Prognostic Significance of the N-Terminal Pro-B-Type Natriuretic Peptide in Lung Transplant Candidates on the Waiting List
Abstract
:1. Introduction
2. Materials and Methods
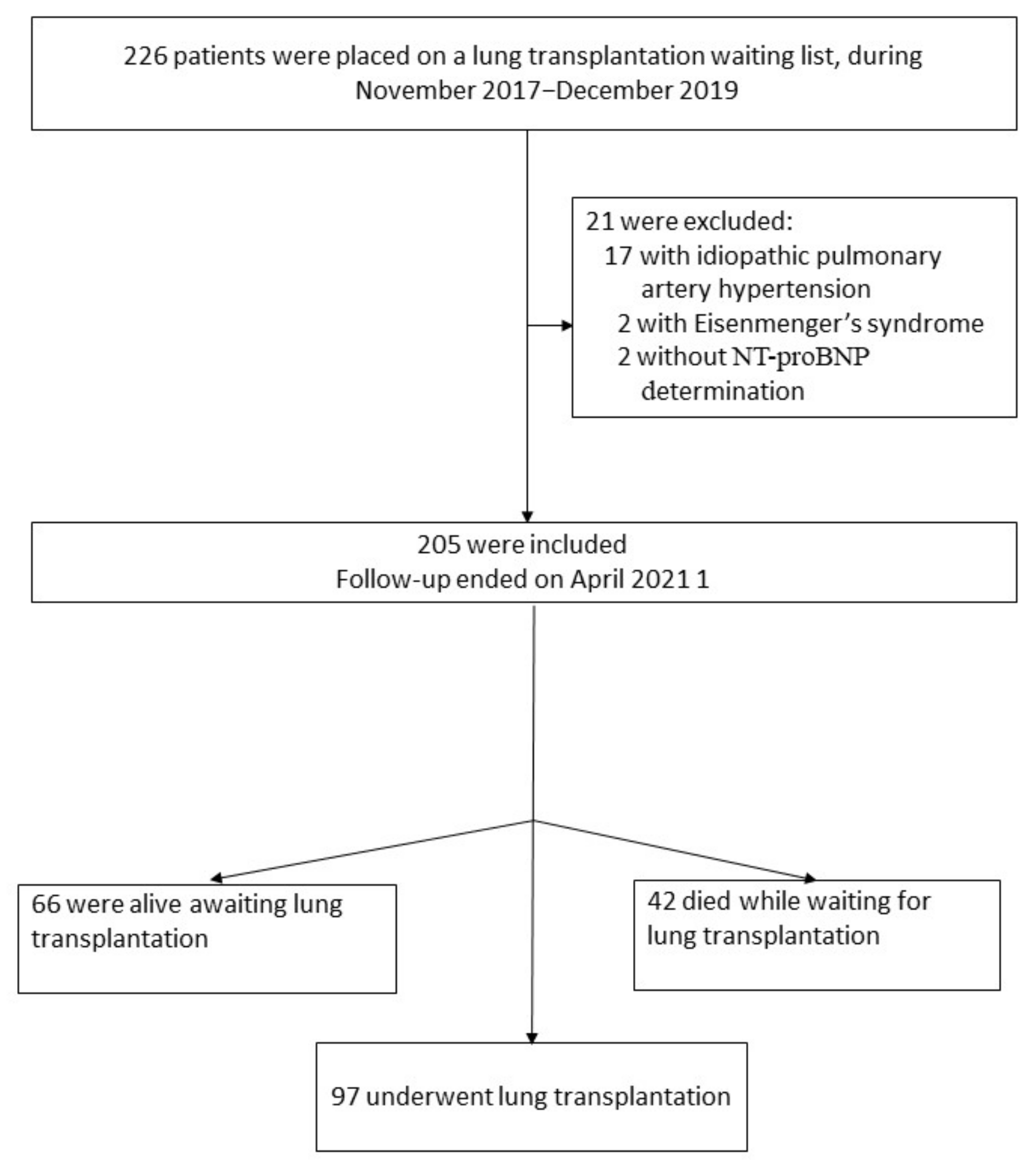
2.1. Study Population and Design
2.2. Follow-Up Protocol
2.3. NT-proBNP Laboratory Analysis
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
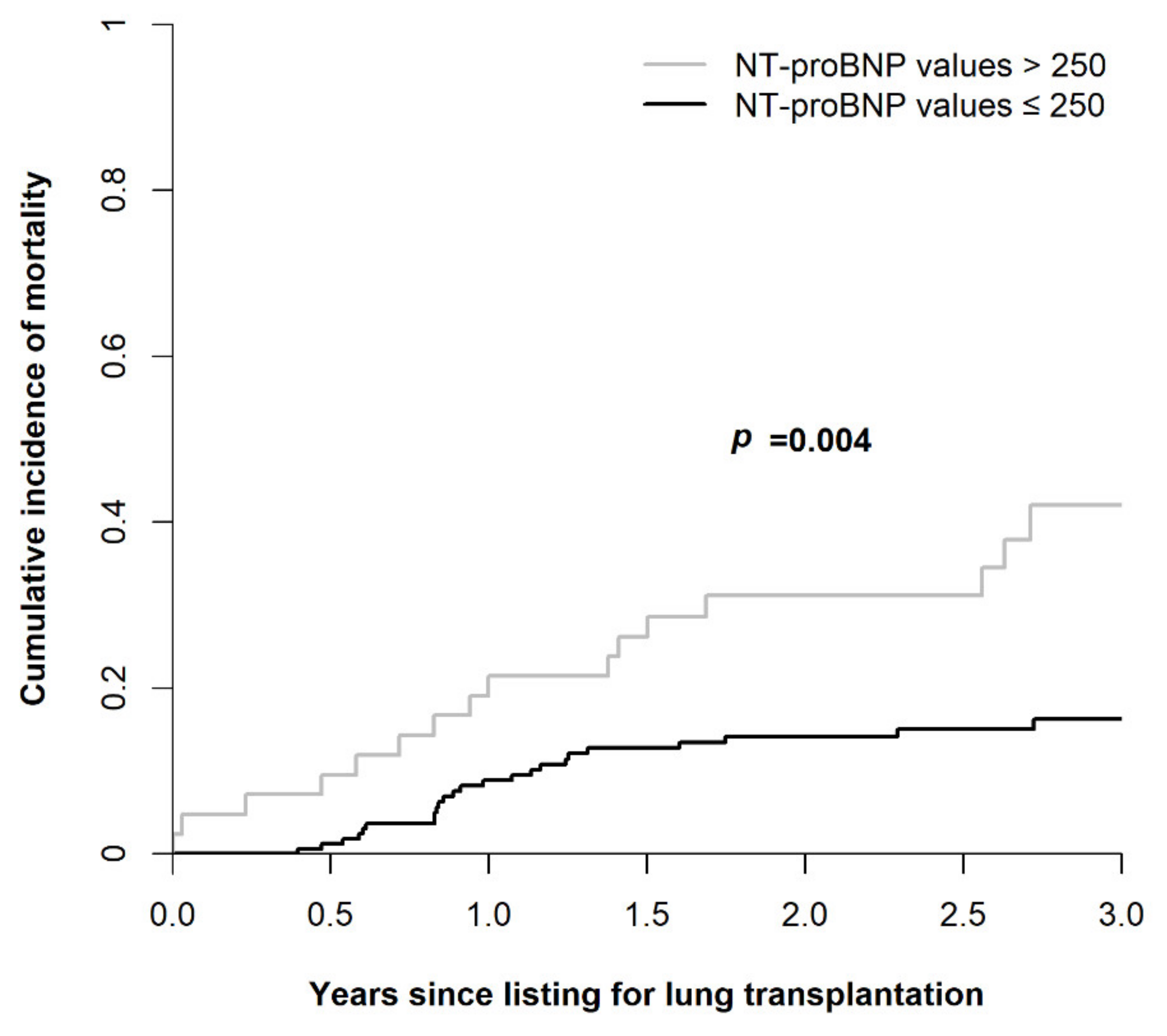
3.2. Survival Analysis
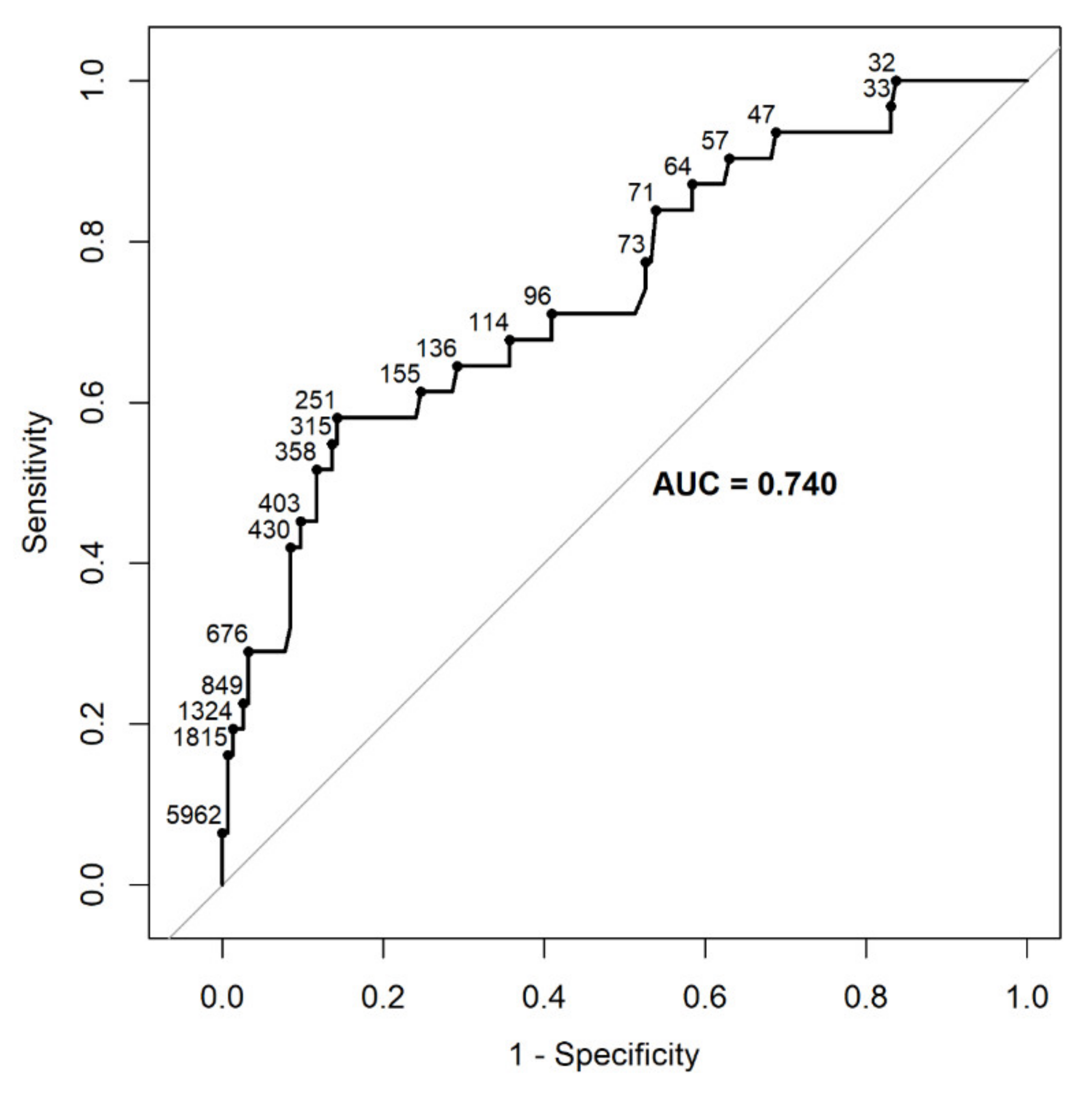
3.2.1. Univariate Analysis
3.2.2. Multivariate Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Del Ry, S.; Manuela, M.; Clerico, A. Natriuretic peptide system and the heart. Front. Horm. Res. 2014, 43, 134–143. [Google Scholar] [PubMed]
- Doyama, K.; Fukumoto, M.; Takemura, G.; Tanaka, M.; Oda, T.; Hasegawa, K.; Inada, T.; Ohtani, S.; Fujiwara, T.; Itoh, H.; et al. Expression and distribution of brain natriuretic peptide in human right atria. J. Am. Coll. Cardiol. 1998, 32, 1832–1838. [Google Scholar] [CrossRef]
- Hill, N.S.; Klinger, J.R.; Warburton, R.R.; Pietras, L.; Wrenn, D.S. Brain natriuretic peptide: Possible role in the modulation of hypoxic pulmonary hypertension. Am. J. Physiol. 1994, 266, 308–315. [Google Scholar] [CrossRef] [PubMed]
- Cargill, R.I.; Lipworth, B.J. Atrial natriuretic peptide and brain natriuretic peptide in cor pulmonale. Hemodynamic and endocrine effects. Chest 1996, 110, 1220–1225. [Google Scholar] [CrossRef] [PubMed]
