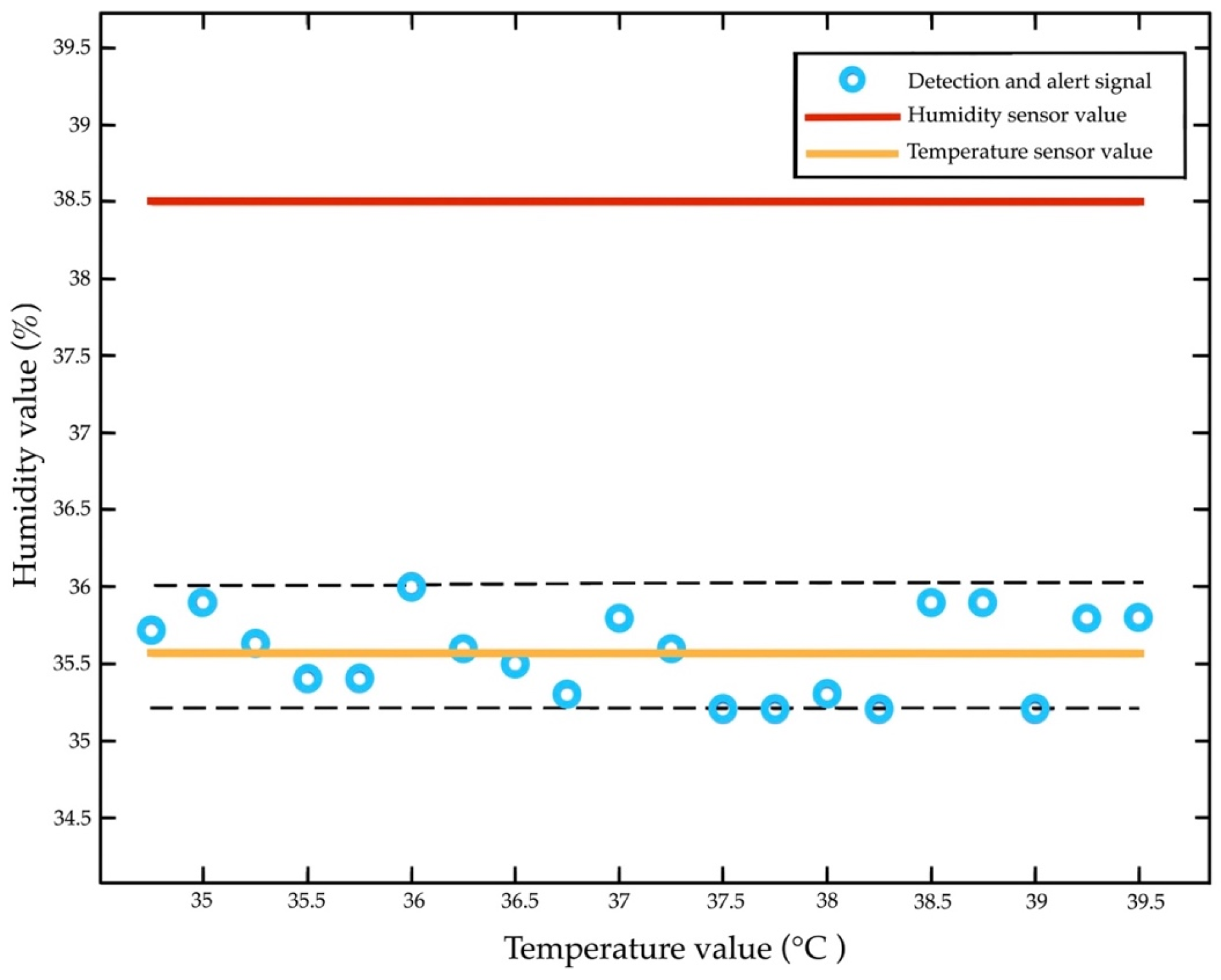
4.6. Static Test
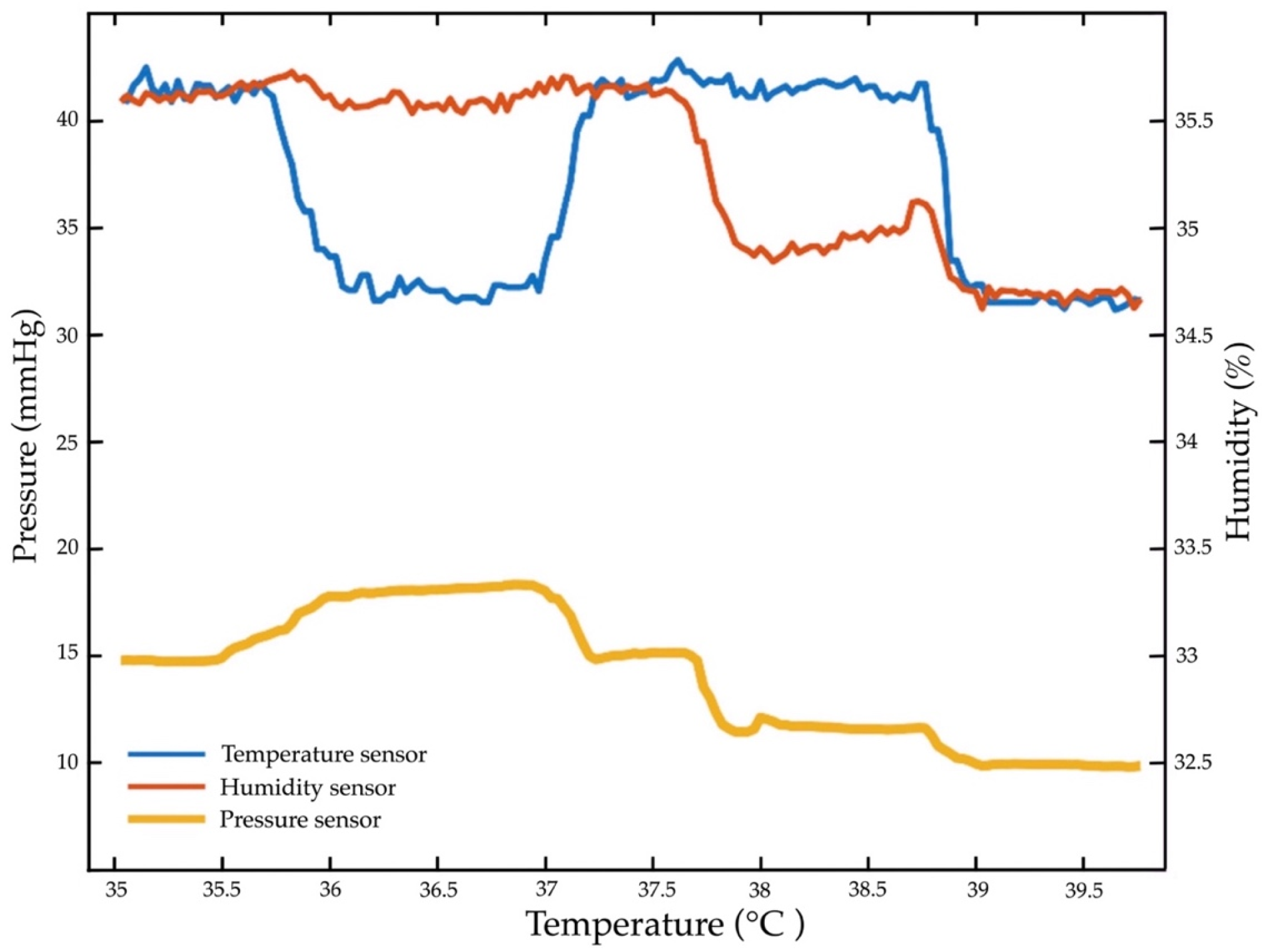
4.7. Repeated Temperature, Humidity, and Pressure Sensor Test
5. Discussion
5.1. Discussion with Rsults
5.2. Practical Diagnostics
5.3. Innovation Device Contributions
6. Conclusions
Limitations and Future Direction
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kelechi, T.J. Commentary: Chronic tissue injury. J. Wound Ostomy Cont. Nurs. 2019, 46, 192–193. [Google Scholar] [CrossRef] [PubMed]
- Mamom, J. The effects of a community-based discharge-planning model for continuing pressure ulcer care on wound healing rates, nutritional status, and infection rates of elderly patients in Thailand. Songklanakarin J. Sci. Technol. 2017, 39, 341–346. [Google Scholar]
- Mamom, J.; Ruchiwit, M.; Hain, D. Strategies of repositioning for effective pressure ulcer prevention in immobilized patients in home-based palliative care: An integrative literature reviews. J. Med. Assoc. Thai. 2020, 103, 111–117. [Google Scholar]
- Shiferaw, W.S.; Aynalem, Y.A.; Akalu, T.Y. Prevalence of pressure ulcers among hospitalized adult patients in Ethiopia: A systematic review and meta-analysis. BMC Dermatol. 2020, 20, 15. [Google Scholar] [CrossRef] [PubMed]
- Triantafyllou, C.; Chorianopoulou, E.; Kourkouni, E.; Zaoutis, T.E.; Kourlaba, G. Prevalence, incidence, length of stay and cost of healthcare-acquired pressure ulcers in pediatric populations: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2021, 115, 103843. [Google Scholar] [CrossRef]
- Bates-Jensen, B.M.; McCreath, H.E.; Nakagami, G.; Patlan, A. Subepidermal moisture detection of heel pressure injury: The pressure ulcer detection study outcomes. Int. Wound J. 2018, 15, 297–309. [Google Scholar] [CrossRef] [PubMed]
- Bates-Jensen, B.M.; McCreath, H.E.; Pongquan, V. Subepidermal moisture is associated with early pressure ulcer damage in nursing home residents with dark skin tones: Pilot findings. J. Wound Ostomy Cont. Nurs. 2009, 36, 277–284. [Google Scholar] [CrossRef]
- Moghadas, H.; Mushahwar, V.K. Passive microwave resonant sensor for detection of deep tissue injuries. Actuators B Chem. 2018, 277, 69–77. [Google Scholar] [CrossRef]
- Gefen, A. The compression intensity index: A practical anatomical estimate of the biomechanical risk for a deep tissue injury. Technol. Health Care. 2008, 16, 141–149. [Google Scholar] [CrossRef] [PubMed]
- Loerakker, S.; Stekelenburg, A.; Strijkers, G.J.; Rijpkema, J.J.; Baaijens, F.P.; Bader, D.L.; Nicolay, K.; Oomens, C.W. Temporal effects of mechanical loading on deformation-induced damage in skeletal muscle tissue. Ann. Biomed. Eng. 2010, 38, 2577–2587. [Google Scholar] [CrossRef]
