Extra-Gynecological Pelvic Pathology: A Challenge in the Differential Diagnosis of the Female Pelvis
Abstract
1. Introduction
1.1. Ultrasound Technique
1.2. Female Pelvis Anatomy
- (1)
- Imaging of the digestive system;
- (2)
- Imaging of the uro-renal system;
- (3)
- Vascular imaging;
- (4)
- Lymphatic imaging;
- (5)
- Neurological imaging;
- (6)
- Cutaneous images;
- (7)
- Others.
2. Imaging of the Digestive System
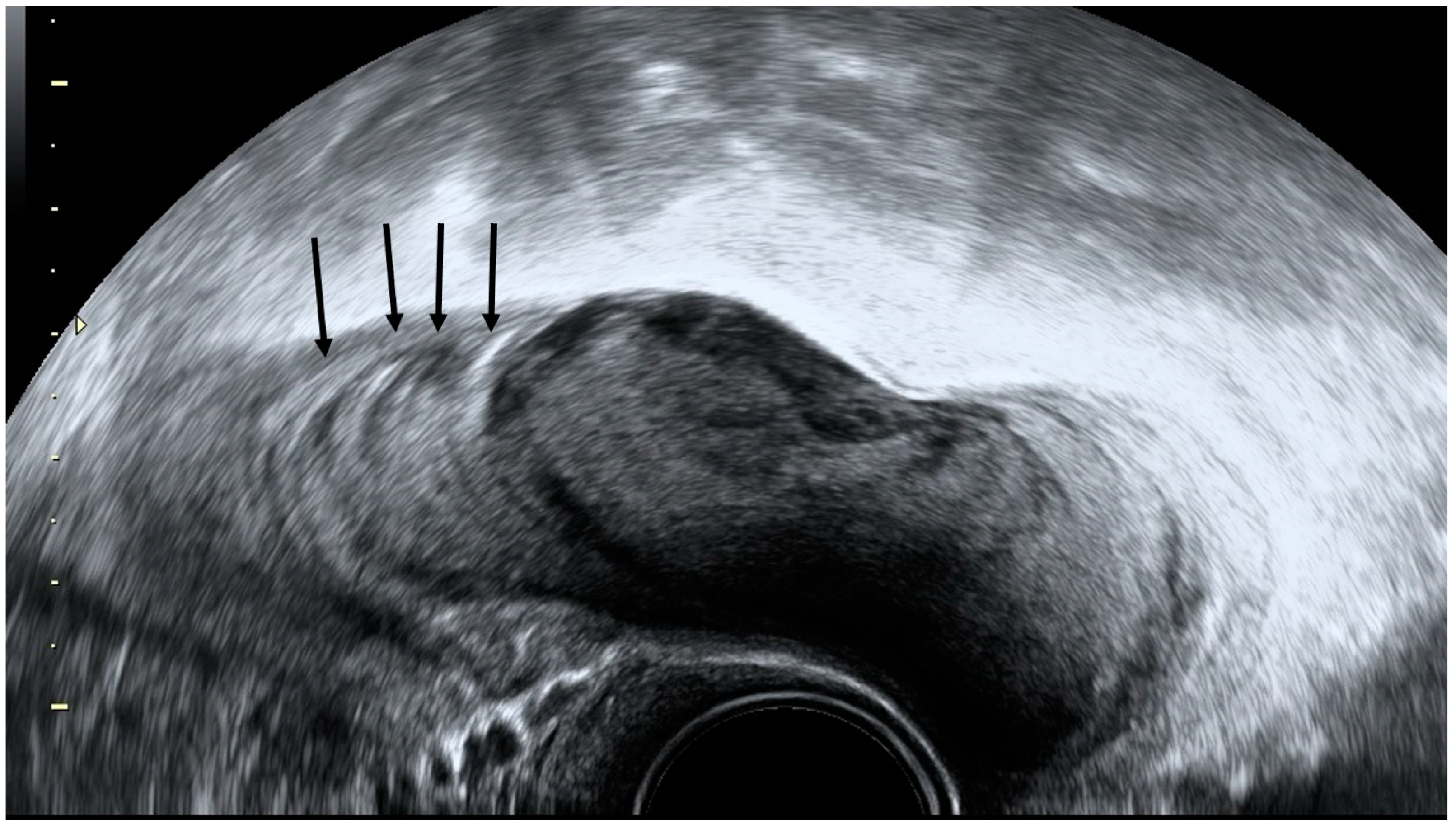
2.1. Appendicitis
2.2. Appendicular Plastron
2.3. Appendiceal Mucocele
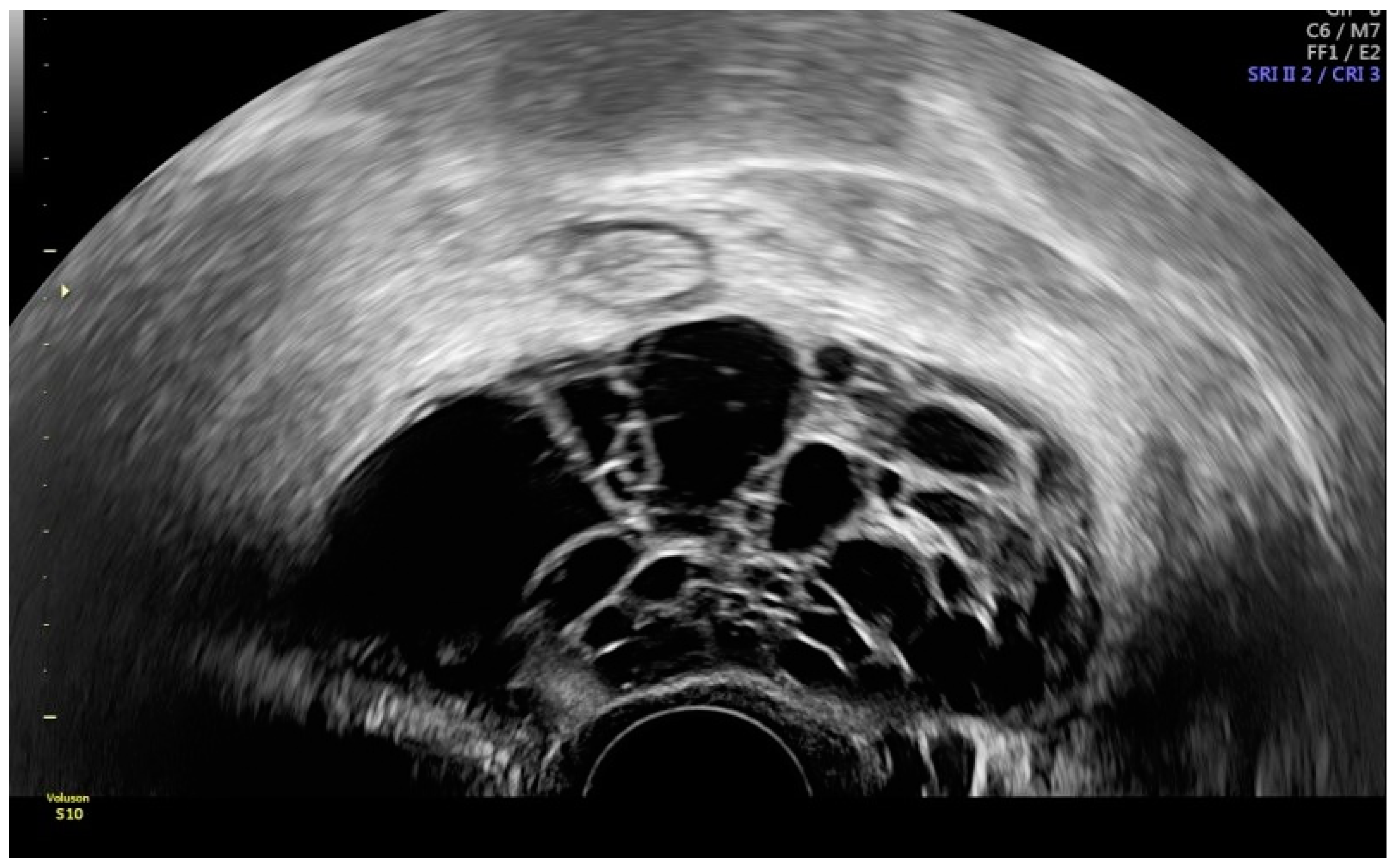
2.4. Diverticulosis and Diverticulitis
2.5. Bowel Tumors
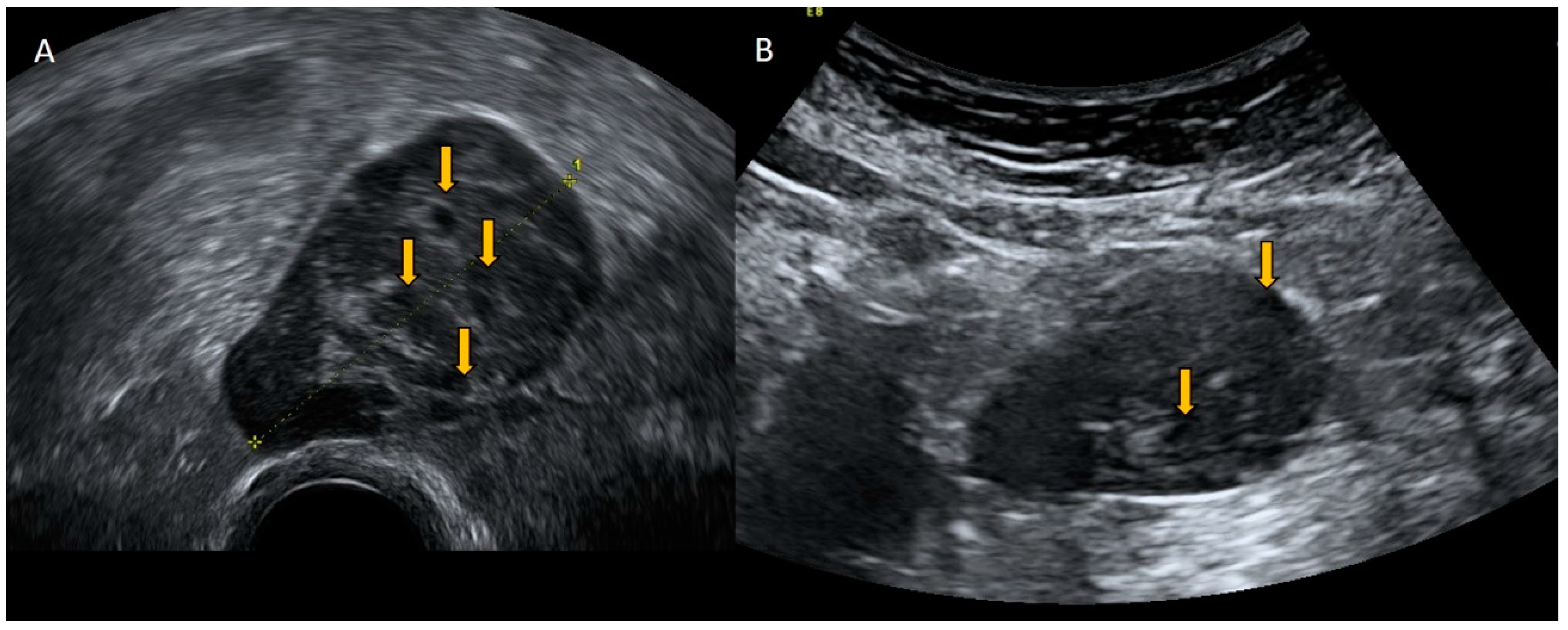
3. Imaging of the Uro-Renal System
3.1. Mega Ureter and Ureterocele
3.2. Benign and Malignant Bladder Pathology
3.3. Pelvic Kidney
4. Vascular Imaging
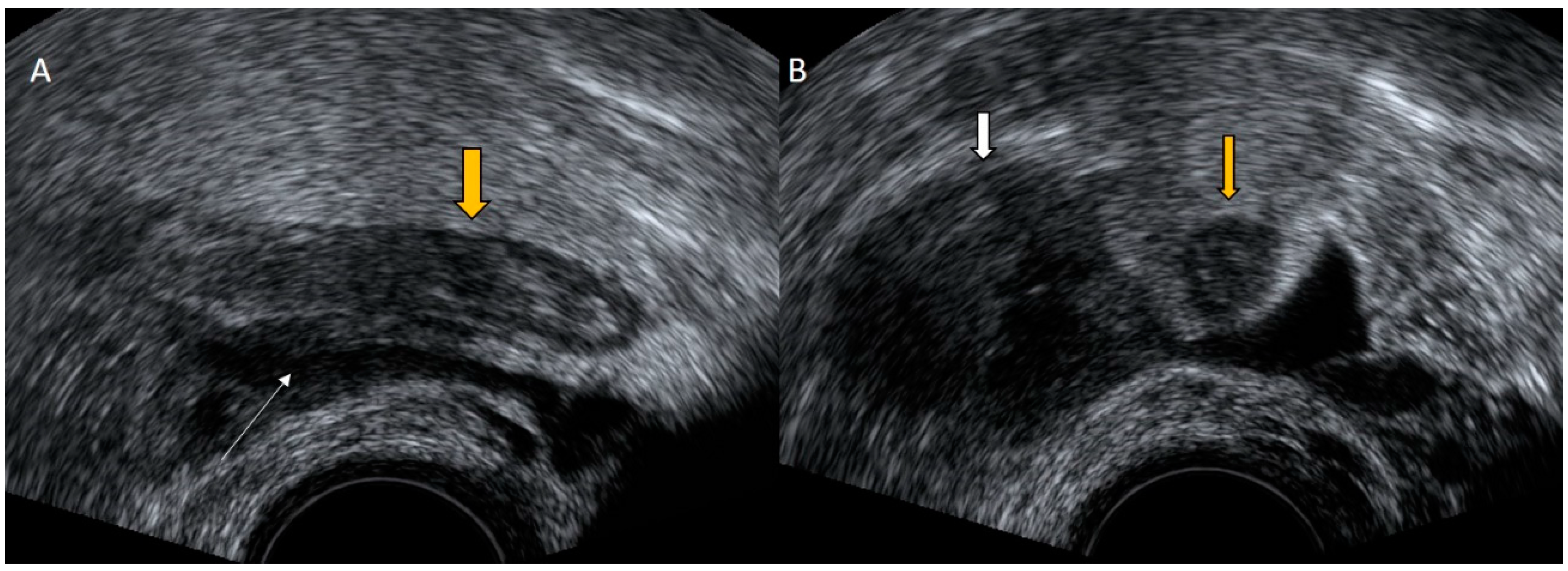
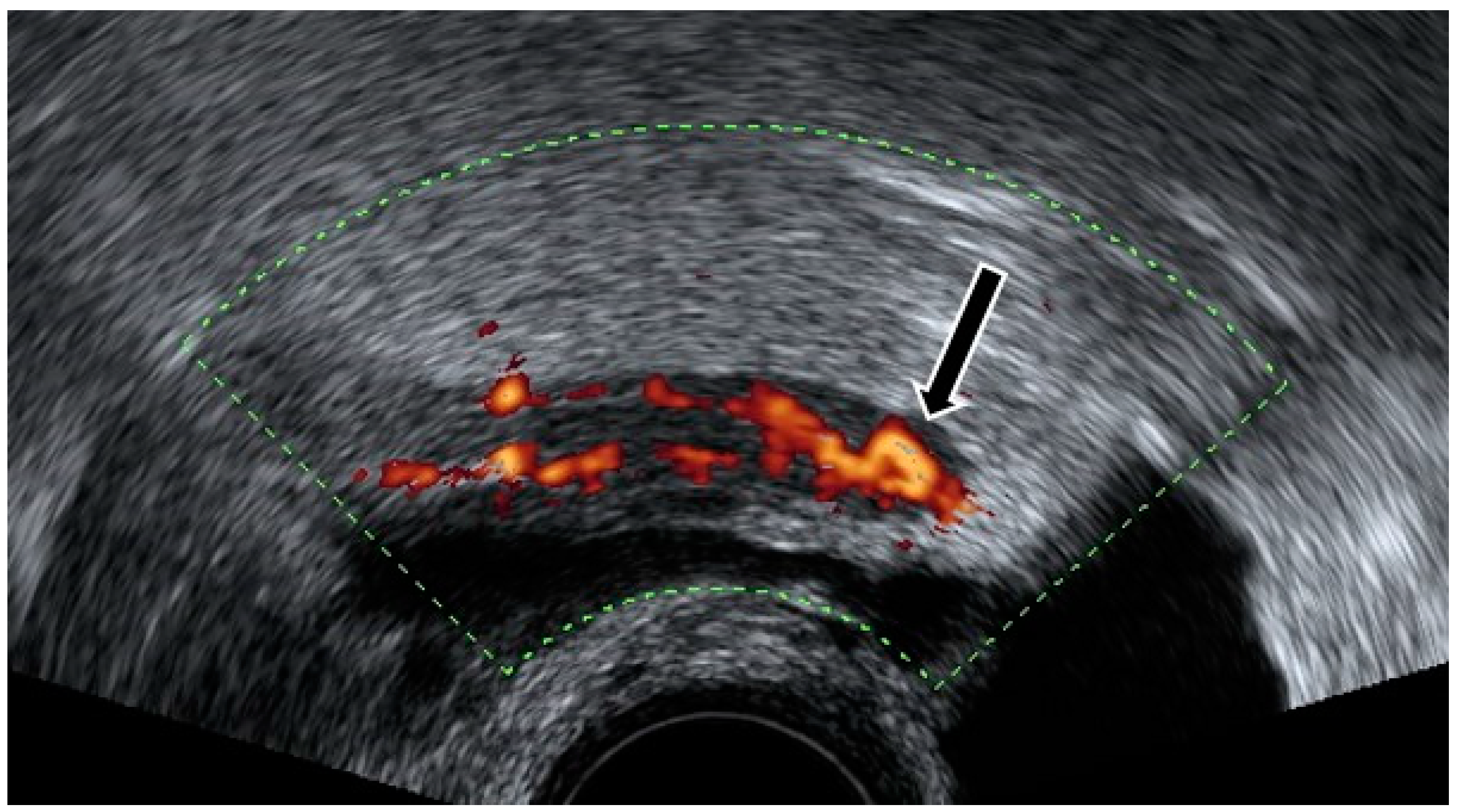
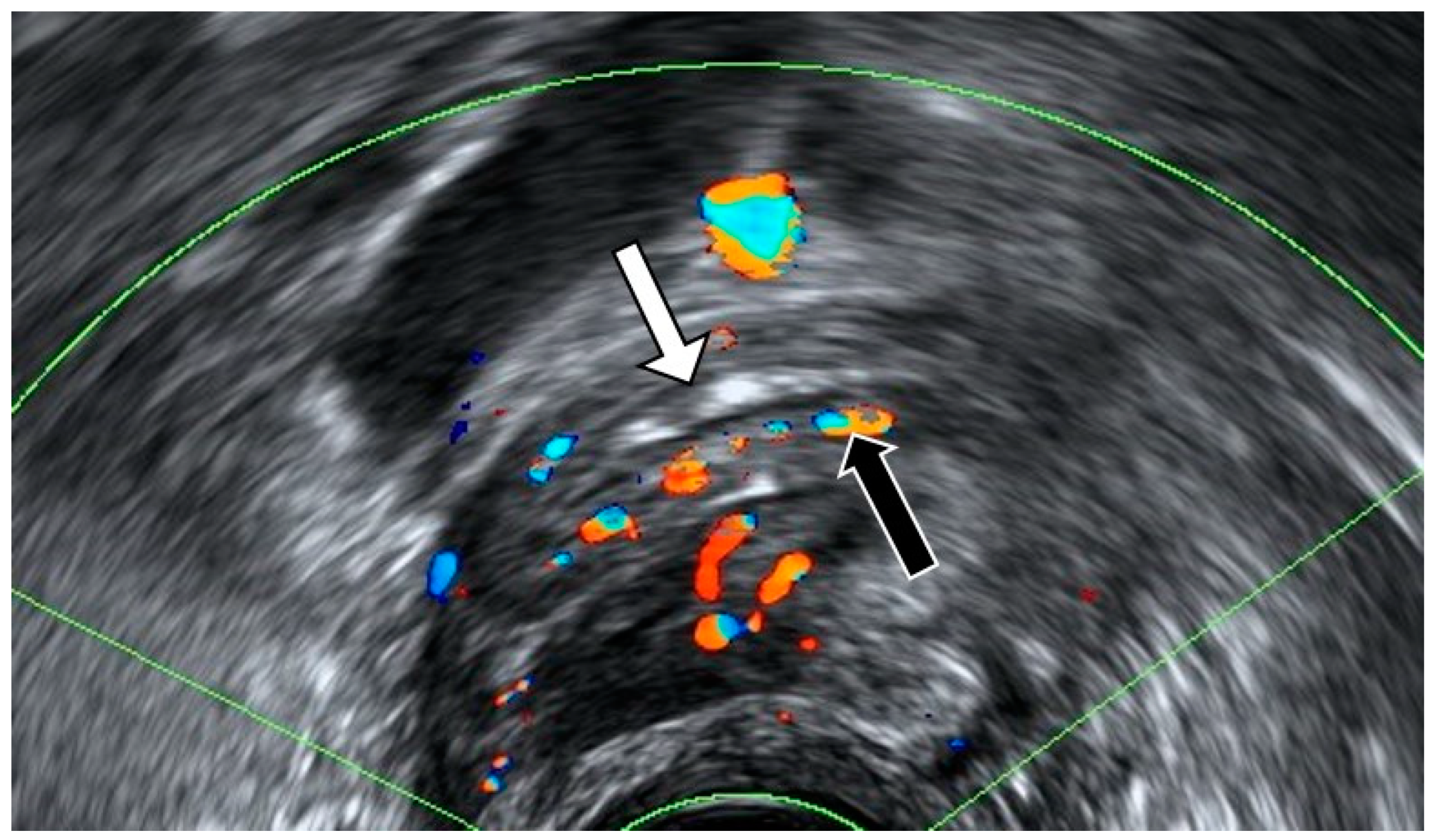
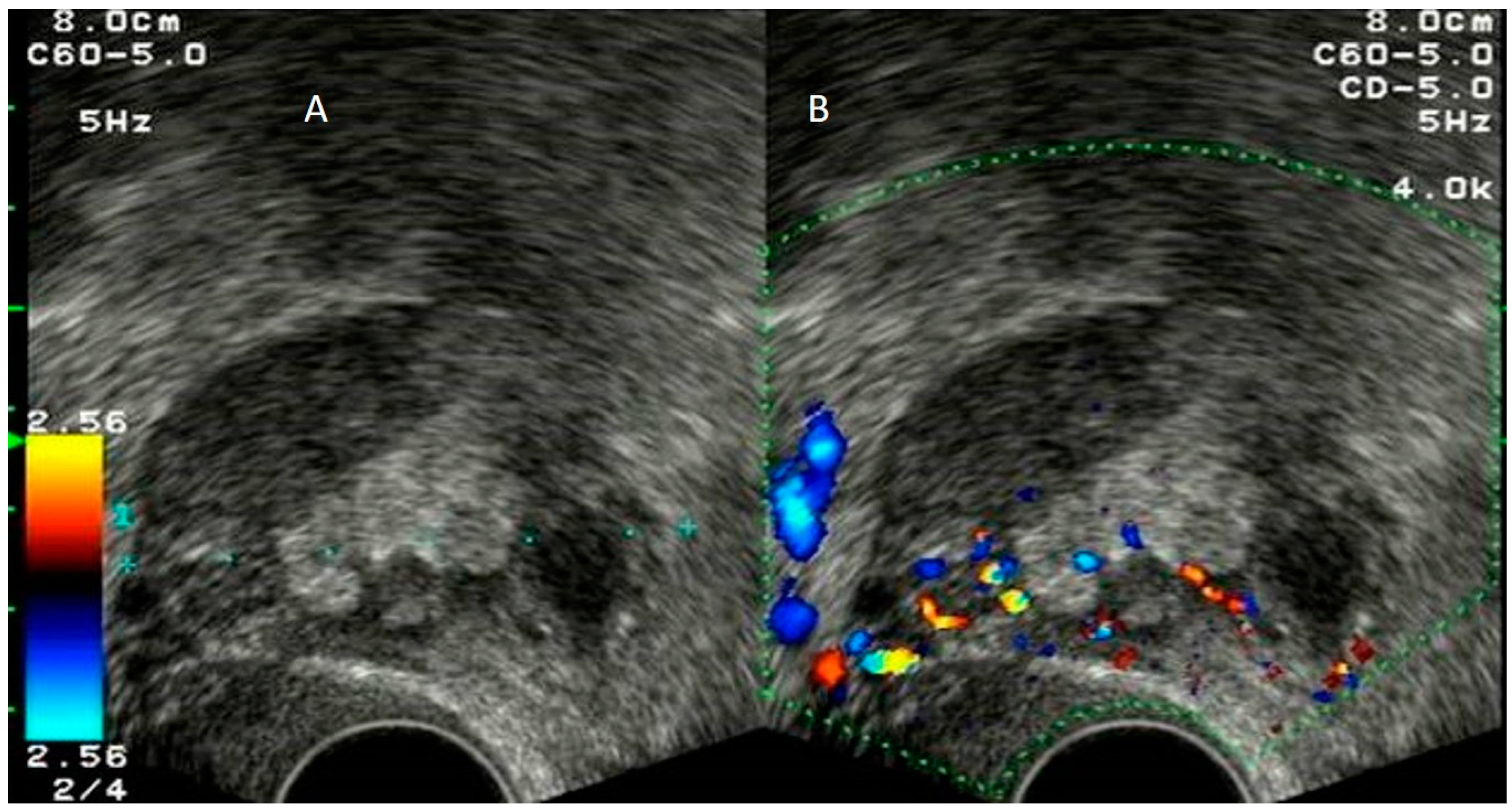
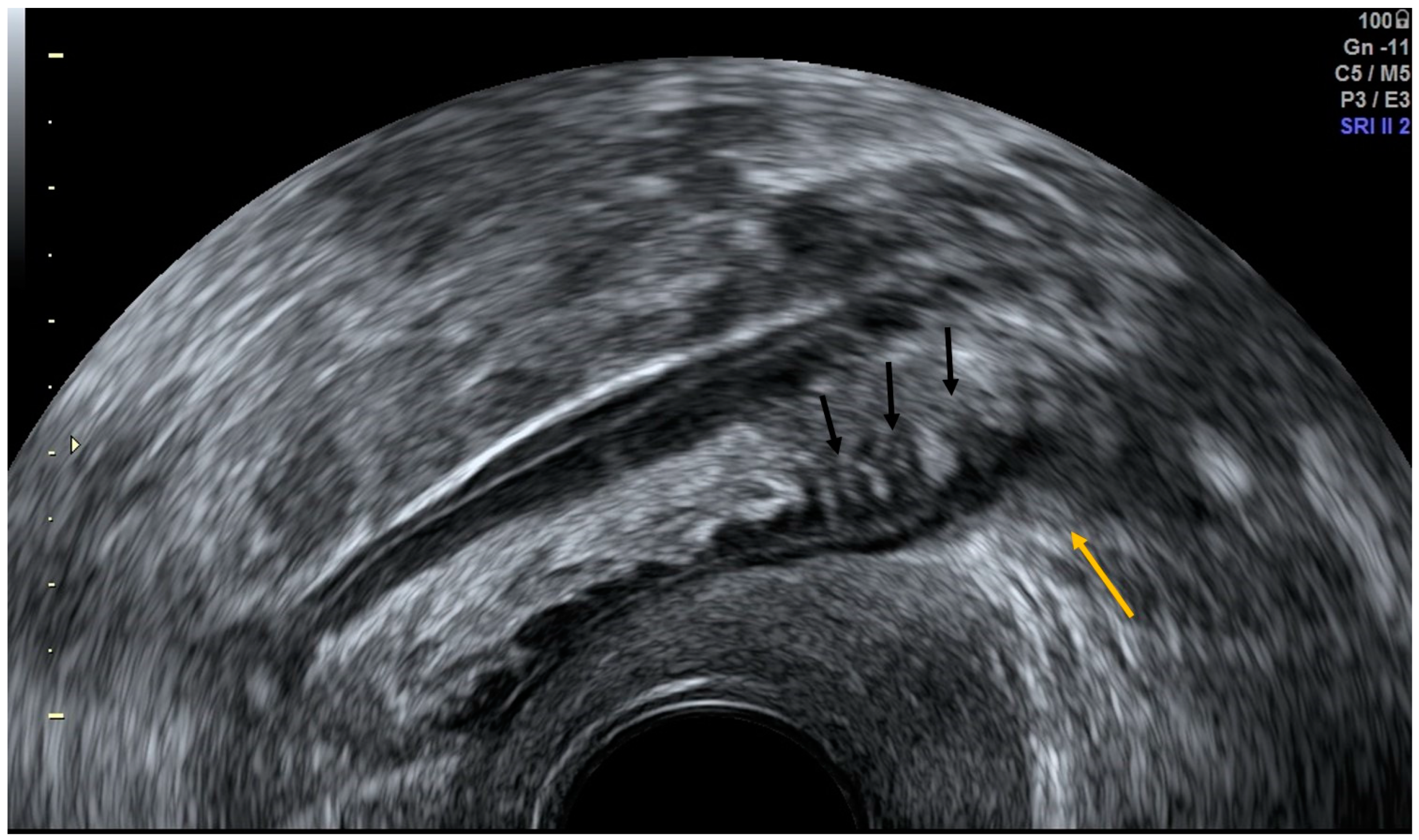
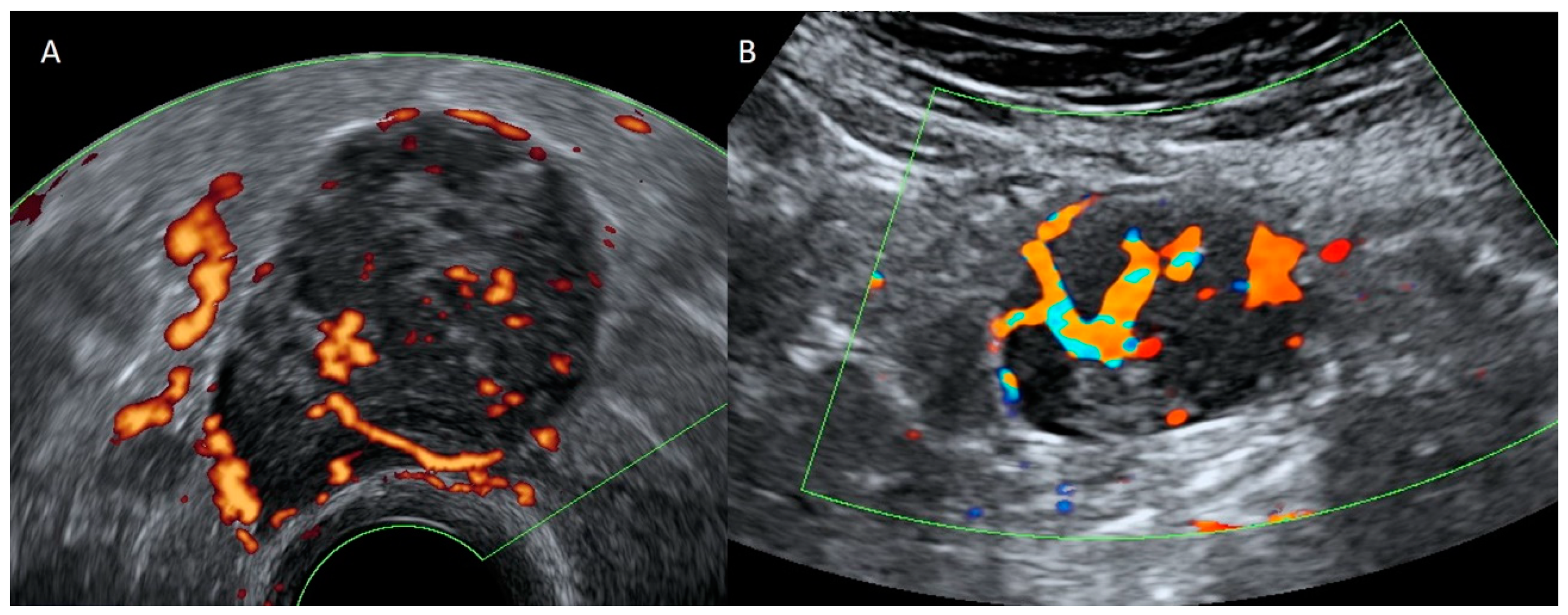
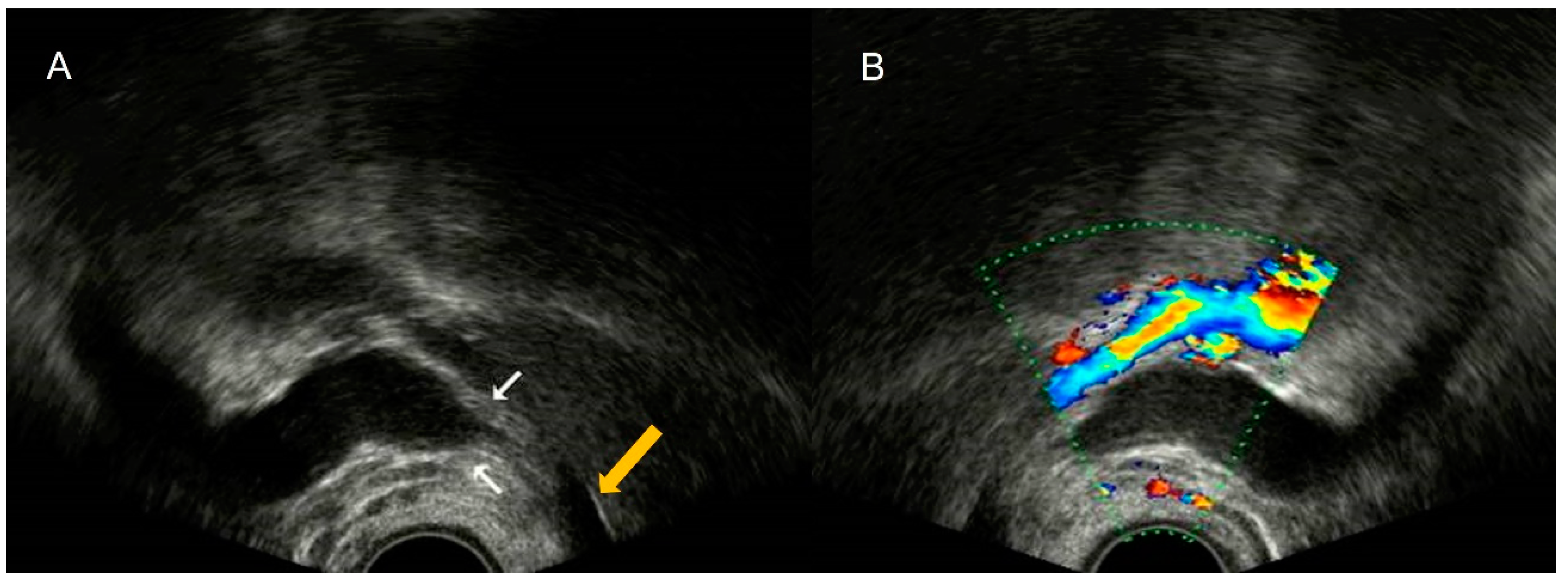
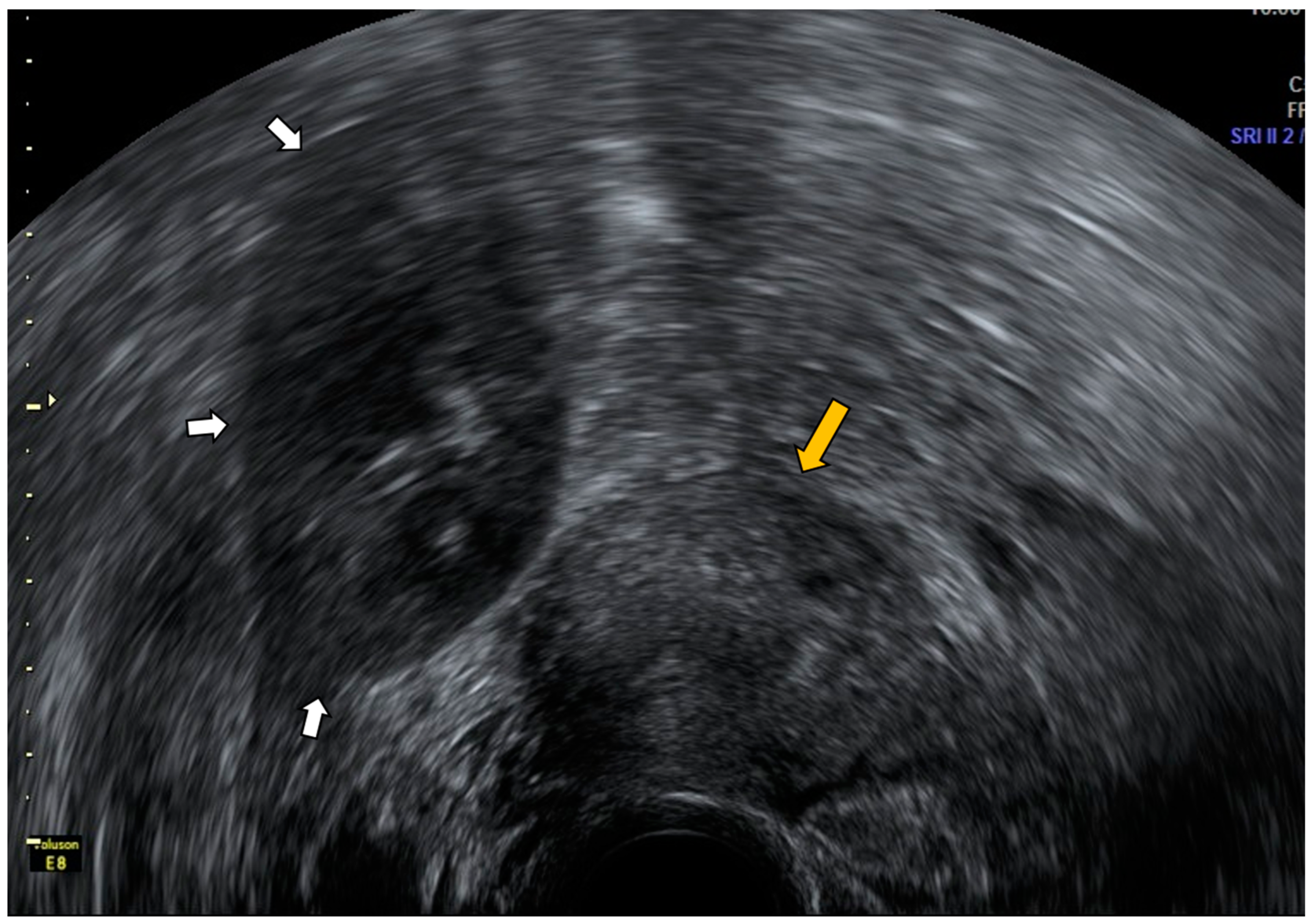
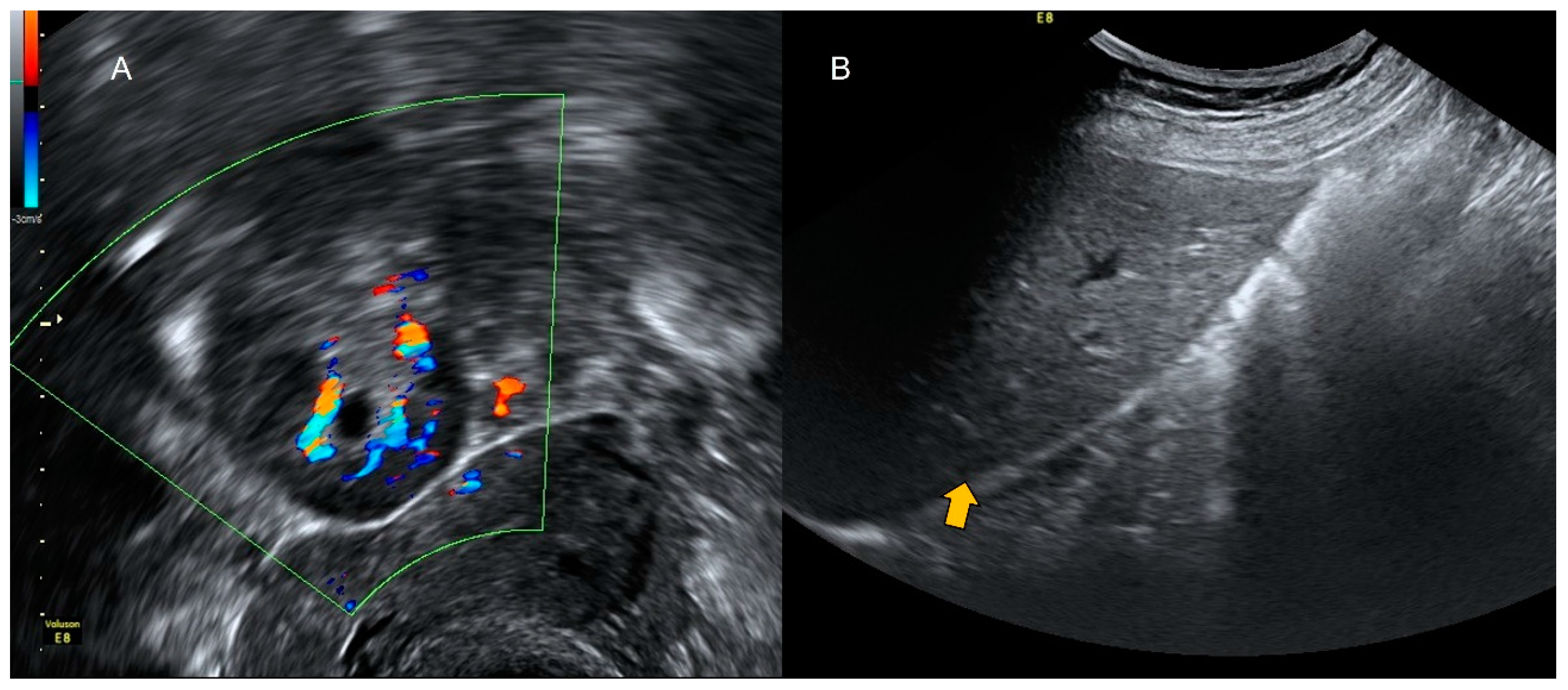
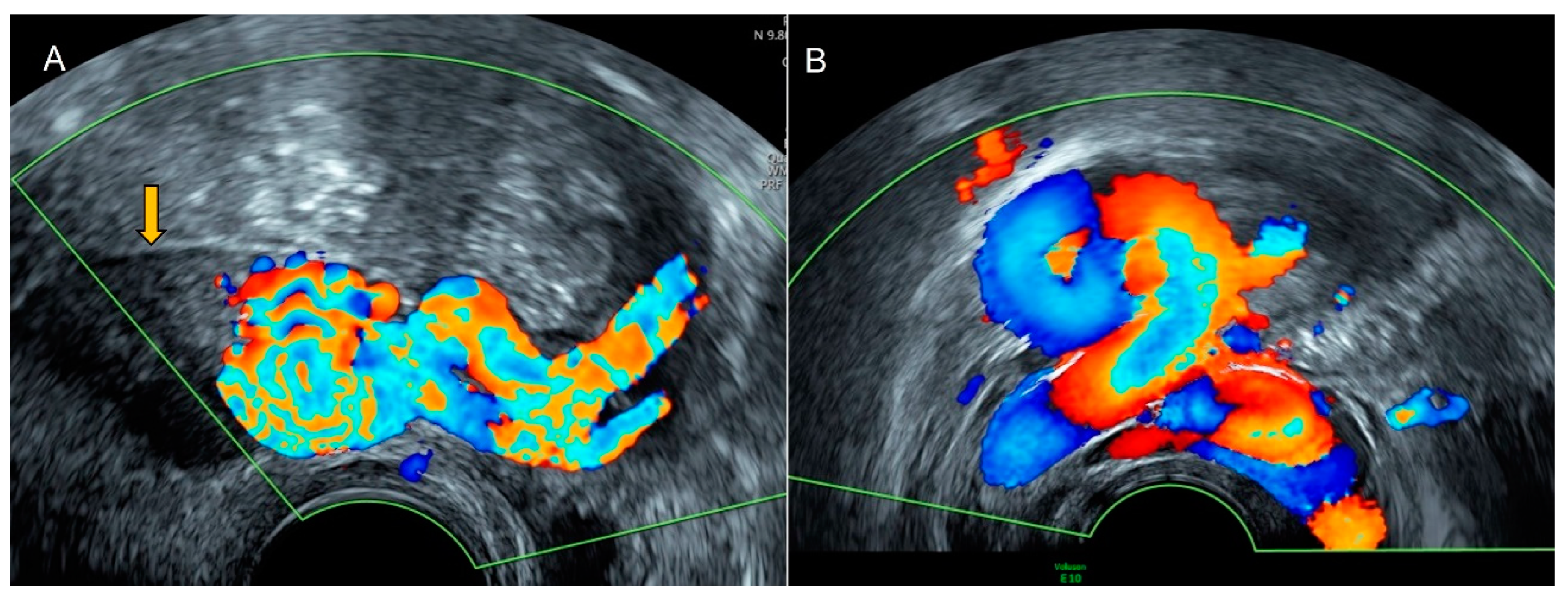
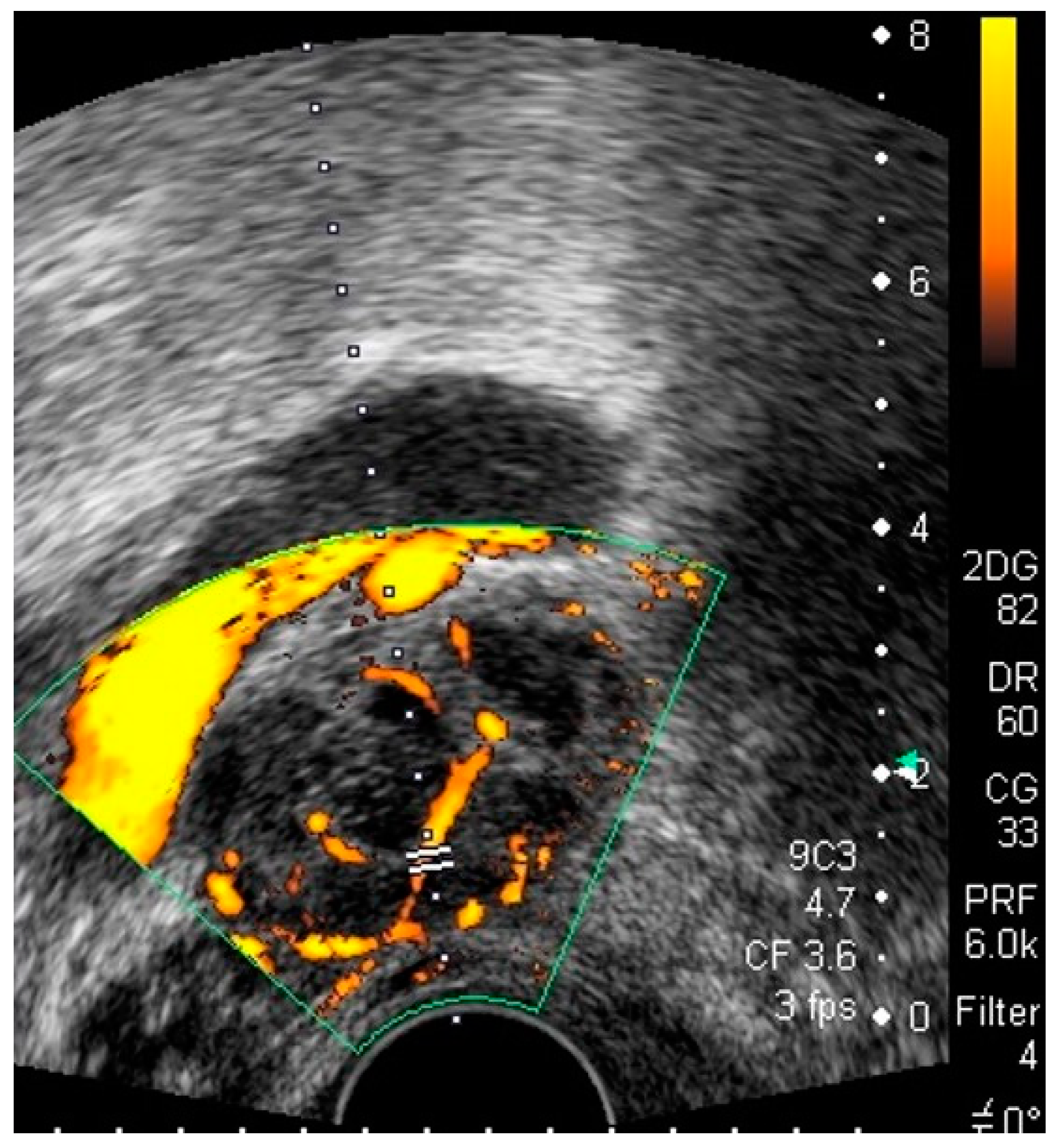
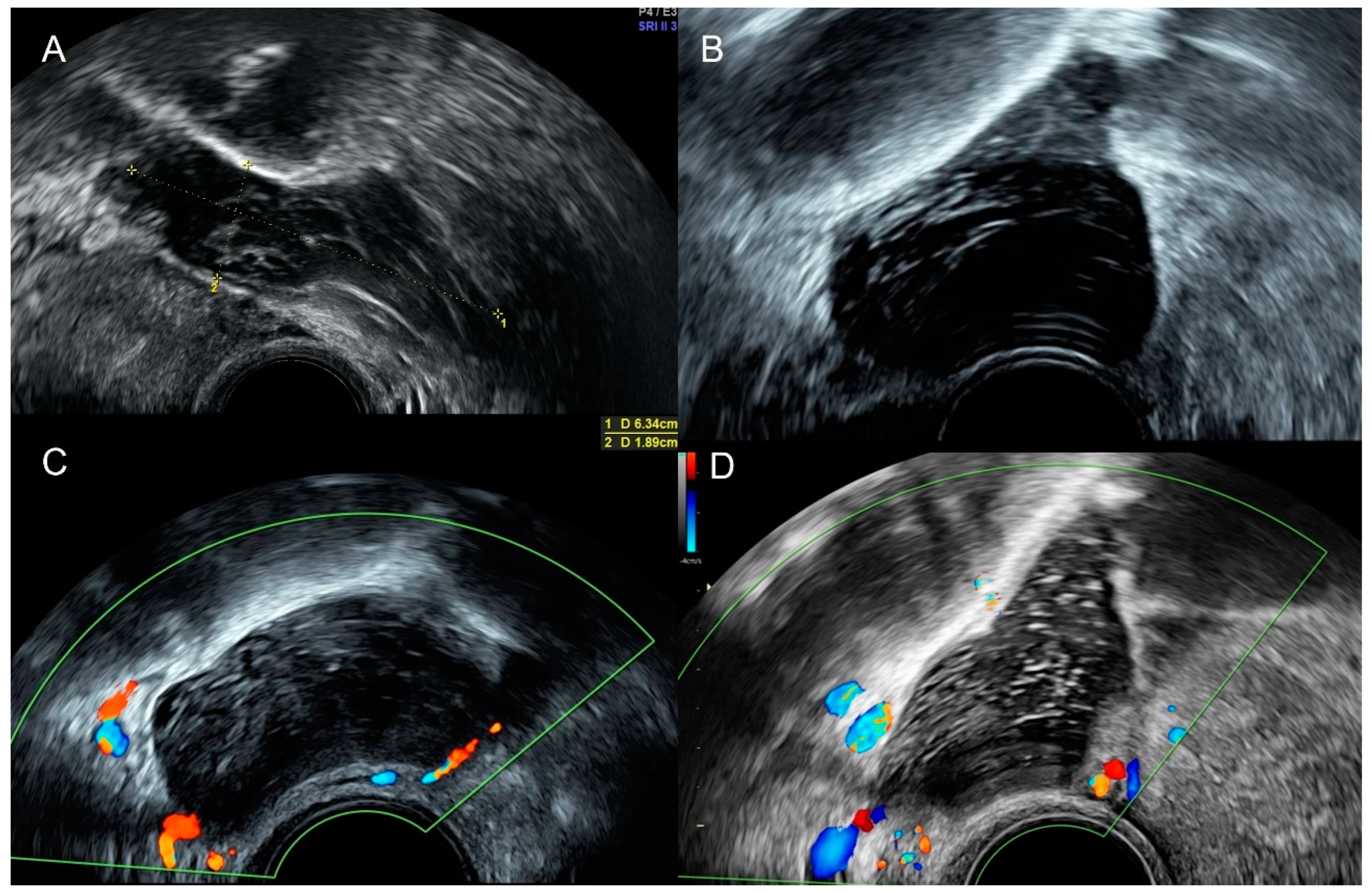