- Galiè, N.; Humbert, M.; Vachiery, J.L.; Gibbs, S.; Lang, I.; Torbicki, A.; Simonneau, G.; Peacock, A.; Noordegraaf, A.V.; Beghetti, M.; et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS). Eur. Respir. J. 2015, 46, 903–975. [Google Scholar] [CrossRef] [PubMed]
- Corte, T.J.; Wort, S.J.; Gatzoulis, M.A.; Engel, R.; Giannakoulas, G.; Macdonald, P.M.; Wells, A.U. Elevated brain natriuretic peptide predicts mortality in interstitial lung disease. Eur. Respir. J. 2010, 36, 819–825. [Google Scholar] [CrossRef] [PubMed]
- Leuchte, H.H.; Baumgartner, R.A.; El Nounou, M.; Vogeser, M.; Neurohr, C.; Trautnitz, M.; Behr, J. Brain natriuretic peptide is a prognostic parameter in chronic lung disease. Am. J. Respir. Crit. Care Med. 2006, 173, 744–750. [Google Scholar] [CrossRef] [PubMed]
- Leuchte, H.H.; Neurohr, C.; Baumgartner, R.; Holzapfel, M.; Giehrl, W.; Vogeser, M.; Behr, J. Brain natriuretic peptide and exercise capacity in lung fibrosis and pulmonary hypertension. Am. J. Respir. Crit. Care Med. 2004, 170, 360–365. [Google Scholar] [CrossRef] [PubMed]
- Pavasini, R.; Tavazzi, G.; Biscaglia, S.; Guerra, F.; Pecoraro, A.; Zaraket, F.; Gallo, F.; Spitaleri, G.; Contoli, M.; Ferrari, R.; et al. Amino terminal pro brain natriuretic peptide predicts all-cause mortality in patients with chronic obstructive pulmonary disease: Systematic review and meta-analysis. Chronic Respir. Dis. 2017, 14, 117–126. [Google Scholar] [CrossRef] [PubMed]
- Weill, D.; Benden, C.; Corris, P.A.; Dark, J.H.; Davis, R.D.; Keshavjee, S.; Lederer, D.J.; Mulligan, M.J.; Patterson, G.A.; Singer, L.G.; et al. A consensus document for the selection of lung transplant candidates: 2014—An update from the Pulmonary Transplantation Council of the International Society for Heart and Lung Transplantation. J. Heart Lung Transplant. 