Comparison between Machine Learning and Multiple Linear Regression to Identify Abnormal Thallium Myocardial Perfusion Scan in Chinese Type 2 Diabetes
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Th-201 Scan
2.3. Laboratory Evaluation
2.4. Statistical Analysis:
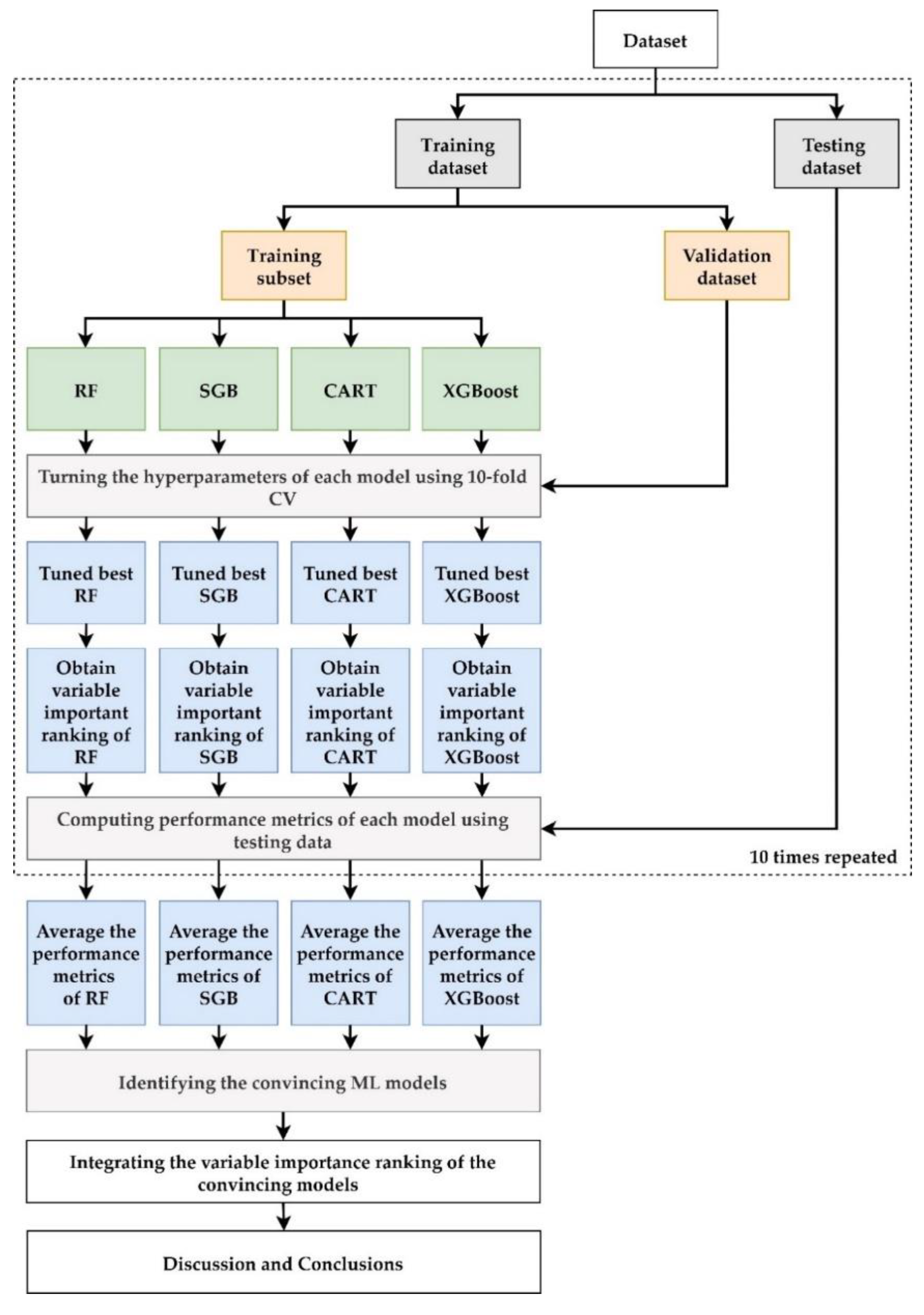
2.5. ML Methods and Proposed Scheme
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lo, C.J.; Tang, H.Y.; Huang, C.Y.; Lin, C.M.; Ho, H.Y.; Shiao, M.S.; Cheng, M.L. Metabolic Signature Differentiated Diabetes Mellitus from Lipid Disorder in Elderly Taiwanese. J. Clin. Med. 2018, 8, 13–27. [Google Scholar] [CrossRef] [PubMed]
- IDF Diabetes Atlas. Available online: https://www.diabetesatlas.org/data/en/country/194/tw.html (accessed on 1 May 2022).
