Thoracic Aortic Dilation: Implications for Physical Activity and Sport Participation
Abstract
1. Introduction
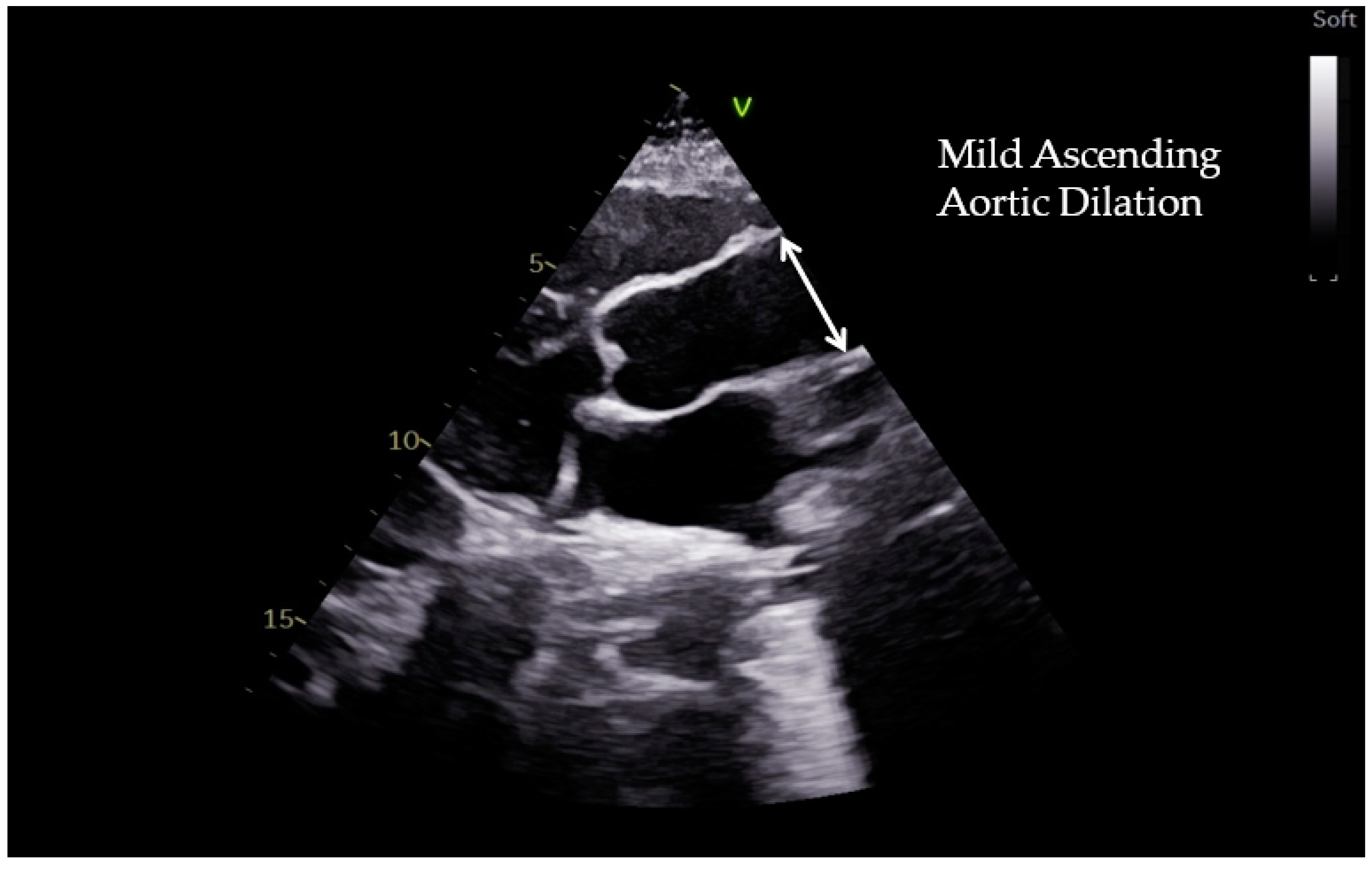
2. Measuring the Aortic Root and Ascending Aorta
3. Aortic Dilation in Athletes
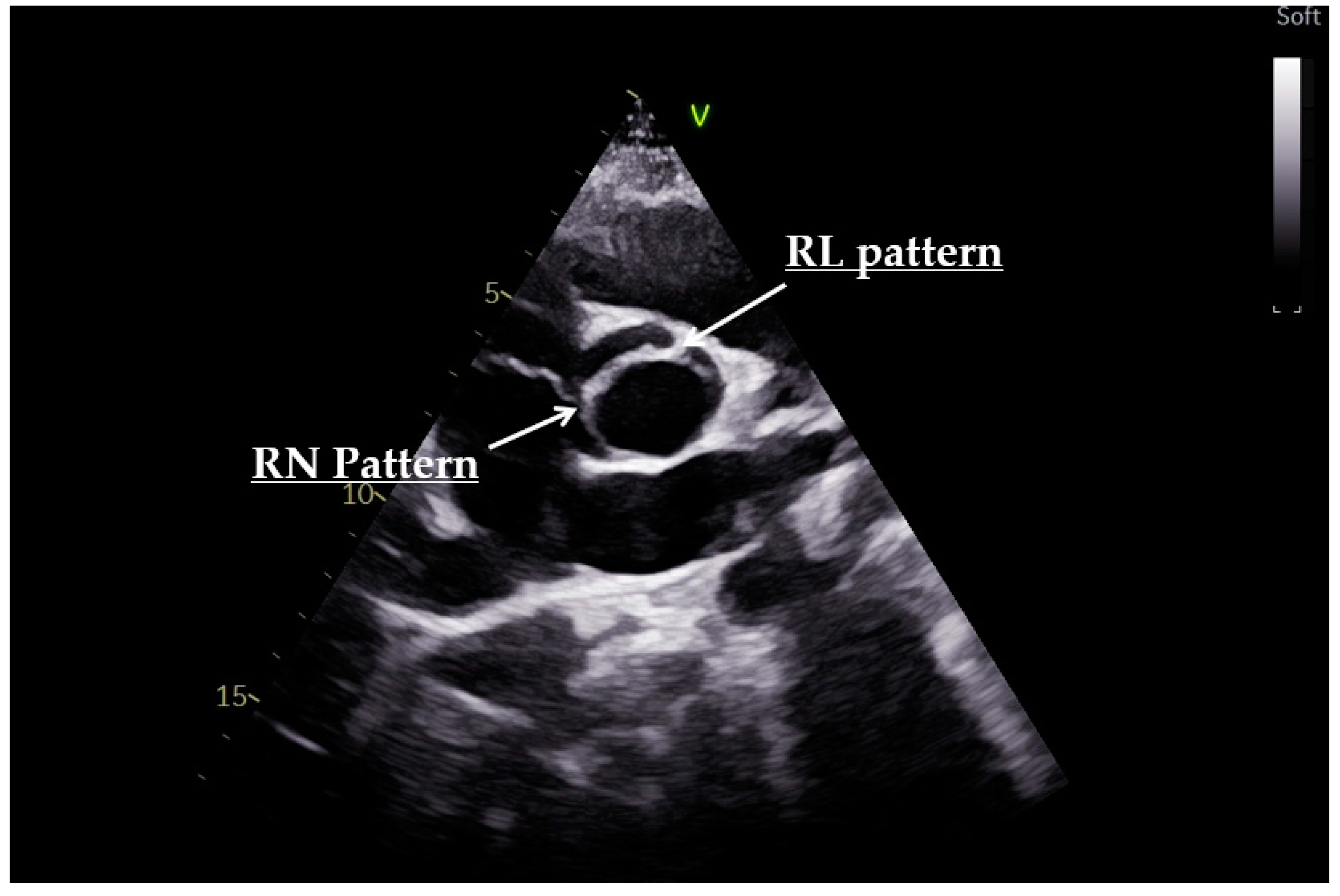
4. Bicuspid Aortic Valve
5. Heritable Thoracic Aortic Disease
6. Future Direction
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Prior, D.L.; La Gerche, A. The athlete’s heart. Heart 2012, 98, 947–955. [Google Scholar] [CrossRef] [PubMed]
- Pelliccia, A.; Sharma, S.; Gati, S.; Bäck, M.; Börjesson, M.; Caselli, S.; Collet, J.P.; Corrado, D.; Drezner, J.A.; ESC Scientific Document Group; et al. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur. Heart J. 2021, 42, 17–96, Erratum in Eur. Heart J. 2021, 42, 548–549. [Google Scholar] [CrossRef]
- Monda, E.; Palmiero, G.; Lioncino, M.; Rubino, M.; Cirillo, A.; Fusco, A.; Caiazza, M.; Verrillo, F.; Diana, G.; Mauriello, A.; et al. Multimodality Imaging in Cardiomyopathies with Hypertrophic Phenotypes. J. Clin. Med. 2022, 11, 868. [Google Scholar] [CrossRef] [PubMed]
- Limongelli, G.; Nunziato, M.; D’Argenio, V.; Esposito, M.V.; Monda, E.; Mazzaccara, C.; Caiazza, M.; D’Aponte, A.; D’Andrea, A.; Bossone, E.; et al. Yield and clinical significance of genetic screening in elite and amateur athletes. Eur. J. Prev. Cardiol. 2020, 28, 1081–1090. [Google Scholar] [CrossRef] [PubMed]
- Limongelli, G.; Monda, E.; Nunziato, M.; Salvatore, F. Genetic evaluation in athletes and cascade family screening: Reply. Eur. J. Prev. Cardiol. 2022, 29, e41–e43. [Google Scholar] [CrossRef]
- Mitchell, J.H.; Haskell, W.; Snell, P.; Van Camp, S.P. Task Force 8: Classification of sports. J. Am. Coll. Cardiol. 2005, 45, 1364–1367. [Google Scholar] [CrossRef]
- Fagard, R.H. Athlete’s heart: A meta-analysis of the echocardiographic experience. Int. J. Sports Med. 1996, 17 (Suppl. S3), S140–S144. [Google Scholar] [CrossRef]
- Iskandar, A.; Thompson, P.D. A meta-analysis of aortic root size in elite athletes. Circulation 2013, 127, 791–798. [Google Scholar] [CrossRef]
- Erbel, R.; Aboyans, V.; Boileau, C.; Bossone, E.; Bartolomeo, R.D.; Eggebrecht, H.; Evangelista, A.; Falk, V.; Frank, H.; Gaemperli, O.; et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur. Heart J. 2014, 35, 2873–2926, Erratum in Eur. Heart J. 2015, 36, 2779. [Google Scholar] [CrossRef]
- Maron, B.J.; Doerer, J.J.; Haas, T.S.; Tierney, D.M.; Mueller, F.O. Sudden deaths in young competitive athletes: Analysis of 1866 deaths in the United States, 1980–2006. Circulation 2009, 119, 1085–1092. [Google Scholar] [CrossRef]
