The Clinical Manifestation of SARS-CoV-2 in Critically Ill Patients with Klebsiella pneumoniae NDM Hospitalized in the ICU of a Modular Hospital during the Third Wave of the Pandemic in Poland—An Observational Cohort Study
Abstract
:1. Introduction
2. Material and Methods
2.1. Study Design
2.2. Setting
2.3. Participants
2.4. Microbiological Analysis
2.5. Study Size
2.6. Statistical Methods
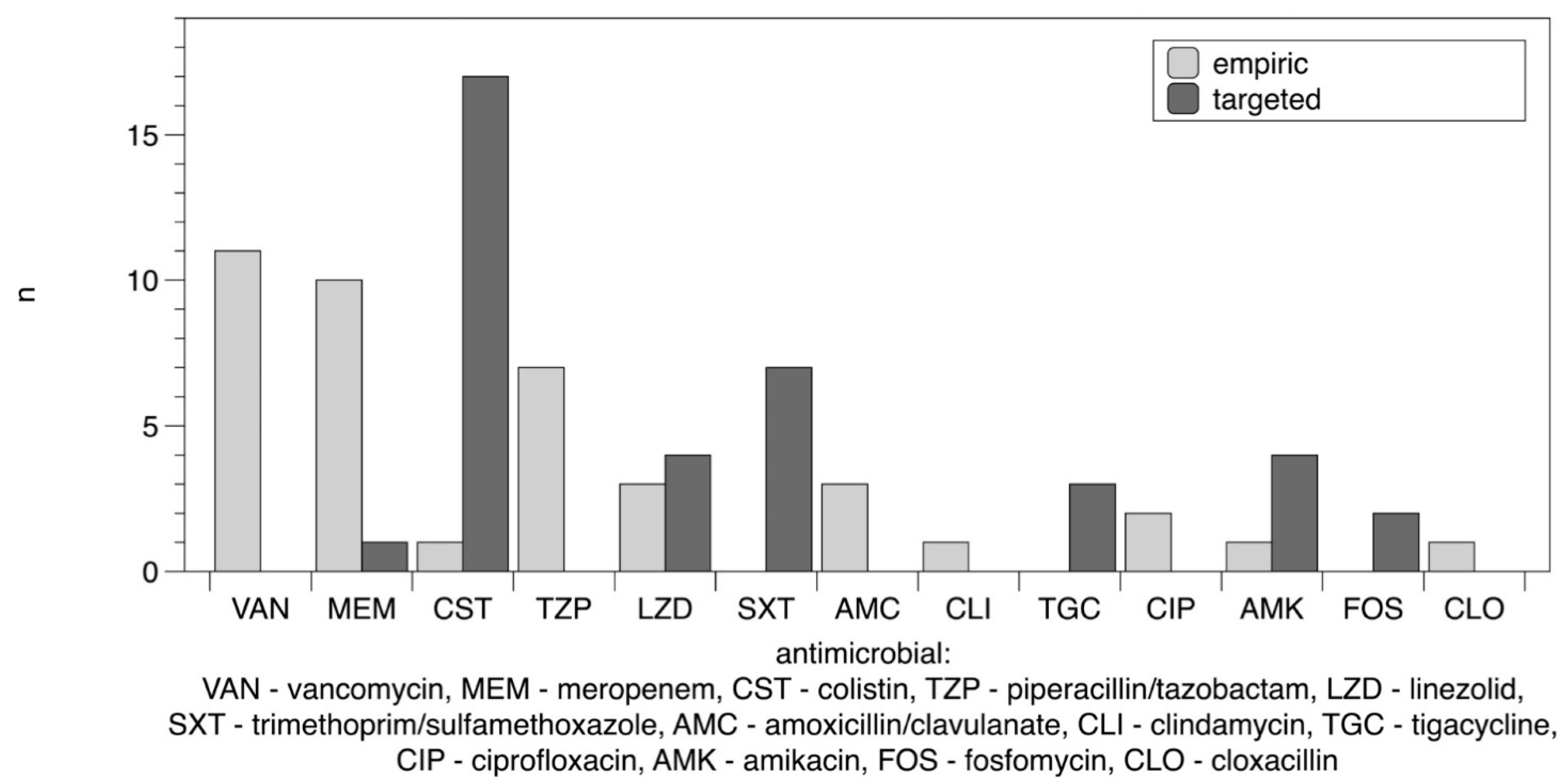
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- COVID-19 Coronavirus Pandemic. Available online: https://www.worldometers.info/coronavirus/ (accessed on 7 January 2022).