- Sun, H.; Saeedi, P.; Karuranga, S.; Pinkepank, M.; Ogurtsova, K.; Duncan, B.B.; Stein, C.; Basit, A.; Chan, J.C.N.; Mbanya, J.C.; et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res. Clin. Pract. 2022, 183, 109119. [Google Scholar] [CrossRef] [PubMed]
- Emerging Risk Factors Collaboration; Di Angelantonio, E.; Kaptoge, S.; Wormser, D.; Willeit, P.; Butterworth, A.S.; Bansal, N.; O’Keeffe, L.M.; Gao, P.; Wood, A.M.; et al. Association of Cardiometabolic Multimorbidity With Mortality. JAMA 2015, 314, 52–60. [Google Scholar] [CrossRef] [PubMed]
- IDF Diabetes Atlas. 7th ed. 2015. Available online: www.idf.org/diabetesatlas (accessed on 1 May 2022).
- Morrish, N.J.; Wang, S.L.; Stevens, L.K.; Fuller, J.H.; Keen, H. Mortality and causes of death in the WHO Multinational Study of Vascular Disease in Diabetes. Diabetologia 2001, 44 (Suppl. S2), S14–S21. [Google Scholar] [CrossRef]
- Stamler, J.; Vaccaro, O.; Neaton, J.D.; Wentworth, D. Diabetes, other risk factors, and 12-yr cardiovascular mortality for men screened in the Multiple Risk Factor Intervention Trial. Diabetes Care 1993, 16, 434–444. [Google Scholar] [CrossRef]
- Schramm, T.K.; Gislason, G.H.; Kober, L.; Rasmussen, S.; Rasmussen, J.N.; Abildstrom, S.Z.; Hansen, M.L.; Folke, F.; Buch, P.; Madsen, M.; et al. Diabetes patients requiring glucose-lowering therapy and nondiabetics with a prior myocardial infarction carry the same cardiovascular risk: A population study of 3.3 million people. Circulation 2008, 117, 1945–1954. [Google Scholar] [CrossRef]
- Alabas, O.A.; Hall, M.; Dondo, T.B.; Rutherford, M.J.; Timmis, A.D.; Batin, P.D.; Deanfield, J.E.; Hemingway, H.; Gale, C.P. Long-term excess mortality associated with diabetes following acute myocardial infarction: A population-based cohort study. J. Epidemiol. Community Health 2017, 71, 25–32. [Google Scholar] [CrossRef]
- Arenja, N.; Mueller, C.; Ehl, N.F.; Brinkert, M.; Roost, K.; Reichlin, T.; Sou, S.M.; Hochgruber, T.; Osswald, S.; Zellweger, M.J. Prevalence, extent, and independent predictors of silent myocardial infarction. Am. J. Med. 2013, 126, 515–522. [Google Scholar] [CrossRef]
- Passa, P.; Drouin, P.; Issa-Sayegh, M.; Blasco, A.; Masquet, C.; Monassier, J.P.; Paillole, C. Coronary disease and diabetes. Diabete Metab. 1995, 21, 446–451. [Google Scholar]
- Anonymous. Consensus development conference on the diagnosis of coronary heart disease in people with diabetes: 10–11 February 1998, Miami, Florida. American Diabetes Association. Diabetes Care 1998, 21, 1551–1559. [Google Scholar] [CrossRef]
- Mark, D.B.; Hlatky, M.A.; Harrell, F.E., Jr.; Lee, K.L.; Califf, R.M.; Pryor, D.B. Exercise treadmill score for predicting prognosis in coronary artery disease. Ann. Intern. Med. 1987, 106, 793–800. [Google Scholar] [CrossRef] [PubMed]
- Mark, D.B.; Shaw, L.; Harrell, F.E., Jr.; Hlatky, M.A.; Lee, K.L.; Bengtson, J.R.; McCants, C.B.; Califf, R.M.; Pryor, D.B. Prognostic value of a treadmill exercise score in outpatients with suspected coronary artery disease. N. Engl. J. Med. 1991, 325, 849–853. [Google Scholar] [CrossRef] [PubMed]
- Giri, S.; Shaw, L.J.; Murthy, D.R.; Travin, M.I.; Miller, D.D.; Hachamovitch, R.; Borges-Neto, S.; Berman, D.S.; Waters, D.D.; Heller, G.V. Impact of diabetes on the risk stratification using stress single-photon emission computed tomography myocardial perfusion imaging in patients with symptoms suggestive of coronary artery disease. Circulation 2002, 105, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Scholte, A.J.; Schuijf, J.D.; Kharagjitsingh, A.V.; Dibbets-Schneider, P.; Stokkel, M.P.; van der Wall, E.E.; Bax, J.J. Prevalence and predictors of an abnormal stress myocardial perfusion study in asymptomatic patients with type 2 diabetes mellitus. Eur. J. Nucl. Med. Mol. Imaging 2009, 36, 567–575. [Google Scholar] [CrossRef] [PubMed]
