Assessing the Role of Lipopolysaccharide (LPS) Receptor (CD14) in Septic Cardiomyopathy: The Value of Immunohistochemical Diagnostics
Abstract
:1. Introduction
2. Materials and Methods
2.1. Case Selection
2.2. Specimen Preparation and Immunohistochemical Investigation
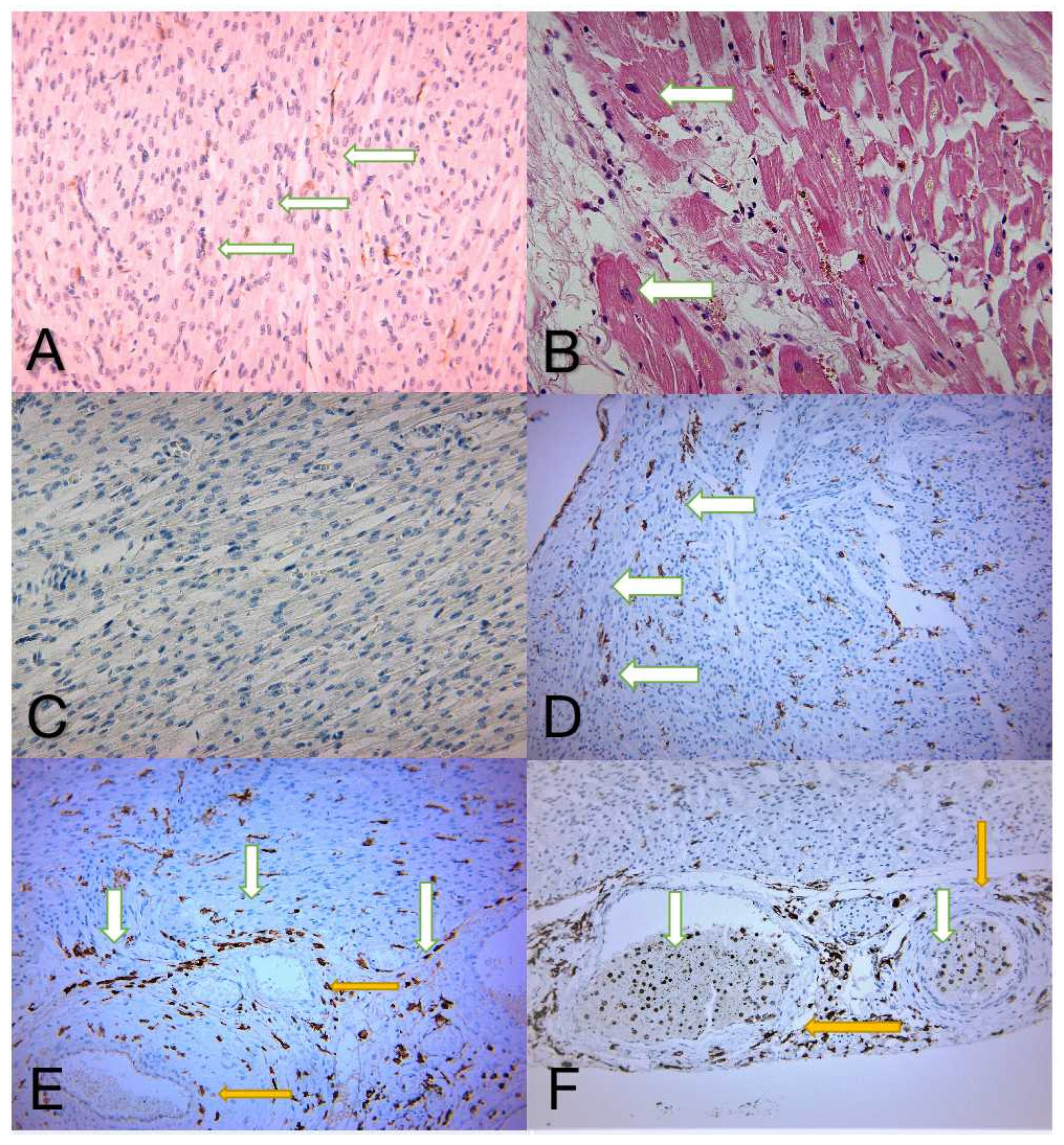
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dantes, R.B.; Epstein, L. Combatting Sepsis: A Public Health Perspective. Clin. Infect. Dis. 2018, 67, 1300–1302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reinhart, K.; Daniels, R.; Kissoon, N.; Machado, F.R.; Schachter, R.D.; Finfer, S. Recognizing Sepsis as a Global Health Priority—A WHO Resolution. N. Engl. J. Med. 2017, 377, 414–417. [Google Scholar] [CrossRef] [PubMed]
- Pusta, C.T.J.; Bungau, S.; Buhas, C.L.; Popa, A.R.; Vesa, C.M.; Buhas, B.A.; Bardaca (Urducea), C.; Tit, D.M.; Abdel-Daim, M.; Judea, A.S. Experimental Study Upon the Virulence of Infectious Microbial Agents Involved in Violent Deaths Presenting Septic States. Rev. Chim. 2019, 70, 2720–2726. [Google Scholar] [CrossRef]
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.-D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef]
- Parker, M.M.; Shelhamer, J.H.; Bacharach, S.L.; Green, M.V.; Natanson, C.; Frederick, T.M.; Damske, B.A.; Parrillo, J.E. Profound but Reversible Myocardial Depression in Patients with Septic Shock. Ann. Intern. Med. 1984, 100, 483–490. [Google Scholar] [CrossRef]
- Reil, P.M.; Maghiar, T.T.; Seidl, K.; Borza, C.; Nunkoo, V.; Buhas, C.L.; Bungau, S.; Stanescu, A.M.A.; Pop, O.L.; Pusta, C.T.J. The role of BCL2 protein and tumour protein p53 in septic cardiomyopathy. Rev. Chim. 2019, 70, 3842–3846. [Google Scholar] [CrossRef]
- Sharkey, S.W.; Shear, W.; Hodges, M.; Herzog, C.A. Reversible Myocardial Contraction Abnormalities in Patients with an Acute Noncardiac Illness. Chest 1998, 114, 98–105. [Google Scholar] [CrossRef]
- Iga, K.; Hori, K.; Kitaguchi, K.; Matsumura, T.; Gen, H.; Tomonaga, G.; Tamamura, T. Transient segmental asynergy of the left ventricle of patients with various clinical manifestations possibly unrelated to the coronary artery disease. Jpn. Circ. J. 1991, 55, 1061–1067. [Google Scholar] [CrossRef]
- Blanco, J.; Muriel-Bombín, A.; Sagredo, V.; Taboada, F.; Gandía, F.; Tamayo, L.; Collado, J.; García-Labattut, Á.; Carriedo, D.; Valledor, M.; et al. Incidence, organ dysfunction and mortality in severe sepsis: A Spanish multicentre study. Crit. Care 2008, 12, R158. [Google Scholar] [CrossRef] [Green Version]
- Beesley, S.J.; Weber, G.; Sarge, T.; Nikravan, S.; Grissom, C.K.; Lanspa, M.J.; Shahul, S.; Brown, S.M. Septic Cardiomyopathy. Crit. Care Med. 2018, 46, 625–634. [Google Scholar] [CrossRef]