2015, 34, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Januzzi, J.L.; van Kimmenade, R.; Lainchbury, J.; Bayes-Genis, A.; Ordonez-Llanos, J.; Santalo-Bel, M.; Pinto, Y.M.; Richards, M. NT-proBNP testing for diagnosis and short-term prognosis in acute destabilized heart failure: An international pooled analysis of 1256 patients: The International Collaborative of NT-proBNP Study. Eur. Heart J. 2006, 27, 330–337. [Google Scholar] [CrossRef] [PubMed]
- Egan, T.M.; Murray, S.; Bustami, R.T.; Shearon, T.H.; McCullough, K.P.; Edwards, L.B.; Coke, M.A.; Garrity, E.R.; Sweet, S.C.; Heiney, D.A.; et al. Development of the new lung allocation system in the United States. Am. J. Transplant. 2006, 6, 1212–1227. [Google Scholar] [CrossRef] [PubMed]
- Seeger, W.; Adir, Y.; Barberà, J.A.; Champion, H.; Coghlan, J.G.; Cottin, V.; De Marco, T.; Galiè, N.; Ghio, S.; Gibbs, S.; et al. Pulmonary hypertension in chronic lung diseases. J. Am. Coll. Cardiol. 2013, 62, D109–D116. [Google Scholar] [CrossRef] [PubMed]
- Hoeper, M.M.; Lee, S.H.; Voswinckel, R.; Palazzini, M.; Jais, X.; Marinelli, A.; Barst, R.J.; Ghofrani, H.A.; Jing, Z.C.; Opitz, C.; et al. Complications of right heart catheterization procedures in patients with pulmonary hypertension in experienced centers. J. Am. Coll. Cardiol. 2006, 48, 2546–2552. [Google Scholar] [CrossRef] [PubMed]