- Koopaie, M.; Ghafourian, M.; Manifar, S.; Younespour, S.; Davoudi, M.; Kolahdooz, S.; Shirkhoda, M. Evaluation of CSTB and DMBT1 expression in saliva of gastric cancer patients and controls. BMC Cancer 2022, 22, 473. [Google Scholar] [CrossRef]
- Wang, C.; Li, Y.; Tsuboshita, Y.; Sakurai, T.; Goto, T.; Yamaguchi, H.; Yamashita, Y.; Sekiguchi, A.; Tachimori, H. Alzheimer’s Disease Neuroimaging I: A high-generalizability machine learning framework for predicting the progression of Alzheimer’s disease using limited data. NPJ Digit. Med. 2022, 5, 43. [Google Scholar] [CrossRef]
- Xu, S.; Arnetz, J.E.; Arnetz, B.B. Applying machine learning to explore the association between biological stress and near misses in emergency medicine residents. PLoS ONE 2022, 17, e0264957. [Google Scholar] [CrossRef]
- Steiner, H.E.; Giles, J.B.; Patterson, H.K.; Feng, J.; El Rouby, N.; Claudio, K.; Marcatto, L.R.; Tavares, L.C.; Galvez, J.M.; Calderon-Ospina, C.A.; et al. Machine Learning for Prediction of Stable Warfarin Dose in US Latinos and Latin Americans. Front. Pharmacol. 2021, 12, 749786. [Google Scholar] [CrossRef]
- Lin, Z.; Chou, W.C.; Cheng, Y.H.; He, C.; Monteiro-Riviere, N.A.; Riviere, J.E. Predicting Nanoparticle Delivery to Tumors Using Machine Learning and Artificial Intelligence Approaches. Int. J. Nanomed. 2022, 17, 1365–1379. [Google Scholar] [CrossRef]
- Mitchell, T.M. Machine Learning; New York McGraw Hill: New York, NY, USA, 1997. [Google Scholar]
- Ye, Y.; Xiong, Y.; Zhou, Q.; Wu, J.; Li, X.; Xiao, X. Comparison of Machine Learning Methods and Conventional Logistic Regressions for Predicting Gestational Diabetes Using Routine Clinical Data: A Retrospective Cohort Study. J. Diabetes Res. 2020, 2020, 4168340. [Google Scholar] [CrossRef]
- Marateb, H.R.; Mansourian, M.; Faghihimani, E.; Amini, M.; Farina, D. A hybrid intelligent system for diagnosing microalbuminuria in type 2 diabetes patients without having to measure urinary albumin. Comput. Biol. Med. 2014, 45, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Nusinovici, S.; Tham, Y.C.; Chak Yan, M.Y.; Wei Ting, D.S.; Li, J.; Sabanayagam, C.; Wong, T.Y.; Cheng, C.Y. Logistic regression was as good as machine learning for predicting major chronic diseases. J. Clin. Epidemiol. 2020, 122, 56–69. [Google Scholar] [CrossRef] [PubMed]
- Miller, D.D.; Brown, E.W. Artificial Intelligence in Medical Practice: The Question to the Answer? Am. J. Med. 2018, 131, 129–133. [Google Scholar] [CrossRef]
- Association, A.D. Introduction: The American Diabetes Association’s (ADA) evidence-based practice guidelines, standards, and related recommendations and documents for diabetes care. Diabetes Care 2012, 35 (Suppl. S1), S1–S2. [Google Scholar]
- Hachamovitch, R.; Berman, D.S.; Shaw, L.J.; Kiat, H.; Cohen, I.; Cabico, J.A.; Friedman, J.; Diamond, G.A. Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: Differential stratification for risk of cardiac death and myocardial infarction. Circulation 1998, 97, 535–543. [Google Scholar] [CrossRef] [PubMed]
- Gimelli, A.; Rossi, G.; Landi, P.; Marzullo, P.; Iervasi, G.; L’Abbate, A.; Rovai, D. Stress/Rest Myocardial Perfusion Abnormalities by Gated SPECT: Still the Best Predictor of Cardiac Events in Stable Ischemic Heart Disease. J. Nucl. Med. 2009, 50, 546–553. [Google Scholar] [CrossRef]
- Nakajima, K.; Yamasaki, Y.; Kusuoka, H.; Izumi, T.; Kashiwagi, A.; Kawamori, R.; Shimamoto, K.; Yamada, N.; Nishimura, T. Cardiovascular events in Japanese asymptomatic patients with type 2 diabetes: A 1-year interim report of a J-ACCESS 2 investigation using myocardial perfusion imaging. Eur. J. Nucl. Med. Mol Imaging 2009, 36, 2049–2057. [Google Scholar] [CrossRef] [PubMed]
