Diagnostic Performance of 99mTc-Methoxy-Isobuty-Isonitrile (MIBI) for Risk Stratification of Hypofunctioning Thyroid Nodules: A European Multicenter Study
Abstract
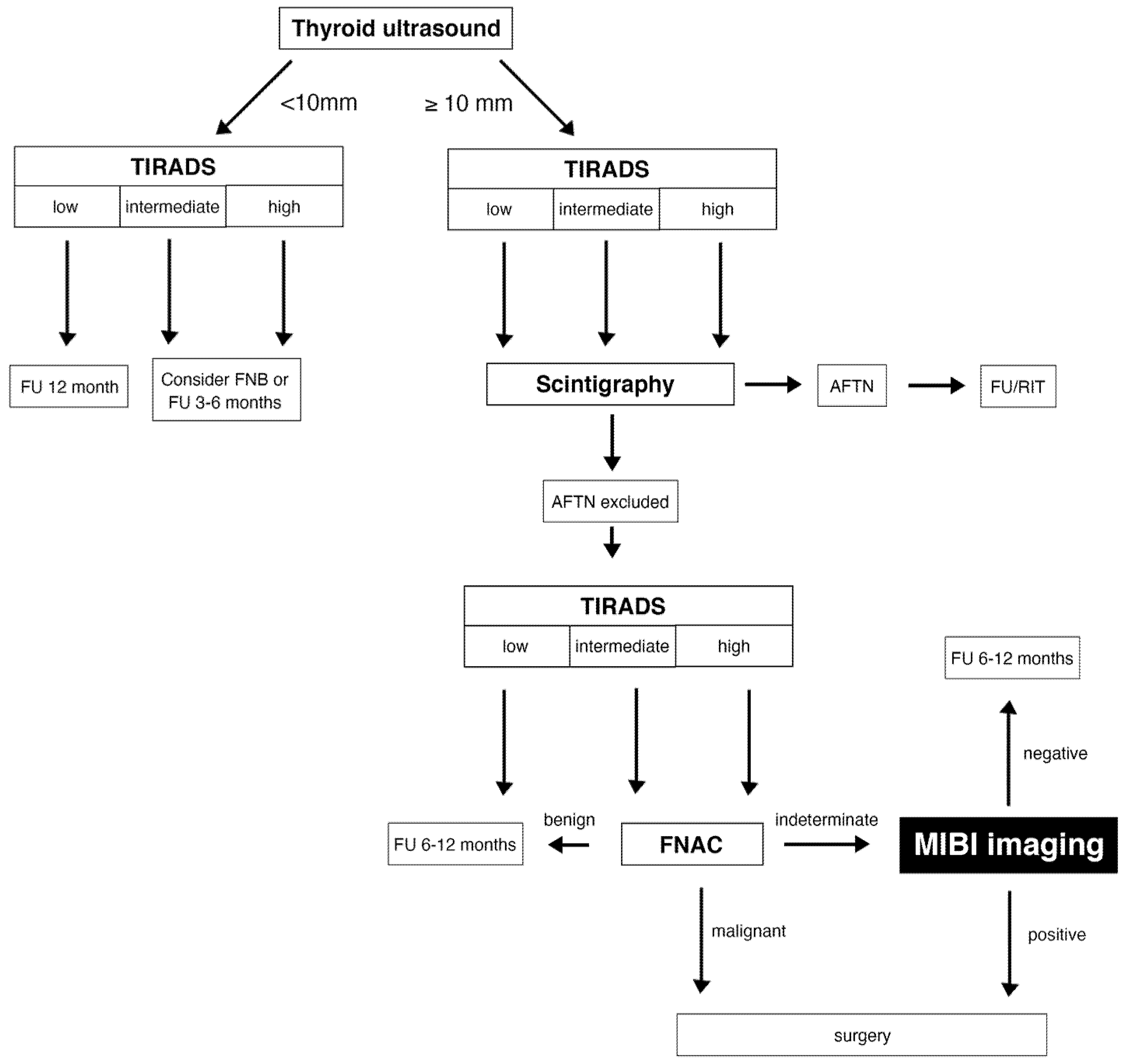
:1. Introduction
2. Methods
2.1. Patients
- a
- age ≥ 18 years,
- b
- hypofunctioning TN of at least 10 mm in maximum diameter,
- c
- EU-TIRADS risk class 4 (intermediate-risk) or 5 (high-risk) as determined by thyroid ultrasound,
- d
- MIBI imaging and:
- (1)
- FNAC with indeterminate results (Bethesda classification III, IV, ICCRTC TIR 3A/B/4) with available histopathological results, or
- (2)
- FNAC with benign results (Bethesda classification II, ICCRTC TIR 2) with either histopathological results or follow-up of at least 12 months without progression (not more than 3 mm growth in one diameter).