- Michelena, H.I.; Prakash, S.K.; Della Corte, A.; Bissell, M.M.; Anavekar, N.; Mathieu, P.; Bossé, Y.; Limongelli, G.; Bossone, E.; Benson, D.W.; et al. Bicuspid aortic valve: Identifying knowledge gaps and rising to the challenge from the International Bicuspid Aortic Valve Consortium (BAVCon). Circulation 2014, 129, 2691–2704. [Google Scholar] [CrossRef] [PubMed]
- Hagan, P.G.; Nienaber, C.A.; Isselbacher, E.M.; Bruckman, D.; Karavite, D.J.; Russman, P.L.; Evangelista, A.; Fattori, R.; Suzuki, T.; Oh, J.K.; et al. The International Registry of Acute Aortic Dissection (IRAD): New insights into an old disease. JAMA 2000, 283, 897–903. [Google Scholar] [CrossRef] [PubMed]
- Elefteriades, J.A. Natural history of thoracic aortic aneurysms: Indications for surgery, and surgical versus nonsurgical risks. Ann. Thorac. Surg. 2002, 74, S1877–S1880; discussion S1892–S1898. [Google Scholar] [CrossRef]
- Heuts, S.; Adriaans, B.P.; Rylski, B.; Mihl, C.; Bekkers, S.C.A.M.; Olsthoorn, J.R.; Natour, E.; Bouman, H.; Berezowski, M.; Kosiorowska, K.; et al. Evaluating the diagnostic accuracy of maximal aortic diameter, length and volume for prediction of aortic dissection. Heart 2020, 106, 892–897. [Google Scholar] [CrossRef]
- Devereux, R.B.; de Simone, G.; Arnett, D.K.; Best, L.G.; Boerwinkle, E.; Howard, B.V.; Kitzman, D.; Lee, E.T.; Mosley, T.H., Jr.; Weder, A.; et al. Normal limits in relation to age, body size and gender of two-dimensional echocardiographic aortic root dimensions in persons ≥15 years of age. Am. J. Cardiol. 2012, 110, 1189–1194. [Google Scholar] [CrossRef]
- Rozado, J.; Martin, M.; Pascual, I.; Hernandez-Vaquero, D.; Moris, C. Comparing American, European and Asian practice guidelines for aortic diseases. J. Thorac. Dis. 2017, 9 (Suppl. S6), S551–S560. [Google Scholar] [CrossRef] [PubMed]
- Zafar, M.A.; Li, Y.; Rizzo, J.A.; Charilaou, P.; Saeyeldin, A.; Velasquez, C.A.; Mansour, A.M.; Bin Mahmood, S.U.; Ma, W.G.; Brownstein, A.J.; et al. Height alone, rather than body surface area, suffices for risk estimation in ascending aortic aneurysm. J. Thorac. Cardiovasc. Surg. 2018, 155, 1938–1950. [Google Scholar] [CrossRef]
- Muraru, D.; Maffessanti, F.; Kocabay, G.; Peluso, D.; Dal Bianco, L.; Piasentini, E.; Jose, S.P.; Iliceto, S.; Badano, L.P. Ascending aorta diameters measured by echocardiography using both leading edge-to-leading edge and inner edge-to-inner edge conventions in healthy volunteers. Eur. Heart J. Cardiovasc. Imaging 2014, 15, 415–422. [Google Scholar] [CrossRef]
- Evangelista, A.; Flachskampf, F.A.; Erbel, R.; Antonini-Canterin, F.; Vlachopoulos, C.; Rocchi, G.; Sicari, R.; Nihoyannopoulos, P.; Zamorano, J.; on behalf of the European Association of Echocardiography; et al. Echocardiography in aortic diseases: EAE recommendations for clinical practice. Eur. J. Echocardiogr. 2010, 11, 645–658, Erratum in Eur. J. Echocardiogr. 2011, 12, 642. [Google Scholar] [CrossRef]