- Finkelhor, R.S.; Lewis, S.A.; Pillai, D. Limitations and strengths of doppler/echo pulmonary artery systolic pressure-right heart catheterization correlations: A systematic literature review. Echocardiography 2015, 32, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Ni, J.R.; Yan, P.J.; Liu, S.D.; Hu, Y.; Yang, K.H.; Song, B.; Lei, J.Q. Diagnostic accuracy of transthoracic echocardiography for pulmonary hypertension: A systematic review and meta-analysis. BMJ Open 2019, 9, e033084. [Google Scholar] [CrossRef] [PubMed]
- Keir, G.J.; Wort, S.J.; Kokosi, M.; George, P.M.; Walsh, S.L.; Jacob, J.; Price, L.; Bax, S.; Renzoni, E.A.; Maher, T.M.; et al. Pulmonary hypertension in interstitial lung disease: Limitations of echocardiography compared to cardiac catheterization. Respirology 2018, 23, 687–694. [Google Scholar] [CrossRef] [PubMed]
- Arcasoy, S.M.; Christie, J.D.; Ferrari, V.A.; Sutton, M.S.J.; Zisman, D.A.; Blumenthal, N.P.; Pochettino, A.; Kotloff, R.M. Echocardiographic assessment of pulmonary hypertension in patients with advanced lung disease. Am. J. Respir. Crit. Care Med. 2003, 167, 735–740. [Google Scholar] [CrossRef] [PubMed]
- Fisher, M.R.; Criner, G.J.; Fishman, A.P.; Hassoun, P.M.; Minai, O.A.; Scharf, S.M.; Fessler, A.H.E.; NETT Research Group. Estimating pulmonary artery pressures by echocardiography in patients with emphysema. Eur. Respir. J. 2007, 30, 914–921. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Ch Patients’ Characteristics | Total Population Results (n = 205) | Survivors Waiting Transplantation (n = 66) | Non-Survivors Waiting Transplantation (n = 42) | Lung Transplant Recipients (n = 97) | p-Value |
