Detection of Incomplete Irreversible Electroporation (IRE) and Microwave Ablation (MWA) of Hepatocellular Carcinoma (HCC) Using Iodine Quantification in Dual Energy Computed Tomography (DECT)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Participant Selection and Patient Characteristics
2.2. Irreversible Electroporation (IRE)
2.3. Microwave Ablation (MWA)
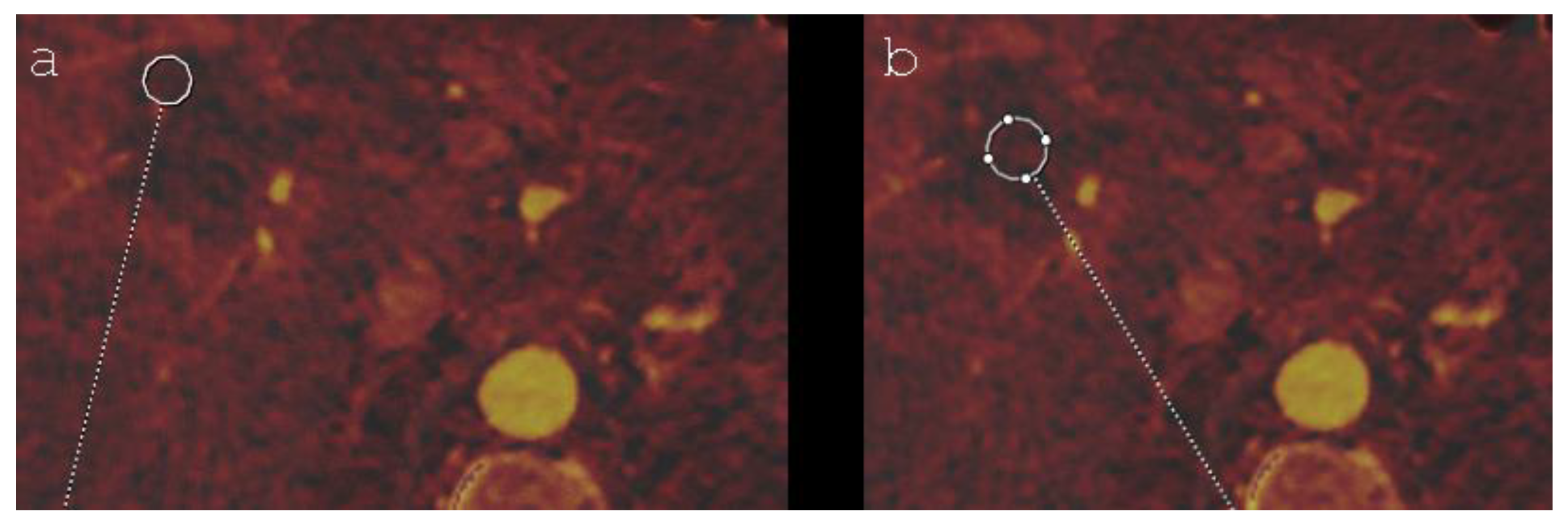
2.4. Image Acquisition and Evaluation
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sasson, A.R.; Sigurdson, E.R. Surgical treatment of liver metastases. Semin. Oncol. 2002, 29, 107–118. [Google Scholar] [CrossRef]
- Ahmed, M. Image-guided tumor ablation: Standardization of terminology and reporting criteria—A 10-year update: Supplement to the consensus document. J. Vasc. Interv. Radiol. 2014, 25, 1706–1708. [Google Scholar] [CrossRef] [PubMed]
- Dollinger, M.; Müller-Wille, R.; Zeman, F.; Haimerl, M.; Niessen, C.; Beyer, L.P.; Lang, S.A.; Teufel, A.; Stroszczynski, C.; Wiggermann, P. Irreversible electroporation of malignant hepatic tumors—Alterations in venous structures at subacute follow-up and evolution at mid-term follow-up. PLoS ONE 2015, 10, 0135773. [Google Scholar] [CrossRef] [PubMed]
- Rubinsky, B.; Onik, G.; Mikus, P. Irreversible electroporation: A new ablation modality-clinical implications. Technol. Cancer Res. Treat. 2007, 6, 37–48. [Google Scholar] [CrossRef] [PubMed]
- Meloni, M.F.; Andreano, A.; Bovo, G.; Chiarpotto, B.; Amabile, C.; Gelsomino, S.; Lazzaroni, S.; Sironi, S. Acute portal venous injury after microwave ablation in an in vivo porcine model: A rare possible complication. J. Vasc. Interv. Radiol. 2011, 22, 947–951. [Google Scholar] [CrossRef] [PubMed]
- Crocetti, L.; De Baere, T.; Lencioni, R. Quality improvement guidelines for radiofrequency ablation of liver tumours. Cardiovasc. Intervent. Radiol. 2010, 33, 11–17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Din, A.T.U.; Chaudhary, F.M.D.; Chaudhary, N.A.; Siddiqui, K.H. Irreversible electroporation for liver tumors: A review of literature. Cureus 2019, 11, e4994. [Google Scholar]
- Mathy, R.M.; Tinoush, P.; da Florencia, R.D.; Braun, A.; Ghamarnejad, O.; Radeleff, B.; Kauczor, H.-U.; Chang, D.-H. Impact of needle positioning on ablation success of irreversible electroporation: A unicentric retrospective analysis. Sci. Rep. 2020, 10, 21902. [Google Scholar] [CrossRef]
- Sutter, O.; Calvo, J.; N’Kontchou, G.; Nault, J.C.; Ourabia, R.; Nahon, P.; Ganne-Carrié, N.; Bourcier, V.; Zentar, N.; Bouhafs, F.; et al. Safety and efficacy of irreversible electroporation for the treatment of hepatocellular carcinoma not amenable to thermal ablation techniques: A retrospective single-center case series. Radiology 2017, 284, 877–886. [Google Scholar] [CrossRef]
- Gazelle, G.S.; Goldberg, S.N.; Solbiati, L.; Livraghi, T. Tumor ablation with radio-frequency energy. Radiology 2000, 217, 633–646. [Google Scholar] [CrossRef]