- Tseng, C.J.; Lu, C.J.; Chang, C.C.; Chen, G.D.; Cheewakriangkrai, C. Integration of data mining classification techniques and ensemble learning to identify risk factors and diagnose ovarian cancer recurrence. Artif. Intell. Med. 2017, 78, 47–54. [Google Scholar] [CrossRef]
- Shih, C.C.; Lu, C.J.; Chen, G.D.; Chang, C.C. Risk Prediction for Early Chronic Kidney Disease: Results from an Adult Health Examination Program of 19,270 Individuals. Int. J. Environ. Res. Public Health 2020, 17, 4973. [Google Scholar] [CrossRef]
- Chang, C.C.; Chen, S.H. Developing a Novel Machine Learning-Based Classification Scheme for Predicting SPCs in Breast Cancer Survivors. Front. Genet. 2019, 10, 848. [Google Scholar] [CrossRef]
- Lee, T.S.; Chen, I.F.; Chang, T.J.; Lu, C.J. Forecasting Weekly Influenza Outpatient Visits Using a Two-Dimensional Hierarchical Decision Tree Scheme. Int. J. Environ. Res. Public Health 2020, 17, 4743. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.C.; Yeh, J.H.; Chen, Y.M.; Jhou, M.J.; Lu, C.J. Clinical Predictors of Prolonged Hospital Stay in Patients with Myasthenia Gravis: A Study Using Machine Learning Algorithms. J. Clin. Med. 2021, 10, 4393. [Google Scholar] [CrossRef] [PubMed]
- Chiu, Y.L.; Jhou, M.J.; Lee, T.S.; Lu, C.J.; Chen, M.S. Health Data-Driven Machine Learning Algorithms Applied to Risk Indicators Assessment for Chronic Kidney Disease. Risk Manag. Healthc Policy 2021, 14, 4401–4412. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.W.; Shen, H.L.; Lu, C.J.; Chen, S.H.; Chen, H.Y. Comparison of Different Machine Learning Classifiers for Glaucoma Diagnosis Based on Spectralis OCT. Diagnostics 2021, 11, 1718. [Google Scholar] [CrossRef]
- Wu, T.E.; Chen, H.A.; Jhou, M.J.; Chen, Y.N.; Chang, T.J.; Lu, C.J. Evaluating the Effect of Topical Atropine Use for Myopia Control on Intraocular Pressure by Using Machine Learning. J. Clin. Med. 2020, 10, 111. [Google Scholar] [CrossRef]
- Chang, C.C.; Yeh, J.H.; Chiu, H.C.; Chen, Y.M.; Jhou, M.J.; Liu, T.C.; Lu, C.J. Utilization of Decision Tree Algorithms for Supporting the Prediction of Intensive Care Unit Admission of Myasthenia Gravis: A Machine Learning-Based Approach. J. Pers. Med. 2022, 12, 32. [Google Scholar] [CrossRef]
- Breiman, L.F.J.; Olshen, R.A.; Stone, C.J. Classification and Regression Trees; Wadsworth, Champman & Hall/CRC: New York, NY, USA, 1984. [Google Scholar]
- Patel, N. US: Study of various decision tree pruning methods with their empirical comparison in WEKA. Int. J. Comp. Appl. 2012, 60, 20–25. [Google Scholar]
- Tierney, N.J.; Harden, F.A.; Harden, M.J.; Mengersen, K.L. Using decision trees to understand structure in missing data. BMJ Open 2015, 5, e007450. [Google Scholar] [CrossRef]
- Breiman, L. Random Forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef]
- Calle, M.L.; Urrea, V. Letter to the editor: Stability of Random Forest importance measures. Brief Bioinform. 2011, 12, 86–89. [Google Scholar] [CrossRef]
- Friedman, J.H. Greedy function approximation: A gradient boosting machine. Ann. Stat. 2001, 29, 1189–1232. [Google Scholar] [CrossRef]
- Friedman, J.H. Stochastic gradient boosting. Comput. Stat. Data Anal. 2002, 38, 367–378. [Google Scholar] [CrossRef]
- Chen, T.; Guestrin, C. XGBoost: A Scalable Tree Boosting System. In Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining; ACM: New York, NY, USA, 2016. [Google Scholar]
- Torlay, L.; Perrone-Bertolotti, M.; Thomas, E.; Baciu, M. Machine learning-XGBoost analysis of language networks to classify patients with epilepsy. Brain Inform. 2017, 4, 159–169. [Google Scholar] [CrossRef] [PubMed]
- Breiman, L.C.A.; Liaw, A.; Wiener, M. Randomforest: Breiman and Cutler’s Random Forests for Classification and Regression. R Package Version 4.6-14. 2022. Available online: https://cran.r-project.org/web/packages/randomForest/randomForest.pdf (accessed on 1 May 2022).
