One-Day Prostate Cancer Diagnosis: Biparametric Magnetic Resonance Imaging and Digital Pathology by Fluorescence Confocal Microscopy
Abstract
:1. Introduction
2. Materials and Methods
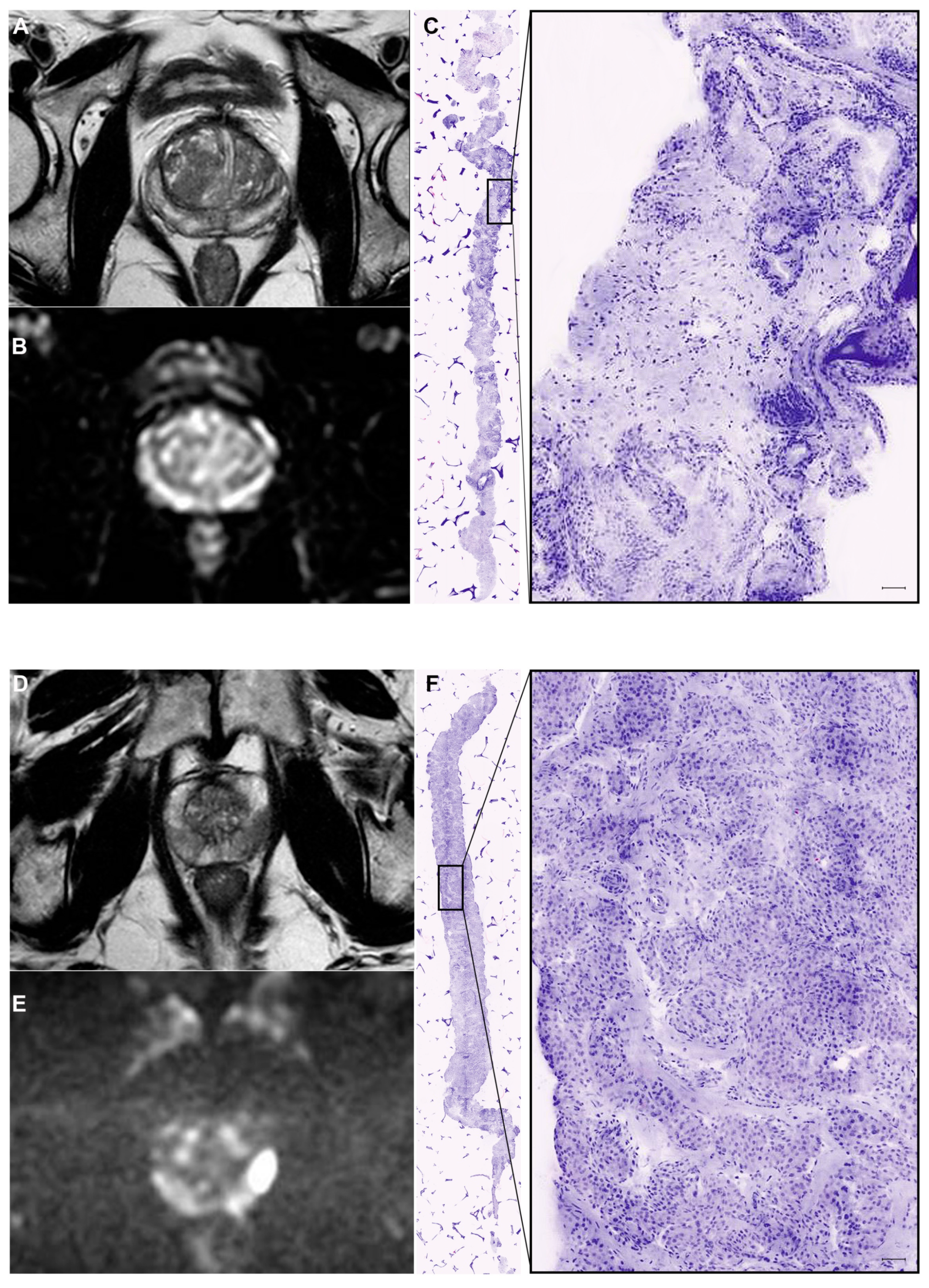
2.1. Biparametric MRI
2.2. Prostate Biopsy
2.3. Pathology
2.4. Pre-Discharge Clinical Assessment
2.5. Patients’ Satisfaction Questionnaire
2.6. Study Outcomes and Statistical Analysis
3. Results
3.1. Per-Patient Analysis
3.2. Per-Core Analysis
3.3. Patient Satisfaction Questionnaire
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Welch, H.G.; Albertsen, P.C. Reconsidering Prostate Cancer Mortality—The Future of PSA Screening. N. Engl. J. Med. 2020, 382, 1557–1563. [Google Scholar] [CrossRef] [PubMed]
- US Preventive Services Task Force; Grossman, D.C.; Curry, S.J.; Owens, D.K.; Bibbins-Domingo, K.; Caughey, A.B.; Davidson, K.W.; Doubeni, C.A.; Ebell, M.; Epling, J.W., Jr.; et al. Screening for Prostate Cancer: US Preventive Services Task Force Recommendation Statement. JAMA 2018, 319, 1901–1913. [Google Scholar] [CrossRef]
- Shoag, J.E.; Nyame, Y.A.; Gulati, R.; Etzioni, R.; Hu, J.C. Reconsidering the Trade-offs of Prostate Cancer Screening. N. Engl. J. Med. 2020, 382, 2465–2468. [Google Scholar] [CrossRef]
- Vickers, A.J.; Eastham, J.A.; Scardino, P.T.; Lilja, H. The Memorial Sloan Kettering Cancer Center Recommendations for Prostate Cancer Screening. Urology 2016, 91, 12–18. [Google Scholar] [CrossRef] [Green Version]
- Mottet, N.; van den Bergh, R.C.N.; Briers, E.; Cornford, P.; De Santis, M.; Fanti, S.; Gillessen, S.; Grummet, J.; Henry, A.M.; Lam, T.B.; et al. EAU-ESTRO-ESUR-SIOG Guidelines on Prostate Cancer 2020. In European Association of Urology Guidelines, 2020th ed.; European Association of Urology Guidelines Office: Arnhem, The Netherlands, 2020; Volume Presented at the EAU Annual Congress Amsterdam 2020. [Google Scholar]
- Falagario, U.G.; Busetto, G.M.; Netti, G.S.; Sanguedolce, F.; Selvaggio, O.; Infante, B.; Ranieri, E.; Stallone, G.; Carrieri, G.; Cormio, L. Prospective Validation of Pentraxin-3 as a Novel Serum Biomarker to Predict the Risk of Prostate Cancer in Patients Scheduled for Prostate Biopsy. Cancers 2021, 13, 1611. [Google Scholar] [CrossRef] [PubMed]
- Hamzeh, O.; Alkhateeb, A.; Zheng, J.Z.; Kandalam, S.; Leung, C.; Atikukke, G.; Cavallo-Medved, D.; Palanisamy, N.; Rueda, L. A Hierarchical Machine Learning Model to Discover Gleason Grade-Specific Biomarkers in Prostate Cancer. Diagnostics 2019, 9, 219. [Google Scholar] [CrossRef] [Green Version]
