Evaluating the Feasibility of Machine-Learning-Based Predictive Models for Precancerous Cervical Lesions in Patients Referred for Colposcopy
Abstract
1. Introduction
2. Materials and Methods
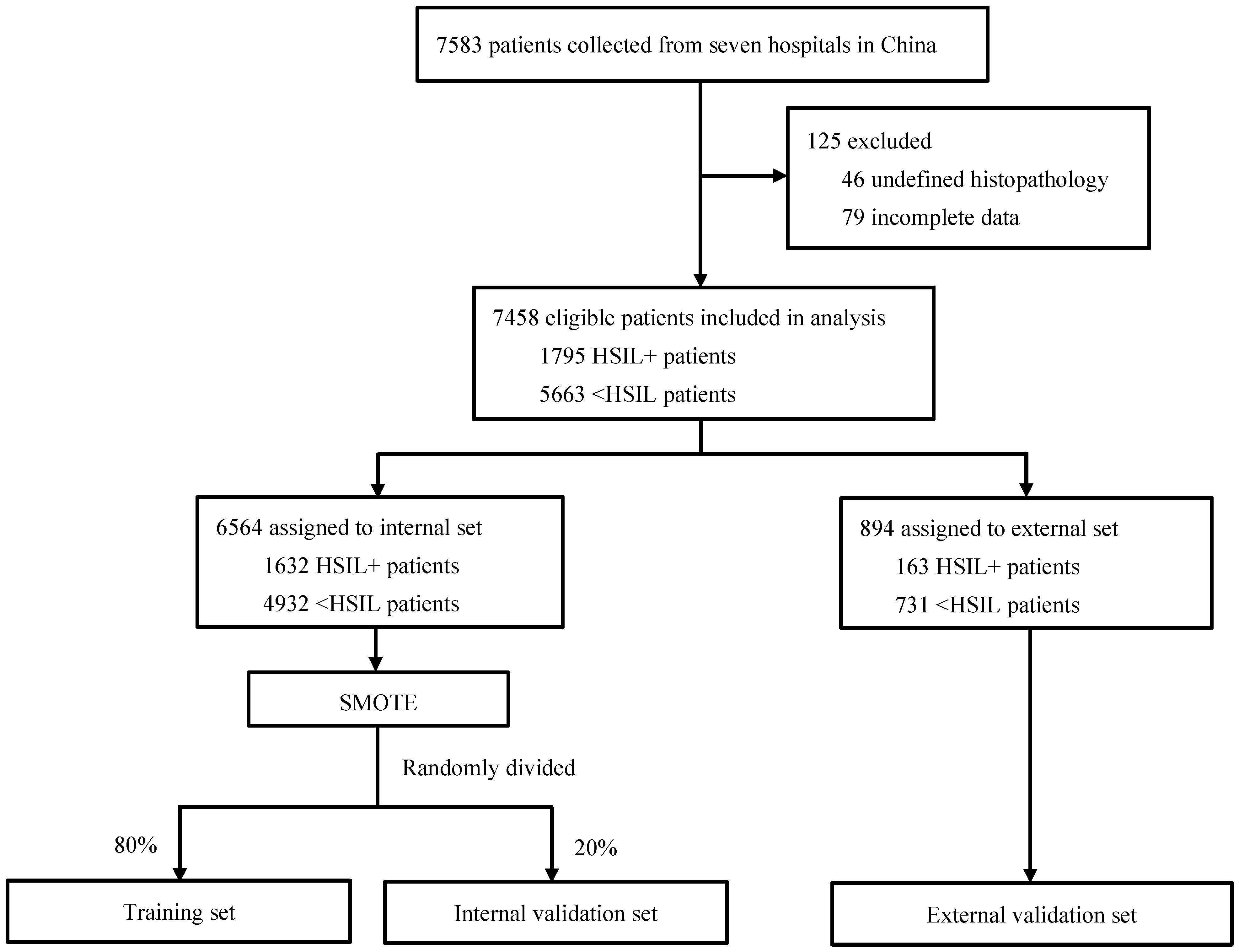
2.1. Study Design and Population
2.2. Screening Tests, Colposcopy, and Histology Diagnosis
2.3. Development and Validation of ML Models
2.4. Statistical Analysis