- Kirkland, T.N.; Viriyakosol, S. Structure-function analysis of soluble and membrane-bound CD14. Prog. Clin. Biol. Res. 1998, 397, 79–87. [Google Scholar] [PubMed]
- Funda, D.P.; Tučková, L.; Farré, M.A.; Iwase, T.; Moro, I.; Tlaskalová-Hogenová, H. CD14 Is Expressed and Released as Soluble CD14 by Human Intestinal Epithelial Cells In Vitro: Lipopolysaccharide Activation of Epithelial Cells Revisited. Infect. Immun. 2001, 69, 3772–3781, Erratum in Infect. Immun. 2001, 69, 5216. [Google Scholar] [CrossRef] [Green Version]
- Kitchens, R. Role of CD14 in Cellular Recognition of Bacterial Lipopolysaccharides. Chem. Immunol. 2000, 74, 61–82. [Google Scholar] [CrossRef] [PubMed]
- Tapping, R.I.; Tobias, P.S. Soluble CD14-Mediated Cellular Responses to Lipopolysaccharide. Chem. Immunol. 2000, 74, 108–121. [Google Scholar] [CrossRef] [PubMed]
- Ranoa, D.R.; Kelley, S.L.; Tapping, R.I. Human Lipopolysaccharide-binding Protein (LBP) and CD14 Independently Deliver Triacylated Lipoproteins to Toll-like Receptor 1 (TLR1) and TLR2 and Enhance Formation of the Ternary Signaling Complex. J. Biol. Chem. 2013, 288, 9729–9741. [Google Scholar] [CrossRef] [Green Version]
- Takeda, K.; Kaisho, T.; Akira, S. Toll-Like Receptors. Annu. Rev. Immunol. 2003, 21, 335–376. [Google Scholar] [CrossRef]
- Arbour, N.C.; Lorenz, E.; Schutte, B.C.; Zabner, J.; Kline, J.N.; Jones, M.; Frees, K.; Watt, J.L.; Schwartz, D.A. TLR4 mutations are associated with endotoxin hyporesponsiveness in humans. Nat. Genet. 2000, 25, 187–191. [Google Scholar] [CrossRef]
- Baumgarten, G.; Knuefermann, P.; Schuhmacher, G.; Vervölgyi, V.; von Rappard, J.; Dreiner, U.; Fink, K.; Djoufack, C.; Hoeft, A.; Grohé, C.; et al. Toll-Like Receptor 4, Nitric Oxide, and Myocardial Depression in Endotoxemia. Shock 2006, 25, 43–49. [Google Scholar] [CrossRef]
- Knuefermann, P.; Nemoto, S.; Misra, A.; Nozaki, N.; DeFreitas, G.; Goyert, S.M.; Carabello, B.A.; Mann, D.L.; Vallejo, J.G. CD14-deficient mice are protected against lipopolysaccharide-induced cardiac inflammation and left ventricular dysfunction. Circulation 2002, 106, 2608–2615. [Google Scholar] [CrossRef] [Green Version]
- Ferrero, E.; Jiao, D.; Tsuberi, B.Z.; Tesio, L.; Rong, G.W.; Haziot, A.; Goyert, S.M. Transgenic mice expressing human CD14 are hypersensitive to lipopolysaccharide. Proc. Natl. Acad. Sci. USA 1993, 90, 2380–2384. [Google Scholar] [CrossRef] [Green Version]
- Müller-Werdan, U.; Schumann, H.; Loppnow, H.; Fuchs, R.; Darmer, D.; Stadler, J.; Holtz, J.; Werdan, K. Endotoxin and Tumor Necrosis FactorαExert a Similar Proinflammatory Effect in Neonatal Rat Cardiomyocytes, but have Different Cardiodepressant Profiles. J. Mol. Cell. Cardiol. 1998, 30, 1027–1036. [Google Scholar] [CrossRef] [PubMed]
