Validity and Reliability of the Staden Schizophrenia Anxiety Rating Scale
Abstract
:1. Introduction
2. Methods
2.1. Participants
2.2. Assessments and Measuring Instruments
2.3. Procedures and Ethics Approval
2.4. Statistical Analyses
3. Results
3.1. Descriptive Features
3.2. Convergent and Criterion-Related Validity
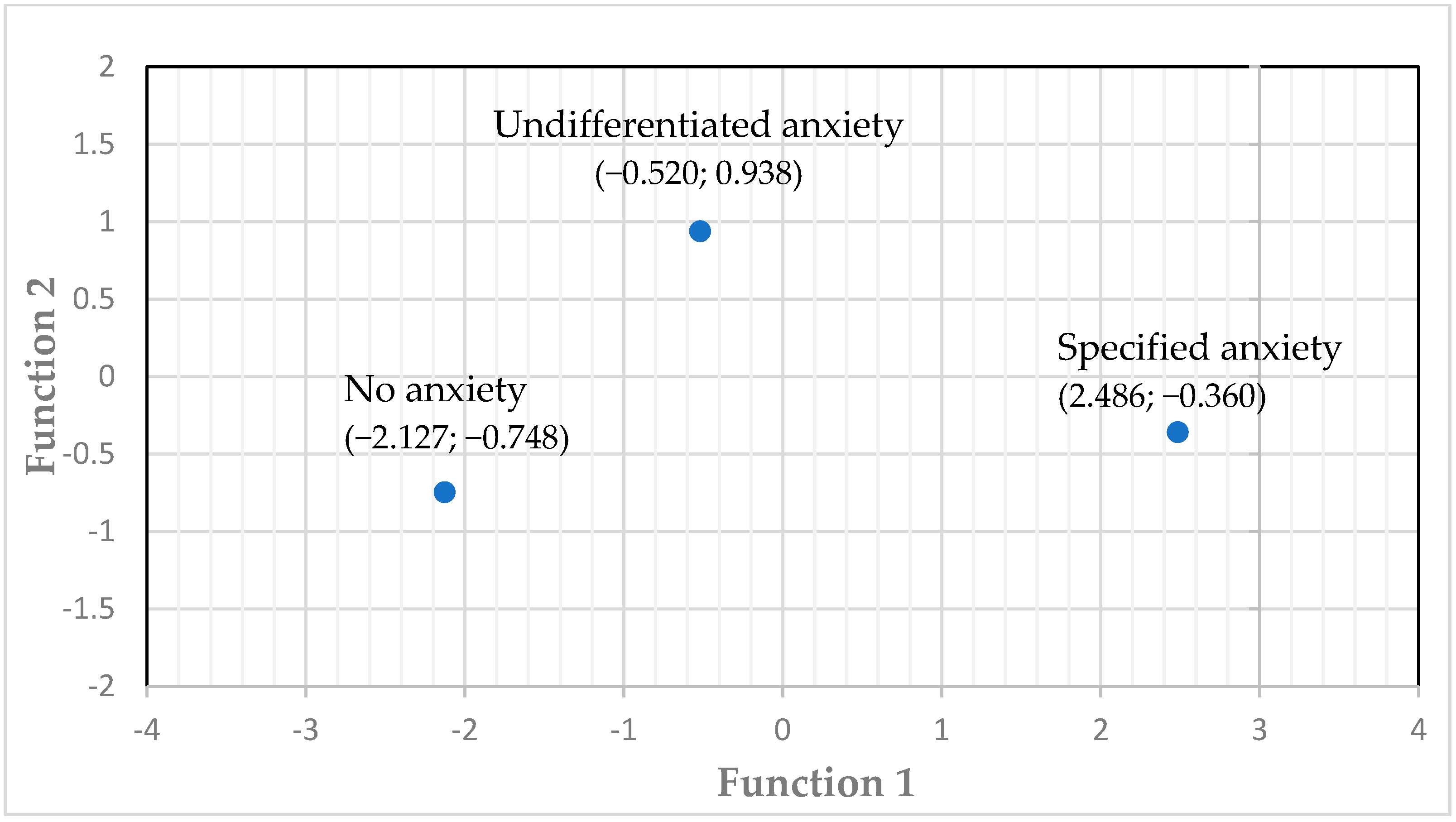
3.3. Discriminant Validity
3.4. Internal Consistency and Split-Half Reliability
3.5. Standard Error of Measurement
3.6. Structural Validity and Consistency of Measurement
3.7. Inter-Rater Reliability
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Naidu, K.; van Staden, W.; Fletcher, L. Discerning undifferentiated anxiety from syndromal anxiety in acute-phase schizophrenia. Ann. Gen. Psychiatry 2020, 19, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Achim, A.M.; Maziade, M.; Raymond, É.; Olivier, D.; Mérette, C.; Roy, M.-A. How prevalent are anxiety disorders in schizophrenia? A meta-analysis and critical review on a significant association. Schizophr. Bull. 2011, 37, 811–821. [Google Scholar] [CrossRef] [PubMed]
- Nebioglu, M.; Altindag, A. The prevalence of comorbid anxiety disorders in outpatients with schizophrenia. Int. J. Psychiatry Clin. Pract. 2009, 13, 312–317. [Google Scholar] [CrossRef] [PubMed]
- Kiran, C.; Chaudhury, S. Prevalence of comorbid anxiety disorders in schizophrenia. Ind. Psychiatry J. 2016, 25, 35. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Text Revision, 4th ed.; American Psychiatric Publishing: Arlington, VA, USA, 2000. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Arlington, VA, USA, 2013. [Google Scholar]
- Seedat, S.; Fritelli, V.; Oosthuizen, P.; Emsley, R.A.; Stein, D.J. Measuring anxiety in patients with schizophrenia. J. Nerv. Ment. Dis. 2007, 195, 320–324. [Google Scholar] [CrossRef]
- Smith, E.L.; Garety, P.A.; Harding, H.; Hardy, A. Are there reliable and valid measures of anxiety for people with psychosis? A systematic review of psychometric properties. Psychol. Psychother. Theory Res. Pract. 2021, 94, 173–198. [Google Scholar] [CrossRef]
- Naidu, K.; van Staden, W.C.; van der Linde, M. Severity of psychotic episodes in predicting concurrent depressive and anxiety features in acute phase schizophrenia. BMC Psychiatry 2014, 14, 1–7. [Google Scholar] [CrossRef]
- Temmingh, H.; Stein, D.J. Anxiety in patients with schizophrenia: Epidemiology and management. CNS Drugs 2015, 29, 819–832. [Google Scholar] [CrossRef]
- Bosanac, P.; Mancuso, S.G.; Castle, D.J. Anxiety symptoms in psychotic disorders: Results from the Second Australian National Mental Health Survey. Clin. Schizophr. Relat. Psychoses 2016, 10, 93–100. [Google Scholar] [CrossRef]