- Leong, K.; Knipe, H.; Binny, S.; Pascoe, H.; Better, N.; Langenberg, F.; Lui, E.; Joshi, S.B. Aortic root measurement on CT: Linear dimensions, aortic root area and comparison with echocardiography. A retrospective cross sectional study. Br. J. Radiol. 2021, 94, 20201232. [Google Scholar] [CrossRef]
- Prihadi, E.; Delgado, V. Multimodality Imaging of the Aorta: Implications for Patient Surveillance. J. Am. Soc. Echocardiogr. 2016, 29, 838–841. [Google Scholar] [CrossRef] [PubMed]
- Asch, F.M.; Yuriditsky, E.; Prakash, S.K.; Roman, M.J.; Weinsaft, J.W.; Weissman, G.; Weigold, W.G.; Morris, S.A.; Ravekes, W.J.; Holmes, K.W.; et al. The Need for Standardized Methods for Measuring the Aorta: Multimodality Core Lab Experience From the GenTAC Registry. JACC Cardiovasc. Imaging 2016, 9, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Pelliccia, A.; Di Paolo, F.M.; De Blasiis, E.; Quattrini, F.M.; Pisicchio, C.; Guerra, E.; Culasso, F.; Maron, B.J. Prevalence and clinical significance of aortic root dilation in highly trained competitive athletes. Circulation 2010, 122, 698–706. [Google Scholar] [CrossRef] [PubMed]
- Gati, S.; Malhotra, A.; Sedgwick, C.; Papamichael, N.; Dhutia, H.; Sharma, R.; Child, A.H.; Papadakis, M.; Sharma, S. Prevalence and progression of aortic root dilatation in highly trained young athletes. Heart 2019, 105, 920–925. [Google Scholar] [CrossRef]
- Boraita, A.; Heras, M.E.; Morales, F.; Marina-Breysse, M.; Canda, A.; Rabadan, M.; Barriopedro, M.I.; Varela, A.; de la Rosa, A.; Tuñón, J. Reference Values of Aortic Root in Male and Female White Elite Athletes According to Sport. Circ. Cardiovasc. Imaging 2016, 9, e005292. [Google Scholar] [CrossRef]
- Sillesen, A.S.; Vøgg, O.; Pihl, C.; Raja, A.A.; Sundberg, K.; Vedel, C.; Zingenberg, H.; Jørgensen, F.S.; Vejlstrup, N.; Iversen, K.; et al. Prevalence of Bicuspid Aortic Valve and Associated Aortopathy in Newborns in Copenhagen, Denmark. JAMA 2021, 325, 561–567. [Google Scholar] [CrossRef]
- Verma, S.; Siu, S.C. Aortic dilatation in patients with bicuspid aortic valve. N. Engl. J. Med. 2014, 370, 1920–1929. [Google Scholar] [CrossRef]
- D’Ascenzi, F.; Valentini, F.; Anselmi, F.; Cavigli, L.; Bandera, F.; Benfari, G.; D’Andrea, A.; Di Salvo, G.; Esposito, R.; Evola, V.; et al. Bicuspid aortic valve and sports: From the echocardiographic evaluation to the eligibility for sports competition. Scand. J. Med. Sci. Sports 2021, 31, 510–520. [Google Scholar] [CrossRef]
- Sievers, H.H.; Schmidtke, C. A classification system for the bicuspid aortic valve from 304 surgical specimens. J. Thorac. Cardiovasc. Surg. 2007, 133, 1226–1233. [Google Scholar] [CrossRef]