2.2. Thyroid Ultrasound
2.3. Fine Needle Aspiration Cytology
- (1)
- The Bethesda system for reporting thyroid cytology (TBSRTC): class I non-diagnostic, class II benign, class III indeterminate (atypia of undetermined significance/follicular lesion of undetermined significance), class IV follicular neoplasm/suspicious for a follicular neoplasm, class V suspicious for malignancy, and class VI malignant [14].
- (2)
- The Italian consensus for the classification and reporting of thyroid cytology (ICCRTC): TIR I non-diagnostic, TIR 1C non-diagnostic cystic, TIR 2 benign, TIR 3A low-risk indeterminate lesion, TIR 3B high-risk indeterminate lesion, TIR 4 suspicious of malignancy, TIR 5 malignant [15].
2.4. MIBI Imaging
MIBI Image Analyses
- (1)
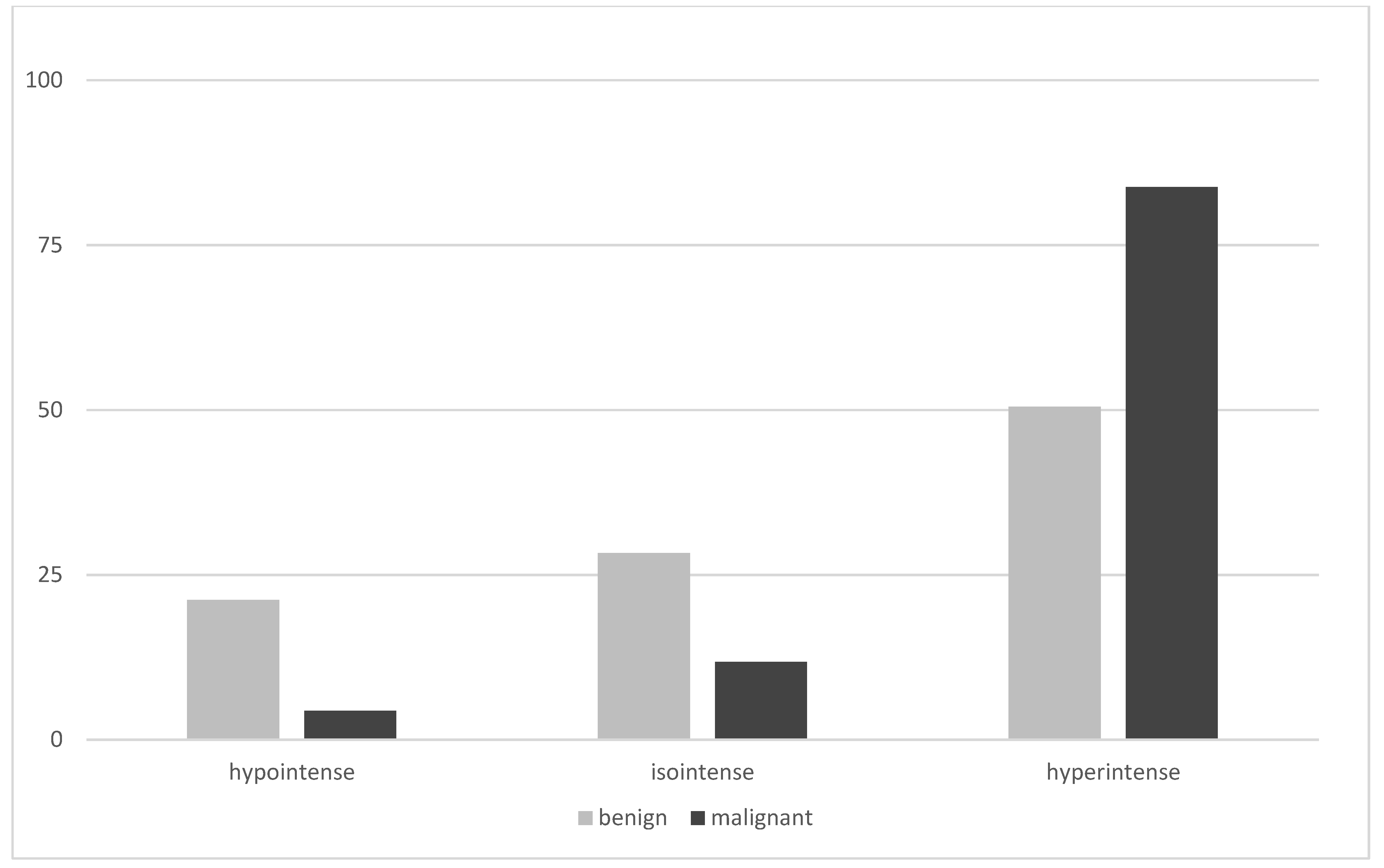
- For both, early and late planar and SPECT images, the visual method described the MIBI uptake in the TN compared to the paranodular thyroid tissue as hypointense (uptake TN < uptake in paranodular tissue), isointense (uptake TN = uptake paranodular), and hyperintense (uptake TN > uptake paranodular). A hypointense MIBI uptake was defined as benign, isointense or hyperintense MIBI uptake was considered suspicious for malignancy [2].