3. Results
3.1. Characteristics of Study Population
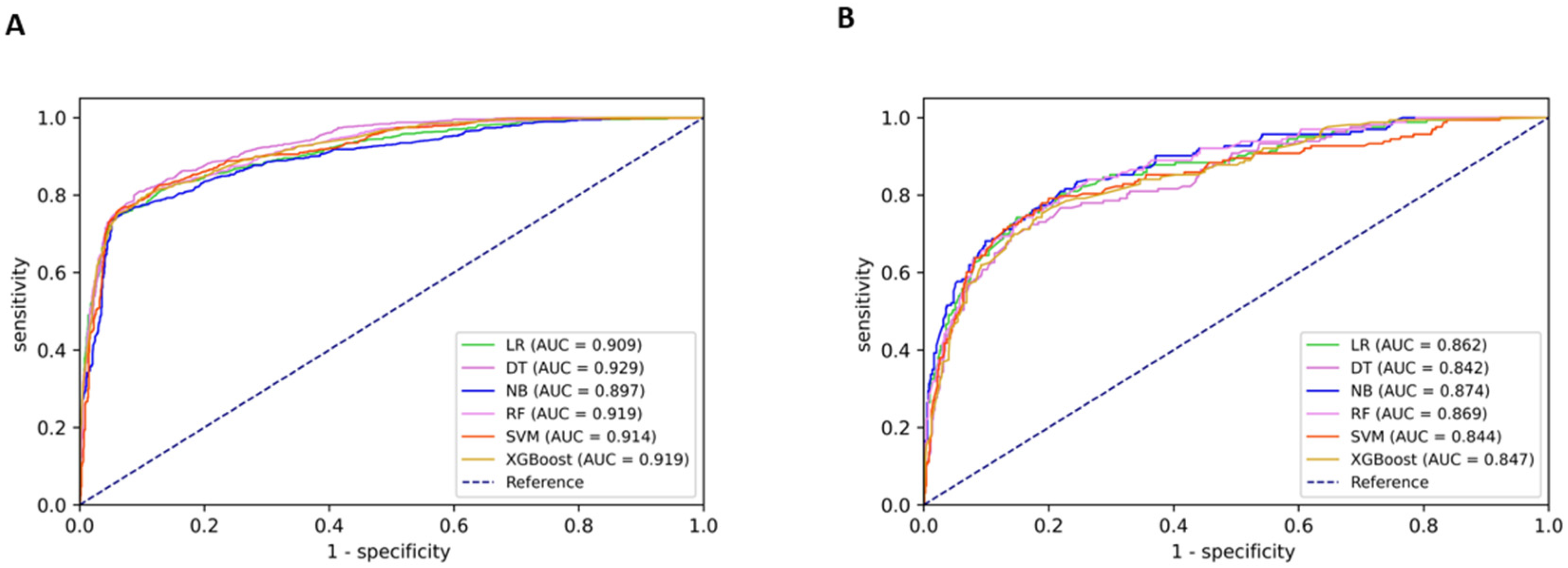
3.2. Model Performance and Variable Ranking
3.3. Subgroup Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Strategy to Accelerate the Elimination of Cervical Cancer as a Public Health Problem. Available online: https://www.who.int/publications/i/item/9789240014107 (accessed on 17 November 2020).