|---|---|---|---|---|---|
| Age (years) | 59.3 ± 10.4 | 61.6 ± 8.7 | 62.0 ± 7.1 | 56.6 ± 11.9 | <0.001 |
| Male sex | 136 (66.3%) | 41 (62.1%) | 20 (47.6%) | 75 (77.3%) | 0.002 |
| Reason for transplantation | 0.001 | ||||
| Interstitial lung disease | 111 (54.1%) | 27 (41.0%) | 29 (69.0%) | 55(56.7%) | |
| Idiopathic pulmonary fibrosis | 62 | 15 | 16 | 31 | |
| Autoimmune ILD | 10 | 3 | 1 | 6 | |
| Hypersnsitivity pneumonitis | 11 | 2 | 3 | 6 | |
| I-NSIP | 11 | 4 | 5 | 2 | |
| Occupational ILD | 9 | 1 | 1 | 7 | |
| Drug induced ILD | 3 | 1 | 1 | 1 | |
| Sarcoidosis | 3 | 1 | 1 | 1 | |
| Others | 2 | 0 | 1 | 1 | |
| COPD | 72 (35.1%) | 35 (53.0%) | 12 (28.6%) | 25 (25.8%) | |
| Non cystic fibrosis bronchiectasis | 9 (4.4%) | 2 (3.0%) | 0 (0.0%) | 7 (7.2%) | |
| Cystic Fibrosis | 6 (2.9%) | 1 (1.5%) | 0 (0.0%) | 5 (5.2%) | |
| Graft versus host disease | 5 (2.4%) | 1 (1.5%) | 0 (0.0%) | 4 (4.1%) | |
| Others | 2 (1.0%) | 0 (0.0%) | 1 (2.4%) | 1 (1.0%) | |
| Body mass index (kg/m2) | 26.9 ± 5.6 | 26.1 ± 6.4 | 28.5 ± 5.6 | 26.6 ± 5.0 | 0.09 |
| NT-proBNP (pg/mL) | 287.6 ± 911.8 | 142 ± 224 | 571 ± 1698 | 263 ± 671 | 0.054 |
| Serum creatinine (normal 0.5–0.9 mg/dL) | 0.8 ± 0.5 | 0.8 ± 0.3 | 0.9 ± 0.7 | 0.9 ± 0.5 | 0.46 |
| Six-minute walk test distance (meters) | 283 ± 121 | 287 ± 127 | 227 ± 132 | 304 ± 106 | 0.006 |
| Data of lung function test | |||||
| FEV1 (% of predicted value) | 39 ± 18 | 37± 19 | 39 ± 18 | 40 ± 18 | 0.52 |
| FVC (% of predicted value) | 49 ± 16 | 52 ± 17 | 45 ± 14 | 48 ± 16 | 0.09 |