- Alkhateeb, A.; Rezaeian, I.; Singireddy, S.; Cavallo-Medved, D.; Porter, L.A.; Rueda, L. Transcriptomics Signature from Next-Generation Sequencing Data Reveals New Transcriptomic Biomarkers Related to Prostate Cancer. Cancer Inform. 2019, 18, 1176935119835522. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ankerst, D.P.; Straubinger, J.; Selig, K.; Guerrios, L.; De Hoedt, A.; Hernandez, J.; Liss, M.A.; Leach, R.J.; Freedland, S.J.; Kattan, M.W.; et al. A Contemporary Prostate Biopsy Risk Calculator Based on Multiple Heterogeneous Cohorts. Eur. Urol. 2018, 74, 197–203. [Google Scholar] [CrossRef]
- Falagario, U.G.; Jambor, I.; Lantz, A.; Ettala, O.; Stabile, A.; Taimen, P.; Aronen, H.J.; Knaapila, J.; Perez, I.M.; Gandaglia, G.; et al. Combined Use of Prostate-specific Antigen Density and Magnetic Resonance Imaging for Prostate Biopsy Decision Planning: A Retrospective Multi-institutional Study Using the Prostate Magnetic Resonance Imaging Outcome Database (PROMOD). Eur. Urol. Oncol. 2020, 4, 971–979. [Google Scholar] [CrossRef]
- Kasivisvanathan, V.; Rannikko, A.S.; Borghi, M.; Panebianco, V.; Mynderse, L.A.; Vaarala, M.H.; Briganti, A.; Budaus, L.; Hellawell, G.; Hindley, R.G.; et al. MRI-Targeted or Standard Biopsy for Prostate-Cancer Diagnosis. N. Engl. J. Med. 2018, 378, 1767–1777. [Google Scholar] [CrossRef]
- Ahdoot, M.; Wilbur, A.R.; Reese, S.E.; Lebastchi, A.H.; Mehralivand, S.; Gomella, P.T.; Bloom, J.; Gurram, S.; Siddiqui, M.; Pinsky, P.; et al. MRI-Targeted, Systematic, and Combined Biopsy for Prostate Cancer Diagnosis. N. Engl. J. Med. 2020, 382, 917–928. [Google Scholar] [CrossRef]
- Lazzeri, G.; Troiano, G.; Porchia, B.R.; Centauri, F.; Mezzatesta, V.; Presicce, G.; Matarrese, D.; Gusinu, R. Waiting times for prostate cancer: A review. J. Public Health Res. 2020, 9, 1778. [Google Scholar] [CrossRef] [PubMed]
- van der Leest, M.; Israel, B.; Cornel, E.B.; Zamecnik, P.; Schoots, I.G.; van der Lelij, H.; Padhani, A.R.; Rovers, M.; van Oort, I.; Sedelaar, M.; et al. High Diagnostic Performance of Short Magnetic Resonance Imaging Protocols for Prostate Cancer Detection in Biopsy-naive Men: The Next Step in Magnetic Resonance Imaging Accessibility. Eur. Urol. 2019, 76, 574–581. [Google Scholar] [CrossRef] [PubMed]
- Perez, I.M.; Jambor, I.; Kauko, T.; Verho, J.; Ettala, O.; Falagario, U.; Merisaari, H.; Kiviniemi, A.; Taimen, P.; Syvanen, K.T.; et al. Qualitative and Quantitative Reporting of a Unique Biparametric MRI: Towards Biparametric MRI-Based Nomograms for Prediction of Prostate Biopsy Outcome in Men With a Clinical Suspicion of Prostate Cancer (IMPROD and MULTI-IMPROD Trials). J. Magn. Reson. Imaging 2019, 51, 1556–1567. [Google Scholar] [CrossRef]