- Van Putten, T. The many faces of akathisia. Compr. Psychiatry 1975, 16, 43–47. [Google Scholar] [CrossRef]
- Howland, R.H.; Rush, A.J.; Wisniewski, S.R.; Trivedi, M.H.; Warden, D.; Fava, M.; Davis, L.L.; Balasubramani, G.; McGrath, P.; Berman, S.R. Concurrent anxiety and substance use disorders among outpatients with major depression: Clinical features and effect on treatment outcome. Drug Alcohol Depend. 2009, 99, 248–260. [Google Scholar] [CrossRef] [PubMed]
- Fusar-Poli, P.; Nelson, B.; Valmaggia, L.; Yung, A.R.; McGuire, P.K. Comorbid depressive and anxiety disorders in 509 individuals with an at-risk mental state: Impact on psychopathology and transition to psychosis. Schizophr. Bull. 2014, 40, 120–131. [Google Scholar] [CrossRef] [PubMed]
- Majadas, S.; Olivares, J.; Galan, J.; Diez, T. Prevalence of depression and its relationship with other clinical characteristics in a sample of patients with stable schizophrenia. Compr. Psychiatry 2012, 53, 145–151. [Google Scholar] [CrossRef] [PubMed]
- Veras, A.B.; Cougo, S.; Meira, F.; Peixoto, C.; Barros, J.A.; Nardi, A.E.; Malaspina, D.; Poyurovsky, M.; Kahn, J.P. Schizophrenia dissection by five anxiety and depressive subtype comorbidities: Clinical implications and evolutionary perspective. Psychiatry Res. 2017, 257, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Dlagnekova, A.; van Staden, W.; Masenge, A. Validity and reliability of the Vigour Assessment Scale in avolitional schizophrenia outpatients. Schizophr. Res. 2021, 235, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Kay, S.R.; Opler, L.A.; Lindenmayer, J.-P. Reliability and validity of the positive and negative syndrome scale for schizophrenics. Psychiatry Res. 1988, 23, 99–110. [Google Scholar] [CrossRef]
- Liemburg, E.; Castelein, S.; Stewart, R.; van der Gaag, M.; Aleman, A.; Knegtering, H.; Genetic Risk and Outcome of Psychosis (GROUP) Investigators. Two subdomains of negative symptoms in psychotic disorders: Established and confirmed in two large cohorts. J. Psychiatr. Res. 2013, 47, 718–725. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, M. The assessment of anxiety states by rating. Br. J. Med. Psychol. 1959, 32, 50–52. [Google Scholar] [CrossRef] [PubMed]
- First, M.B.S.R.; Miriam, G.; Williams, J.B.W. Structured Clinical Interview for DSM-IV-TR Axis I Disorders; Research Version, Non-Patient Edition. (SCID-I/NP); Biometrics Research, New York State Psychiatric Institute: New York, NY, USA, 2002. [Google Scholar]
- Lobbestael, J.; Leurgans, M.; Arntz, A. Inter-rater reliability of the Structured Clinical Interview for DSM-IV Axis I disorders (SCID I) and Axis II disorders (SCID II). Clin. Psychol. Psychother. 2011, 18, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Addington, D.; Addington, J.; Maticka-Tyndale, E. Assessing depression in schizophrenia: The Calgary Depression Scale. Br. J. Psychiatry 1993, 163, 39–44. [Google Scholar] [CrossRef]