- Comstock, K.L.; Krown, K.A.; Page, M.; Martin, D.; Ho, P.; Pedraza, M.; Castro, E.N.; Nakajima, N.; Glembotski, C.C.; Quintana, P.; et al. LPS-Induced TNF-α Release from and Apoptosis in Rat Cardiomyocytes: Obligatory Role for CD14 in Mediating the LPS Response. J. Mol. Cell. Cardiol. 1998, 30, 2761–2775. [Google Scholar] [CrossRef] [PubMed]
- Klco, J.; Kulkarni, S.; Kreisel, F.H.; Nguyen, T.-D.T.; Hassan, A.; Frater, J.L. Immunohistochemical Analysis of Monocytic Leukemias: Usefulness of CD14 and Krüppel-like Factor 4, a Novel Monocyte Marker. Am. J. Clin. Pathol. 2011, 135, 720–730. [Google Scholar] [CrossRef] [PubMed]
- Wright, S.D.; Ramos, R.A.; Tobias, P.S.; Ulevitch, R.J.; Mathison, J.C. CD14, a receptor for complexes of lipopolysaccharide (LPS) and LPS binding protein. Science 1990, 249, 1431–1433. [Google Scholar] [CrossRef]
- Baldini, M.; Lohman, I.C.; Halonen, M.; Erickson, R.P.; Holt, P.G.; Martinez, F.D. A Polymorphism* in the 5′ Flanking Region of the CD14 Gene Is Associated with Circulating Soluble CD14 Levels and with Total Serum Immunoglobulin E. Am. J. Respir. Cell Mol. Biol. 1999, 20, 976–983. [Google Scholar] [CrossRef]
- Angele, M.K.; Pratschke, S.; Hubbard, W.J.; Chaudry, I.H. Gender differences in sepsis: Cardiovascular and immunological aspects. Virulence 2014, 5, 12–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mehedintu, C.; Bratila, E.; Brinduse, L.A.; Cirstoiu, M.M.; Berceanu, C.; Bordea, A.; Comandasu, D.-E.; Veliscu, A.C.; Bratu, O.; Sava, C.; et al. Controled Ovarian Stimulation with Urinary Gonadotrophins and Recombinant Gonadotrophins in Current Practice. Rev. Chim. 2019, 69, 3611–3615. [Google Scholar] [CrossRef]
- Backhed, F.; Meijer, L.; Normark, S.; Richter-Dahlfors, A. TLR4-dependent recognition of lipopolysaccharide by epithelial cells requires sCD14. Cell. Microbiol. 2002, 4, 493–501. [Google Scholar] [CrossRef]
- Ulevitch, R.J.; Tobias, P.S. Receptor-Dependent Mechanisms of Cell Stimulation by Bacterial Endotoxin. Annu. Rev. Immunol. 1995, 13, 437–457. [Google Scholar] [CrossRef]
- Pugin, J.; Schürer-Maly, C.C.; Leturcq, D.; Moriarty, A.; Ulevitch, R.J.; Tobias, P.S. Lipopolysaccharide activation of human endothelial and epithelial cells is mediated by lipopolysaccharide-binding protein and soluble CD14. Proc. Natl. Acad. Sci. USA 1993, 90, 2744–2748. [Google Scholar] [CrossRef] [Green Version]