- Yıldız, A.; Karadağ, A.; Yıldız, A.; Çakar, V. Determination of the effect of prophylactic dressing on the prevention of skin injuries associated with personal protective equipments in health care workers during COVID-19 pandemic. J. Tissue Viability 2021, 30, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Mamom, J.; Daovisan, H. Telenursing: How do caregivers treat and prevent pressure injury in bedridden patients during the COVID-19 pandemic in Thailand? Using an embedded approach. J. Telemed. Telecare 2022, 1357633X221078485. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.; Yan, Y.; Bai, W.; Xue, Y.; Gamble, P.; Tian, L.; Kandela, I.; Haney, C.R.; Spees, W.; Lee, Y.; et al. Bioresorbable pressure sensors protected with thermally grown silicon dioxide for the monitoring of chronic diseases and healing processes. Nat. Biomed. Eng. 2019, 3, 37–46. [Google Scholar] [CrossRef] [PubMed]
- Bates-Jensen, B.M.; McCreath, H.E.; Harputlu, D.; Patlan, A. Reliability of the Bates-Jensen wound assessment tool for pressure injury assessment: The pressure ulcer detection study. Wound Repair Regen. 2019, 27, 386–395. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.; Kim, B.; Meng, E. Chronically implanted pressure sensors: Challenges and state of the field. Sensors 2014, 14, 20620–20644. [Google Scholar] [CrossRef]
- Bates-Jensen, B.M.; Reilly, S.; Hilliard, C.; Patton, D.; Moore, Z. Subepidermal moisture and pressure injury in a pediatric population: A prospective observational study. J. Wound Ostomy Cont. Nurs. 2020, 47, 329–335. [Google Scholar] [CrossRef]
- Gianino, E.; Miller, C.; Gilmore, J. Smart wound dressings for diabetic chronic wounds. Bioengineering 2018, 5, 51. [Google Scholar] [CrossRef] [PubMed]
- Hariri, A.; Chen, F.; Moore, C.; Jokerst, J.V. Noninvasive staging of pressure ulcers using photoacoustic imaging. Wound Repair Regen. 2019, 27, 488–496. [Google Scholar] [CrossRef]
- Jiang, G. Design challenges of implantable pressure monitoring system. Front. Neurosci. 2010, 4, 29. [Google Scholar] [CrossRef]
- Bader, D.L.; Worsley, P.R.; Gefen, A. Bioengineering considerations in the prevention of medical device-related pressure ulcers. Clin. Biomech. 2019, 67, 70–77. [Google Scholar] [CrossRef]
- Angulo-Urarte, A.; Wal, T.; Huveneers, S. Cell-cell junctions as sensors and transducers of mechanical forces. Biochim. Biophys. Acta Biomembr. 2020, 1862, 183316. [Google Scholar] [CrossRef] [PubMed]
- Qiu, K.; Zhao, Z.; Haghiashtiani, G.; Guo, S.Z.; He, M.; Su, R.; Zhu, Z.; Bhuiyan, D.B.; Murugan, P.; Meng, F.; et al. 3D printed organ models with physical properties of tissue and integrated sensors. Adv. Mater. Technol. 2018, 3, 1700235. [Google Scholar] [CrossRef] [PubMed]