- Grasselli, G.; Pesenti, A.; Cecconi, M. Critical Care Utilization for the COVID-19 Outbreak in Lombardy, Italy: Early Experience and Forecast During an Emergency Response. JAMA 2020, 323, 1545. Available online: https://jamanetwork.com/journals/jama/fullarticle/2763188 (accessed on 7 January 2022). [CrossRef] [PubMed] [Green Version]
- Livingston, E.; Bucher, K. Coronavirus Disease 2019 (COVID-19) in Italy. JAMA 2020, 323, 1335. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; McGoogan, J.M. Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases from the Chinese Center for Disease Control and Prevention. JAMA 2020, 323, 1239. [Google Scholar] [CrossRef]
- Murthy, S.; Archambault, P.M.; Atique, A.; Carrier, F.M.; Cheng, M.P.; Codan, C.; Daneman, N.; Dechert, W.; Douglas, S.; Fiest, K.M.; et al. Characteristics and outcomes of patients with COVID-19 admitted to hospital and intensive care in the first phase of the pandemic in Canada: A national cohort study. Can. Med. Assoc. Open Access J. 2021, 9, E181–E188. [Google Scholar] [CrossRef]
- Arentz, M.; Yim, E.; Klaff, L.; Lokhandwala, S.; Riedo, F.X.; Chong, M.; Lee, M. Characteristics and Outcomes of 21 Critically Ill Patients with COVID-19 in Washington State. JAMA 2020, 323, 1612. [Google Scholar] [CrossRef] [Green Version]
- Richardson, S.; Hirsch, J.S.; Narasimhan, M.; Crawford, J.M.; McGinn, T.; Davidson, K.W.; Barnaby, D.P.; Becker, L.B.; Chelico, J.D.; Cohen, S.L.; et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized with COVID-19 in the New York City Area. JAMA 2020, 323, 2052. [Google Scholar] [CrossRef]
- Porretta, A.D.; Baggiani, A.; Arzilli, G.; Casigliani, V.; Mariotti, T.; Mariottini, F.; Scardina, G.; Sironi, D.; Totaro, M.; Barnini, S.; et al. Increased Risk of Acquisition of New Delhi Metallo-Beta-Lactamase-Producing Carbapenem-Resistant Enterobacterales (NDM-CRE) among a Cohort of COVID-19 Patients in a Teaching Hospital in Tuscany, Italy. Pathogens 2020, 9, 635. [Google Scholar] [CrossRef]
- Tiri, B.; Sensi, E.; Marsiliani, V.; Cantarini, M.; Priante, G.; Vernelli, C.; Martella, L.A.; Costantini, M.; Mariottini, A.; Andreani, P.; et al. Antimicrobial Stewardship Program, COVID-19, and Infection Control: Spread of Carbapenem-Resistant Klebsiella Pneumoniae Colonization in ICU COVID-19 Patients. What Did Not Work? J. Clin. Med. 2020, 9, 2744. [Google Scholar] [CrossRef]
- Kampmeier, S.; Tönnies, H.; Correa-Martinez, C.L.; Mellmann, A.; Schwierzeck, V. A nosocomial cluster of vancomycin resistant enterococci among COVID-19 patients in an intensive care unit. Antimicrob. Resist. Infect. Control 2020, 9, 154. [Google Scholar] [CrossRef]
- Nori, P.; Szymczak, W.; Puius, Y.; Sharma, A.; Cowman, K.; Gialanella, P.; Fleischner, Z.; Corpuz, M.; Torres-Isasiga, J.; Bartash, R.; et al. Emerging Co-Pathogens: New Delhi Metallo-beta-lactamase producing Enterobacterales Infections in New York City COVID-19 Patients. Int. J. Antimicrob. Agents 2020, 56, 106179. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Risk Assessment on the Spread of Carbapenemase-Producing Enterobacteriaceae (CPE): Through Patient Transfer between Healthcare Facilities, with Special Emphasis on Cross-Border Transfer; Publications Office: Luxembourg, 2011; Available online: https://data.europa.eu/doi/10.2900/59034 (accessed on 7 January 2022).
