Echocardiography in Prone Positioned Critically Ill Patients: A Wealth of Information from a Single View
Abstract
:1. Introduction
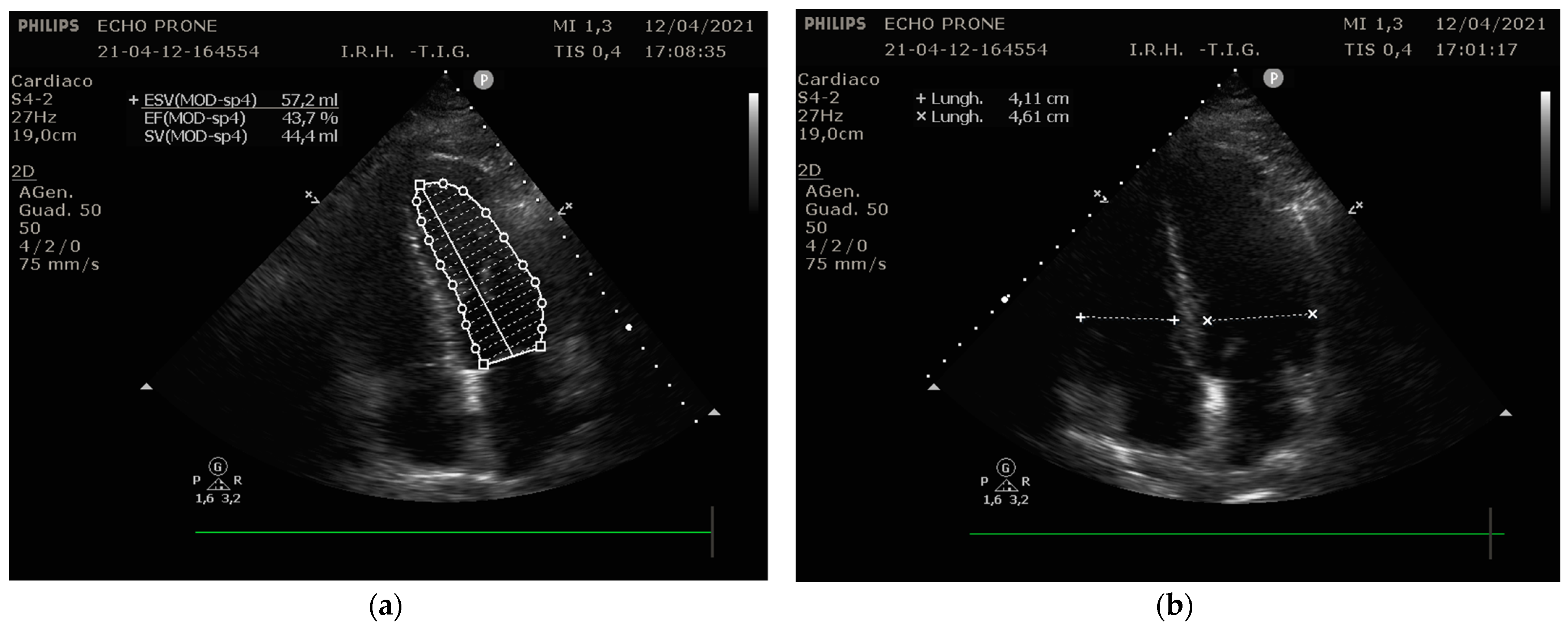
2. Technique Proposal
3. Literature Review
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Taccone, P.; Pesenti, A.; Latini, R.; Polli, F.; Vagginelli, F.; Mietto, C.; Caspani, L.; Raimondi, F.; Bordone, G.; Iapichino, G. Prone positioning in patients with moderate and severe acute respiratory distress syndrome: A randomized controlled trial. J. Am. Med. Assoc. 2009, 302, 1977–1984. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marini, J.J.; Gattinoni, L. Management of COVID-19 respiratory dis- tress. Am. Med. Assoc. 2020, 24, E1–E2. [Google Scholar]
- Gattinoni, L.; Coppola, S.; Cressoni, M.; Busana, M.; Rossi, S.; Chiumello, D. Covid-19 does not lead to a “typical” acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 2020, 201, 1299–1300. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gattinoni, L.; Chiumello, D.; Rossi, S. COVID-19 pneumonia: ARDS or not? Crit. Care 2020, 24, 154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zochios, V.; Parhar, K.; Tunnicliffe, W.; Roscoe, A.; Gao, F. The right ventricle in ARDS. Chest 2017, 152, 181–193. [Google Scholar] [CrossRef]
- Mekontso Dessap, A.; Proost, O.; Boissier, F.; Louis, B.; Roche Campo, F.; Brochard, L. Transesophageal echocardiography in prone position during severe acute respiratory distress syndrome. Intensive Care Med. 2011, 37, 430–434. [Google Scholar] [CrossRef]
- Giustiniano, E.; Bragato, R.M.; Padua, E.; Negri, K.; Cecconi, M. Echocardiography during prone-position mechanical ventilation in patients with COVID-19: A proposal for a new approach. J. Am. Soc. Echocardiogr. 2020, 33, 905–906. [Google Scholar] [CrossRef]
- Giustiniano, E.; Fazzari, F.; Bragato, R.M.; Curzi, M.; Cecconi, M. Trans-thoracic Echocardiography in Prone Positioning COVID-19 Patients: A Small Case Series. SN Compr. Clin. Med. 2020, 2, 2381–2386. [Google Scholar] [CrossRef]
- Ajam, M.; Drake, M.; Ran, R.; Mukundan, S.; Masri, A.; Rahmouni, H. Approach to echocardiography in ARDS patients in the prone position: A systematic review. Echocardiography 2022, 39, 330–338. [Google Scholar] [CrossRef]
- Ciozda, W.; Kedan, I.; Kehl, D.W.; Zimmer, R.; Khandwalla, R.; Kimchi, A. The efficacy of sonographic measurement of inferior vena cava diameter as an estimate of central venous pressure. Cardiovasc. Ultrasound 2015, 14, 33. [Google Scholar] [CrossRef] [Green Version]
- Ugalde, D.; Medel, J.N.; Mercado, P.; Pairumani, R.; Eisen, D.; Petruska, E.; Montoya, J.; Morales, F.; Araya, C.; Valenzuela, E.D. Critical care echocardiography in prone position patients during COVID-19 pandemic: A feasibility study. J. Ultrasound 2022, 1–5. [Google Scholar] [CrossRef]