- Addington, D.; Addington, J.; Atkinson, M. A psychometric comparison of the Calgary depression scale for schizophrenia and the Hamilton depression rating scale. Schizophr. Res. 1996, 19, 205–212. [Google Scholar] [CrossRef]
- Robitschek, C.; Ashton, M.W.; Spering, C.C.; Geiger, N.; Byers, D.; Schotts, G.C.; Megan, T.A. Development psychometric evaluation of the Personal Growth Initiative, Scale–II. J. Couns. Psychol. 2012, 59, 274. [Google Scholar] [CrossRef] [PubMed]
- Carver, C.S.; White, T.L. Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: The BIS/BAS scales. J. Personal. Soc. Psychol. 1994, 67, 319. [Google Scholar] [CrossRef]
- Barch, D.M.; Dowd, E.C. Goal representations and motivational drive in schizophrenia: The role of prefrontal–striatal interactions. Schizophr. Bull. 2010, 36, 919–934. [Google Scholar] [CrossRef] [PubMed]
- Reddy, L.F.; Green, M.F.; Rizzo, S.; Sugar, C.A.; Blanchard, J.J.; Gur, R.E.; Kring, A.M.; Horan, W.P. Behavioral approach and avoidance in schizophrenia: An evaluation of motivational profiles. Schizophr. Res. 2014, 159, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Yockey, R.D.; Kralowec, C.J. Confirmatory factor analysis of the procrastination assessment scale for students. Sage Open 2015, 5, 2158244015611456. [Google Scholar] [CrossRef]
- Ferrari, J.R. Reliability of academic and dispositional measures of procrastination. Psychol. Rep. 1989, 64 (Suppl. S3), 1057–1058. [Google Scholar] [CrossRef]
- Hasanagic, A.; Ozsagir, C.B. The Validity Exploration of General Procrastination Scale (Lay, 1986). Epihany 2018, 11. [Google Scholar] [CrossRef]
- De Vries, J.; Van der Steeg, A.F.; Roukema, J.A. Psychometric properties of the Fatigue Assessment Scale (FAS) in women with breast problems. Int. J. Clin. Health Psychol. 2010, 10, 125–139. [Google Scholar]
- Dunning, M.J.; Giallo, R. Fatigue, parenting stress, self-efficacy and satisfaction in mothers of infants and young children. J. Reprod. Infant Psychol. 2012, 30, 145–159. [Google Scholar] [CrossRef]
- Zhang, M.; Sparer, E.H.; Murphy, L.A.; Dennerlein, J.T.; Fang, D.; Katz, J.N.; Caban-Martinez, A.J. Development and validation of a fatigue assessment scale for US construction workers. Am. J. Ind. Med. 2015, 58, 220–228. [Google Scholar] [CrossRef] [PubMed]
- Prion, S.; Haerling, K.A. Making sense of methods and measurement: Pearson product-moment correlation coefficient. Clin. Simul. Nurs. 2014, 11, 587–588. [Google Scholar] [CrossRef]
- Campbell, D.T.; Fiske, D.W. Convergent and discriminant validation by the multitrait-multimethod matrix. Psychol. Bull. 1959, 56, 81–105. [Google Scholar] [CrossRef] [PubMed]