- Silva, A.; Metrôlho, J.; Ribeiro, F.; Fidalgo, F.; Santos, O.; Dionisio, R. A review of intelligent sensor-based systems for pressure ulcer prevention. Computers 2022, 11, 6. [Google Scholar] [CrossRef]
- Arakawa, T. Recent research and developing trends of wearable sensors for detecting blood pressure. Sensors 2018, 18, 2772. [Google Scholar] [CrossRef] [PubMed]
- Moore, Z.; Patton, D.; Rhodes, S.L.; O’Connor, T. Subepidermal moisture (SEM) and bioimpedance: A literature review of a novel method for early detection of pressure-induced tissue damage (pressure ulcers). Int. Wound J. 2017, 14, 331–337. [Google Scholar] [CrossRef]
- Keller, B.P.; Schuurman, J.P.; Werken, C. Can near infrared spectroscopy measure the effect of pressure on oxygenation of sacral soft tissue? J. Wound Care 2006, 15, 213–217. [Google Scholar] [CrossRef]
- Malone, E.; Santos, G.S.; Holder, D.; Arridge, S. Multifrequency electrical impedance tomography using spectral constraints. IEEE Trans. Med. Imaging 2014, 33, 340–350. [Google Scholar] [CrossRef]
- Oliveira, A.L.; Moore, Z.; O’Connor, T.; Patton, D. Accuracy of ultrasound, thermography and subepidermal moisture in predicting pressure ulcers: A systematic review. J. Wound Care 2017, 26, 199–215. [Google Scholar] [CrossRef]
- Nakagami, G.; Schultz, G.; Gibson, D.J.; Phillips, P.; Kitamura, A.; Minematsu, T.; Miyagaki, T.; Hayashi, A.; Sasaki, S.; Sugama, J.; et al. Biofilm detection by wound blotting can predict slough development in pressure ulcers: A prospective observational study. Wound Repair Regen. 2017, 25, 131–138. [Google Scholar] [CrossRef]
- Fakhari, A.; Berkland, C. Applications and emerging trends of hyaluronic acid in tissue engineering, as a dermal filler and in osteoarthritis treatment. Acta Biomater. 2013, 9, 7081–7092. [Google Scholar] [CrossRef]
- Okonkwo, H.; Bryant, R.; Milne, J.; Molyneaux, D.; Sanders, J.; Cunningham, G.; Brangman, S.; Eardley, W.; Chan, G.K.; Mayer, B.; et al. A blinded clinical study using a subepidermal moisture biocapacitance measurement device for early detection of pressure injuries. Wound Repair Regen. 2020, 28, 364–374. [Google Scholar] [CrossRef] [PubMed]
- Budri, A.M.V.; Moore, Z.; Patton, D.; O’Connor, T.; Nugent, L.; Mc Cann, A.; Avsar, P. Impaired mobility and pressure ulcer development in older adults: Excess movement and too little movement-two sides of the one coin? J. Clin. Nurs. 2020, 29, 2927–2944. [Google Scholar] [CrossRef] [PubMed]
- Semedo, P.; Wang, P.M.; Andreucci, T.H.; Cenedeze, M.A.; Teixeira, V.P.; Reis, M.A.; Pacheco-Silva, A.; Câmara, N.O. Mesenchymal stem cells ameliorate tissue damages triggered by renal ischemia and reperfusion injury. Transplant. Proc. 2007, 39, 421–423. [Google Scholar] [CrossRef] [PubMed]