- Gbm: Generalized Boosted Regression Models. R Package Version 2.1.8. Available online: https://CRAN.R-project.org/package=gbm (accessed on 1 May 2022).
- Therneau, T.A.B. Rpart: Recursive Partitioning and Regression Trees. R Package Version 4.1-15. 2022. Available online: https://rdrr.io/cran/rpart/ (accessed on 1 May 2022).
- Chen, T.H.T.; Benesty, M.; Benesty, M.; Khotilovich, V.; Tang, Y.; Cho, H.; Chen, K.; Mitchell, R.; Cano, I.; Zhou, T.; et al. Xgboost: Ex-treme Gradient Boosting. R Package Version 1.5.0.2. 2022. Available online: https://oa.mg/author/A2126135973 (accessed on 1 May 2022).
- Kuhn, M. Caret: Classification and Regression Training. R Package Version 6.0-90. 2022. Available online: https://webcache.googleusercontent.com/search?q=cache:dFJOj8ytZqYJ:https://rdrr.io/cran/caret/+&cd=3&hl=zh-CN&ct=clnk&client=firefox-b-d (accessed on 1 May 2022).
- Alkhawam, H.; Nguyen, J.; Sayanlar, J.; Sogomonian, R.; Desai, R.; Jolly, J.; Vyas, N.; Syed, U.; Homsi, M.; Rubinstein, D. Coronary artery disease in patients with body mass index >/=30 kg/m(2): A retrospective chart analysis. J. Community Hosp. Intern. Med. Perspect. 2016, 6, 31483. [Google Scholar] [CrossRef] [PubMed]
- Wolk, R.; Berger, P.; Lennon, R.J.; Brilakis, E.S.; Somers, V.K. Body mass index: A risk factor for unstable angina and myocardial infarction in patients with angiographically confirmed coronary artery disease. Circulation 2003, 108, 2206–2211. [Google Scholar] [CrossRef]
- Katzel, L.I.; Sorkin, K.D.; Colman, E.; Goldberg, A.P.; Busby-Whitehead, M.J.; Lakatta, L.E.; Becker, L.C.; Lakatta, E.G.; Fleg, J.L. Risk factors for exercise-induced silent myocardial ischemia in healthy volunteers. Am. J. Cardiol. 1994, 74, 869–874. [Google Scholar] [CrossRef]
- Ades, P.A.; Savage, P.D. Obesity in coronary heart disease: An unaddressed behavioral risk factor. Circulation 2007, 104, 117–119. [Google Scholar]
- Colombo, M.G.; Kirchberger, I.; Amann, U.; Heier, M.; Thilo, C.; Kuch, B.; Peters, A.; Meisinger, C. Association between admission anemia and long-term mortality in patients with acute myocardial infarction: Results from the MONICA/KORA myocardial infarction registry. BMC Cardiovasc. Disord. 2018, 18, 50. [Google Scholar] [CrossRef]
- Kaul, S.; Alladi, S.; Mridula, K.R.; Bandaru, V.C.; Umamashesh, M.; Anjanikumar, D.; Lalitha, P.; Chandrasekhar, R. Prevalence and risk factors of asymptomatic carotid artery stenosis in Indian population: An 8-year follow-up study. Neurol. India 2017, 65, 279–285. [Google Scholar] [CrossRef]
- Ducrocq, G.; Simon, T.; Steg, P.G.; Investigators, R. Effect of Restrictive or Liberal Blood Transfusion on Major Cardiovascular Events in Patients With Acute Myocardial Infarction and Anemia-Reply. JAMA 2021, 325, 2506–2507. [Google Scholar] [CrossRef]