| FEV1/FVC ratio | 0.7 ± 0.3 | 0.6 ± 0.3 | 0.7 ± 0.3 | 0.7 ± 0.2 | 0.21 |
| TLC (% of predicted value) | 79 ± 37 | 89 ± 37 | 70 ± 36 | 76 ± 36 | 0.01 |
| RV (% of predicted value) | 137 ± 97 | 158 ± 93 | 119 ± 97 | 131 ± 99 | 0.09 |
| DLCO (% of predicted value) | 33 ± 12 | 35 ± 13 | 28 ± 10 | 35 ± 13 | 0.01 |
| Data of right heart catheterization | |||||
| MPAP (mmHg) | 25.1 ± 9.9 | 23.2 ± 8.8 | 25.0 ± 9.3 | 26.5 ± 11.0 | 0.15 |
| PCWP (mmHg) | 10.6 ± 6.7 | 9.6 ± 6.4 | 10.3 ± 7.7 | 11.4 ± 6.4 | 0.26 |
| CI (L/min/m2) | 2.4 ± 0.6 | 2.5 ± 0.6 | 2.4 ± 0.6 | 2.4 ± 0.6 | 0.32 |
| CO (L/min) | 4.5 ± 1.3 | 4.5 ± 1.2 | 4.2 ± 1.2 | 4.6 ± 1.4 | 0.21 |
| PVR (WU) | 3.2 ± 0.1 | 3.2 ± 2.0 | 3.9 ± 2.3 | 4.0 ± 4.2 | 0.37 |
| Data of Lung Function Test | Total Population of the Study (n = 205) | Patients with ILD (n = 101) | Patients with COPD (n = 72) | p-Value |
|---|---|---|---|---|
| FEV1 (% of predicted value) | 39 ± 18 | 51 ± 16 | 26 ± 9 | <0.0001 |
| FVC (% of predicted value) | 48 | 47 ± 14 | 54 ± 15 | <0.0001 |
| FEV1/FVC ratio | 0.67 ± 0.2 | 0.87 ± 0.1 | 0.39 ± 0.1 | <0.0001 |
| TLC (% of predicted value) | 79 ± 37 | 51 ± 15 | 117 ± 21 | <0.0001 |
| RV (% of predicted value) | 137 ± 97 | 63 ± 31 | 228 ± 66 | <0.0001 |
| DLCO (% of predicted value) | 33 ± 12 | 33 ± 12 | 31 ± 12 | 0.07 |
| Parameter | r | p-Value |
|---|---|---|
| Age | 0.16 | 0.02 |
| Six-minute walk test distance (meters) | −0.14 | 0.06 |
| Data of lung function test | ||
| FEV1 (% of predicted value) | 0.12 | 0.1 |
| FVC (% of predicted value) | 0.16 | 0.02 |