- Bortolotti, P.; Faure, E.; Kipnis, E. Inflammasomes in tissue damages and immune disorders after trauma. Front. Immunol. 2018, 9, 1900. [Google Scholar] [CrossRef]
- Maver, T.; Maver, U.; Kleinschek, K.S.; Raščan, I.M.; Smrke, D.M. Advanced therapies of skin injuries. Wien. Klin. Wochenschr. 2015, 127, 187–198. [Google Scholar] [CrossRef]
- Edsberg, L.E.; Black, J.M.; Goldberg, M.; McNichol, L.; Moore, L.; Sieggreen, M. Revised national pressure ulcer advisory panel pressure injury staging system: Revised pressure injury staging system. J. Wound Ostomy Cont. Nurs. 2016, 43, 585–597. [Google Scholar] [CrossRef]
- Aoi, N.; Yoshimura, K.; Kadono, T.; Nakagami, G.; Iizuka, S.; Higashino, T.; Araki, J.; Koshima, I.; Sanada, H. Ultrasound assessment of deep tissue injury in pressure ulcers: Possible prediction of pressure ulcer progression. Plast. Reconstr. Surg. 2009, 124, 540–550. [Google Scholar] [CrossRef]
- Li, Z.; Lin, F.; Thalib, L.; Chaboyer, W. Global prevalence and incidence of pressure injuries in hospitalised adult patients: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2020, 105, 103546. [Google Scholar] [CrossRef]
- Kolluru, C.; Williams, M.; Chae, J.; Prausnitz, M.R. Recruitment and collection of dermal interstitial fluid using a microneedle patch. Adv. Healthc. Mater. 2019, 8, e1801262. [Google Scholar] [CrossRef]
- Kokate, J.Y.; Leland, K.J.; Held, A.M.; Hansen, G.L.; Kveen, G.L.; Johnson, B.A.; Wilke, M.S.; Sparrow, E.M.; Iaizzo, P.A. Temperature-modulated pressure ulcers: A porcine model. Arch. Phys. Med. Rehabil. 1995, 76, 666–673. [Google Scholar] [CrossRef]
- Kuzubasoglu, B.A.; Bahadir, S.K. Flexible temperature sensors: A review. Sens. Actuator A Phys. 2020, 315, 112282. [Google Scholar] [CrossRef]
- Li, Q.; Zhang, L.N.; Tao, X.M.; Ding, X. Review of flexible temperature sensing networks for wearable physiological monitoring. Adv. Healthc. Mater. 2017, 6, 1601371. [Google Scholar] [CrossRef] [PubMed]
- Lu, D.; Yan, Y.; Avila, R.; Kandela, I.; Stepien, I.; Seo, M.H.; Bai, W.; Yang, Q.; Li, C.; Haney, C.R.; et al. Bioresorbable, wireless, passive sensors as temporary implants for monitoring regional body temperature. Adv. Healthc. Mater. 2020, 9, e2000942. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.-H.; Chen, Y.-C.; Cheng, K.-S.; Yu, P.-J.; Wang, J.-L.; Ko, N.-Y. Higher periwound temperature associated with wound healing of pressure ulcers detected by infrared thermography. J. Clin. Med. 2021, 10, 2883. [Google Scholar] [CrossRef]
- Padula, W.V.; Gibbons, R.D.; Valuck, R.J.; Makic, M.B.; Mishra, M.K.; Pronovost, P.J.; Meltzer, D.O. Are evidence-based practices associated with effective prevention of hospital-acquired pressure ulcers in US academic medical centers? Med. Care 2016, 54, 512–518. [Google Scholar] [CrossRef]