- Jambor, I.; Bostrom, P.J.; Taimen, P.; Syvanen, K.; Kahkonen, E.; Kallajoki, M.; Perez, I.M.; Kauko, T.; Matomaki, J.; Ettala, O.; et al. Novel biparametric MRI and targeted biopsy improves risk stratification in men with a clinical suspicion of prostate cancer (IMPROD Trial). J. Magn. Reson. Imaging 2017, 46, 1089–1095. [Google Scholar] [CrossRef]
- Rocco, B.; Sighinolfi, M.C.; Sandri, M.; Spandri, V.; Cimadamore, A.; Volavsek, M.; Mazzucchelli, R.; Lopez-Beltran, A.; Eissa, A.; Bertoni, L.; et al. Digital Biopsy with Fluorescence Confocal Microscope for Effective Real-time Diagnosis of Prostate Cancer: A Prospective, Comparative Study. Eur. Urol. Oncol. 2020, 4, 784–791. [Google Scholar] [CrossRef]
- Cormio, L.; Lucarelli, G.; Selvaggio, O.; Di Fino, G.; Mancini, V.; Massenio, P.; Troiano, F.; Sanguedolce, F.; Bufo, P.; Carrieri, G. Absence of Bladder Outlet Obstruction Is an Independent Risk Factor for Prostate Cancer in Men Undergoing Prostate Biopsy. Medicine 2016, 95, e2551. [Google Scholar] [CrossRef] [PubMed]
- Cormio, L.; Lucarelli, G.; Netti, G.S.; Stallone, G.; Selvaggio, O.; Troiano, F.; Di Fino, G.; Sanguedolce, F.; Bufo, P.; Grandaliano, G.; et al. Post-void residual urinary volume is an independent predictor of biopsy results in men at risk for prostate cancer. Anticancer Res. 2015, 35, 2175–2182. [Google Scholar]
- Cormio, L.; Cindolo, L.; Troiano, F.; Marchioni, M.; Di Fino, G.; Mancini, V.; Falagario, U.; Selvaggio, O.; Sanguedolce, F.; Fortunato, F.; et al. Development and Internal Validation of Novel Nomograms Based on Benign Prostatic Obstruction-Related Parameters to Predict the Risk of Prostate Cancer at First Prostate Biopsy. Front. Oncol. 2018, 8, 438. [Google Scholar] [CrossRef] [PubMed]
- Cormio, L.; Pagliarulo, V.; Lorusso, F.; Selvaggio, O.; Perrone, A.; Sanguedolce, F.; Bufo, P.; Carrieri, G. Combined perianal-intrarectal (PI) lidocaine-prilocaine (LP) cream and lidocaine-ketorolac gel provide better pain relief than combined PI LP cream and periprostatic nerve block during transrectal prostate biopsy. BJU Int. 2012, 109, 1776–1780. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cormio, L.; Scattoni, V.; Lorusso, F.; Perrone, A.; Di Fino, G.; Selvaggio, O.; Sanguedolce, F.; Bufo, P.; Montorsi, F.; Carrieri, G. Prostate cancer detection rates in different biopsy schemes. Which cores for which patients? World J. Urol. 2014, 32, 341–346. [Google Scholar] [CrossRef] [PubMed]
- van Leenders, G.; van der Kwast, T.H.; Grignon, D.J.; Evans, A.J.; Kristiansen, G.; Kweldam, C.F.; Litjens, G.; McKenney, J.K.; Melamed, J.; Mottet, N.; et al. The 2019 International Society of Urological Pathology (ISUP) Consensus Conference on Grading of Prostatic Carcinoma. Am. J. Surg. Pathol. 2020, 44, e87–e99. [Google Scholar] [CrossRef] [PubMed]