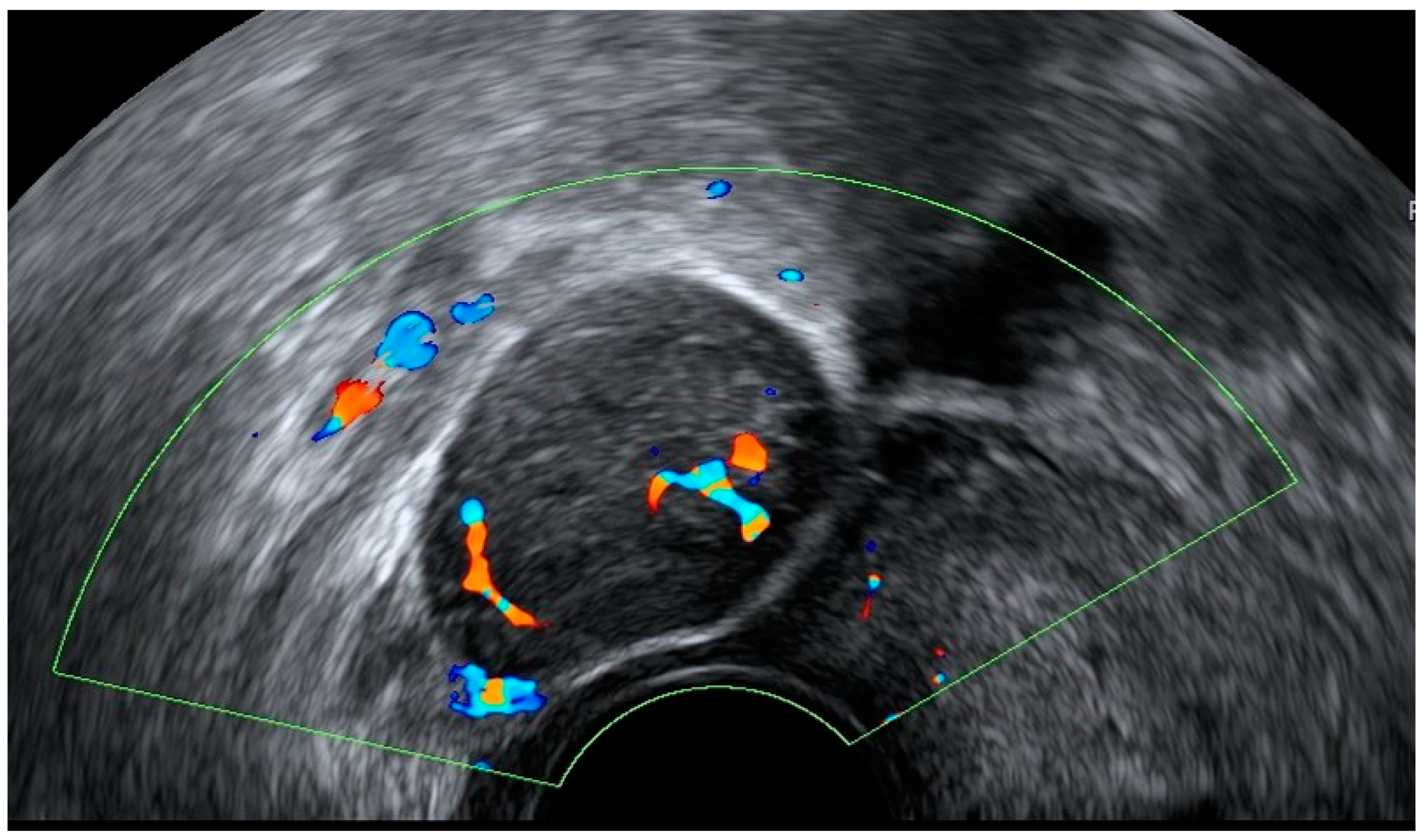
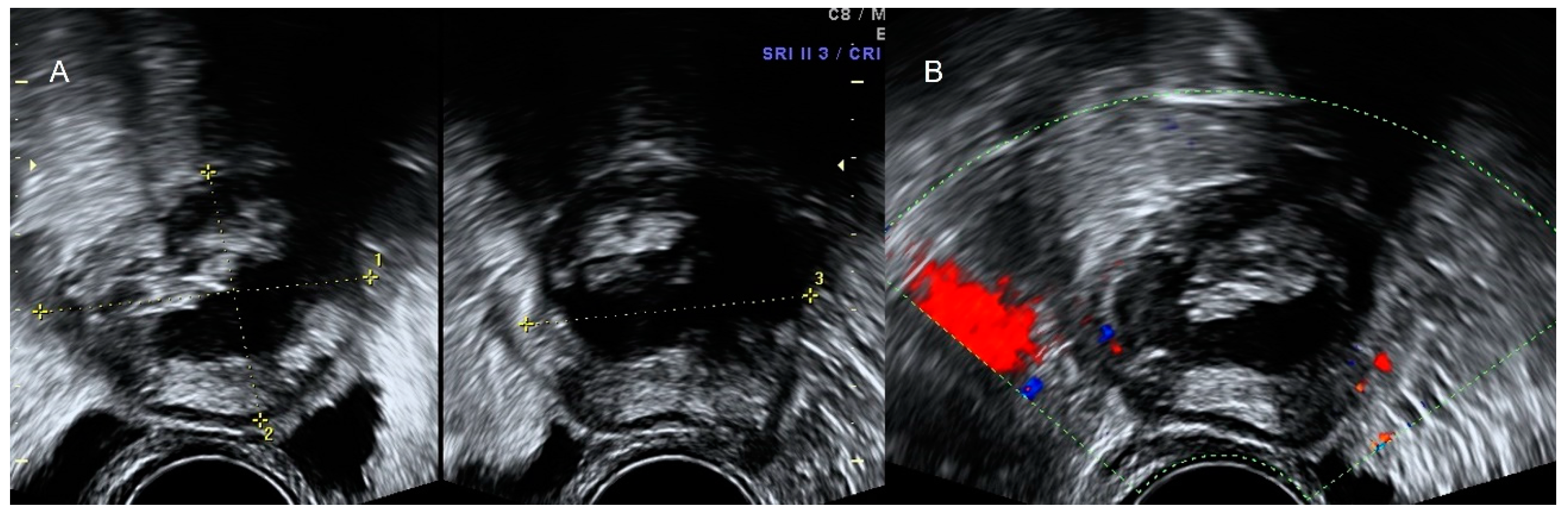
4.1. Pelvic Congestion
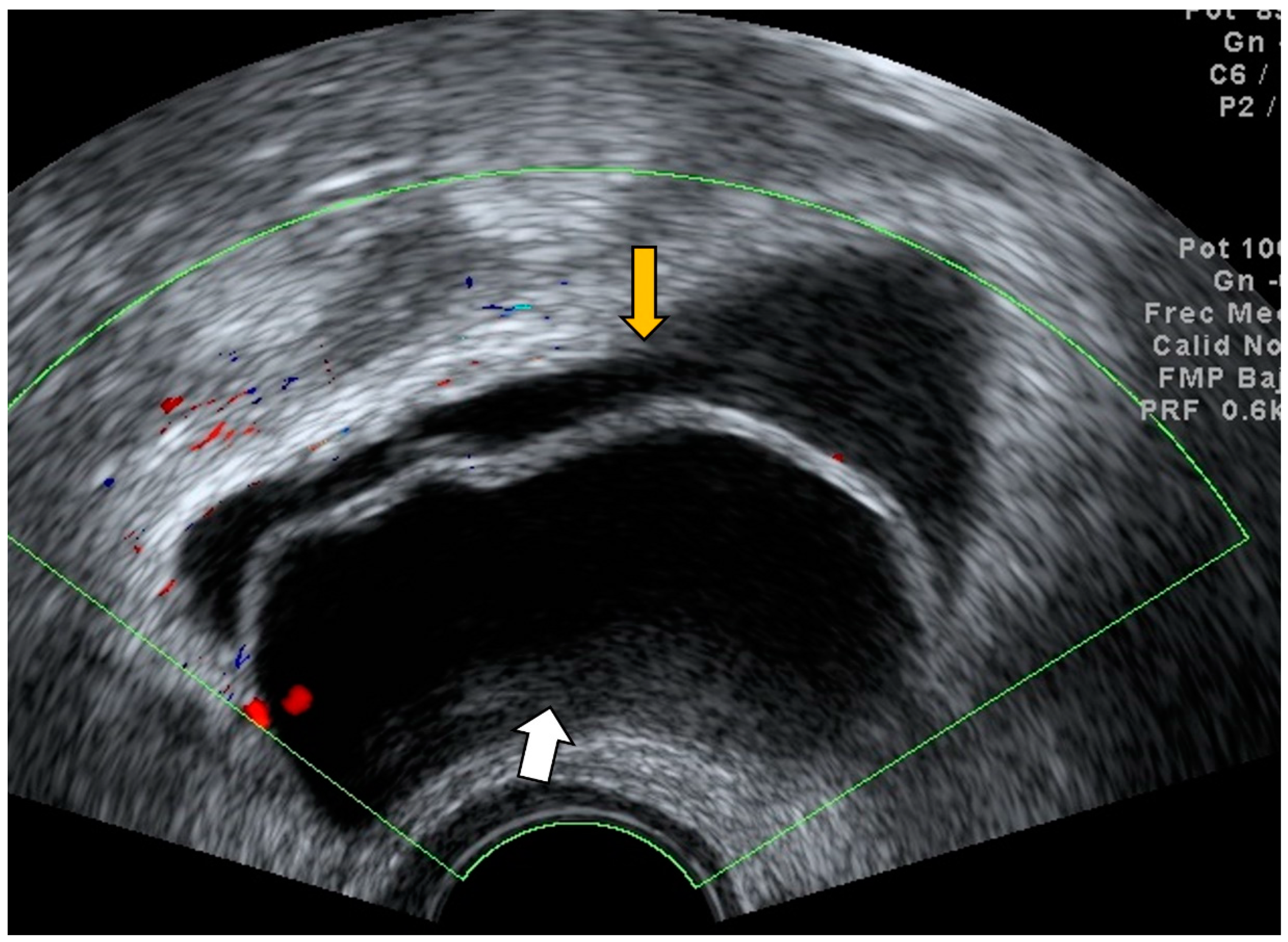
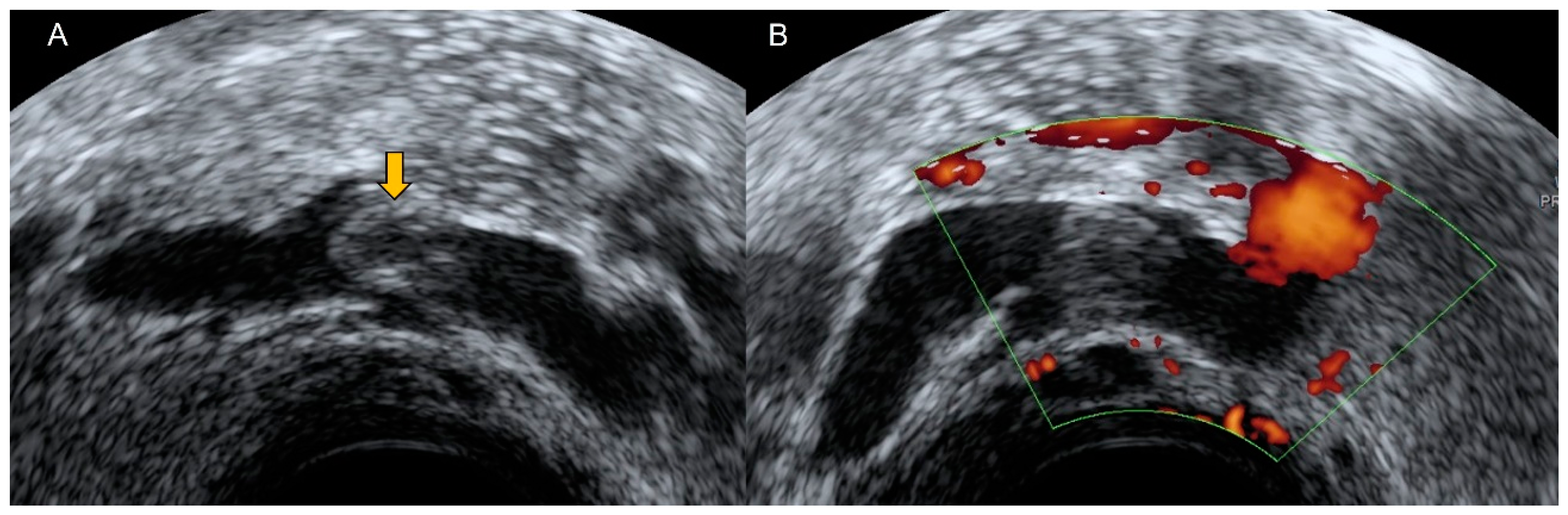
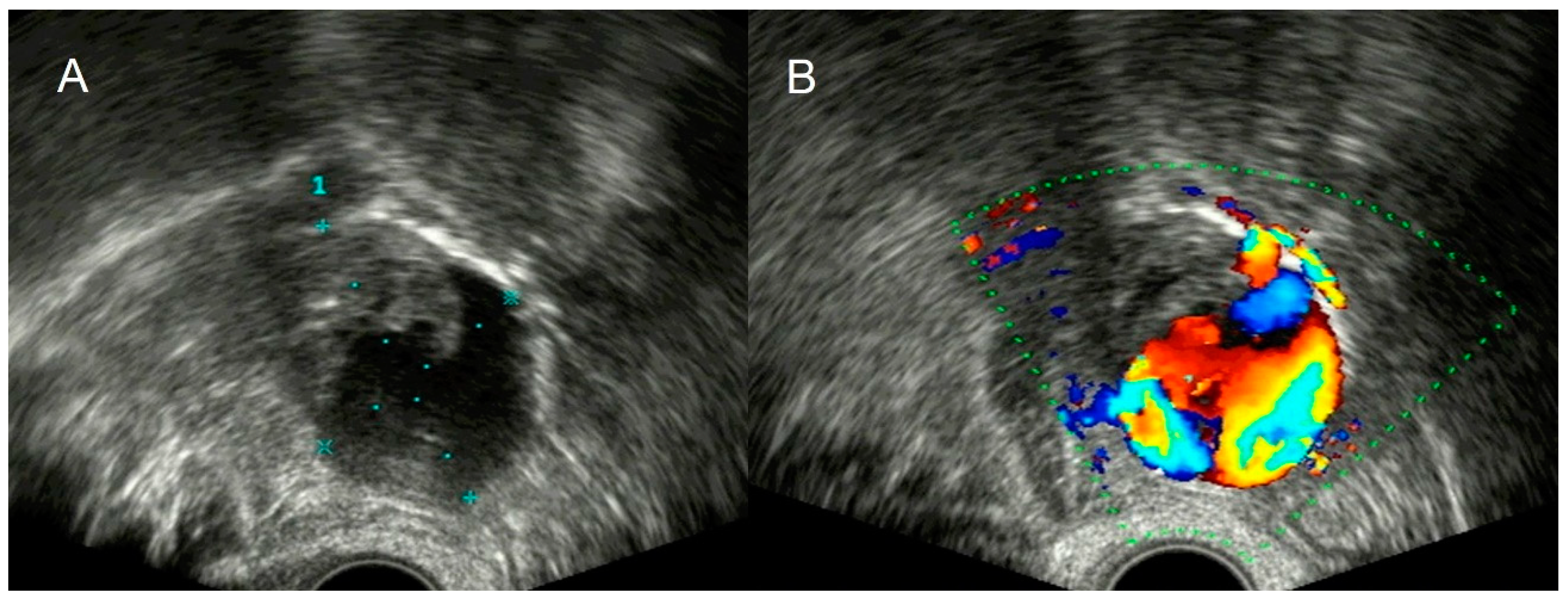
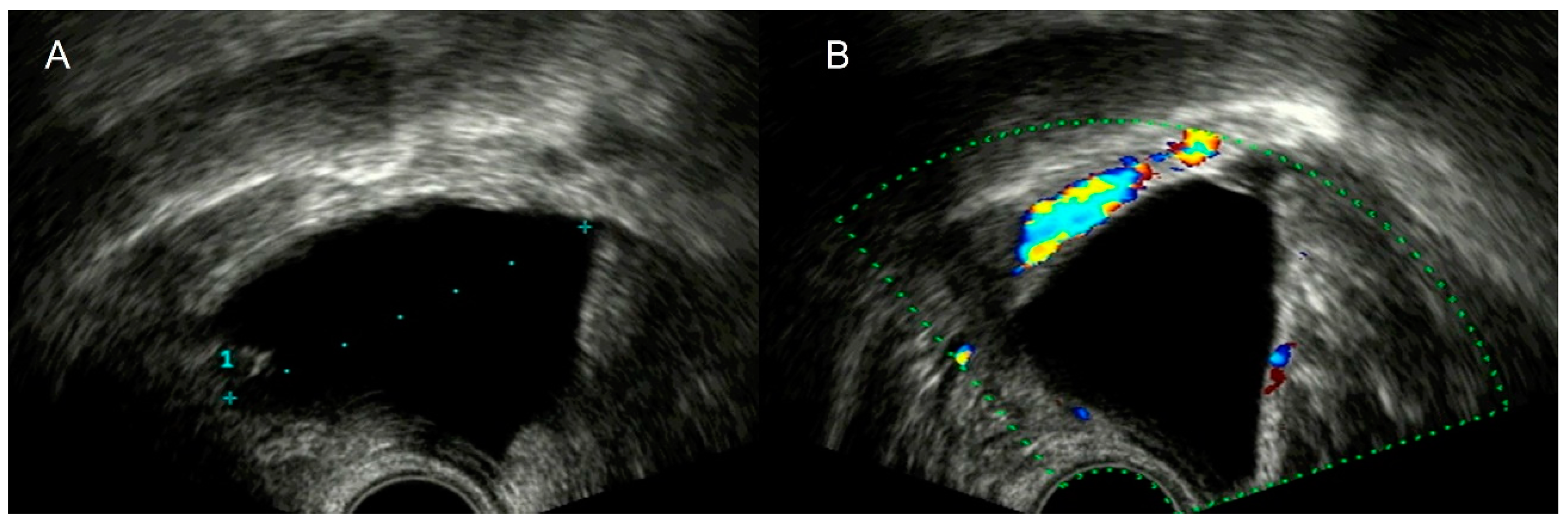
4.2. Thrombosis
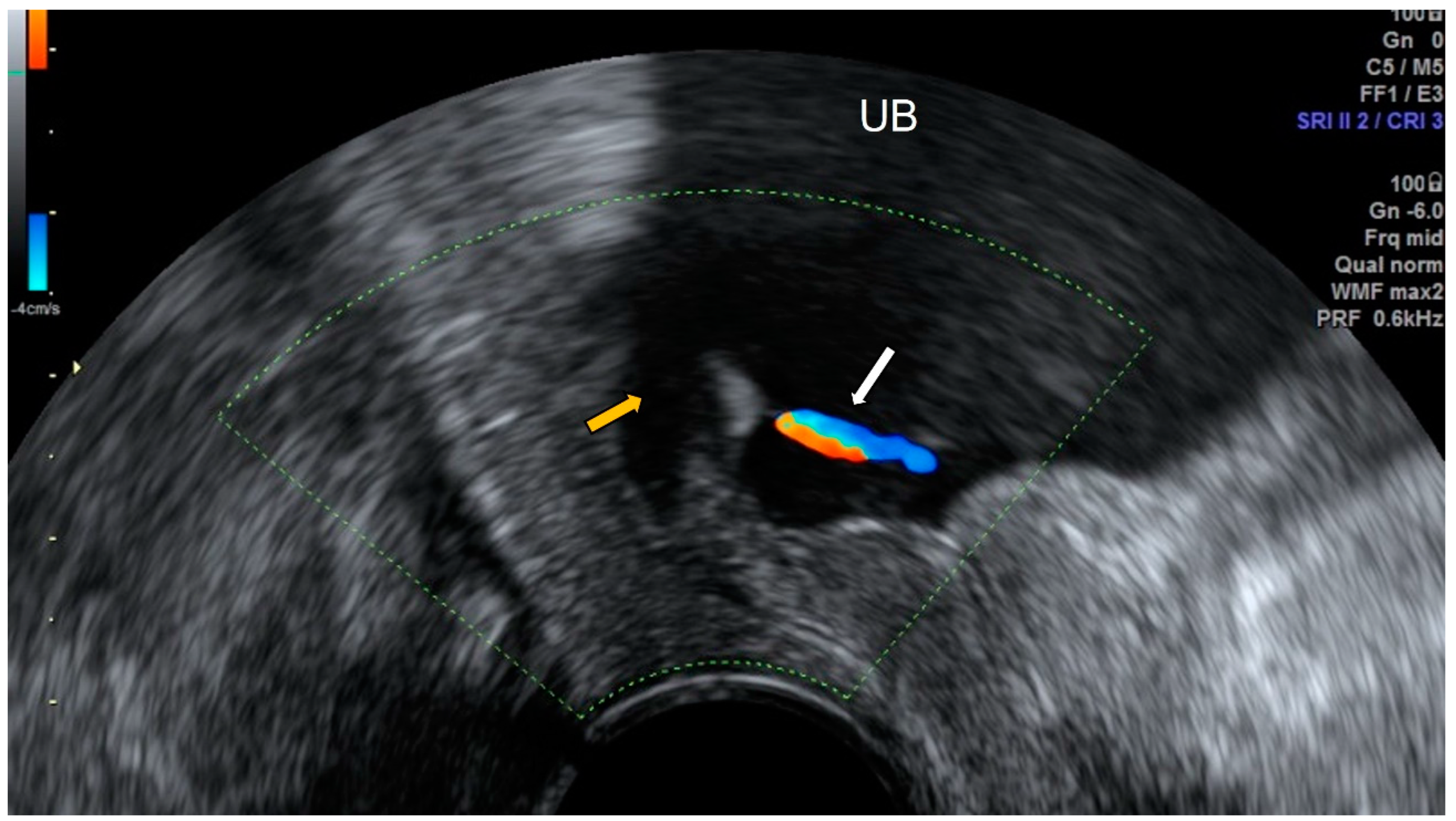
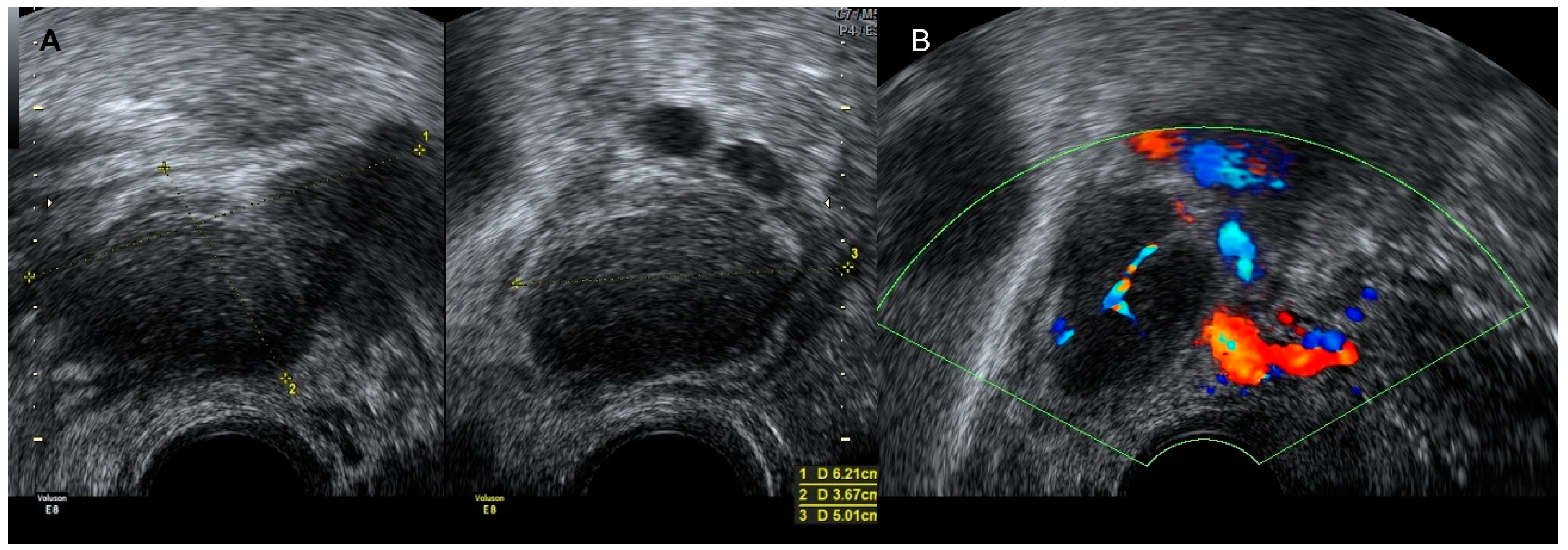
4.3. Aneurysm
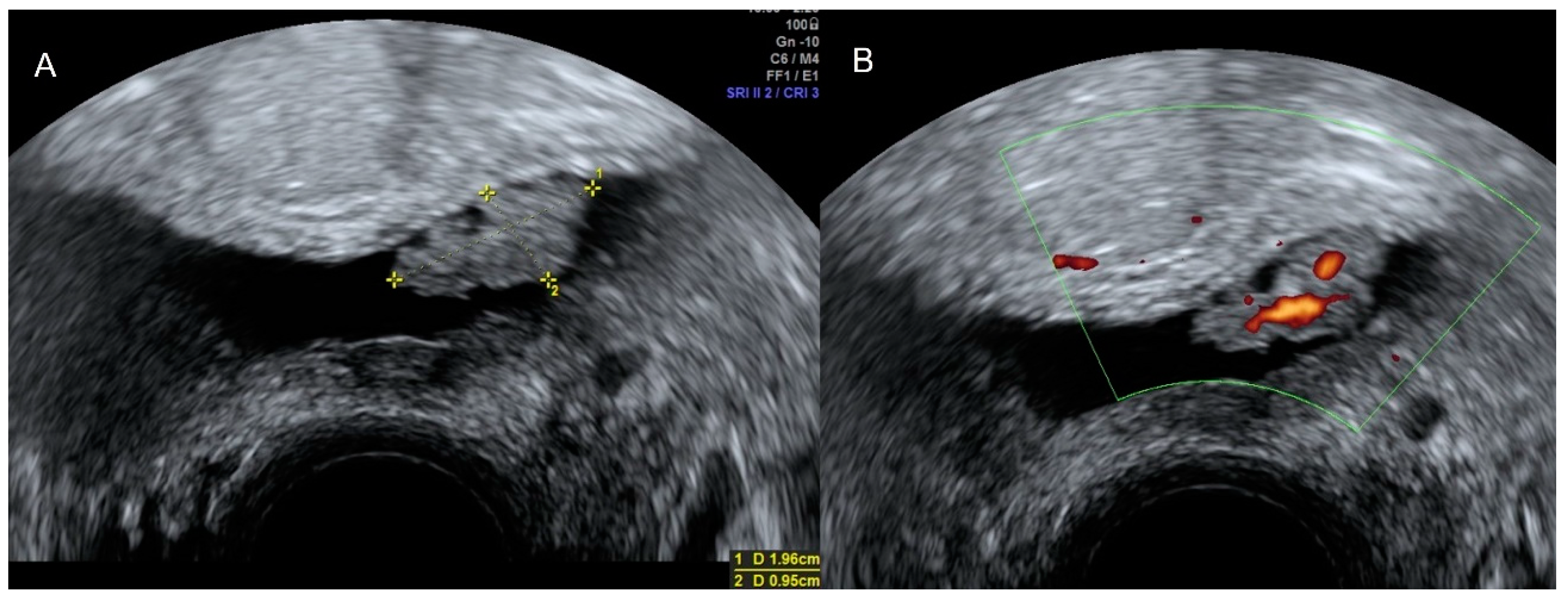
5. Lymphatic Imaging
6. Neurogenic Imaging
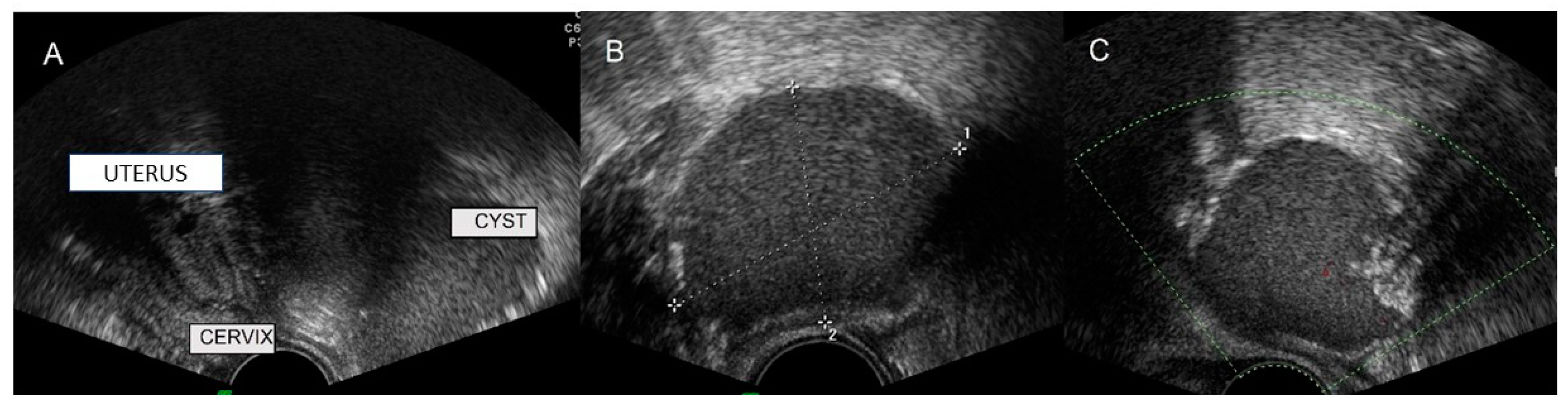
6.1. Tarlov Cyst
6.2. Neurogenic Tumors: Schwannoma and Neurofibroma
7. Soft-Tissues Images
8. Others
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Benacerraf, B.R.; Abuhamad, A.Z.; Bromley, B.; Goldstein, S.R.; Groszmann, Y.; Shipp, T.D.; Timor-Tritsch, I. Consider ultrasound first for imaging the female pelvis. Am. J. Obstet. Gynecol. 2015, 212, 450–455. [Google Scholar] [CrossRef] [PubMed]
- Minton, K.K.; Abuhamad, A.Z. 2012 Ultrasound First Forum proceedings. J. Ultrasound Med. 2013, 32, 555–566. [Google Scholar] [CrossRef] [PubMed]
- Loutradis, D.; Antsaklis, A.; Creatsas, G.; Hatzakis, A.; Kanakas, N.; Gougoulakis, A.; Michalas, S.; Aravantinos, D. The validity of gynecological ultrasonography. Gynecol. Obstet. Investig. 1990, 29, 47–50. [Google Scholar] [CrossRef]