- Mvududu, N.H.; Sink, C.A. Factor analysis in counseling research and practice. Couns. Outcome Res. Eval. 2013, 4, 75–98. [Google Scholar] [CrossRef]
- Priebe, S.; McCabe, R.; Junghan, U.; Kallert, T.; Ruggeri, M.; Slade, M.; Reininghaus, U. Association between symptoms and quality of life in patients with schizophrenia: A pooled analysis of changes over time. Schizophr. Res. 2011, 133, 17–21. [Google Scholar] [CrossRef] [PubMed]
- Romm, K.L.; Melle, I.; Thoresen, C.; Andreassen, O.A.; Rossberg, J.I. Severe social anxiety in early psychosis is associated with poor premorbid functioning, depression, and reduced quality of life. Compr. Psychiatry 2012, 53, 434–440. [Google Scholar] [CrossRef]
- Achim, A.M.; Ouellet, R.; Lavoie, M.-A.; Vallières, C.; Jackson, P.L.; Roy, M.-A. Impact of social anxiety on social cognition and functioning in patients with recent-onset schizophrenia spectrum disorders. Schizophr. Res. 2013, 145, 75–81. [Google Scholar] [CrossRef]
- Wigman, J.T.; van Nierop, M.; Vollebergh, W.A.; Lieb, R.; Beesdo-Baum, K.; Wittchen, H.-U.; van Os, J. Evidence that psychotic symptoms are prevalent in disorders of anxiety and depression, impacting on illness onset, risk, and severity—implications for diagnosis and ultra–high risk research. Schizophr. Bull. 2012, 38, 247–257. [Google Scholar] [CrossRef]
- Lysaker, P.H.; Salyers, M.P. Anxiety symptoms in schizophrenia spectrum disorders: Associations with social function, positive and negative symptoms, hope and trauma history. Acta Psychiatr. Scand. 2007, 116, 290–298. [Google Scholar] [CrossRef]
- Juven-Wetzler, A.; Fostick, L.; Cwikel-Hamzany, S.; Balaban, E.; Zohar, J. Treatment with ziprasidone for schizophrenia patients with OCD. Eur. Neuropsychopharmacol. 2014, 24, 1454–1462. [Google Scholar] [CrossRef]
- Mazeh, D.; Bodner, E.; Weizman, R.; Delayahu, Y.; Cholostoy, A.; Martin, T.; Barak, Y. Co-morbid social phobia in schizophrenia. Int. J. Soc. Psychiatry 2009, 55, 198–202. [Google Scholar] [CrossRef] [PubMed]
- Tarrier, N.; Picken, A. Co-morbid PTSD and suicidality in individuals with schizophrenia and substance and alcohol abuse. Soc. Psychiatry Psychiatr. Epidemiol. 2011, 46, 1079–1086. [Google Scholar] [CrossRef] [PubMed]
- Le Moigne, A.; Csernansky, J.; Leadbetter, R.A.; Andorn, A.C.; Graham, J.A.; Heath, A.T.; Walling, D.P.; Newcomer, J.W.; Marder, S.R. PANSS Individual Item and Marder Dimension Analyses From a Pivotal Trial of RBP-7000 (Monthly Extended-Release Risperidone) in Schizophrenia Patients. J. Clin. Psychiatry 2021, 82, 37024. [Google Scholar] [CrossRef] [PubMed]