- Lewin, J.S.; Connell, C.F.; Duerk, J.L.; Chung, Y.-C.; Clampitt, M.E.; Spisak, J.; Gazelle, G.S.; Haaga, J.R. Interactive MRI-guided radiofrequency interstitial thermal ablation of abdominal tumors: Clinical trial for evaluation of safety and feasibility. J. Magn. Reson. Imaging 1998, 8, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Bäumler, W.; Wiggermann, P.; Lürken, L.; Dollinger, M.; Stroszczynski, C.; Beyer, L.; Schicho, A. Early detection of local tumor progression after irreversible electroporation (IRE) of a hepatocellular carcinoma using Gd-EOB-DTPA-based MR imaging at 3T. Cancers 2021, 13, 1595. [Google Scholar] [CrossRef] [PubMed]
- Skornitzke, S.; Fritz, F.; Mayer, P.; Koell, M.; Hansen, J.; Pahn, G.; Hackert, T.; Kauczor, H.-U. Dual-energy CT iodine maps as an alternative quantitative imaging biomarker to abdominal CT perfusion: Determination of appropriate trigger delays for acquisition using bolus tracking. Br. J. Radiol. 2018, 91, 20170351. [Google Scholar] [CrossRef]
- Wolfram, S.; Stephan, S.; Franziska, F.; Miriam, K.; Jens, H.; Gregor, P.; Lars, G.; Hans-Ulrich, K. Correlation of quantitative dual-energy computed tomography iodine maps and abdominal computed tomography perfusion measurements: Are single-acquisition dual-energy computed tomography iodine maps more than a reduced-dose surrogate of conventional computed tomography perfusion? Investig. Radiol. 2015, 50, 703–708. [Google Scholar]
- Llovet, J.M.; Bru, C.; Bruix, J. Prognosis of hepatocellular carcinoma: The BCLC staging classification. Semin. Liver Dis. 1999, 19, 329–338. [Google Scholar] [CrossRef] [PubMed]
- Niessen, C.; Igl, J.; Pregler, B.; Beyer, L.; Noeva, E.; Dollinger, M.; Schreyer, A.G.; Jung, E.M.; Stroszczynski, C.; Wiggermann, P. Factors associated with short-term local recurrence of liver cancer after percutaneous ablation using irreversible electroporation: A prospective single-center study. J. Vasc. Interv. Radiol. 2015, 26, 694–702. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, M.; Solbiati, L.; Brace, C.L.; Breen, D.J.; Callstrom, M.R.; Charboneau, J.W.; Chen, M.-H.; Choi, B.I.; De Baère, T.; Dodd, G.D., III; et al. Image-guided tumor ablation: Standardization of terminology and reporting criteria-a 10-year update. Radiology 2014, 273, 241–260. [Google Scholar] [CrossRef] [PubMed]
- Izzo, F.; Granata, V.; Grassi, R.; Fusco, R.; Palaia, R.; Delrio, P.; Carrafiello, G.; Azoulay, D.; Petrillo, A.; A Curley, S. Radiofrequency ablation and microwave ablation in liver tumors: An update. Oncologist 2019, 24, e990–e1005. [Google Scholar] [CrossRef] [Green Version]
- Kurilova, I.; Gonzalez-Aguirre, A.; Beets-Tan, R.G.; Erinjeri, J.; Petre, E.N.; Gonen, M.; Bains, M.; Kemeny, N.E.; Solomon, S.B.; Sofocleous, C.T. Microwave ablation in the management of colorectal cancer pulmonary metastases. Cardiovasc. Interv. Radiol. 2018, 41, 1530–1544. [Google Scholar] [CrossRef]