- Cook, J.R.; Dillie, K.S.; Hakeem, A.; Bhatti, S.; Chang, S.M. Effectiveness of anemia and chronic kidney disease as predictors for presence and severity of coronary artery disease in patients undergoing stress myocardial perfusion study. Am. J. Cardiol. 2008, 102, 266–271. [Google Scholar] [CrossRef] [PubMed]
- Al-Ahmad, A.; Rand, W.M.; Manjunath, G.; Konstam, M.A.; Salem, D.N.; Levey, A.S.; Sarnak, M.J. Reduced kidney function and anemia as risk factors for mortality in patients with left ventricular dysfunction. J. Am. Coll. Cardiol. 2001, 38, 955–962. [Google Scholar] [CrossRef]
- Metivier, F.; Marchais, S.J.; Guerin, A.P.; Pannier, B.; London, G.M. Pathophysiology of anaemia: Focus on the heart and blood vessels. Nephrol. Dial. Transplant. 2000, 15 (Suppl. S3), 14–18. [Google Scholar] [CrossRef] [PubMed]
- Curtis, A.B.; Karki, R.; Hattoum, A.; Sharma, U.C. Arrhythmias in Patients >/=80 Years of Age: Pathophysiology, Management, and Outcomes. J. Am. Coll. Cardiol. 2018, 71, 2041–2057. [Google Scholar] [CrossRef]
- Paneni, F.; Diaz Canestro, C.; Libby, P.; Luscher, T.F.; Camici, G.G. The Aging Cardiovascular System: Understanding It at the Cellular and Clinical Levels. J. Am. Coll. Cardiol. 2017, 69, 1952–1967. [Google Scholar] [CrossRef]
- Badimon, L.; Bugiardini, R.; Cubedo, J. Pathophysiology of acute coronary syndromes in the elderly. Int. J. Cardiol. 2016, 222, 1105–1109. [Google Scholar] [CrossRef]
- Srinivasan, M.P.; Kamath, P.K.; Bhat, N.M.; Pai, N.D.; Bhat, R.U.; Shah, T.D.; Singhal, A.; Mahabala, C. Severity of coronary artery disease in type 2 diabetes mellitus: Does the timing matter? Indian Heart J. 2016, 68, 158–163. [Google Scholar] [CrossRef][Green Version]
- van Wijngaarden, R.P.T.; Overbeek, J.A.; Heintjes, E.M.; Schubert, A.; Diels, J.; Straatman, H.; Steyerberg, E.W.; Herings, R.M.C. Relation Between Different Measures of Glycemic Exposure and Microvascular and Macrovascular Complications in Patients with Type 2 Diabetes Mellitus: An Observational Cohort Study. Diabetes Ther. 2017, 8, 1097–1109. [Google Scholar] [CrossRef]
- Zhao, W.; Katzmarzyk, P.T.; Horswell, R.; Wang, Y.; Johnson, J.; Hu, G. HbA1c and coronary heart disease risk among diabetic patients. Diabetes Care 2014, 37, 428–435. [Google Scholar] [CrossRef]
- Holman, R.R.; Paul, S.K.; Bethel, M.A.; Matthews, D.R.; Neil, H.A. 10-year follow-up of intensive glucose control in type 2 diabetes. N. Engl. J. Med. 2008, 359, 1577–1589. [Google Scholar] [CrossRef]
- Fox, C.S.; Larson, M.G.; Leip, E.P.; Culleton, B.; Wilson, P.W.; Levy, D. Predictors of new-onset kidney disease in a community-based population. JAMA 2004, 291, 844–850. [Google Scholar] [CrossRef]
- Go, A.S.; Chertow, G.M.; Fan, D.; McCulloch, C.E.; Hsu, C.Y. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N. Engl. J. Med. 2004, 351, 1296–1305. [Google Scholar] [CrossRef]