- Clinical Breakpoints—Breakpoints and Guidance. Available online: https://www.eucast.org/clinical_breakpoints/ (accessed on 7 January 2022).
- Mędrzycka-Dąbrowska, W.; Lange, S.; Zorena, K.; Dąbrowski, S.; Ozga, D.; Tomaszek, L. Carbapenem-Resistant Klebsiella pneumoniae Infections in ICU COVID-19 Patients—A Scoping Review. J. Clin. Med. 2021, 10, 2067. [Google Scholar] [CrossRef] [PubMed]
- Bentivegna, E.; Luciani, M.; Arcari, L.; Santino, I.; Simmaco, M.; Martelletti, P. Reduction of Multidrug-Resistant (MDR) Bacterial Infections during the COVID-19 Pandemic: A Retrospective Study. Int. J. Environ. Res. Public Health 2021, 18, 1003. [Google Scholar] [CrossRef] [PubMed]
- Montrucchio, G.; Corcione, S.; Sales, G.; Curtoni, A.; de Rosa, F.G.; Brazzi, L. Carbapenem-resistant Klebsiella pneumoniae in ICU-admitted COVID-19 patients: Keep an eye on the ball. J. Glob. Antimicrob. Resist. 2020, 23, 398–400. [Google Scholar] [CrossRef]
- Mathers, A.J.; Vegesana, K.; German-Mesner, I.; Ainsworth, J.; Pannone, A.; Crook, D.W.; Sifri, C.D.; Sheppard, A.; Stoesser, N.; Peto, T.; et al. Risk factors for Klebsiella pneumoniae carbapenemase (KPC) gene acquisition and clinical outcomes across multiple bacterial species. J. Hosp. Infect. 2020, 104, 456–468. [Google Scholar] [CrossRef] [Green Version]
- Salinas, A.F.; Mortari, E.P.; Terreri, S.; Quintarelli, C.; Pulvirenti, F.; Di Cecca, S.; Guercio, M.; Milito, C.; Bonanni, L.; Auria, S.; et al. SARS-CoV-2 Vaccine Induced Atypical Immune Responses in Antibody Defects: Everybody Does their Best. J. Clin. Immunol. 2021, 41, 1709–1722. [Google Scholar] [CrossRef]
- Hu, C.; Li, J.; Xing, X.; Gao, J.; Zhao, S.; Xing, L. The effect of age on the clinical and immune characteristics of critically ill patients with COVID-19: A preliminary report. PLoS ONE 2021, 16, e0248675. [Google Scholar] [CrossRef]
- Feng, X.; Li, S.; Sun, Q.; Zhu, J.; Chen, B.; Xiong, M.; Cao, G. Immune-Inflammatory Parameters in COVID-19 Cases: A Systematic Review and Meta-Analysis. Front. Med. 2020, 7, 301. [Google Scholar] [CrossRef]
- Sayah, W.; Berkane, I.; Guermache, I.; Sabri, M.; Lakhal, F.Z.; Rahali, S.Y.; Djidjeli, A.; Merah, F.; Belaid, B.; Berkani, L.; et al. Interleukin-6, procalcitonin and neutrophil-to-lymphocyte ratio: Potential immune-inflammatory parameters to identify severe and fatal forms of COVID-19. Cytokine 2021, 141, 155428. [Google Scholar] [CrossRef]
- Karruli, A.; Boccia, F.; Gagliardi, M.; Patauner, F.; Ursi, M.P.; Sommese, P.; de Rosa, R.; Murino, P.; Ruocco, G.; Corcione, A.; et al. Multidrug-Resistant Infections and Outcome of Critically Ill Patients with Coronavirus Disease 2019: A Single Center Experience. Microb. Drug Resist. 2021, 27, 1167–1175. [Google Scholar] [CrossRef]
- Aljuhani, O.; Al Sulaiman, K.; Alshabasy, A.; Eljaaly, K.; Al Shaya, A.I.; Noureldeen, H.; Aboudeif, M.; Al Dosari, B.; Alkhalaf, A.; Korayem, G.B.; et al. Association between tocilizumab and emerging multidrug-resistant organisms in critically ill patients with COVID-19: A multicenter, retrospective cohort study. BMC Infect. Dis. 2021, 21, 1127. [Google Scholar] [CrossRef] [PubMed]
- Chedid, M.; Waked, R.; Haddad, E.; Chetata, N.; Saliba, G.; Choucair, J. Antibiotics in treatment of COVID-19 complications: A review of frequency, indications, and efficacy. J. Infect. Public Health 2021, 14, 570–576. [Google Scholar] [CrossRef] [PubMed]