- (2)
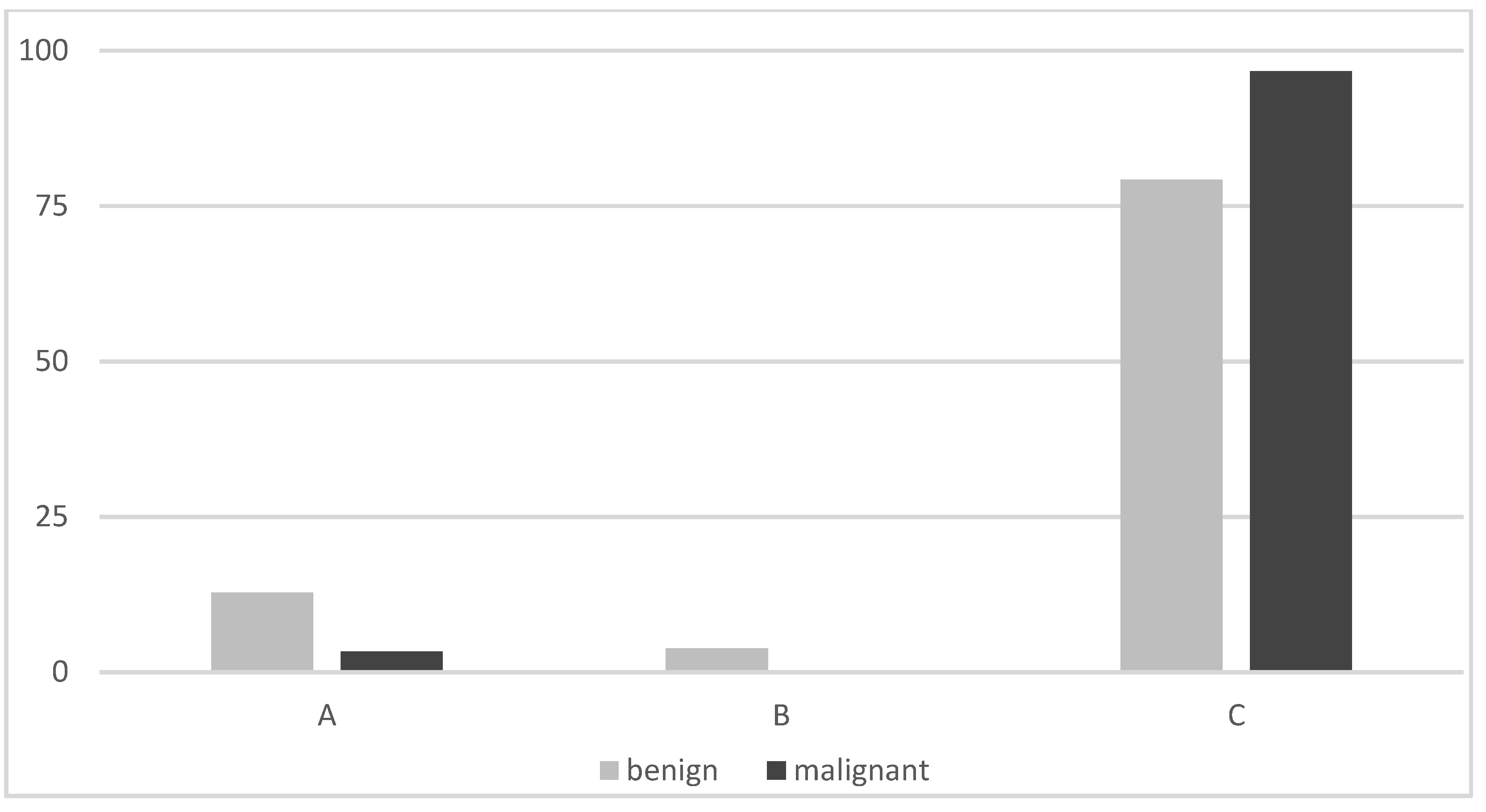
- The visual assessment of washout kinetics of MIBI was classified as follows:
- (i)
- visual pattern A: reduced uptake in the nodule in the early and late image,
- (ii)
- visual pattern B: uptake in the nodule that decreases from early to late image,
- (iii)
- visual pattern C: uptake in the nodule that remains unchanged or has further increased on the delayed image.