- Gibson, L.E.; di Fenza, R.; Berra, L.; Bittner, E.A.; Chang, M.G. Transthoracic echocardiography in prone patients with acute respiratory distress syndrome: A feasibility study. Crit. Care Explor. 2020, 2, e0179. [Google Scholar] [CrossRef]
- García-Cruz, E.; Manzur-Sandoval, D.; Gopar-Nieto, R.; Murillo-Ochoa, A.L.; Bejarano-Alva, G.; Rojas-Velasco, G.; Álvarez-Álvarez, R.J.; Baranda-Tovar, F. Transthoracic echocardiography during prone position ventilation: Lessons from the COVID-19 pandemic. J. Am. Coll. Emerg. Physicians Open 2020, 1, 730–736. [Google Scholar] [CrossRef]
- Marvaki, A.; Papachristidis, A.; Nakou, E.; Toth, E.; O’Gallagher, K.; Fisher, R.; Shah, A.M.; Monaghan, M.J. Innovative transthoracic echocardiographic imaging on prone ventilated patients with COVID-19 using a transesophageal probe. JACC Cardiovasc. Imaging 2020, 13, 2465–2467. [Google Scholar] [CrossRef]
- Roemer, S.; Kaminski, A.; Payne, A.; Tanel, E.; Perez Moreno, A.C.; Jaglan, A.; Khandheria, B.K. Feasibility of Transthoracic Imaging of the Heart in the Prone Position. J. Am. Soc. Echocardiogr. 2020, 33, 1147–1148. [Google Scholar] [CrossRef]
- Santos-Martínez, L.E.; Mendoza-Copa, G.; García-Cruz, E.; Álvarez-Álvarez, R.J.; Bucio-Reta, R.E.; González-Ruiz, F.J.; Ramos-Enríquez, Á.; Hernández-Márquez, M.Á.; Baranda-Tovar, F.M. Feasibility in the echocardiographic estimation of parameters of the right ventricle in prone position. Arch Cardiol. Mex. 2020, 90, 130–137. [Google Scholar] [CrossRef]
- Taha, H.S.; Mohamed, A.M.; Mahrous, H.A.; Shaker, M.M.; Alsayed, O.S.; Sayed, H.G.; Rizk, H.H.; Abdelwahab, M.A. Correlation of echocardiographic parameters in prone and supine positions in normal adults using a novel approach. Echocardiography 2021, 38, 892–900. [Google Scholar] [CrossRef]
- Dharmavaram, S.; Jellish, W.S.; Nockels, R.P.; Shea, J.; Mehmood, R.; Ghanayem, A.; Kleinman, B.; Jacobs, W. Effect of prone positioning systems on hemodynamic and cardiac function during lumbar spine surgery: An echocardiographic study. Spine 2006, 31, 1388–1393. [Google Scholar] [CrossRef]
- Meirelles Almeida, C.A.; Nedel, W.L.; Morais, V.D.; Boniatti, M.M.; de Almeida-Filho, O.C. Diastolic dysfunction as a predictor of weaning failure: A systematic review and meta-analysis. J. Crit. Care 2016, 34, 135–141. [Google Scholar] [CrossRef]
- McMurray, J.J.; Adamopoulos, S.; Anker, S.D.; Auricchio, A.; Böhm, M.; Dickstein, K.; Falk, V.; Filippatos, G.; Fonseca, C.; Gomez-Sanchez, M.A.; et al. ESC Committee for Practice Guidelines. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2012, 33, 1787–1847. [Google Scholar] [CrossRef]
- Repessé, X.; Charron, C.; Vieillard-Baron, A. Right ventricular failure in acute lung injury and acute respiratory distress syndrome. Minerva Anestesiol. 2012, 78, 941–948. [Google Scholar]
- Sato, R.; Dugar, S.; Cheungpasitporn, W.; Schleicher, M.; Collier, P.; Vallabhajosyula, S.; Duggal, A. The impact of right ventricular injury on the mortality in patients with acute respiratory distress syndrome: A systematic review and meta-analysis. Crit. Care 2021, 25, 172. [Google Scholar] [CrossRef]