- Michelena, H.I.; Khanna, A.D.; Mahoney, D.; Margaryan, E.; Topilsky, Y.; Suri, R.M.; Eidem, B.; Edwards, W.D.; Sundt, T.M.; Enriquez-Sarano, M. Incidence of aortic complications in patients with bicuspid aortic valves. JAMA 2011, 306, 1104–1112. [Google Scholar] [CrossRef]
- Baumgartner, H.; De Backer, J.; Babu-Narayan, S.V.; Budts, W.; Chessa, M.; Diller, G.P.; Lung, B.; Kluin, J.; Lang, I.M.; Meijboom, F.; et al. 2020 ESC Guidelines for the management of adult congenital heart disease. Eur. Heart J. 2021, 42, 563–645. [Google Scholar] [CrossRef] [PubMed]
- Davies, R.R.; Kaple, R.K.; Mandapati, D.; Gallo, A.; Botta, D.M., Jr.; Elefteriades, J.A.; Coady, M.A. Natural history of ascending aortic aneurysms in the setting of an unreplaced bicuspid aortic valve. Ann. Thorac. Surg. 2007, 83, 1338–1344. [Google Scholar] [CrossRef] [PubMed]
- Tzemos, N.; Therrien, J.; Yip, J.; Thanassoulis, G.; Tremblay, S.; Jamorski, M.T.; Webb, G.D.; Siu, S.C. Outcomes in adults with bicuspid aortic valves. JAMA 2008, 300, 1317–1325. [Google Scholar] [CrossRef] [PubMed]
- Michelena, H.I.; Della Corte, A.; Prakash, S.K.; Milewicz, D.M.; Evangelista, A.; Enriquez-Sarano, M. Bicuspid aortic valve aortopathy in adults: Incidence, etiology, and clinical significance. Int. J. Cardiol. 2015, 201, 400–407. [Google Scholar] [CrossRef] [PubMed]
- Longobardo, L.; Jain, R.; Carerj, S.; Zito, C.; Khandheria, B.K. Bicuspid Aortic Valve: Unlocking the Morphogenetic Puzzle. Am. J. Med. 2016, 129, 796–805. [Google Scholar] [CrossRef]
- Braverman, A.C.; Harris, K.M.; Kovacs, R.J.; Maron, B.J. Eligibility and Disqualification Recommendations for Competitive Athletes With Cardiovascular Abnormalities: Task Force 7: Aortic Diseases, Including Marfan Syndrome: A Scientific Statement From the American Heart Association and American College of Cardiology. J. Am. Coll. Cardiol. 2015, 66, 2398–2405. [Google Scholar] [CrossRef]
- Finocchiaro, G.; Papadakis, M.; Robertus, J.L.; Dhutia, H.; Steriotis, A.K.; Tome, M.; Mellor, G.; Merghani, A.; Malhotra, A.; Behr, E.; et al. Etiology of Sudden Death in Sports: Insights From a United Kingdom Regional Registry. J. Am. Coll. Cardiol. 2016, 67, 2108–2115. [Google Scholar] [CrossRef]
- Finocchiaro, G.; Westaby, J.; Bhatia, R.; Malhotra, A.; Behr, E.R.; Papadakis, M.; Sharma, S.; Sheppard, M.N. Sudden Death in Female Athletes: Insights From a Large Regional Registry in the United Kingdom. Circulation 2021, 144, 1827–1829. [Google Scholar] [CrossRef]
- Tseng, Z.H.; Salazar, J.W.; Olgin, J.E.; Ursell, P.C.; Kim, A.S.; Bedigian, A.; Probert, J.; Hart, A.P.; Moffatt, E.; Vittinghoff, E. Refining the World Health Organization Definition: Predicting Autopsy-Defined Sudden Arrhythmic Deaths Among Presumed Sudden Cardiac Deaths in the POST SCD Study. Circ. Arrhythm. Electrophysiol. 2019, 12, e007171. [Google Scholar] [CrossRef]