- Beyer, D.; Schulte, B.; Kaiser, C. Ultrasound diagnosis of the acute abdomen. Bildgebung 1993, 60, 241–247. [Google Scholar] [PubMed]
- Recker, F.; Weber, E.; Strizek, B.; Gembruch, U.; Westerway, S.C.; Dietrich, C.F. Point-of-care ultrasound in obstetrics and gynecology. Arch. Gynecol. Obstet. 2021, 303, 871–876. [Google Scholar] [CrossRef]
- Roach, M.K.; Andreotti, R.F. The Normal Female Pelvis. Clin. Obstet. Gynecol. 2017, 60, 3–10. [Google Scholar] [CrossRef]
- D’Souza, N.; Nugent, K. Appendicitis. Am. Fam. Physician 2016, 93, 142–143. [Google Scholar]
- Wagner, J.M.; McKinney, W.P.; Carpenter, J.L. Does this patient have appendicitis? JAMA 1996, 276, 1589–1594. [Google Scholar] [CrossRef]
- Old, J.L.; Dusing, R.W.; Yap, W.; Dirks, J. Imaging for suspected appendicitis. Am. Fam. Physician 2005, 71, 71–78. [Google Scholar]
- Molander, P.; Paavonen, J.; Sjöberg, J.; Savelli, L.; Cacciatore, B. Transvaginal sonography in the diagnosis of acute appendicitis. Ultrasound Obstet. Gynecol. 2002, 20, 496–501. [Google Scholar] [CrossRef]
- Baba, T.F.; Mbar, W.T.M.; Lamine, D.M.; Aly, S.M.; Noel, T.J.; Mamadou, C.; Tidiane, T.C.; Ibrahima, K. Plastron appendiculaire: Intervention en urgence ou différée: À propos d’une série de 27 cas dans la clinique chirurgicale de l’Hôpital Aristide Le Dantec. Pan Afr. Med. J. 2018, 29, 15. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.M.; Al-Tarakji, M.; Shahid, F.; Qabani, A.S.; Shah, A.A.; Ahmed, K.; Khan, M.B.; Inamullah. From Diagnosis to Management; Mucocele of Stump Appendicitis, Extremely Rare Finding in an Uncommon Surgical Disease: Literature Review. Int. J. Surg. Oncol. 2021, 2021, 8816643. [Google Scholar] [CrossRef] [PubMed]
- Caspi, B.; Cassif, E.; Auslender, R.; Herman, A.; Hagay, Z.; Appelman, Z. The onion skin sign: A specific sonographic marker of appendiceal mucocele. J. Ultrasound Med. 2004, 23, 117–121. [Google Scholar] [CrossRef] [PubMed]
- Shaaban, A.M.; Rezvani, M.; Olpin, J.D.; Kennedy, A.M.; Gaballah, A.H.; Foster, B.R.; Menias, C.O.; Elsayes, K.M. Nongynecologic Findings Seen at Pelvic US. Radiographics 2017, 37, 2045–2062. [Google Scholar] [CrossRef][Green Version]
- Brenner, H.; Kloor, M.; Pox, C.P. Colorectal cancer. Lancet 2014, 383, 1490–1502. [Google Scholar] [CrossRef]
- Parab, T.M.; DeRogatis, M.J.; Boaz, A.M.; Grasso, S.A.; Issack, P.S.; Duarte, D.A.; Urayeneza, O.; Vahdat, S.; Qiao, J.H.; Hinika, G.S. Gastrointestinal stromal tumors: A comprehensive review. J. Gastrointest. Oncol. 2019, 10, 144–154. [Google Scholar] [CrossRef]