| TLC (% of predicted value) | 0.01 | 0.9 |
| DLCO (% of predicted value) | −0.26 | <0.001 |
| Data of right heart catheterization | ||
| MPAP (mmHg) | 0.4 | <0.001 |
| PCWP (mmHg) | 0.12 | 0.11 |
| CI (L/min/m2) | −0.29 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Izhakian, S.; Frajman, A.; Freidkin, L.; Shtraichman, O.; Rosengarten, D.; Pertzov, B.; Barac, Y.D.; Kramer, M.R. Prognostic Significance of the N-Terminal Pro-B-Type Natriuretic Peptide in Lung Transplant Candidates on the Waiting List. Diagnostics 2022, 12, 2112. https://doi.org/10.3390/diagnostics12092112
Izhakian S, Frajman A, Freidkin L, Shtraichman O, Rosengarten D, Pertzov B, Barac YD, Kramer MR. Prognostic Significance of the N-Terminal Pro-B-Type Natriuretic Peptide in Lung Transplant Candidates on the Waiting List. Diagnostics. 2022; 12(9):2112. https://doi.org/10.3390/diagnostics12092112
Chicago/Turabian StyleIzhakian, Shimon, Assaf Frajman, Lev Freidkin, Osnat Shtraichman, Dror Rosengarten, Barak Pertzov, Yaron D. Barac, and Mordechai Reuven Kramer. 2022. "Prognostic Significance of the N-Terminal Pro-B-Type Natriuretic Peptide in Lung Transplant Candidates on the Waiting List" Diagnostics 12, no. 9: 2112. https://doi.org/10.3390/diagnostics12092112
APA StyleIzhakian, S., Frajman, A., Freidkin, L., Shtraichman, O., Rosengarten, D., Pertzov, B., Barac, Y. D., & Kramer, M. R. (2022). Prognostic Significance of the N-Terminal Pro-B-Type Natriuretic Peptide in Lung Transplant Candidates on the Waiting List. Diagnostics, 12(9), 2112. https://doi.org/10.3390/diagnostics12092112