- Roberts, W.C.; Ko, J.M. Frequency by decades of unicuspid, bicuspid, and tricuspid aortic valves in adults having isolated aortic valve replacement for aortic stenosis, with or without associated aortic regurgitation. Circulation 2005, 111, 920–925. [Google Scholar] [CrossRef]
- Fedak, P.W.; Verma, S.; David, T.E.; Leask, R.L.; Weisel, R.D.; Butany, J. Clinical and pathophysiological implications of a bicuspid aortic valve. Circulation 2002, 106, 900–904. [Google Scholar] [CrossRef] [PubMed]
- Tadros, T.M.; Klein, M.D.; Shapira, O.M. Ascending aortic dilatation associated with bicuspid aortic valve: Pathophysiology, molecular biology, and clinical implications. Circulation 2009, 119, 880–890. [Google Scholar] [CrossRef] [PubMed]
- Hope, M.D.; Hope, T.A.; Meadows, A.K.; Ordovas, K.G.; Urbania, T.H.; Alley, M.T.; Higgins, C.B. Bicuspid aortic valve: Four-dimensional MR evaluation of ascending aortic systolic flow patterns. Radiology 2010, 255, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Baleilevuka-Hart, M.; Teng, B.J.; Carson, K.A.; Ravekes, W.J.; Holmes, K.W. Sports Participation and Exercise Restriction in Children with Isolated Bicuspid Aortic Valve. Am. J. Cardiol. 2020, 125, 1673–1677. [Google Scholar] [CrossRef]
- Bonow, R.O.; Nishimura, R.A.; Thompson, P.D.; Udelson, J.E. Eligibility and Disqualification Recommendations for Competitive Athletes With Cardiovascular Abnormalities: Task Force 5: Valvular Heart Disease: A Scientific Statement From the American Heart Association and American College of Cardiology. J. Am. Coll. Cardiol. 2015, 66, 2385–2392. [Google Scholar] [CrossRef]
- Stefani, L.; Galanti, G.; Innocenti, G.; Mercuri, R.; Maffulli, N. Exercise training in athletes with bicuspid aortic valve does not result in increased dimensions and impaired performance of the left ventricle. Cardiol. Res. Pract. 2014, 2014, 238694. [Google Scholar] [CrossRef][Green Version]
- Spataro, A.; Pelliccia, A.; Rizzo, M.; Biffi, A.; Masazza, G.; Pigozzi, F. The natural course of bicuspid aortic valve in athletes. Int. J. Sports Med. 2008, 29, 81–85. [Google Scholar] [CrossRef]
- Boraita, A.; Morales-Acuna, F.; Marina-Breysse, M.; Heras, M.E.; Canda, A.; Fuentes, M.E.; Chacón, A.; Diaz-Gonzalez, L.; Rabadan, M.; Parra Laca, B.; et al. Bicuspid aortic valve behaviour in elite athletes. Eur. Heart J. Cardiovasc. Imaging 2019, 20, 772–780. [Google Scholar] [CrossRef]
- Galanti, G.; Stefani, L.; Toncelli, L.; Vono, M.C.; Mercuri, R.; Maffulli, N. Effects of sports activity in athletes with bicuspid aortic valve and mild aortic regurgitation. Br. J. Sports Med. 2010, 44, 275–279. [Google Scholar] [CrossRef]