- Schaible, J.; Pregler, B.; Bäumler, W.; Einspieler, I.; Jung, E.-M.; Stroszczynski, C.; Beyer, L.P. Safety margin assessment after microwave ablation of liver tumors: Inter- and intrareader variability. Radiol. Oncol. 2020, 54, 57–61. [Google Scholar] [CrossRef] [Green Version]
- Distelmaier, M.; Barabasch, A.; Heil, P.; Kraemer, N.; Isfort, P.; Keil, S.; Kuhl, C.; Bruners, P. Midterm safety and efficacy of irreversible electroporation of malignant liver tumors located close to major portal or hepatic veins. Radiology 2017, 285, 1023–1031. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.W.; Chen, C.; Prieto, V.E.; Dry, S.M.; Loh, C.T.; Kee, S.T. Advanced hepatic ablation technique for creating complete cell death: Irreversible electroporation. Radiology 2010, 255, 426–433. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.; Loh, C.T.; Kee, S.T. Imaging guided percutaneous irreversible electroporation: Ultrasound and immunohistological correlation. Technol. Cancer Res. Treat. 2007, 6, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Zhang, Y.; Klein, R.; Nijm, G.M.; Sahakian, A.V.; Omary, R.A.; Yang, G.-Y.; Larson, A.C. Irreversible electroporation therapy in the liver: Longitudinal efficacy studies in a rat model of hepatocellular carcinoma. Cancer Res. 2010, 70, 1555–1563. [Google Scholar] [CrossRef] [Green Version]
- Guo, Y.; Zhang, Y.; Nijm, G.M.; Sahakian, A.V.; Yang, G.-Y.; Omary, R.A.; Larson, A.C. Irreversible electroporation in the liver: Contrast-enhanced inversion-recovery MR imaging approaches to differentiate reversibly electroporated penumbra from irreversibly electroporated ablation zones. Radiology 2011, 258, 461–468. [Google Scholar] [CrossRef]
- Zhang, L.; Wang, N.; Mao, J.; Liu, X.; Gao, Z.; Dai, X.; Feng, B. Dual-energy CT-derived volumetric iodine concentration for the assessment of therapeutic response after microwave ablation in a rabbit model with intrahepatic VX2 tumor. J. Vasc. Interv. Radiol. 2018, 29, 1455–1461. [Google Scholar] [CrossRef]
- Padia, S.A.; Johnson, G.E.; Yeung, R.S.; Park, J.O.; Hippe, D.S.; Kogut, M.J. Irreversible electroporation in patients with hepatocellular carcinoma: Immediate versus delayed findings at MR imaging. Radiology 2016, 278, 285–294. [Google Scholar] [CrossRef] [Green Version]
- Yu, H.-C.; Cheng, J.-S.; Lai, K.-H.; Lin, C.-P.; Lo, G.-H.; Lin, C.-K.; Hsu, P.-I.; Chan, H.-H.; Lo, C.-C.; Tsai, W.-L.; et al. Factors for early tumor recurrence of single small hepatocellular carcinoma after percutaneous radiofrequency ablation therapy. World J. Gastroenterol. 2005, 11, 1439–1444. [Google Scholar] [CrossRef]
- S3-Leitlinie Diagnostik und Therapie des Hepatozellulären Karzinoms und Biliärer Karzinome (Version 2). Available online: https://www.leitlinienprogramm-onkologie.de/fileadmin/user_upload/Downloads/Leitlinien/HCC/Version_2/LL_HCC_bili%C3%A4re_Karzinome_Langversion_2.0.pdf (accessed on 3 April 2022).