- Arteaga-Livias, K.; Pinzas-Acosta, K.; Perez-Abad, L.; Panduro-Correa, V.; Rabaan, A.A.; Pecho-Silva, S.; Dámaso-Mata, B. A multidrug-resistant Klebsiella pneumoniae outbreak in a Peruvian hospital: Another threat from the COVID-19 pandemic. Infect. Control Hosp. Epidemiol. 2021, 43, 267–268. [Google Scholar] [CrossRef] [PubMed]
- Liew, Y.; Lee, W.H.; Tan, L.; Kwa, A.L.; Thien, S.Y.; Cherng, B.P.; Chung, S.J. Antimicrobial stewardship programme: A vital resource for hospitals during the global outbreak of coronavirus disease 2019 (COVID-19). Int. J. Antimicrob. Agents 2020, 56, 106145. [Google Scholar] [CrossRef] [PubMed]
- Amarsy, R.; Jacquier, H.; Munier, A.L.; Merimèche, M.; Berçot, B.; Mégarbane, B. Outbreak of NDM-1-producing Klebsiella pneumoniae in the intensive care unit during the COVID-19 pandemic: Another nightmare. Am. J. Infect. Control 2021, 49, 1324–1326. [Google Scholar] [CrossRef] [PubMed]
- Rawson, T.M.; Moore, L.S.; Zhu, N.; Ranganathan, N.; Skolimowska, K.; Gilchrist, M.; Satta, G.; Cooke, G.; Holmes, A. Bacterial and Fungal Coinfection in Individuals with Coronavirus: A Rapid Review to Support COVID-19 Antimicrobial Prescribing. Clin. Infect. Dis. 2020, 71, 2459–2468. [Google Scholar] [CrossRef] [PubMed]
- Nori, P.; Cowman, K.; Chen, V.; Bartash, R.; Szymczak, W.; Madaline, T.; Katiyar, C.P.; Jain, R.; Aldrich, M.; Weston, G.; et al. Bacterial and fungal coinfections in COVID-19 patients hospitalized during the New York City pandemic surge. Infect. Control Hosp. Epidemiol. 2021, 42, 84–88. [Google Scholar] [CrossRef]
- Hughes, S.; Troise, O.; Donaldson, H.; Mughal, N.; Moore, L.S.P. Bacterial and fungal coinfection among hospitalized patients with COVID-19: A retrospective cohort study in a UK secondary-care setting. Clin. Microbiol. Infect. 2020, 26, 1395–1399. [Google Scholar] [CrossRef]
- Baiou, A.; Elbuzidi, A.A.; Bakdach, D.; Zaqout, A.; Alarbi, K.M.; Bintaher, A.A.; Ali, M.M.; Elarabi, A.M.; Ali, G.A.; Daghfal, J.; et al. Clinical characteristics and risk factors for the isolation of multi-drug-resistant Gram-negative bacteria from critically ill patients with COVID-19. J. Hosp. Infect. 2021, 110, 165–171. [Google Scholar] [CrossRef]
- Parisi, S.G.; Bartolini, A.; Santacatterina, E.; Castellani, E.; Ghirardo, R.; Berto, A.; Franchin, E.; Menegotto, N.; de Canale, E.; Tommasini, T.; et al. Prevalence of Klebsiella pneumoniae strains producing carbapenemases and increase of resistance to colistin in an Italian teaching hospital from January 2012 to December 2014. BMC Infect. Dis. 2015, 15, 244. [Google Scholar] [CrossRef] [Green Version]
| Patient Number | Age, Gender | Comorbidities | Duration of Hospitalization (Days) | COVID Treatment | Empiric Antimicrobial Treatment | Targeted Antimicrobial Treatment | Origin of K. pneumoniae Isolates | Superimposed Infection | Days from ICU Admission to the Isolation of K. pneumoniae NDM in Urine | The Highest Concentration of IL-6 | The Highest Concentration of PCT | The Highest Concentration of CRP | Outcome | Occurrence of Clostridioides difficile |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 71, M | hypertension Multiple sclerosis | 17 | remdesivir steroids plasma of convalescents | vancomycin meropenem fluconazole | colistin | urine respiratory tract rectum | 7 | 14.7 | 0.46 | 30.1 | died | no | |