- Monda, E.; Fusco, A.; Della Corte, A.; Caiazza, M.; Cirillo, A.; Gragnano, F.; Giugliano, M.P.; Citro, R.; Rubino, M.; Esposito, A.; et al. Impact of Regular Physical Activity on Aortic Diameter Progression in Paediatric Patients with Bicuspid Aortic Valve. Pediatr. Cardiol. 2021, 42, 1133–1140. [Google Scholar] [CrossRef]
- Pyeritz, R.E. Heritable thoracic aortic disorders. Curr. Opin. Cardiol. 2014, 29, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Albornoz, G.; Coady, M.A.; Roberts, M.; Davies, R.R.; Tranquilli, M.; Rizzo, J.A.; Elefteriades, J.A. Familial thoracic aortic aneurysms and dissections—incidence, modes of inheritance, and phenotypic patterns. Ann. Thorac. Surg. 2006, 82, 1400–1405. [Google Scholar] [CrossRef] [PubMed]
- Teixidó-Tura, G.; Franken, R.; Galuppo, V.; Gutiérrez García-Moreno, L.; Borregan, M.; Mulder, B.J.; García-Dorado, D.; Evangelista, A. Heterogeneity of aortic disease severity in patients with Loeys-Dietz syndrome. Heart 2016, 102, 626–632. [Google Scholar] [CrossRef] [PubMed]
- Stout, M. The Marfan syndrome: Implications for athletes and their echocardiographic assessment. Echocardiography 2009, 26, 1075–1081. [Google Scholar] [CrossRef]
- Dietz, H.C.; Pyeritz, R.E. Mutations in the human gene for fibrillin-1 (FBN1) in the Marfan syndrome and related disorders. Hum. Mol. Genet. 1995, 4, 1799–1809. [Google Scholar] [CrossRef]
- Demolder, A.; von Kodolitsch, Y.; Muiño-Mosquera, L.; De Backer, J. Myocardial Function, Heart Failure and Arrhythmia in Marfan Syndrome: A Systematic Literature Review. Diagnostics 2020, 10, 751. [Google Scholar] [CrossRef]
- De Paepe, A.; Devereux, R.B.; Dietz, H.C.; Hennekam, R.C.; Pyeritz, R.E. Revised diagnostic criteria for the Marfan syndrome. Am. J. Med. Genet. 1996, 62, 417–426. [Google Scholar] [CrossRef]
- Loeys, B.L.; Dietz, H.C.; Braverman, A.C.; Callewaert, B.L.; De Backer, J.; Devereux, R.B.; Hilhorst-Hofstee, Y.; Jondeau, G.; Faivre, L.; Milewicz, D.M.; et al. The revised Ghent nosology for the Marfan syndrome. J. Med. Genet. 2010, 47, 476–485. [Google Scholar] [CrossRef]
- Gibson, C.; Nielsen, C.; Alex, R.; Cooper, K.; Farney, M.; Gaufin, D.; Cui, J.Z.; van Breemen, C.; Broderick, T.L.; Vallejo-Elias, J.; et al. Mild aerobic exercise blocks elastin fiber fragmentation and aortic dilatation in a mouse model of Marfan syndrome associated aortic aneurysm. J. Appl. Physiol. 2017, 123, 147–160. [Google Scholar] [CrossRef]
- Mas-Stachurska, A.; Siegert, A.M.; Batlle, M.; Gorbenko Del Blanco, D.; Meirelles, T.; Rubies, C.; Bonorino, F.; Serra-Peinado, C.; Bijnens, B.; Baudin, J.; et al. Cardiovascular Benefits of Moderate Exercise Training in Marfan Syndrome: Insights from an Animal Model. J. Am. Heart Assoc. 2017, 6, e006438. [Google Scholar] [CrossRef]