- Jiang, X.; Hou, X.; Dong, N.; Deng, H.; Wang, Y.; Ling, X.; Guo, H.; Zhang, L.; Cai, F. Skin temperature and vascular attributes as early warning signs of pressure injury. J. Tissue Viability 2020, 29, 258–263. [Google Scholar] [CrossRef]
- Tang, W.; Bhushan, B.; Ge, S. Friction, adhesion and durability and influence of humidity on adhesion and surface charging of skin and various skin creams using atomic force microscopy. J. Microsc. 2010, 239, 99–116. [Google Scholar] [CrossRef]
- Kim, C.G.; Park, S.; Ko, J.W.; Jo, S. The relationship of subepidermal moisture and early stage pressure injury by visual skin assessment. J. Tissue Viability 2018, 27, 130–134. [Google Scholar] [CrossRef]
- Yusuf, S.; Okuwa, M.; Shigeta, Y.; Dai, M.; Iuchi, T.; Rahman, S.; Usman, A.; Kasim, S.; Sugama, J.; Nakatani, T.; et al. Microclimate and development of pressure ulcers and superficial skin changes. Int. Wound J. 2015, 12, 40–46. [Google Scholar] [CrossRef]
- Schwartz, D.; Magen, Y.K.; Levy, A.; Gefen, A. Effects of humidity on skin friction against medical textiles as related to prevention of pressure injuries. Int. Wound J. 2018, 15, 866–874. [Google Scholar] [CrossRef]
- Gefen, A.; Gershon, S. An observational, prospective cohort pilot study to compare the use of subepidermal moisture measurements versus ultrasound and visual skin assessments for early detection of pressure injury. Ostomy Wound Manag. 2018, 64, 12–27. [Google Scholar] [CrossRef]
- Rodriguez, A.M.; Nakhle, J.; Griessinger, E.; Vignais, M.L. Intercellular mitochondria trafficking highlighting the dual role of mesenchymal stem cells as both sensors and rescuers of tissue injury. Cell Cycle 2018, 17, 712–721. [Google Scholar] [CrossRef] [PubMed]
- Gao, L.; Yu, J.; Li, Y.; Wang, P.; Shu, J.; Deng, X.; Li, L. An ultrahigh sensitive paper-based pressure sensor with intelligent thermotherapy for skin-integrated electronics. Nanomaterials 2020, 10, 2536. [Google Scholar] [CrossRef] [PubMed]
- Defloor, T.; Grypdonck, M.H. Do pressure relief cushions really relieve pressure? West. J. Nurs. Res. 2000, 22, 335–350. [Google Scholar] [CrossRef]
- Minami, K.; Kokubo, Y.; Maeda, I.; Hibino, S. A flexible pressure sensor could correctly measure the depth of chest compression on a mattress. Am. J. Emerg. Med. 2016, 34, 899–902. [Google Scholar] [CrossRef]
- Hudec, R.; Matúška, S.; Kamencay, P.; Benco, M. A smart IoT system for detecting the position of a lying person using a novel textile pressure sensor. Sensors 2021, 21, 206. [Google Scholar] [CrossRef]