- Bass, E.J.; Freeman, A.; Jameson, C.; Punwani, S.; Moore, C.M.; Arya, M.; Emberton, M.; Ahmed, H.U. Prostate cancer diagnostic pathway: Is a one-stop cognitive MRI targeted biopsy service a realistic goal in everyday practice? A pilot cohort in a tertiary referral centre in the UK. BMJ Open 2018, 8, e024941. [Google Scholar] [CrossRef] [Green Version]
- Bass, E.J.; Pantovic, A.; Connor, M.; Gabe, R.; Padhani, A.R.; Rockall, A.; Sokhi, H.; Tam, H.; Winkler, M.; Ahmed, H.U. A systematic review and meta-analysis of the diagnostic accuracy of biparametric prostate MRI for prostate cancer in men at risk. Prostate Cancer Prostatic Dis. 2020, 24, 596–611. [Google Scholar] [CrossRef] [PubMed]
- Jambor, I.; Kahkonen, E.; Taimen, P.; Merisaari, H.; Saunavaara, J.; Alanen, K.; Obsitnik, B.; Minn, H.; Lehotska, V.; Aronen, H.J. Prebiopsy multiparametric 3T prostate MRI in patients with elevated PSA, normal digital rectal examination, and no previous biopsy. J. Magn. Reson. Imaging 2015, 41, 1394–1404. [Google Scholar] [CrossRef]
- Russo, F.; Mazzetti, S.; Regge, D.; Ambrosini, I.; Giannini, V.; Manfredi, M.; De Luca, S.; Bollito, E.; Porpiglia, F. Diagnostic Accuracy of Single-plane Biparametric and Multiparametric Magnetic Resonance Imaging in Prostate Cancer: A Randomized Noninferiority Trial in Biopsy-naive Men. Eur. Urol. Oncol. 2021, 4, 855–862. [Google Scholar] [CrossRef] [PubMed]
- Eldred-Evans, D.; Burak, P.; Connor, M.J.; Day, E.; Evans, M.; Fiorentino, F.; Gammon, M.; Hosking-Jervis, F.; Klimowska-Nassar, N.; McGuire, W.; et al. Population-Based Prostate Cancer Screening With Magnetic Resonance Imaging or Ultrasonography: The IP1-PROSTAGRAM Study. JAMA Oncol. 2021, 7, 395–402. [Google Scholar] [CrossRef] [PubMed]
- Selvaggio, O.; Falagario, U.G.; Bruno, S.M.; Recchia, M.; Sighinolfi, M.C.; Sanguedolce, F.; Milillo, P.; Macarini, L.; Rastinehad, A.R.; Sanchez-Salas, R.; et al. Intraoperative Digital Analysis of Ablation Margins (DAAM) by Fluorescent Confocal Microscopy to Improve Partial Prostate Gland Cryoablation Outcomes. Cancers 2021, 13, 4382. [Google Scholar] [CrossRef] [PubMed]
- Marenco, J.; Calatrava, A.; Casanova, J.; Claps, F.; Mascaros, J.; Wong, A.; Barrios, M.; Martin, I.; Rubio, J. Evaluation of Fluorescent Confocal Microscopy for Intraoperative Analysis of Prostate Biopsy Cores. Eur. Urol. Focus 2020, 7, 1254–1259. [Google Scholar] [CrossRef]

| Digital FCM | Standard HE | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pt. | Age | PSA | Q-Max | DRE | P-Vol | PI-RADS | Bx GG | Pos. Cores | Bx GG | Pos. Cores |
| 1 | 50 | 3.71 | 32 | Neg. | 50 | N/A | 0 | 0 | 0 | 0 |
| 2 | 57 | 4.49 | 11 | Neg | 60 | 4 | 0 | 0 | 0 | 0 |
| 3 | 69 | 4.49 | 21 | Susp | 24 | 3 | 0 | 0 | 0 | 0 |
| 4 | 59 | 12 | 11 | Susp | 40 | 5 | 4 | 9 | 4 | 10 |