- Benninghoven, D.; Hamann, D.; von Kodolitsch, Y.; Rybczynski, M.; Lechinger, J.; Schroeder, F.; Vogler, M.; Hoberg, E. Inpatient rehabilitation for adult patients with Marfan syndrome: An observational pilot study. Orphanet. J. Rare Dis. 2017, 12, 127. [Google Scholar] [CrossRef] [PubMed]
- Braverman, A.C. Exercise and the Marfan syndrome. Med. Sci. Sports Exerc. 1998, 30 (Suppl. S10), S387–S395. [Google Scholar] [CrossRef] [PubMed]
- De Backer, J.; Bondue, A.; Budts, W.; Evangelista, A.; Gallego, P.; Jondeau, G.; Loeys, B.; Peña, M.L.; Teixido-Tura, G.; van de Laar, I.; et al. Genetic counselling and testing in adults with congenital heart disease: A consensus document of the ESC Working Group of Grown-Up Congenital Heart Disease, the ESC Working Group on Aorta and Peripheral Vascular Disease and the European Society of Human Genetics. Eur. J. Prev. Cardiol. 2020, 27, 1423–1435. [Google Scholar] [CrossRef] [PubMed]



| Recreational Sport | Competitive Sport | ||
|---|---|---|---|
| Aortic Stenosis | |||
| Mild | All sports Class I; LoE C | All sports Class I; LoE C | |
| Moderate | Low-moderate intensity LVEF > 50%, good functional capacity, and normal exercise test. Class IIa; LoE C | Low-moderate intensity LVEF > 50%, good functional capacity, and normal exercise test. Class IIb; LoE C | |
| Severe | Low intensity LVEF > 50% and normal BP response during exercise. Class IIb; LoE C | Low intensity LVEF > 50% and normal BP response during exercise. Class IIb; LoE C | |
| Moderate and high intensity is not recommended for individuals with LVEF < 50% and/or exercise-induced arrhythmias. Class III; LoE C | Moderate and high intensity is not recommended for individuals with LVEF < 50% and/or exercise-induced arrhythmias. Class III; LoE C | ||
| Aortic Regurgitation | |||
| Mild | All sports Class I; LoE C | All sports Class I; LoE C | |
| Moderate | All sports should be considered non-dilated LV with LVEF > 50% and normal exercise stress test. Class IIa; LoE C | All sports should be considered for individuals with LVEF > 50% and normal exercise test. Class IIa; LoE C | |
| Severe | Low and moderate intensity may be considered for individuals with a mild or moderately dilated LV with LVEF > 50% and normal exercise stress test. Class IIb; LoE C | Low and moderate intensity may be considered for individuals with a mild or moderately dilated LV with LVEF > 50% and normal exercise stress test. Class IIb; LoE C | |
| Moderate or high-intensity is not recommended for individuals with LVEF < 50% and/or exercise-induced arrhythmias. Class III; LoE C | Moderate or high intensity is not recommended for individuals with severe AR and/or LVEF < 50% and/or exercise-induced arrhythmias. Class III; LoE C | ||
| Aortopathy | Sport Category | ||
| Low Intensity | Intermediate Intensity | High Intensity | |