- Sakurai, H.; Yasui-Furukori, N.; Suzuki, T.; Uchida, H.; Baba, H.; Watanabe, K.; Inada, K.; Kikuchi, Y.S.; Kikuchi, T.; Katsuki, A.; et al. Pharmacological treatment of schizophrenia: Japanese expert consensus. Pharmacopsychiatry 2021, 54, 60–67. [Google Scholar] [CrossRef]
- Garay, R.P.; Samalin, L.; Hameg, A.; Llorca, P.-M. Investigational drugs for anxiety in patients with schizophrenia. Expert Opin. Investig. Drugs 2015, 24, 507–517. [Google Scholar] [CrossRef]
- McGrath, J.; Saha, S.; Chant, D.; Welham, J. Schizophrenia: A concise overview of incidence, prevalence, and mortality. Epidemiol. Rev. 2008, 30, 67–76. [Google Scholar] [CrossRef]
| Descriptive Feature | All Data Sets n = 353 | Data Set No 1 n = 60 | Data Set No 2 n = 51 | Data Set No 3 n = 242 | |
|---|---|---|---|---|---|
| Gender | Male | 74.5% n = 263 | 80% n = 48 | 76.5% n = 39 | 72.7% n = 176 |
| Female | 25.5% n = 90 | 20% n = 12 | 23.5% n = 12 | 27.3% n = 66 | |
| Age | Minimum | 18 | 19 | 19 | 18 |
| Maximum | 64 | 60 | 64 | 62 | |
| Mean | 36.7 | 33.8 | 37.0 | 37.4 | |
| Standard Deviation | 11.0 | 10.4 | 13.3 | 10.6 |
| Instrument | Descriptive | Combined Data Sets | Data Set No 1 n = 60 | Data Set No 2 n = 51 | Data Set No 3 n = 242 |
|---|---|---|---|---|---|
| Staden Schizophrenia Anxiety Rating Scale (S-SARS) | Mean | 6.75 | 14.58 | 18.88 | 2.26 |
| SD | 9.52 | 9.62 | 10.13 | 4.67 | |
| 95% CI 1 of the mean | 5.79–7.75 | 12.28–16.82 | 16.12–21.64 | 1.66–2.85 | |
| Hamilton Anxiety Scale (HAM-A) | Mean | 11.05 | 10.85 | 11.29 | No data |
| SD | 9.03 | 10.68 | 6.68 | No data | |
| 95% CI of the mean | 9.48–12.68 | 8.32–13.42 | 9.45–13.18 | No data | |
| Calgary Depressive Symptoms Scale (CDSS) | Mean | 5.69 | 5.05 | 6.45 | 1.33 |
| SD | 5.69 | 5.81 | 5.50 | 2.78 | |
| 95% CI of the mean | 4.54–6.73 | 3.58–6.47 | 5.02–7.94 | 0.98–1.69 | |
| Barnes Akathisia Scale (BAS) | Mean | 1.04 | 0.5 | 1.67 | No data |
| SD | 1.69 | 1.2 | 1.96 | No data | |
| 95% CI of the mean | 0.73–1.39 | 0.22–0.83 | 1.18–2.24 | No data | |
| Structured Clinical Interview for Positive and Negative Symptoms of Schizophrenia (SCI-PANSS) | Mean | 100.76 | 103.43 | 97.61 | No data |
| SD | 16.0 | 13.87 | 17.83 | No data | |
| 95% CI of the mean | 97.78–103.92 | 99.95–106.77 | 92.83–102.59 | No data | |
| Avolitional items on the SCI-PANSS (G13, N2, N4 on SCI-PANSS) | Mean | 12.65 | 10.28 | 10.18 | 13.76 |
| SD | 3.40 | 2.85 | 2.99 | 3.01 | |
| 95% CI of the mean | 12.29–13.0 | 9.52–11.02 | 9.33–10.94 | 13.38–14.14 |
| Instrument | Mean | Standard Deviation | 95% Confidence Interval of the Mean |
|---|---|---|---|
| Vigour Assessment Scale (VAS) | 12.02 | 25.42 | 8.81–15.24 |
| Personal Growth and Initiative Scale-II (PGIS–II) | 39.59 | 13.66 | 37.86–41.32 |
| Behaviour inhibition (BIS) | 19.82 | 4.38 | 19.19–20.37 |
| Drive (BAS-D) | 11.24 | 3.16 | 10.84–11.61 |