- Lee, K.-H.; Kwon, Y.-E.; Lee, H.; Lee, Y.; Seo, J.; Kwon, O.; Kang, S.-W.; Lee, D. Active body pressure relief system with time-of-flight optical pressure sensors for pressure ulcer prevention. Sensors 2019, 19, 3862. [Google Scholar] [CrossRef]
- Wong, H.; Kaufman, J.; Baylis, B.; Conly, J.M.; Hogan, D.B.; Stelfox, H.T.; Southern, D.A.; Ghali, W.A.; Ho, C.H. Efficacy of a pressure-sensing mattress cover system for reducing interface pressure: Study protocol for a randomized controlled trial. Trials 2015, 16, 434. [Google Scholar] [CrossRef]
- Chai, C.Y.; Sadou, O.; Worsley, P.R.; Bader, D.L. Pressure signatures can influence tissue response for individuals supported on an alternating pressure mattress. J. Tissue Viability 2017, 26, 180–188. [Google Scholar] [CrossRef]
- Majerus, S.J.A.; Fletter, P.C.; Ferry, E.K.; Zhu, H.; Gustafson, K.J.; Damaser, M.S. Suburothelial bladder contraction detection with implanted pressure sensor. PLoS ONE 2017, 12, e0168375. [Google Scholar] [CrossRef]
- Malmsjö, M.; Ingemansson, R.; Martin, R.; Huddleston, E. Negative-pressure wound therapy using gauze or open-cell polyurethane foam: Similar early effects on pressure transduction and tissue contraction in an experimental porcine wound model. Wound Repair Regen. 2009, 17, 200–205. [Google Scholar] [CrossRef] [PubMed]
- Aloweni, F.A.B.; Ang, S.Y.; Chang, Y.Y.; Ng, X.P.; Teo, K.Y.; Choh, A.C.L.; Goh, I.H.Q.; Lim, S.H. Evaluation of infrared technology to detect category I and suspected deep tissue injury in hospitalised patients. J. Wound Care 2019, 28, S9–S16. [Google Scholar] [CrossRef] [PubMed]
- Mamom, J.; Daovisan, H. Repositioning mattress: How a lateral tilt position reshapes the prevention of pressure ulcers in bedridden patients. J. Med. Eng. Technol. 2022, 8, 658–669. [Google Scholar] [CrossRef]
- Pickham, D.; Berte, N.; Pihulic, M.; Valdez, A.; Mayer, B.; Desai, M. Effect of a wearable patient sensor on care delivery for preventing pressure injuries in acutely ill adults: A pragmatic randomized clinical trial (LS-HAPI study). Int. J. Nurs. Stud. 2018, 80, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Mamom, J.; Rungroungdouyboon, B.; Chuanasa, J. Enhancing the quality of long-term patient care by use of the innovative “electrical bed-turning system” for the prevention of pressure injuries: A pilot study. Sci. Technol. Asia 2022, 27, 128–135. [Google Scholar]
- Redon, P.; Shahzad, A.; Iqbal, T.; Wijns, W. Development of a new detection algorithm to identify acute coronary syndrome using electrochemical biosensors for real-world long-term monitoring. Bioengineering 2021, 8, 28. [Google Scholar] [CrossRef]
| No. | Internal Factors | External Factors | PI Risk | PI Incidence | PI Alert | ||||
|---|---|---|---|---|---|---|---|---|---|