- (3)
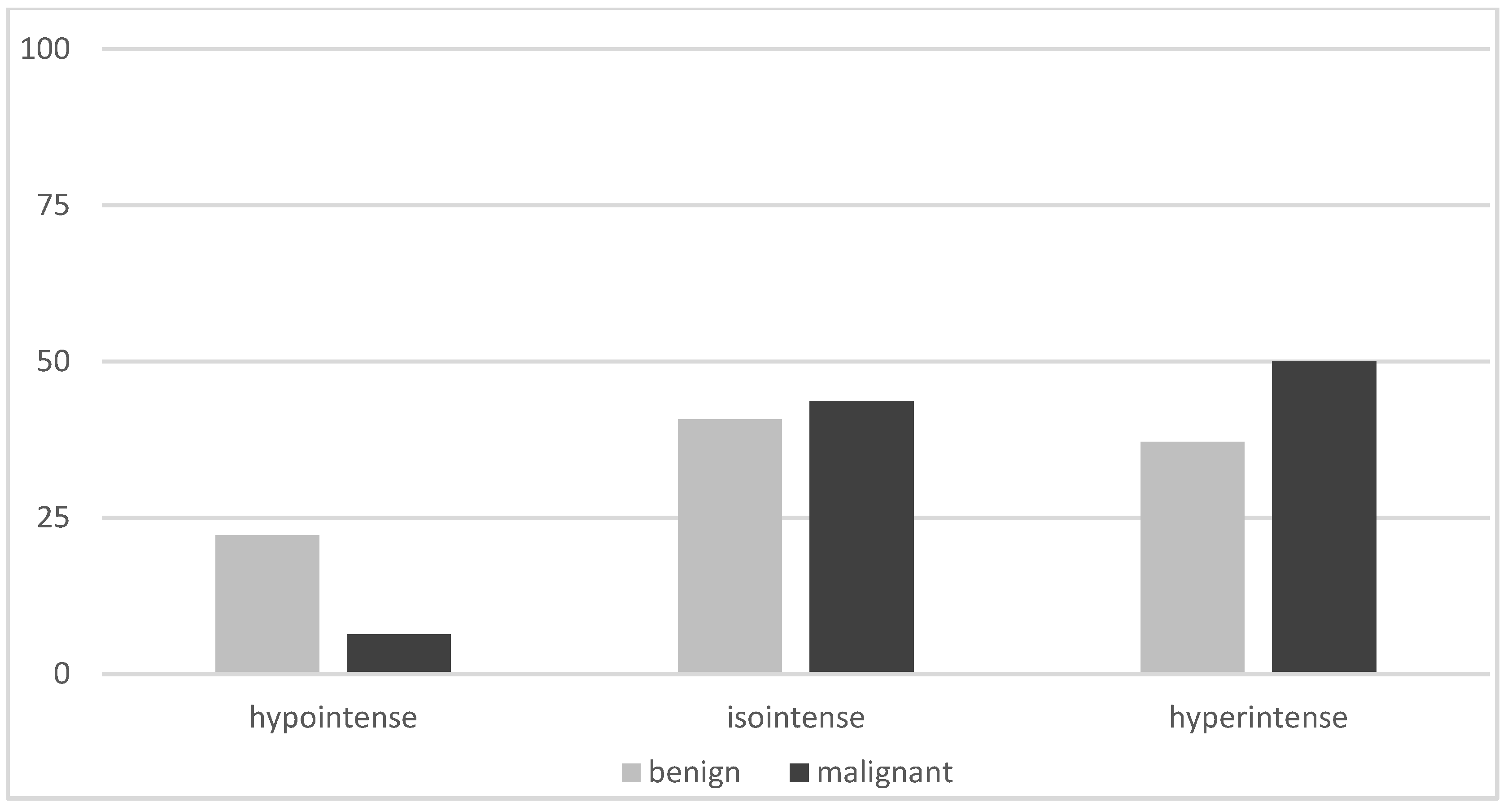
- The WOInd quantifies the percentage MIBI uptake reduction in a TN between the early and the late image. A region of interest (ROI) was drawn manually around the TN of interest on the early image (TN early) and then mirrored outside the thyroid gland for subtracting the background activity (background on the early image).