| Reward-responsiveness (BAS-RS) | 16.14 | 3.24 | 15.17–16.54 |
| Fun-seeking (BAS-FS) | 10.78 | 2.92 | 10.39–11.15 |
| Procrastination Scale (ProcS) | 56.64 | 12.17 | 55.1–58.2 |
| Fatigue Assessment Scale (FAS) | 24.96 | 8.70 | 23.86–26.06 |
| Instruments | S-SARS n = 353 | HAM-A n = 353 | CDSS n = 353 | BAS n = 111 | SCI-PANSS n = 111 | Avolitional Items on SCI-PANSS n = 111 |
|---|---|---|---|---|---|---|
| S-SARS | 1 | 0.711 | 0.722 | 0.418 | 0.455 | −0.268 |
| HAM-A | 0.711 | 1 | 0.581 | 0.320 | 0.258 | 0.123 |
| CDSS | 0.722 | 0.581 | 1 | 0.368 | 0.407 | 0.315 |
| BAS | 0.418 | 0.320 | 0.368 | 1 | 0.235 | 0.190 |
| SCI-PANSS | 0.455 | 0.258 | 0.407 | 0.235 | 1 | 0.679 |
| Avolitional items on SCI-PANSS | −0.268 | 0.123 | 0.315 | 0.190 | 0.679 | 1 |
| 2 S-SARS Item n = 60 | 1 Function 1 | 1 Function 2 |
|---|---|---|
| Item 10: Impairment owing to anxiety | 3 0.652 | 0.271 |
| Item 3: Anxiety attacks | 3 0.622 | −0.461 |
| Item 6: Somatic anxiety | 3 0.574 | 0.067 |
| Item 8: Worry and fear | 3 0.457 | 0.331 |
| Item 9: Control-related anxiety | 3 0.349 | 0.268 |
| Item 4: Situational anxiety | 3 0.204 | −0.168 |
| Item 5: Obsessive-compulsive anxiety | 3 0.170 | −0.081 |
| Item 1: Persecutory and nihilistic anxiety | 0.378 | 3 0.532 |
| Item 7: Psychomotor and cognitive agitation | 0.221 | 3 0.495 |
| Item 2: Perceptual anxiety | 0.295 | 3 0.467 |
| n = 60 | SCID Diagnostic Groups | Predicted Group Membership | Total | |||
|---|---|---|---|---|---|---|
| No anxiety | Anxiety disorder not otherwise specified | Specified anxiety disorder | ||||
| 1 Original | Frequency | No anxiety | 17 | 1 | 0 | 18 |
| Anxiety disorder not otherwise specified | 2 | 19 | 1 | 22 | ||
| Specified anxiety disorder | 0 | 3 | 17 | 20 | ||
| % | No anxiety | 94.4 | 5.6 | 0 | 100 | |
| Anxiety disorder not otherwise specified | 9.1 | 86.4 | 4.5 | 100 | ||
| Specified anxiety disorder | 0 | 15 | 85 | 100 | ||
| 2,3 Cross-Validated | Frequency | No anxiety | 15 | 3 | 0 | 18 |
| Anxiety disorder not otherwise specified | 5 | 14 | 3 | 22 | ||
| Specified anxiety disorder | 0 | 4 | 16 | 20 | ||
| % | No anxiety | 83.3 | 16.7 | 0 | 100 | |
| Anxiety disorder not otherwise specified | 22.7 | 63.6 | 13.6 | 100 | ||
| Specified anxiety disorder | 0 | 20.0 | 80.0 | 100 | ||
| Validity Calculation | Percentage |
|---|---|
| Accuracy | 95% |
| Sensitivity | 95.2% |
| Specificity | 94.4% |
| Positive predictive value | 97.6% |
| Negative predictive value | 89.5% |
| Miss rate or false negative rate | 4.8% |
| Fall out or false positive rate | 5.6% |
| False discovery rate | 2.4% |
| False omission rate | 10.5% |
| Measure | S-SARS | VAS | PGIS | BIS | BAS-D | BAS-RS | BAS-FS | ProcS | FAS |
|---|---|---|---|---|---|---|---|---|---|