- Ambrosio, M.; Testa, A.C.; Moro, F.; Franchi, D.; Scifo, M.C.; Rams, N.; Epstein, E.; Alcazar, J.L.; Hidalgo, J.J.; Van Holsbeke, C.; et al. Imaging in gynecological disease: Clinical and ultrasound features of extra gastrointestinal stromal tumors (eGIST). Ultrasound Obstet. Gynecol. 2020, 56, 749–758. [Google Scholar] [CrossRef]
- Hodges, S.J.; Werle, D.; McLorie, G.; Atala, A. Megaureter. Sci. World J. 2010, 10, 603–612. [Google Scholar] [CrossRef]
- Ahmed, A. Ipsilateral Renal Agenesis With Megaureter, Blind End Proximal Ureter And Ureterocele In An Adult. J. Ayub. Med. Coll. Abbottabad 2017, 29, 150–153. [Google Scholar]
- Shimoya, K.; Shimizu, T.; Hashimoto, K.; Koyama, M.; Sawamura, A.; Murata, Y. Diagnosis of ureterocele with transvaginal sonography. Gynecol. Obstet. Investig. 2002, 54, 58–60. [Google Scholar] [CrossRef]
- Zhong, M.; Gersbach, E.; Rohan, S.M.; Yang, X.J. Primary Adenocarcinoma of the Urinary Bladder: Differential Diagnosis and Clinical Relevance. Arch. Pathol. Lab. Med. 2013, 137, 371–381. [Google Scholar] [CrossRef] [PubMed]
- Betsas, G.; Van Den Bosch, T.; Deprest, J.; Bourne, T.; Timmerman, D. The use of transvaginal ultrasonography to diagnose bladder carcinoma in women presenting with postmenopausal bleeding. Ultrasound Obstet. Gynecol. 2008, 32, 959–960. [Google Scholar] [CrossRef] [PubMed]