2.5. Statistics
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Schmidt, M.; Schenke, S. Update 2019 zur MIBI-Szintigrafie bei hypofunktionellen Schilddrüsenknoten. Nuklearmediziner 2019, 42, 174–182. [Google Scholar] [CrossRef]
- Hurtado-López, L.M.; Arellano-Montaño, S.; Torres-Acosta, E.M.; Zaldivar-Ramirez, F.R.; Duarte-Torres, R.M.; Alonso-De-Ruiz, P.; Martínez-Duncker, I.; Martínez-Duncker, C. Combined use of fine-needle aspiration biopsy, MIBI scans and frozen section biopsy offers the best diagnostic accuracy in the assessment of the hypofunctioning solitary thyroid nodule. Eur. J. Nucl. Med. Mol. Imaging 2004, 31, 1273–1279. [Google Scholar] [CrossRef] [PubMed]
- Treglia, G.; Caldarella, C.; Saggiorato, E.; Ceriani, L.; Orlandi, F.; Salvatori, M.; Giovanella, L. Diagnostic performance of 99mTc-MIBI scan in predicting the malignancy of thyroid nodules: A meta-analysis. Endocrine 2013, 44, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Wale, A.; Miles, K.A.; Young, B.; Zammit, C.; Williams, A.; Quin, J.; Dizdarevic, S. Combined 99mTc-methoxyisobutylisonitrile scintigraphy and fine-needle aspiration cytology offers an accurate and potentially cost-effective investigative strategy for the assessment of solitary or dominant thyroid nodules. Eur. J. Nucl. Med. Mol. Imaging 2013, 41, 105–115. [Google Scholar] [CrossRef] [PubMed]
- Leidig-Bruckner, G.; Cichorowski, G.; Sattler, P.; Bruckner, T.; Sattler, B. Evaluation of thyroid nodules-combined use of 99mTc-methylisobutylnitrile scintigraphy and aspiration cytology to assess risk of malignancy and stratify patients for surgical or nonsurgical therapy-a retrospective cohort study. Clin. Endocrinol. 2012, 76, 749–758. [Google Scholar] [CrossRef]
- Giovanella, L.; Avram, A.M.; Iakovou, I.; Kwak, J.; Lawson, S.A.; Lulaj, E.; Luster, M.; Piccardo, A.; Schmidt, M.; Tulchinsky, M.; et al. EANM practice guideline/SNMMI procedure standard for RAIU and thyroid scintigraphy. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 2514–2525. [Google Scholar] [CrossRef]
- Schenke, S.A.; Campenni, A.; Tuncel, M.; Piccardo, A.; Sager, S.; Crncic, T.B.; Rozic, D.; Goerges, R.; Kara, P.P.; Groener, D.; et al. A multicenter survey of current practices of 99mTc-methoxy-isobutyl-isonitrile (MIBI) imaging for the diagnosis of thyroid nodules: More standardization is essential. Clin. Transl. Imaging 2021, 9, 413–422. [Google Scholar] [CrossRef]
- Campennì, A.; Siracusa, M.; Ruggeri, R.M.; Laudicella, R.; Pignata, S.A.; Baldari, S.; Giovanella, L. Differentiating malignant from benign thyroid nodules with indeterminate cytology by 99mTc-MIBI scan: A new quantitative method for improving diagnostic accuracy. Sci. Rep. 2017, 7, 6147. [Google Scholar] [CrossRef] [Green Version]