| S-SARS | 1 | −0.279 | −0.128 | 0.389 | −0.127 | −0.034 | −0.147 | 0.268 | 0.335 |
| VAS | −0.279 | 1 | 0.662 | −0.045 | 0.531 | 0.542 | 0.421 | −0.656 | −0.684 |
| PGIS | −0.128 | 0.662 | 1 | 0.127 | 0.577 | 0.583 | 0.513 | −0.529 | −0.492 |
| BIS | 0.389 | −0.045 | 0.127 | 1 | 0.142 | 0.256 | 0.198 | 0.109 | 0.237 |
| BAS-D | −0.127 | 0.531 | 0.577 | 0.142 | 1 | 0.676 | 0.642 | −0.434 | −0.376 |
| BAS-RS | −0.034 | 0.542 | 0.583 | 0.256 | 0.676 | 1 | 0.678 | −0.426 | −0.389 |
| BAS-FS | −0.147 | 0.421 | 0.513 | 0.198 | 0.642 | 0.678 | 1 | −0.295 | −0.288 |
| ProcS | 0.268 | −0.656 | −0.529 | 0.109 | −0.434 | −0.426 | −0.295 | 1 | 0.618 |
| FAS | 0.335 | −0.684 | −0.492 | 0.237 | −0.376 | −0.389 | −0.288 | 0.618 | 1 |
| Internal Consistency Indicator | Combined Data Sets n = 353 | Data Set No 1 n = 60 | Data Set No 2 n = 51 | Data Set No 3 n = 242 | |
|---|---|---|---|---|---|
| Cronbach’s alpha coefficient | Items 1–10 | 0.931 | 0.875 | 0.875 | 0.891 |
| Split halves | Cronbach α (Items 1–5) | 0.804 | 0.686 | 0.749 | 0.647 |
| Cronbach α (Items 6–10) | 0.917 | 0.849 | 0.792 | 0.885 | |
| Correlation coefficient | 0.882 | 0.772 | 0.815 | 0.837 | |
| Spearman–Brown coefficient | 0.937 | 0.872 | 0.898 | 0.911 | |
| Guttman Split-Half coefficient | 0.928 | 0.864 | 0.897 | 0.874 | |
| Standard error of measurement (SEM) | 2.50 | 3.40 | 3.58 | 1.54 |
| S-SARS Item | 1,2 Single Factor |
|---|---|
| Item 10: Impairment owing to anxiety | 0.893 |
| Item 8: Worry and fear | 0.891 |
| Item 1: Persecutory and nihilistic anxiety | 0.870 |
| Item 9: Control-related anxiety | 0.846 |
| Item 6: Somatic anxiety | 0.812 |
| Item 2: Perceptual anxiety | 0.781 |
| Item 7: Psychomotor and cognitive agitation | 0.732 |
| Item 3: Anxiety attacks | 0.731 |
| Item 4: Situational anxiety | 0.543 |
| Item 5: Obsessive-compulsive anxiety | 0.423 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Van Staden, W.; Dlagnekova, A.; Naidu, K. Validity and Reliability of the Staden Schizophrenia Anxiety Rating Scale. Diagnostics 2022, 12, 831. https://doi.org/10.3390/diagnostics12040831
Van Staden W, Dlagnekova A, Naidu K. Validity and Reliability of the Staden Schizophrenia Anxiety Rating Scale. Diagnostics. 2022; 12(4):831. https://doi.org/10.3390/diagnostics12040831
Chicago/Turabian StyleVan Staden, Werdie, Antonia Dlagnekova, and Kalai Naidu. 2022. "Validity and Reliability of the Staden Schizophrenia Anxiety Rating Scale" Diagnostics 12, no. 4: 831. https://doi.org/10.3390/diagnostics12040831
APA StyleVan Staden, W., Dlagnekova, A., & Naidu, K. (2022). Validity and Reliability of the Staden Schizophrenia Anxiety Rating Scale. Diagnostics, 12(4), 831. https://doi.org/10.3390/diagnostics12040831