- Rosendorff, C.; Lackland, D.T.; Allison, M.; Aronow, W.S.; Black, H.R.; Blumenthal, R.S.; Cannon, C.P.; de Lemos, J.A.; Elliott, W.J.; Findeiss, L.; et al. Treatment of hypertension in patients with coronary artery disease: A scientific statement from the American Heart Association, American College of Cardiology, and American Society of Hypertension. Hypertension 2015, 65, 1372–1407. [Google Scholar] [CrossRef] [PubMed]
- Escobar, E. Hypertension and coronary heart disease. J. Hum. Hypertens 2002, 16 (Suppl. S1), S61–S63. [Google Scholar] [CrossRef] [PubMed]
- Chen, I.; Lu, C.J. Sales forecasting by combining clustering and machine-learning techniques for computer retailing. Neural. Comput. Applic. 2017, 28, 2633–2647. [Google Scholar] [CrossRef]
- Jiang, F.; Jiang, Y.; Zhi, H.; Dong, Y.; Li, H.; Ma, S.; Wang, Y.; Dong, Q.; Shen, H.; Wang, Y. Artificial intelligence in healthcare: Past, present and future. Stroke Vasc. Neurol. 2017, 2, 230–243. [Google Scholar] [CrossRef]
- Koteluk, O.; Wartecki, A.; Mazurek, S.; Kolodziejczak, I.; Mackiewicz, A. How Do Machines Learn? Artificial Intelligence as a New Era in Medicine. J. Pers. Med. 2021, 11, 32. [Google Scholar] [CrossRef]

| Variables | Description | Unit |
|---|---|---|
| V1: Sex | Male/Female | - |
| V2: Age | Patient age | year |
| V3: Body mass index | Body mass index | Kg/m2 |
| V4: Duration of diabetes | Duration of diabetes | year |
| V5: Smoking | No/Yes | - |
| V9: Glycated hemoglobin | HbA1c (Glycated hemoglobin) | % |
| V10: Triglyceride | Triglyceride baseline | mg/dL |
| V11:High density lipoprotein cholesterol | High-Density Lipoprotein Cholesterol | mg/dL |
| V12: Low density lipoprotein cholesterol | Low-Density Lipoprotein Cholesterol | mg/dL |
| V13: Alanine aminotransferase baseline | Alanine aminotransferase | U/L |
| V14: Creatinine | Creatinine | mg/dL |
| V6: Systolic blood pressure | Systolic blood pressure | mmHg |
| V7: Diastolic blood pressure | Diastolic blood pressure b | mmHg |
| V8: Hemoglobin | Hb | |
| V15: Microalbuminuria | Urine albumin to creatinine ratio = microalbumin (mg/dL)/urine creatinine(mg/dL) | mg/g |
| Metrics | Calculation * |
|---|---|
| SMAPE | |
| RAE | |
| RRSE | |
| RMSE |
| Variables | Mean ± SD | N |
|---|---|---|
| Age | 68.09 ± 10.07 | 796 |
| Body mass index | 26.17 ± 3.89 | 588 |
| Duration of diabetes | 13.81 ± 8.02 | 589 |
| Fasting plasma glucose | 150.09 ± 46.05 | 591 |
| Glycated hemoglobin | 7.68 ± 1.39 | 590 |
| Triglyceride | 123.65 ± 79.32 | 586 |
| High-density lipoprotein cholesterol | 49.53 ± 14.98 | 524 |
| Low-density lipoprotein cholesterol | 95.52 ± 26.18 | 588 |
| Alanine aminotransferase baseline | 23.66 ± 13.60 | 588 |
| Creatinine | 1.16 ± 0.99 | 587 |
| Systolic blood pressure | 131.08± 15.36 | 514 |
| Diastolic blood pressure | 73.35 ± 10.09 | 514 |