- Giovanella, L.; Campenni, A.; Treglia, G.; Verburg, F.A.; Trimboli, P.; Ceriani, L.; Bongiovanni, M. Molecular imaging with 99mTc-MIBI and molecular testing for mutations in differentiating benign from malignant follicular neoplasm: A prospective comparison. Eur. J. Nucl. Med. Mol. Imaging 2015, 43, 1018–1026. [Google Scholar] [CrossRef] [Green Version]
- Russ, G.; Bonnema, S.J.; Erdogan, M.F.; Durante, C.; Ngu, R.; Leenhardt, L. European Thyroid Association Guidelines for Ultrasound Malignancy Risk Stratification of Thyroid Nodules in Adults: The EU-TIRADS. Eur. Thyroid J. 2017, 6, 225–237. [Google Scholar] [CrossRef] [Green Version]
- Mathur, A.; Olson, M.T.; Zeiger, M.A. Follicular Lesions of the Thyroid. Surg. Clin. N. Am. 2014, 94, 499–513. [Google Scholar] [CrossRef] [PubMed]
- Heinzel, A.; Müller, D.; Behrendt, F.F.; Giovanella, L.; Mottaghy, F.M.; Verburg, F.A. Thyroid nodules with indeterminate cytology: Molecular imaging with 99mTc-methoxyisobutylisonitrile (MIBI) is more cost-effective than the Afirma® gene expression classifier. Eur. J. Nucl. Med. Mol. Imaging 2014, 41, 1497–1500. [Google Scholar] [CrossRef] [PubMed]
- Trimboli, P.; Treglia, G.; Guidobaldi, L.; Saggiorato, E.; Nigri, G.; Crescenzi, A.; Romanelli, F.; Orlandi, F.; Valabrega, S.; Sadeghi, R.; et al. Clinical characteristics as predictors of malignancy in patients with indeterminate thyroid cytology: A meta-analysis. Endocrine 2013, 46, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Cibas, E.S.; Ali, S.Z. The 2017 Bethesda System for Reporting Thyroid Cytopathology. Thyroid 2017, 27, 1341–1346. [Google Scholar] [CrossRef]
- Nardi, F.; Basolo, F.; Crescenzi, A.; Fadda, G.; Frasoldati, A.; Orlandi, F.; Palombini, L.; Papini, E.; Zini, M.; Pontecorvi, A.; et al. Italian consensus for the classification and reporting of thyroid cytology. J. Endocrinol. Investig. 2014, 37, 593–599. [Google Scholar] [CrossRef]
- Schenke, S.; Zimny, M.; Rink, T.; Stahl, U.; Fritzel, M.; Klett, R. 99mTc-MIBI scintigraphy of hypofunctional thyroid nodules. Comparison of planar and SPECT imaging. Nuklearmedizin 2014, 53, 105–110. [Google Scholar] [CrossRef]
- Riazi, A.; Kalantarhormozi, M.; Nabipour, I.; Eghbali, S.S.; Farzaneh, M.R.; Javadi, H.; Ostovar, A.; Seyedabadi, M.; Assadi, M. Technetium-99m methoxyisobutylisonitrile scintigraphy in the assessment of cold thyroid nodules: Is it time to change the approach to the management of cold thyroid nodules? Nucl. Med. Commun. 2014, 35, 51–57. [Google Scholar] [CrossRef]
- Melloul, M.; Paz, A.; Koren, R.; Cytron, S.; Feinmesser, R.; Gal, R. 99Tc-MIBI scintigraphy of parathyroid adenomas and its relation to tumour size and oxyphil cell abundance. Eur. J. Nucl. Med. Mol. Imaging 2001, 28, 209–213. [Google Scholar] [CrossRef]