| Characteristics | IRE | MWA |
|---|---|---|
| Number of patients | 27 | 27 |
| Age (years) | ||
| Mean ± SD | 70.2 ± 9.5 | 67.6 ± 10.5 |
| Range | 52−89 | 52−85 |
| Sex, n (%) | ||
| Male | 25 (92.6) | 25 (92.6) |
| Female | 2 (7.4) | 2 (7.4) |
| Diameter of the ablation area (cm) | ||
| Mean ± SD | 5.4 ± 0.9 | 5.4 ± 0.8 |
| Tumor localization, n (%) | ||
| Segment I | 2 (7.4) | 0 (0.0) |
| Segment II | 1 (3.7) | 3 (11.1) |
| Segment III | 3 (11.1) | 1 (3.7) |
| Segment IVa | 3 (11.1) | 1 (3.7) |
| Segment IVb | 1 (3.7) | 1 (3.7) |
| Segment V | 7 (25.9) | 7 (25.9) |
| Segment VI | 4 (14.9) | 4 (14.9) |
| Segment VII | 1 (3.7) | 3 (11.1) |
| Segment VIII | 5 (18.5) | 7 (25.9) |
| Tumor stage (BCLC System), n (%) | ||
| 0 | 2 (7.4) | 2 (7.4) |
| A1 | 10 (37.0) | 9 (33.3) |
| A2 | 8 (29.6) | 6 (22.3) |
| A3 | 7 (26.0) | 9 (33.3) |
| A4 | 0 (0) | 1 (3.7) |
| B | 0 (0) | 0 (0) |
| C | 0 (0) | 0 (0) |
| D | 0 (0) | 0 (0) |
| IRE | MWA | |||
|---|---|---|---|---|
| p-Value | 95% Confidence Interval | p-Value | 95% Confidence Interval | |
| Pair 1: Mean VIC (central ablation zone)–Mean VIC (peripheral ablation zone) | 0.000 | −0.85– (−0.44) | 0.110 | −0.28–0.03 |
| Pair 2: Mean VIC (non-ablated liver parenchyma)–Mean VIC (central ablation zone) | 0.000 | 0.96–1.31 | 0.000 | 0.44–0.94 |
| Pair 3: Mean VIC (non-ablated liver parenchyma)–Mean VIC (peripheral ablation zone) | 0.001 | 0.23–0.76 | 0.000 | 0.28–0.84 |
| Ablation Technique | Mean VIC (mg/mL) in Patients with Local Tumor Progression | Mean VIC (mg/mL) in Patients without Local Tumor Progression | p-Value | 95% Confidence Interval |
|---|---|---|---|---|
| IRE | 1.60 | 0.81 | 0.005 | 0.26–1.31 |
| MWA | 1.13 | 0.35 | 0.000 | 0.46–1.09 |
| Local Tumor Progression | IRE | MWA | ||
|---|---|---|---|---|
| p-Value | 95% Confidence Interval | p-Value | 95% Confidence Interval | |
| Yes | 0.155 | −0.24– 0.94 | 0.005 | 0.41–0.99 |
| No | 0.000 | −0.90–(−0.38) | 0.000 | −0.99–(−0.57) |
| Variable | OR (95% CI) | p-Value |
|---|---|---|
| Age | 0.97 (0.88–1.06) | 0.451 |
| Tumor stage (BCLC System) | 7.23 (1.67–31.22) | 0.008 * |
| Sex: female vs. male | 3.22 (0.24–43.66) | 0.379 |
| Tumor localization: segment I-IV vs. segment V-VIII | 1.82 (0.29–11.47) | 0.524 |
| Ablation method: IRE vs. MWA | 0.44 (0.08–2.25) | 0.320 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bäumler, W.; Beyer, L.P.; Lürken, L.; Wiggermann, P.; Stroszczynski, C.; Dollinger, M.; Schicho, A. Detection of Incomplete Irreversible Electroporation (IRE) and Microwave Ablation (MWA) of Hepatocellular Carcinoma (HCC) Using Iodine Quantification in Dual Energy Computed Tomography (DECT). Diagnostics 2022, 12, 986. https://doi.org/10.3390/diagnostics12040986
Bäumler W, Beyer LP, Lürken L, Wiggermann P, Stroszczynski C, Dollinger M, Schicho A. Detection of Incomplete Irreversible Electroporation (IRE) and Microwave Ablation (MWA) of Hepatocellular Carcinoma (HCC) Using Iodine Quantification in Dual Energy Computed Tomography (DECT). Diagnostics. 2022; 12(4):986. https://doi.org/10.3390/diagnostics12040986
Chicago/Turabian StyleBäumler, Wolf, Lukas Philipp Beyer, Lukas Lürken, Philipp Wiggermann, Christian Stroszczynski, Marco Dollinger, and Andreas Schicho. 2022. "Detection of Incomplete Irreversible Electroporation (IRE) and Microwave Ablation (MWA) of Hepatocellular Carcinoma (HCC) Using Iodine Quantification in Dual Energy Computed Tomography (DECT)" Diagnostics 12, no. 4: 986. https://doi.org/10.3390/diagnostics12040986
APA StyleBäumler, W., Beyer, L. P., Lürken, L., Wiggermann, P., Stroszczynski, C., Dollinger, M., & Schicho, A. (2022). Detection of Incomplete Irreversible Electroporation (IRE) and Microwave Ablation (MWA) of Hepatocellular Carcinoma (HCC) Using Iodine Quantification in Dual Energy Computed Tomography (DECT). Diagnostics, 12(4), 986. https://doi.org/10.3390/diagnostics12040986