| Microalbuminuria | 196.53± 723.55 | 551 |
| N (%) | N | |
| Sex | 796 | |
| Male | 369 (53.64%) | |
| Female | 427 (46.36%) | |
| Smoking | 329 | |
| No | 212 (64.44%) | |
| Yes | 117 (35.56%) |
| Mean (SD) | SMAPE | RAE | RRSE | RMSE |
|---|---|---|---|---|
| MLR | 1.120(0.04) | 1.049(0.06) | 1.054(0.03) | 7.760(0.39) |
| RF | 1.070(0.03) | 1.043(0.05) | 1.042(0.02) | 7.683(0.48) |
| SGB | 1.074(0.03) | 1.026(0.05) | 1.039(0.03) | 7.661(0.45) |
| CART | 1.055(0.04) | 1.031(0.06) | 1.049(0.03) | 7.736(0.56) |
| XGBoost | 1.058(0.04) | 1.017(0.05) | 1.032(0.02) | 7.613(0.58) |
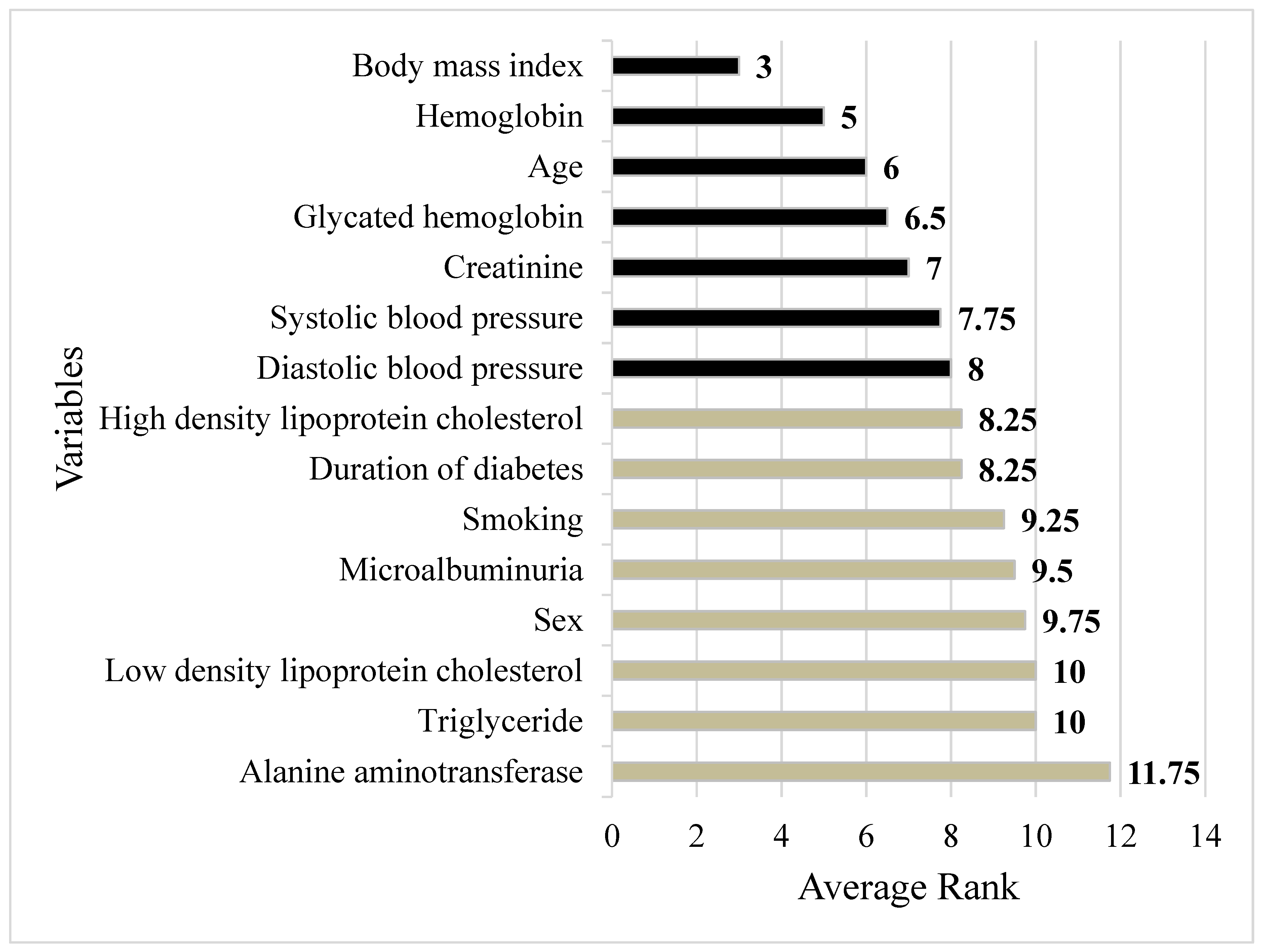
| Variables | RF | SGB | CART | XGBoost | Average |
|---|---|---|---|---|---|
| Sex | 5 | 14 | 6 | 14 | 9.75 |
| Age | 2 | 4 | 3 | 15 | 6 |
| Body mass index | 4 | 1 | 1 | 6 | 3 |
| Duration of diabetes | 1 | 13 | 11 | 8 | 8.25 |
| Smoking | 6 | 15 | 15 | 1 | 9.25 |
| Hemoglobin | 8 | 6 | 4 | 2 | 5 |
| Glycated hemoglobin | 9 | 2 | 5 | 10 | 6.5 |
| Triglyceride | 10 | 10 | 8 | 12 | 10 |
| High density lipoprotein cholesterol | 11 | 7 | 10 | 5 | 8.25 |
| Low density lipoprotein cholesterol | 12 | 5 | 12 | 11 | 10 |
| Alanine aminotransferase baseline | 13 | 8 | 13 | 13 | 11.75 |
| Creatinine | 14 | 3 | 2 | 9 | 7 |
| Systolic blood pressure | 7 | 11 | 9 | 4 | 7.75 |
| Diastolic blood pressure | 3 | 12 | 14 | 3 | 8 |
| Microalbuminuria | 15 | 9 | 9 | 9 | 9.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, J.-D.; Pei, D.; Chen, F.-Y.; Wu, C.-Z.; Lu, C.-H.; Huang, L.-Y.; Kuo, C.-H.; Kuo, S.-W.; Chen, Y.-L. Comparison between Machine Learning and Multiple Linear Regression to Identify Abnormal Thallium Myocardial Perfusion Scan in Chinese Type 2 Diabetes. Diagnostics 2022, 12, 1619. https://doi.org/10.3390/diagnostics12071619
Lin J-D, Pei D, Chen F-Y, Wu C-Z, Lu C-H, Huang L-Y, Kuo C-H, Kuo S-W, Chen Y-L. Comparison between Machine Learning and Multiple Linear Regression to Identify Abnormal Thallium Myocardial Perfusion Scan in Chinese Type 2 Diabetes. Diagnostics. 2022; 12(7):1619. https://doi.org/10.3390/diagnostics12071619
Chicago/Turabian StyleLin, Jiunn-Diann, Dee Pei, Fang-Yu Chen, Chung-Ze Wu, Chieh-Hua Lu, Li-Ying Huang, Chun-Heng Kuo, Shi-Wen Kuo, and Yen-Lin Chen. 2022. "Comparison between Machine Learning and Multiple Linear Regression to Identify Abnormal Thallium Myocardial Perfusion Scan in Chinese Type 2 Diabetes" Diagnostics 12, no. 7: 1619. https://doi.org/10.3390/diagnostics12071619
APA StyleLin, J.-D., Pei, D., Chen, F.-Y., Wu, C.-Z., Lu, C.-H., Huang, L.-Y., Kuo, C.-H., Kuo, S.-W., & Chen, Y.-L. (2022). Comparison between Machine Learning and Multiple Linear Regression to Identify Abnormal Thallium Myocardial Perfusion Scan in Chinese Type 2 Diabetes. Diagnostics, 12(7), 1619. https://doi.org/10.3390/diagnostics12071619