- Arbab, A.S.; Koizumi, K.; Toyama, K.; Araki, T. Uptake of technetium-99m-tetrofosmin, technetium-99m-MIBI and thallium-201 in tumor cell lines. J. Nucl. Med. 1996, 37, 1551–1556. [Google Scholar]
- Campennì, A.; Giovanella, L.; Siracusa, M.; Alibrandi, A.; Pignata, S.A.; Giovinazzo, S.; Trimarchi, F.; Ruggeri, R.M.; Baldari, S. 99mTc-Methoxy-Isobutyl-Isonitrile Scintigraphy Is a Useful Tool for Assessing the Risk of Malignancy in Thyroid Nodules with Indeterminate Fine-Needle Cytology. Thyroid 2016, 26, 1101–1109. [Google Scholar] [CrossRef]
- Schenke, S.A.; Klett, R.; Wagner, P.-R.; Mott, S.; Zimny, M.; Feek, U.; Kreissl, M.C. Characteristics of different histological subtypes of thyroid nodules classified with 99mTc-methoxy-isobutyl-isonitrile imaging and Thyroid Imaging Reporting And Data System. Nucl. Med. Commun. 2020, 42, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Saggiorato, E.; Angusti, T.; Rosas, R.; Martinese, M.; Finessi, M.; Arecco, F.; Trevisiol, E.; Bergero, N.; Puligheddu, B.; Volante, M.; et al. 99mTc-MIBI Imaging in the Presurgical Characterization of Thyroid Follicular Neoplasms: Relationship to Multidrug Resistance Protein Expression. J. Nucl. Med. 2009, 50, 1785–1793. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kresnik, E.; Gallowitsch, H.J.; Mikosch, P.; Gomez, I.; Lind, P. Technetium-99m-MIBI Scintigraphy of Thyroid Nodules in an Endenic Goiter Area. J. Nucl. Med. 1997, 38, 62–65. [Google Scholar] [PubMed]
- Schenke, S.; Klett, R.; Acker, P.; Rink, T.; Kreissl, M.C.; Zimny, M. Interobserver Agreement of Planar and SPECT Tc99m-MIBI Scintigraphy for the Assessment of Hypofunctioning Thyroid Nodules. Nuklearmedizin 2019, 58, 258–264. [Google Scholar] [CrossRef]
- Baumgarten, J.; Happel, C.; Ackermann, H.; Grünwald, F. Evaluation der Intra- und Interobserverübereinstimmung von 99mTc-MIBI-Szintigraphien bei hypofunktionellen Knoten. Nuklearmedizin 2017, 56, 132–138. [Google Scholar] [CrossRef]



| All n = 365 | Benign TNs n = 297 | Malignant TNs n = 68 | p-Value | |
|---|---|---|---|---|
| Sex | ||||
| Female n | 284 | 235 | 49 | |
| Male n | 74 | 55 | 19 | |
| Age (years ± SD) | 53.4 (13.1) | 53.7 (12.8) | 52.2 (14.9) | 0.81 |
| Maximum size (mm) | 25 | 25 | 28 | 0.32 |
| Median (25th/75th-p) | (19/33) | (19/32) | (19/34) | |
| Activity (MBq) n | 370 | 370 | 370 | 0.13 |
| Median (25th/75th-p) | (323/384) | (314/399) | (370/370) | |
| Early images (min after injection) n | 271 | 211 | 60 | 0.001 |
| Median (25th/75th-p) | 10 (10/20) | 10 (10/20) | 10 (10/10) | |
| Late images (min after injection) n | 365 | 297 | 68 | 0.12 |
| Median (25th/75th-p) | 60 (60/60) | 60 (60/60) | 60 (60/60) | |