- Khougali, H.S.; Alawad, O.A.M.A.; Farkas, N.; Ahmed, M.M.M.; Abuagla, A.M. Bilateral pelvic kidneys with upper pole fusion and malrotation: A case report and review of the literature. J. Med. Case Rep. 2021, 15, 181. [Google Scholar] [CrossRef] [PubMed]
- Standring, S. Gray’s Anatomy. In The Anatomical Basis of Clinical Practice, 40th ed.; Elsevier: Amsterdam, The Netherlands, 2016. [Google Scholar]
- Pascual, M.A.; Browne, J.L. Pelvic Congestion Syndrome and Pelvic Adhesions. In Ultrasound of Pelvic Pain in the Non-Pregnant Female, 1st ed.; Alcazar, J.L., Pascual, M.A., Guerriero, S., Eds.; CRC Press: Boca Raton, FL, USA, 2019; pp. 122–139. [Google Scholar] [CrossRef]
- Rasche, H. Haemostasis and thrombosis: An overview. Eur. Heart J. Suppl. 2001, 3 (Suppl. Q), Q3–Q7. [Google Scholar] [CrossRef]
- Graupera, B.; Pascual, M.A.; Garcia, P.; Di Paola, R.; Ubeda, B.; Tresserra, F. Atypical ultrasonographic presentation of ovarian vein thrombosis. Eur. J. Gynaecol. Oncol. 2011, 32, 439–440. [Google Scholar]
- Parry, D.J.; Kessel, D.; Scott, D.J.A. Simplifying the internal iliac artery aneurysm. Ann. R. Coll. Surg. Engl. 2001, 83, 302–308. [Google Scholar]