- Ugalde, D.; Medel, J.N.; Romero, C.; Cornejo, R. Transthoracic cardiac ultrasound in prone position: A technique variation description. Intensive Care Med. 2018, 44, 986–987. [Google Scholar] [CrossRef]
- Ho, C.Y.; Solomon, S.D. A Clinician’s Guide to Tissue Doppler Imaging. Circulation 2006, 113, e396–e398. [Google Scholar] [CrossRef]
- Henderson, W.R.; Griesdale, D.E.; Walley, K.R.; Sheel, A.W. Clinical Review: Guyton—the role of mean circulatory filling pressure and right atrial pressure in controlling cardiac output. Crit. Care 2010, 14, 243. [Google Scholar] [CrossRef] [Green Version]
- Meluzin, J.; Spinarova, L.; Bakala, J.; Toman, J.; Krejci, J.; Hude, P.; Kara, T.; Soucek, M. Pulsed Doppler tissue imaging of the velocity of tricuspid annular systolic motion; a new, rapid, and non-invasive method of evaluating right ventricular systolic function. Eur. Heart J. 2001, 22, 340–348. [Google Scholar] [CrossRef] [Green Version]
- Vaishnav, M.; Sedgwick, J. Point-of-care echocardiography—A road to future or a step backwards. Australas. J. Ultrasound Med. 2019, 22, 26–31. [Google Scholar] [CrossRef] [Green Version]
- Carrizales-Sepúlveda, E.F.; Vera-Pineda, R.; Flores-Ramírez, R.; Hernández-Guajardo, D.A.; Pérez-Contreras, E.; Lozano-Ibarra, M.M.; Ordaz-Farías, A. Echocardiographic Manifestations in COVID-19: A Review. Heart Lung Circ. 2021, 30, 1117–1129. [Google Scholar] [CrossRef]
- Neskovic, A.N.; Edvardsen, T.; Galderisi, M.; Garbi, M.; Gullace, G.; Jurcut, R.; Dalen, H.; Hagendorff, A.; Lancellotti, P.; European Association of Cardiovascular Imaging Document Reviewers; et al. Focus cardiac ultrasound: The European Association of Cardiovascular Imaging viewpoint. Eur. Heart J. Cardiovasc. Imaging 2014, 15, 956–960. [Google Scholar] [CrossRef] [Green Version]
- Robba, C.; Wong, A.; Poole, D.; Al Tayar, A.; Arntfield, R.T.; Chew, M.S.; Corradi, F.; Douflé, G.; Goffi, A.; Lamperti, M.; et al. Basic ultrasound head-to-toe skills for intensivists in the general and neuro intensive care unit population: Consensus and expert recommendations of the European Society of Intensive Care Medicine. Intensive Care Med. 2021, 47, 1347–1367. [Google Scholar] [CrossRef]
- Senthilnathan, M.; Kundra, P.; Mishra, S.K.; Velayudhan, S.; Pillai, A.A. Competence of Intensivists in Focused Transthoracic Echocardiography in Intensive Care Unit: A Prospective Observational Study. Indian J. Community Med. 2018, 22, 340–345. [Google Scholar] [CrossRef] [PubMed]


| Study’s First Author | Number of Patients | BMI | Patient Position | COVID | Mechanical Ventilation | Echo Windows (and Probe) | LV Function | RV Function | Other Parameters |
|---|---|---|---|---|---|---|---|---|---|