| Gender | Age | Disease | Pressure (mmHg) | Humidity (%) | °C | ||||
| 1 | Male | 60 | DM + HT | 32 | 30 | 37.2 | High | No | Alert |
| 2 | Female | 58 | DM + HT+DLP | 30 | 20 | 36.7 | No | No | Normal |
| 3 | Male | 75 | DM + HT+DLP+AF | 30 | 40 | 36.5 | No | No | Beware |
| 4 | Female | 88 | DM + HT+DLP | 30 | 50 | 36.7 | Moderate | No | Alert |
| 5 | Female | 90 | DM + HT+DLP | 34 | 30 | 37.1 | High | No | Alert |
| 6 | Male | 60 | DM + HT | 32 | 30 | 36.8 | High | No | Alert |
| 7 | Female | 58 | DM + HT | 25 | 20 | 36.7 | No | No | Normal |
| 8 | Male | 75 | DM + HT + DLP + AF | 30 | 20 | 37.2 | No | No | Beware |
| 9 | Female | 76 | DM + HT + DLP | 32 | 40 | 36.6 | High | No | Alert |
| 10 | Female | 90 | DM + HT + DLP | 34 | 30 | 36.5 | High | No | Alert |
| 11 | Female | 56 | DM + HT | 30 | 20 | 36.6 | No | No | Beware |
| 12 | Male | 48 | DM + HT + DLP | 34 | 30 | 36.5 | Moderate | No | Alert |
| 13 | Male | 66 | DM + HT + DLP | 34 | 40 | 36.5 | High | No | Alert |
| 14 | Female | 59 | DM + HT | 35 | 40 | 37.1 | High | No | Alert |
| 15 | Female | 66 | DM + HT + DLP | 35 | 20 | 37.2 | High | No | Alert |
| No. | Internal Factors | External Factors | PI Risk | PI Incidence | ||||
|---|---|---|---|---|---|---|---|---|
| Gender | Age | Disease | Pressure (mmHg) | Humidity (%) | °C | |||
| 1 | Male | 63 | DM + HT + DLP + AF | 35 | 40 | 37.1 | High | Yes |
| 2 | Female | 58 | DM + HT | 25 | 30 | 36.3 | No | No |
| 3 | Male | 48 | DM + HT + DLP | 31 | 35 | 37.1 | Low | No |
| 4 | Male | 66 | DM + HT + DLP | 34 | 40 | 36.9 | High | Yes |
| 5 | Female | 59 | DM + HT | 34 | 30 | 37 | High | Yes |
| 6 | Male | 66 | DM + HT + DLP | 35 | 40 | 36.6 | High | Yes |
| 7 | Female | 54 | DM + HT | 30 | 20 | 36.8 | No | No |
| 8 | Male | 65 | DM + HT + DLP + AF | 31 | 20 | 37.2 | Moderate | Yes |
| 9 | Female | 70 | DM + HT + DLP | 30 | 50 | 36.6 | Moderate | Yes |
| 10 | Female | 82 | DM + HT + DLP | 34 | 30 | 37.1 | High | Yes |
| 11 | Female | 53 | DM + HT | 30 | 20 | 36.6 | No | No |
| 12 | Male | 50 | DM + HT + DLP | 30 | 20 | 36.7 | No | Yes |
| 13 | Male | 63 | DM + HT + DLP | 34 | 20 | 36.9 | High | Yes |
| 14 | Female | 61 | DM + HT | 34 | 40 | 37.2 | High | Yes |
| 15 | Female | 64 | DM + HT + DLP | 32 | 40 | 37.3 | High | Yes |
| Body Area | Detected | ||||
|---|---|---|---|---|---|
| Supine | Left-Lying | Right-Lying | Recall | ||
| Original | Supine | 35 | 1 | 4 | 0.748 |
| Left-lying | 9 | 27 | 0 | 0.719 | |
| Right-lying | 12 | 1 | 23 | 0.552 | |
| Precision | – | 0.760 | 0.954 | 0.725 | – |
| Temperature | Humidity | ||||
|---|---|---|---|---|---|
| Normal T (°C) | TT (Ω) | RTD (Ω) | Normal (%) | RH (%) | Sensor (Ω) |