| 5 | 66 | 5.14 | 16 | Neg | 37 | 4 | 3 | 8 | 3 | 6 |
| 6 | 65 | 7.6 | 12 | Susp | 54 | 4 | 2 | 12 | 2 | 11 |
| 7 | 71 | 4.34 | 8 | Susp | 68 | 5 | 4 | 17 | 5 | 17 |
| 8 | 62 | 7.36 | 20 | Neg | 98 | 3 | 0 | 0 | 0 | 0 |
| 9 | 57 | 8.55 | 9 | Neg | 98 | 2 | 0 | 0 | 0 | 0 |
| 10 | 53 | 8.77 | 24 | Susp | 77 | 2 | 0 | 0 | 0 | 0 |
| 11 | 66 | 4.96 | 15 | Susp | 64 | 2 | 1 | 7 | 1 | 8 |
| 12 | 57 | 4.81 | 7 | Susp | 66 | 2 | 0 | 0 | 0 | 0 |
| Standard of Care (HE Staining) | |||||||
|---|---|---|---|---|---|---|---|
| Vivascope | Negative | 1 | 2 | 3 | 4 | 5 | Total |
| Negative | 128 | 2 | 0 | 2 | 1 | 0 | 133 |
| 1 | 2 | 9 | 1 | 0 | 1 | 0 | 13 |
| 2 | 0 | 0 | 2 | 3 | 0 | 0 | 5 |
| 3 | 0 | 0 | 1 | 7 | 2 | 0 | 10 |
| 4 | 0 | 0 | 0 | 0 | 20 | 2 | 22 |
| 5 | 0 | 0 | 0 | 0 | 0 | 2 | 2 |
| Total | 130 | 11 | 4 | 12 | 24 | 4 | 185 |
| Agreement | 95% CI | Cohen K | 95% CI | ||||
| Any PCa | 0.962 | (0.934, 0.990) | 0.908 | (0.841, 0.975) | |||
| CsPCa | 0.973 | (0.949, 0.997) | 0.922 | (0.855, 0.990) | |||
| Bx GG | 0.908 | (0.866, 0.950) | 0.805 | (0.722, 0.887) | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Falagario, U.G.; Selvaggio, O.; Sanguedolce, F.; Milillo, P.; Sighinolfi, M.C.; Bruno, S.M.; Recchia, M.; Bettocchi, C.; Busetto, G.M.; Macarini, L.; et al. One-Day Prostate Cancer Diagnosis: Biparametric Magnetic Resonance Imaging and Digital Pathology by Fluorescence Confocal Microscopy. Diagnostics 2022, 12, 277. https://doi.org/10.3390/diagnostics12020277
Falagario UG, Selvaggio O, Sanguedolce F, Milillo P, Sighinolfi MC, Bruno SM, Recchia M, Bettocchi C, Busetto GM, Macarini L, et al. One-Day Prostate Cancer Diagnosis: Biparametric Magnetic Resonance Imaging and Digital Pathology by Fluorescence Confocal Microscopy. Diagnostics. 2022; 12(2):277. https://doi.org/10.3390/diagnostics12020277
Chicago/Turabian StyleFalagario, Ugo Giovanni, Oscar Selvaggio, Francesca Sanguedolce, Paola Milillo, Maria Chiara Sighinolfi, Salvatore Mariano Bruno, Marco Recchia, Carlo Bettocchi, Gian Maria Busetto, Luca Macarini, and et al. 2022. "One-Day Prostate Cancer Diagnosis: Biparametric Magnetic Resonance Imaging and Digital Pathology by Fluorescence Confocal Microscopy" Diagnostics 12, no. 2: 277. https://doi.org/10.3390/diagnostics12020277
APA StyleFalagario, U. G., Selvaggio, O., Sanguedolce, F., Milillo, P., Sighinolfi, M. C., Bruno, S. M., Recchia, M., Bettocchi, C., Busetto, G. M., Macarini, L., Rocco, B., Cormio, L., & Carrieri, G. (2022). One-Day Prostate Cancer Diagnosis: Biparametric Magnetic Resonance Imaging and Digital Pathology by Fluorescence Confocal Microscopy. Diagnostics, 12(2), 277. https://doi.org/10.3390/diagnostics12020277