- Poltorak, A.; He, X.; Smirnova, I.; Liu, M.-Y.; Van Huffel, C.; Du, X.; Birdwell, D.; Alejos, E.; Silva, M.; Galanos, C.; et al. Defective LPS Signaling in C3H/HeJ and C57BL/10ScCr Mice: Mutations in Tlr4 Gene. Science 1998, 282, 2085–2088. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akashi, S.; Saitoh, S.-I.; Wakabayashi, Y.; Kikuchi, T.; Takamura, N.; Nagai, Y.; Kusumoto, Y.; Fukase, K.; Kusumoto, S.; Adachi, Y.; et al. Lipopolysaccharide Interaction with Cell Surface Toll-like Receptor 4-MD-2: Higher affinity than that with MD-2 or CD14. J. Exp. Med. 2003, 198, 1035–1042. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grunwald, U.; Fan, X.; Jack, R.S.; Workalemahu, G.; Kallies, A.; Stelter, F.; Schütt, C. Monocytes can phagocytose Gram-negative bacteria by a CD14-dependent mechanism. J. Immunol. 1996, 157, 8892647. [Google Scholar]
- Medzhitov, R.; Janeway, C.A., Jr. Innate Immunity: The Virtues of a Nonclonal System of Recognition. Cell 1997, 91, 295–298. [Google Scholar] [CrossRef] [Green Version]
- Tennant, I.; Pound, J.; Marr, L.; Willems, J.J.L.P.; Petrova, S.; Ford, C.A.; Paterson, M.; Devitt, A.; Gregory, C.D. Innate recognition of apoptotic cells: Novel apoptotic cell-associated molecular patterns revealed by crossreactivity of anti-LPS antibodies. Cell Death Differ. 2013, 20, 698–708. [Google Scholar] [CrossRef] [Green Version]
- Reil, P.M.; Maghiar, T.T.; Seidl, K.; Borza, C.; Nunkoo, V.; Pascalau, A.; Pop, O.L. The Role of P53 In Sepsis-Induced Cardiomyopathy. Acta Med. Transilv. 2021, 26, 45–47. [Google Scholar] [CrossRef]
- Devitt, A.; Marshall, L.J. The innate immune system and the clearance of apoptotic cells. J. Leukoc. Biol. 2011, 90, 447–457. [Google Scholar] [CrossRef]
- Diaconu, C.; Balaceanu, A.; Morosan, E. Sepsis biomarkers: Past, present and future. Farmacia 2015, 63, 811–815. [Google Scholar]
- Pinto, B.B.; Ripoll, V.R.; Subías-Beltrán, P.; Herpain, A.; Barlassina, C.; Oliveira, E.; Pastorelli, R.; Braga, D.; Barcella, M.; Subirats, L.; et al. Application of an Exploratory Knowledge-Discovery Pipeline Based on Machine Learning to Multi-Scale OMICS Data to Characterise Myocardial Injury in a Cohort of Patients with Septic Shock: An Observational Study. J. Clin. Med. 2021, 10, 4354. [Google Scholar] [CrossRef]
- Muresan, M.; Micle, O.; Antal, L.; Dobjanschi, L.; Antonescu, A.; Vicas, L.; Bodog, F.; Dorofteiu, M. Correlation between reactive oxygen species and homocysteine levels in normal pregnancy. Farmacia 2011, 59, 179–190. [Google Scholar]
- Crăiniceanu, Z.; Olariu, S.; Bloancă, V.; Farca, I.; Bodog, F.; Matusz, P.; Bratu, T. Continuous negative pressure wound therapy in the treatment of a gigantic trophic leg ulcer. Chirurgia 2013, 108, 112–115. [Google Scholar] [PubMed]