| 10 | 1038.8 ± 0.1 | 240.5 ± 0.0 | 10 | 7.5 ± 0.5 | 12,514.9 ± 11.2 |
| 15 | 1057.4 ± 0.1 | 244.2 ± 0.1 | 20 | 17.4 ± 0.6 | 12,689.8 ± 1.6 |
| 20 | 1076.2 ± 0.1 | 248.1 ± 0.1 | 30 | 27.2 ± 0.2 | 12,827.2 ± 2.6 |
| 25 | 1096.3 ± 0.2 | 252.3 ± 0.2 | 40 | 36.5 ± 0.3 | 12,935.5 ± 1.9 |
| 30 | 1114.9 ± 0.6 | 256.0 ± 0.2 | 50 | 45.8 ± 0.2 | 13,032.5 ± 2.7 |
| 35 | 1134.5 ± 1.3 | 260.1 ± 0.2 | 60 | 55.0 ± 0.4 | 13,140.9 ± 3.6 |
| 40 | 1153.7 ± 0.0 | 264.0 ± 0.0 | 70 | 64.4 ± 0.2 | 13,271.1 ± 5.1 |
| No. | SL | HL | SH | HH | ||
|---|---|---|---|---|---|---|
| 1 | 930 | 450 | 660 | 270 | 560 | 2.57 |
| 2 | 770 | 530 | 520 | 360 | 680 | 2.07 |
| 3 | 540 | 470 | 550 | 330 | 510 | 1.70 |
| 4 | 720 | 540 | 600 | 360 | 510 | 2.58 |
| 5 | 700 | 390 | 570 | 350 | 500 | 1.88 |
| 6 | 850 | 530 | 670 | 540 | 400 | 2.00 |
| 7 | 450 | 360 | 490 | 450 | 520 | 1.65 |
| 8 | 700 | 500 | 530 | 370 | 580 | 2.19 |
| 9 | 710 | 550 | 360 | 410 | 460 | 2.16 |
| 10 | 760 | 610 | 420 | 540 | 380 | 1.97 |
| 850 | 640 | 620 | 380 | 590 | 2.07 | |
| 1.69 | 1.47 | 1.25 | 1.31 | 1.48 | – |
| Feature | Value |
|---|---|
| Nominal thicker | 0.30 mm |
| Active sensor area | 35.1 mm × 35.1 mm |
| Semi-conductive layer: 0.10 mm/U1tem | |
| Rubber mattress build | Spacer adhesive: 0.10 mm/Acrylic |
| Conductive layer: 0.10 mm/U1tem | |
| Rear adhesive: 0.5 mm/Acrylic | |
| Wide-force sensitive range | <100 g–1 kg |
| Break force (turn-on force) | 20 g to 100 g |
| Stand-off resistance | 200–1200 kΩ |
| Temperature operating range | 35 °C to + 40 °C |
| Number of actuations (lifetime) | >10 million actuations |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mamom, J.; Rungroungdouyboon, B.; Daovisan, H.; Sri-Ngernyuang, C. Electronic Alert Signal for Early Detection of Tissue Injuries in Patients: An Innovative Pressure Sensor Mattress. Diagnostics 2023, 13, 145. https://doi.org/10.3390/diagnostics13010145
Mamom J, Rungroungdouyboon B, Daovisan H, Sri-Ngernyuang C. Electronic Alert Signal for Early Detection of Tissue Injuries in Patients: An Innovative Pressure Sensor Mattress. Diagnostics. 2023; 13(1):145. https://doi.org/10.3390/diagnostics13010145
Chicago/Turabian StyleMamom, Jinpitcha, Bunyong Rungroungdouyboon, Hanvedes Daovisan, and Chawakorn Sri-Ngernyuang. 2023. "Electronic Alert Signal for Early Detection of Tissue Injuries in Patients: An Innovative Pressure Sensor Mattress" Diagnostics 13, no. 1: 145. https://doi.org/10.3390/diagnostics13010145
APA StyleMamom, J., Rungroungdouyboon, B., Daovisan, H., & Sri-Ngernyuang, C. (2023). Electronic Alert Signal for Early Detection of Tissue Injuries in Patients: An Innovative Pressure Sensor Mattress. Diagnostics, 13(1), 145. https://doi.org/10.3390/diagnostics13010145