- Weinberger, V.; Fischerova, D.; Semeradova, I.; Slama, J.; Cibula, D.; Zikan, M. Ultrasound characteristics of a symptomatic and asymptomatic lymphocele after pelvic and/or paraaortic lymphadenectomy. Taiwan J. Obstet. Gynecol. 2019, 58, 266–272. [Google Scholar] [CrossRef]
- Xiao, J.; Shao, Y.; Zhu, S.; He, X. Characteristics of adult abdominal cystic Lymphangioma: A single-center Chinese cohort of 12 cases. BMC Gastroenterol. 2020, 20, 244. [Google Scholar] [CrossRef]
- Jain, M.; Sahu, N.K.; Naik, S.; Bag, N.D. Symptomatic Tarlov cyst in cervical spine. BMJ Case Rep. 2018, 11, e228051. [Google Scholar] [CrossRef]
- Mastoraki, A.; Toska, F.; Tsiverdis, I.; Kyriazi, M.; Tsagkas, A.; Danias, N.; Smyrniotis, V.; Arkadopoulos, N. Retroperitoneal schwannomas: Dilemmas in diagnostic approach and therapeutic management. J. Gastrointest. Cancer 2013, 44, 371–374. [Google Scholar] [CrossRef]
- Belakhoua, S.M.; Rodriguez, F.J. Diagnostic Pathology of Tumors of Peripheral Nerve. Neurosurgery 2021, 88, 443–456. [Google Scholar] [CrossRef] [PubMed]
- Mentes, O.; Oysul, A.; Harlak, A.; Zeybek, N.; Kozak, O.; Tufan, T. Ultrasonography accurately evaluates the dimension and shape of the pilonidal sinus. Clinics 2009, 64, 189–192. [Google Scholar] [CrossRef] [PubMed]