- Paşcalău, A.V.; Cheregi, C.D.; Mureşan, M.Ş.; Şandor, M.I.; Huniadi, C.A.; Nikin, Z.; Pusta, C.T.J.; Bodog, F.D.; Ionescu, C.; Pop, O.L. CD4+ CD25+ regulatory T-cells role in tumor microenvironment of the squamous cell carcinoma. Rom. J. Morphol. Embryol. 2021, 62, 249–253. [Google Scholar] [CrossRef] [PubMed]
| Infection Site | No. of Patients | Percentage |
|---|---|---|
| Abdominal | 3 | 10.3% |
| CNS | 2 | 6.9% |
| Hematogenous | 2 | 6.9% |
| Pulmonary | 16 | 55.2% |
| Unknown | 2 | 6.9% |
| Urinary | 4 | 13.8% |
| Total | 29 | 100.0% |
| Characteristics | Study Group | Control Group | p-Value |
|---|---|---|---|
| Age (mean value) | 0.3 years (±16.5) | 4.2 months (±2.6) | |
| Gender F:M | 18:11 cases | - | 0.2652 |
| Urban/Rural | 16:13 cases | - | 0.7103 |
| Infection site origins | Lung Urinary tract | - | 0.0001 |
| Group | CD14 Expression Rate | |
|---|---|---|
| <10% | >10% | |
| Control (n = 10) | 10 | 0 |
| Study (n = 29) | 10 | 19 |
| CD14 Expression Rate | ||
|---|---|---|
| <10% | >10% | |
| Age, years (±SD) | 53.70 (±20.8) | 63.73 (±12.9) |
| Intravascular CD14 | Cellular CD14 Expression Rate | |
|---|---|---|
| <10% | >10% | |
| Increased | 2 | 15 |
| Decreased | 8 | 4 |
| Gender | Intravascular CD14 | |
|---|---|---|
| Decreased | Increased | |
| Female | 6 | 12 |
| Male | 6 | 5 |
| Intravascular CD14 | ||
|---|---|---|
| Decreased | Increased | |
| Age, years (±SD) | 57.75 (±15.5) | 62.05 (±17.4) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reil, P.M.; Maghiar, T.T.; Vîlceanu, N.; Pascalau, A.; Judea Pusta, C.T.; Marcu, F.; Cavalu, S.; Pop, O. Assessing the Role of Lipopolysaccharide (LPS) Receptor (CD14) in Septic Cardiomyopathy: The Value of Immunohistochemical Diagnostics. Diagnostics 2022, 12, 781. https://doi.org/10.3390/diagnostics12040781
Reil PM, Maghiar TT, Vîlceanu N, Pascalau A, Judea Pusta CT, Marcu F, Cavalu S, Pop O. Assessing the Role of Lipopolysaccharide (LPS) Receptor (CD14) in Septic Cardiomyopathy: The Value of Immunohistochemical Diagnostics. Diagnostics. 2022; 12(4):781. https://doi.org/10.3390/diagnostics12040781
Chicago/Turabian StyleReil, Peter Michael, Teodor Traian Maghiar, Narcis Vîlceanu, Andrei Pascalau, Claudia Teodora Judea Pusta, Florin Marcu, Simona Cavalu, and Ovidiu Pop. 2022. "Assessing the Role of Lipopolysaccharide (LPS) Receptor (CD14) in Septic Cardiomyopathy: The Value of Immunohistochemical Diagnostics" Diagnostics 12, no. 4: 781. https://doi.org/10.3390/diagnostics12040781
APA StyleReil, P. M., Maghiar, T. T., Vîlceanu, N., Pascalau, A., Judea Pusta, C. T., Marcu, F., Cavalu, S., & Pop, O. (2022). Assessing the Role of Lipopolysaccharide (LPS) Receptor (CD14) in Septic Cardiomyopathy: The Value of Immunohistochemical Diagnostics. Diagnostics, 12(4), 781. https://doi.org/10.3390/diagnostics12040781