| 2 | 73, M | diabetes | 35 | remdesivir steroids clarithromycin | vancomycin meropenem fluconazole | colistin micafungin | urine respiratory tract rectum | P. aeruginosa C. glabrata | 21 | NA | 0.21 | 29.4 | alive | no |
| 3 | 46, M | diabetes obesity | 9 | steroids | vancomycin fluconazole | colistin | urine | A. baumannii | 2 | NA | 0.53 | 23.4 | died | no |
| 4 | 39, M | hypertension obesity depression | 14 | steroids | ceftriaxone PIP/TAZO | meropenem linezolid fluconazole | urine rectum | 14 | 146.7 | 4.17 | 13.3 | died | no | |
| 5 | 66, F | hypertension diabetes hypercholesterolemia | 23 | steroids | vancomycin PIP/TAZO fluconazole | TMT/SMX | urine respiratory tract rectum | A. baumannii | 9 | NA | 20.39 | 67.7 | died | no |
| 6 | 75, F | epilepsy atherosclerosis | 30 | steroids | amox/clav | colistin | urine respiratory tract | 13 | NA | 0.14 | 5.0 | alive | yes | |
| 7 | 71, M | hypertension alcohol abuse | 18 | steroids | amox/clav meropenem vancomycin | colistin TMT/SMX | urine | 11 | NA | 8.93 | 16.5 | died | no | |
| 8 | 68, F | CHD | 26 | remdesivir steroids | ceftriaxone | colistin TMT/SMX linezolid | urine | MRSA P. aeruginosa | 8 | 180.7 | 0.12 | 14.8 | alive | no |
| 9 | 45, F | obesity hypothyroidism | 17 | remdesivir steroids | vancomycin meropenem | colistin linezolid fluconazole | urine rectum | 5 | NA | 0.26 | 32.8 | died | no | |
| 10 | 20, M | 36 | remdesivir steroids | ceftriaxone clindamycin vancomycin | colistin tigecycline linezolid fluconazole micafungin | urine respiratory tract rectum | A. baumannii C. albicans | 4 | NA | 3.04 | 27.8 | alive | no | |
| 11 | 76, M | CHD heart failure myelodysplastic syndrome history of stroke | 34 | steroids plasma of convalescents | ceftriaxone ciprofloxacin amox/clav | colistin | urine | 30 | NA | 29.99 | 21.6 | alive | yes | |
| 12 | 74, F | meningioma | 16 | remdesivir steroids plasma of convalescents | vancomycin meropenem fluconazole | colistin | urine respiratory tract rectum | 14 | 384.8 | 2.28 | 41.1 | died | no | |
| 13 | 78. M | hypertension | 47 | steroids | ceftriaxone ciprofloxacin PIP/TAZO | colistin TMT/SMX amikacin fluconazole | urine | A. baumannii C. albicans C. glabrata | 5 | NA | 8.59 | 48.0 | died | yes |
| 14 | 48, M | hypertension diabetes morbid obesity | 29 | steroids | ceftriaxone | colistin fosfomycin tigecycline TMT/SMX | blood catheter tip urine respiratory tract | A. baumannii | 10 | NA | 46.53 | 26.0 | died | no |
| 15 | 67, M | CHD hypertension diabetes renal failure | 21 | steroids | meropenem linezolid | colistin fluconazole | urine rectum | A. baumannii C. albicans | 8 | 189.1 | 1.18 | 30.1 | died | no |
| 16 | 44, M | 22 | steroids | vancomycin meropenem fluconazole | colistin amikacin | blood urine respiratory tract rectum | A. baumannii | 3 | 670.2 | 30.6 | 27.6 | died | no | |
| 17 | 35, F | obesity | 22 | steroids | PIP/TAZO linezolid | colistin amikacin TMT/SMX | urine | 13 | NA | 12.71 | 14.9 | alive | no | |
| 18 | 70, M | hypertension | 19 | remdesivir steroids | vancomycin meropenem fluconazole cloxacillin | * | urine rectum | A. baumannii | 13 | NA | 1.7 | 33.4 | died | no |