- Kanat, B.H.; Kutluer, N.; Bozan, M.B.; Aksoy, N.; Öztürk, T. A forgotten status: Gossypiboma. Arq. Bras. Cir. Dig. 2021, 34, e1571. [Google Scholar] [CrossRef] [PubMed]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Graupera, B.; Pascual, M.Á.; Guerriero, S.; Browne, J.L.; Valero, B.; Ajossa, S.; Springer, S.; Alcázar, J.L. Extra-Gynecological Pelvic Pathology: A Challenge in the Differential Diagnosis of the Female Pelvis. Diagnostics 2022, 12, 1693. https://doi.org/10.3390/diagnostics12071693
Graupera B, Pascual MÁ, Guerriero S, Browne JL, Valero B, Ajossa S, Springer S, Alcázar JL. Extra-Gynecological Pelvic Pathology: A Challenge in the Differential Diagnosis of the Female Pelvis. Diagnostics. 2022; 12(7):1693. https://doi.org/10.3390/diagnostics12071693
Chicago/Turabian StyleGraupera, Betlem, Maria Ángela Pascual, Stefano Guerriero, Jean Laurent Browne, Beatriz Valero, Silvia Ajossa, Serena Springer, and Juan Luis Alcázar. 2022. "Extra-Gynecological Pelvic Pathology: A Challenge in the Differential Diagnosis of the Female Pelvis" Diagnostics 12, no. 7: 1693. https://doi.org/10.3390/diagnostics12071693
APA StyleGraupera, B., Pascual, M. Á., Guerriero, S., Browne, J. L., Valero, B., Ajossa, S., Springer, S., & Alcázar, J. L. (2022). Extra-Gynecological Pelvic Pathology: A Challenge in the Differential Diagnosis of the Female Pelvis. Diagnostics, 12(7), 1693. https://doi.org/10.3390/diagnostics12071693