| FA (n = 71) | FTC (n = 6) | MNG (n = 86) | MTC (n = 1) | OA (n = 26) | PDTC (n = 1) | PTC (n = 60) | |
|---|---|---|---|---|---|---|---|
| MIBI planar late | |||||||
| Hypointense (%) | 9.9 | 16.7 | 23.3 | 100 | 7.7 | 0 | 1.7 |
| Isointense (%) | 8.5 | 0 | 19.8 | 0 | 0 | 0 | 13.3 |
| Hyperintense (%) | 81.7 | 83.3 | 57 | 0 | 92.3 | 100 | 85 |
| Visual pattern | |||||||
| A (%) | 3.5 | 0 | 17.1 | 100 | 5.3 | n.a. | 1.8 |
| B (%) | 3.5 | 0 | 4.3 | 0 | 0 | n.a. | 0 |
| C (%) | 93 | 100 | 78.6 | 0 | 94.7 | n.a. | 98.2 |
| WOInd | |||||||
| Low washout, ≥−19 (%) | 2.4 | n.a. | 0 | n.a. | 81.8 | n.a. | 100 |
| High washout, <−19 (%) | 97.6 | n.a. | 100 | n.a. | 18.2 | n.a. | 0 |
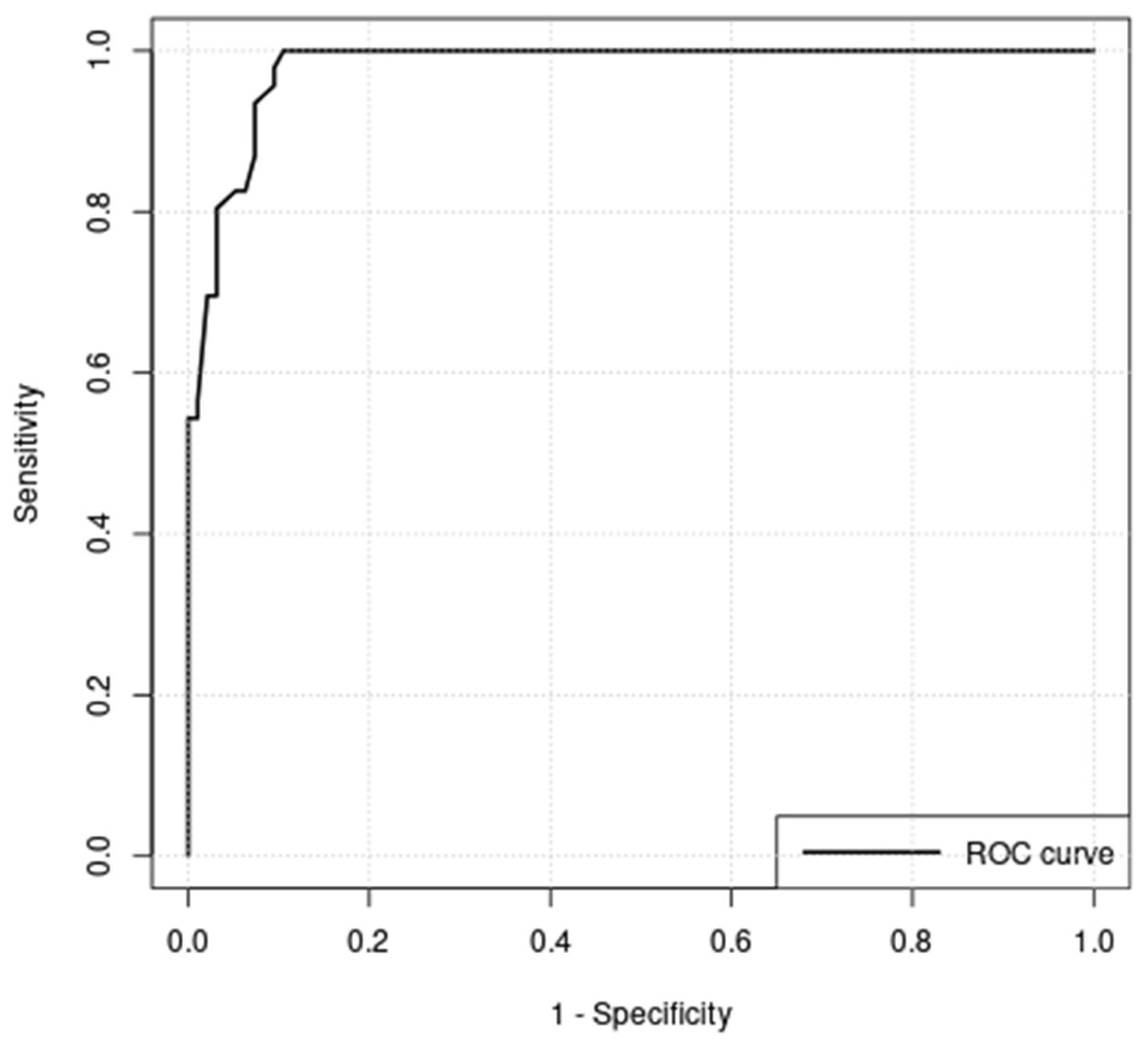
| Sensitivity (%) | Specificity (%) | PPV(%) | NPV (%) | ACC (%) | |
|---|---|---|---|---|---|
| MIBI early | 96.7 | 10.4 | 23.5 | 91.7 | 29.5 |
| MIBI late | 95.6 | 21.2 | 21.7 | 95.5 | 35.1 |
| MIBI-SPECT | 93.8 | 22.2 | 15.2 | 96 | 31.5 |
| Visual pattern | 96.7 | 16.6 | 24.8 | 94.6 | 34.3 |
| Washout index cutoff −19% | 100 | 89.4 | 82.1 | 100 | 92.9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schenke, S.A.; Campennì, A.; Tuncel, M.; Bottoni, G.; Sager, S.; Bogovic Crncic, T.; Rozic, D.; Görges, R.; Özcan, P.P.; Groener, D.; et al. Diagnostic Performance of 99mTc-Methoxy-Isobuty-Isonitrile (MIBI) for Risk Stratification of Hypofunctioning Thyroid Nodules: A European Multicenter Study. Diagnostics 2022, 12, 1358. https://doi.org/10.3390/diagnostics12061358
Schenke SA, Campennì A, Tuncel M, Bottoni G, Sager S, Bogovic Crncic T, Rozic D, Görges R, Özcan PP, Groener D, et al. Diagnostic Performance of 99mTc-Methoxy-Isobuty-Isonitrile (MIBI) for Risk Stratification of Hypofunctioning Thyroid Nodules: A European Multicenter Study. Diagnostics. 2022; 12(6):1358. https://doi.org/10.3390/diagnostics12061358
Chicago/Turabian StyleSchenke, Simone Agnes, Alfredo Campennì, Murat Tuncel, Gianluca Bottoni, Sait Sager, Tatjana Bogovic Crncic, Damir Rozic, Rainer Görges, Pinar Pelin Özcan, Daniel Groener, and et al. 2022. "Diagnostic Performance of 99mTc-Methoxy-Isobuty-Isonitrile (MIBI) for Risk Stratification of Hypofunctioning Thyroid Nodules: A European Multicenter Study" Diagnostics 12, no. 6: 1358. https://doi.org/10.3390/diagnostics12061358
APA StyleSchenke, S. A., Campennì, A., Tuncel, M., Bottoni, G., Sager, S., Bogovic Crncic, T., Rozic, D., Görges, R., Özcan, P. P., Groener, D., Hautzel, H., Klett, R., Kreissl, M. C., & Giovanella, L. (2022). Diagnostic Performance of 99mTc-Methoxy-Isobuty-Isonitrile (MIBI) for Risk Stratification of Hypofunctioning Thyroid Nodules: A European Multicenter Study. Diagnostics, 12(6), 1358. https://doi.org/10.3390/diagnostics12061358