| 19 | 77, F | hypertension | 18 | remdesivir steroids | ceftriaxone | * | urine respiratory tract rectum | A. baumannii | 12 | NA | 0.31 | 27.3 | died | no |
| 20 | 61, M | 33 | steroids tocilizumab | PIP/TAZO meropenem linezolid | colistin amikacin | urine respiratory tract rectum | A. baumannii | 6 | 1331.5 | 2.83 | 23.7 | alive | no | |
| 21 | 61, M | 38 | steroids | ceftriaxone amikacin PIP/TAZO | colistin tigecycline fosfomycin fluconazole | urine respiratory tract rectum | 22 | 89.8 | 0.40 | 21.8 | alive | no | ||
| 22 | 43, M | morbid obesity | 12 | steroids | none | * | urine | 6 | NA | 0.67 | 15.4 | died | no | |
| 23 | 58, M | 34 | steroids | PIP/TAZO meropenem vancomycin | colistin TMT/SMX fluconazole | urine rectum | 25 | NA | 0.44 | 31.9 | alive | no |
| Antimicrobial Agent | Susceptibility | Resistance | ||
|---|---|---|---|---|
| n | Percent | n | Percent | |
| amikacin (AM) | 0 | 0.0% | 23 | 100% |
| amoxicillin/clavulanate (AMC) | 0 | 0.0% | 23 | 100% |
| cefepime (FEP) | 0 | 0.0% | 23 | 100% |
| cefotaxime (CTX) | 0 | 0.0% | 23 | 100% |
| ceftazidime (CAZ) | 0 | 0.0% | 23 | 100% |
| cefuroxime (CF) | 0 | 0.0% | 23 | 100% |
| cefuroxime axetil (CFA) | 0 | 0.0% | 23 | 100% |
| ciprofloxacin (CIP) | 0 | 0.0% | 23 | 100% |
| colistin (CS) | 18 | 78.26% | 5 | 21.74% |
| fosfomycin (FOS) | 12 | 52.17% | 11 | 47.83% |
| gentamycin (GN) | 2 | 8.70% | 21 | 91.30% |
| imipenem (IMI) | 0 | 0.0% | 23 | 100% |
| meropenem (MEM) | 0 | 0.0% | 23 | 100% |
| norfloxacin (NOR) | 0 | 0.0% | 23 | 100% |
| piperacillin/tazobactam (TZP) | 0 | 0.0% | 23 | 100% |
| tigecycline (TGC) | 1 | 4.35% | 22 | 95.65% |
| tobramycin (TOB) | 0 | 0.0% | 23 | 100% |
| trimethoprim/sulfamethoxazole (SXT) | 11 | 47.83% | 12 | 52.17% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guzek, A.; Rybicki, Z.; Woźniak-Kosek, A.; Tomaszewski, D. The Clinical Manifestation of SARS-CoV-2 in Critically Ill Patients with Klebsiella pneumoniae NDM Hospitalized in the ICU of a Modular Hospital during the Third Wave of the Pandemic in Poland—An Observational Cohort Study. Diagnostics 2022, 12, 1118. https://doi.org/10.3390/diagnostics12051118
Guzek A, Rybicki Z, Woźniak-Kosek A, Tomaszewski D. The Clinical Manifestation of SARS-CoV-2 in Critically Ill Patients with Klebsiella pneumoniae NDM Hospitalized in the ICU of a Modular Hospital during the Third Wave of the Pandemic in Poland—An Observational Cohort Study. Diagnostics. 2022; 12(5):1118. https://doi.org/10.3390/diagnostics12051118
Chicago/Turabian StyleGuzek, Aneta, Zbigniew Rybicki, Agnieszka Woźniak-Kosek, and Dariusz Tomaszewski. 2022. "The Clinical Manifestation of SARS-CoV-2 in Critically Ill Patients with Klebsiella pneumoniae NDM Hospitalized in the ICU of a Modular Hospital during the Third Wave of the Pandemic in Poland—An Observational Cohort Study" Diagnostics 12, no. 5: 1118. https://doi.org/10.3390/diagnostics12051118
APA StyleGuzek, A., Rybicki, Z., Woźniak-Kosek, A., & Tomaszewski, D. (2022). The Clinical Manifestation of SARS-CoV-2 in Critically Ill Patients with Klebsiella pneumoniae NDM Hospitalized in the ICU of a Modular Hospital during the Third Wave of the Pandemic in Poland—An Observational Cohort Study. Diagnostics, 12(5), 1118. https://doi.org/10.3390/diagnostics12051118