| Ugalde et al. [11] | 139 (68 in prone position) | N/A | Swimmer | Yes | Yes | -Apical 4-C -Apical 5-C (TTE phased array probe) | -LVEDV -LVESV -MAPSE -LVED area -Mitral E wave -Mitral A wave -Mitral S’ TDI -Mitral e’ TDI -LVOT-VTI -EF -CO -Septal morphology | -RVED area -TR-Gr -TAPSE -Tricuspid S’ wave | -IVC diameter |
| Giustiniano et al. [8] | 8 | N/A | Traditional Prone (with deflated air mattress) | Yes | Yes | -Apical 4-C -Apical 5-C (TTE phased array probe) | -LVEDD -LVOT-VTI -MAPSE -EF | -RVEDD -TAPSE -S’TDI -TR-Gr -RV/LV EDD | |
| Gibson et al. [12] | 27 | 31 ± 5.1 | Swimmer | Yes | Yes | -Apical 4-C -Apical 5-C (TTE phased array probe) | -MAPSE -Mitral E wave -Mitral A wave -e’ TDI -a’ TDI -LVOT-VTI | -TAPSE -S’ TDI -Peak TR- Gradient | |
| Garcia et al. [13] | 15 | 29 ± 4.5 | Swimmer | Yes | Yes | -Apical 4-C -Apical 5-C (TTE phased array probe) | -MAPSE -LVOT-VTI -E/e’ ratio -Regional wall motion abnormalities | -RVEDD -RV/LV -S’ TDI -TAPSE | |
| Marvaki et al. [14] | 21 | 28 ± 4.6 | Traditional prone | Yes | Yes | External TEE Probe for TTE views: -PLAX -PSAX -Apical 4-C -Subcostal SAX | N/A | N/A | (Gross estimation of LV, RV, valves function, and pericardial effusion) |
| Roemer et al. [15] | 24 | N/A | Swimmer | No | No | -Apical 4-C -Apical 2-C -Apical long axis -RV-Focused (TTE phased array probe) | -LV GLS | -RV LS -S’ TDI -RV Systolic Pressure (PAPs) -RV inflow E wave | -IVC diameter (transhepatic) |
| Santos-Martinez et al. [16] | 50 | 25.65 ± 2.71 | Modified Swimmer ** | No | No | -Apical 4-C (TTE phased array probe) | N/A | -TAPSE -S’ TDI -RV FAC -RV End Diastolic area -RV End Systolic area -PAPs -RV/LV ratio | |
| Taha HS et al. [17] | 30 | 26.4 ± 5.9 | Traditional prone | No | No | External TEE probe for TTE views: -PLAX -PSAX | -LVESD -LVEDD -dSWT -dPWT -EF -LA Area -Aortic root area | (Gross estimation of RV and valves abnormalities) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giustiniano, E.; Palma, S.; Meco, M.; Ripani, U.; Nisi, F. Echocardiography in Prone Positioned Critically Ill Patients: A Wealth of Information from a Single View. Diagnostics 2022, 12, 1460. https://doi.org/10.3390/diagnostics12061460
Giustiniano E, Palma S, Meco M, Ripani U, Nisi F. Echocardiography in Prone Positioned Critically Ill Patients: A Wealth of Information from a Single View. Diagnostics. 2022; 12(6):1460. https://doi.org/10.3390/diagnostics12061460
Chicago/Turabian StyleGiustiniano, Enrico, Sergio Palma, Massimo Meco, Umberto Ripani, and Fulvio Nisi. 2022. "Echocardiography in Prone Positioned Critically Ill Patients: A Wealth of Information from a Single View" Diagnostics 12, no. 6: 1460. https://doi.org/10.3390/diagnostics12061460
APA StyleGiustiniano, E., Palma, S., Meco, M., Ripani, U., & Nisi, F. (2022). Echocardiography in Prone Positioned Critically Ill Patients: A Wealth of Information from a Single View. Diagnostics, 12(6), 1460. https://doi.org/10.3390/diagnostics12061460