| <40 mm LOW RISK | All sports are permitted with preference for endurance over power sports; follow-up every 2–3 y | ||
| 40–45 mm LOW-INTERMEDIATE RISK | Avoid high- and very high intensity exercise, contact, and power sports; endurance sports are preferred over power sports. Follow-up every 1–2 y | ||
| 45–50 mm INTERMEDIATE RISK | Only skill sports or mixed and endurance sports at low intensity are permitted. Follow-up every 6–12 months | ||
| >50 mm HIGH RISK | Sports are (temporarily) contraindicated. Follow-up after treatment | ||
| Recommendations for Sports and Surgery in Marfan Syndrome | ||||
|---|---|---|---|---|
| <40 mm | 40–45 mm | 45–49 mm | ≥50 | |
| Advice | Avoid high- and very high intensity exercise, contact, and power sports. Preference for endurance over power sports | Only skill sports or mixed or endurance at low intensity | No sport recommended | |
| Follow-up | 1–2 years | 6 months–1 year | 6 months | Re-evaluate after surgery |
| Surgery | ≥45 surgery recommended if ≥1 high-risk factor. High-risk factors for Marfan syndrome patients are: (a) Aortic diameter at the sinuses of Valsalva ≥5 cm; (b) Rapid increase in aortic dilatation (≥3 mm per year); (c) Family history of aortic dissection at a low aortic size; (d) Progressive aortic regurgitation; (e) Personal history of spontaneous vascular dissection and (f) Desire for pregnancy. | Surgery is indicated | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Monda, E.; Verrillo, F.; Rubino, M.; Palmiero, G.; Fusco, A.; Cirillo, A.; Caiazza, M.; Guarnaccia, N.; Mauriello, A.; Lioncino, M.; et al. Thoracic Aortic Dilation: Implications for Physical Activity and Sport Participation. Diagnostics 2022, 12, 1392. https://doi.org/10.3390/diagnostics12061392
Monda E, Verrillo F, Rubino M, Palmiero G, Fusco A, Cirillo A, Caiazza M, Guarnaccia N, Mauriello A, Lioncino M, et al. Thoracic Aortic Dilation: Implications for Physical Activity and Sport Participation. Diagnostics. 2022; 12(6):1392. https://doi.org/10.3390/diagnostics12061392
Chicago/Turabian StyleMonda, Emanuele, Federica Verrillo, Marta Rubino, Giuseppe Palmiero, Adelaide Fusco, Annapaola Cirillo, Martina Caiazza, Natale Guarnaccia, Alfredo Mauriello, Michele Lioncino, and et al. 2022. "Thoracic Aortic Dilation: Implications for Physical Activity and Sport Participation" Diagnostics 12, no. 6: 1392. https://doi.org/10.3390/diagnostics12061392
APA StyleMonda, E., Verrillo, F., Rubino, M., Palmiero, G., Fusco, A., Cirillo, A., Caiazza, M., Guarnaccia, N., Mauriello, A., Lioncino, M., Perna, A., Diana, G., D’Andrea, A., Bossone, E., Calabrò, P., & Limongelli, G. (2022). Thoracic Aortic Dilation: Implications for Physical Activity and Sport Participation. Diagnostics, 12(6), 1392. https://doi.org/10.3390/diagnostics12061392