- Petousis, S.; Christidis, P.; Margioula-Siarkou, C.; Sparangis, N.; Athanasiadis, A.; Kalogiannidis, I. Discrepancy between colposcopy, punch biopsy and final histology of cone specimen: A prospective study. Arch. Gynecol. Obstet. 2018, 297, 1271–1275. [Google Scholar] [CrossRef] [PubMed]
- Tatiyachonwiphut, M.; Jaishuen, A.; Sangkarat, S.; Laiwejpithaya, S.; Wongtiraporn, W.; Inthasorn, P.; Viriyapak, B.; Warnnissorn, M. Agreement between Colposcopic Diagnosis and Cervical Pathology: Siriraj Hospital Experience. Asian Pac. J. Cancer Prev. 2014, 15, 423–426. [Google Scholar] [CrossRef] [PubMed]
- Benedet, J.L.; Matisic, J.P.; Bertrand, M.A. An analysis of 84244 patients from the British Columbia cytology-colposcopy program. Gynecol. Oncol. 2004, 92, 127–134. [Google Scholar] [CrossRef]
- Fan, A.; Wang, C.; Zhang, L.; Yan, Y.; Han, C.; Xue, F. Diagnostic value of the 2011 International Federation for Cervical Pathology and Colposcopy Terminology in predicting cervical lesions. Oncotarget 2018, 9, 9166–9176. [Google Scholar] [CrossRef]
- Wentzensen, N.; Schiffman, M.; Silver, M.I.; Khan, M.J.; Perkins, R.B.; Smith, K.M.; Gage, J.C.; Gold, M.A.; Conageski, C.; Einstein, M.H.; et al. ASCCP Colposcopy Standards: Risk-Based Colposcopy Practice. J. Low. Genit. Tract Dis. 2017, 21, 230–234. [Google Scholar] [CrossRef]
- Perkins, R.B.; Guido, R.S.; Castle, P.E.; Chelmow, D.; Einstein, M.H.; Garcia, F.; Huh, W.K.; Kim, J.J.; Moscicki, A.B.; Nayar, R.; et al. 2019 ASCCP Risk-Based Management Consensus Guidelines for Abnormal Cervical Cancer Screening Tests and Cancer Precursors. J. Low Genit. Tract. Dis. 2020, 24, 102–131. [Google Scholar] [CrossRef]
- Xue, P.; Seery, S.; Li, Q.; Jiang, Y.; Qiao, Y. Risk-Based Colposcopy for Cervical Precancer Detection: A Cross-Sectional Multicenter Study in China. Diagnostics 2022, 12, 2585. [Google Scholar] [CrossRef]
- Handelman, G.S.; Kok, H.K.; Chandra, R.V.; Razavi, A.H.; Lee, M.J.; Asadi, H. eDoctor: Machine learning and the future of medicine. J. Intern. Med. 2018, 284, 603–619. [Google Scholar] [CrossRef]
- Rajkomar, A.; Dean, J.; Kohane, I. Machine Learning in Medicine. N. Engl. J. Med. 2019, 380, 1347–1358. [Google Scholar] [CrossRef]
- Chen, M.; Zhang, B.; Cai, Z.; Seery, S.; Gonzalez, M.J.; Ali, N.M.; Ren, R.; Qiao, Y.; Xue, P.; Jiang, Y. Acceptance of clinical artificial intelligence among physicians and medical students: A systematic review with cross-sectional survey. Front. Med. 2022, 9, 990604. [Google Scholar] [CrossRef] [PubMed]
- Xue, P.; Wang, J.; Qin, D.; Yan, H.; Qu, Y.; Seery, S.; Jiang, Y.; Qiao, Y. Deep learning in image-based breast and cervical cancer detection: A systematic review and meta-analysis. npj Digit. Med. 2022, 5, 19. [Google Scholar] [CrossRef] [PubMed]
- Kahng, J.; Kim, E.-H.; Kim, H.-G.; Lee, W. Development of a cervical cancer progress prediction tool for human papillomavirus-positive Koreans: A support vector machine-based approach. J. Int. Med. Res. 2015, 43, 518–525. [Google Scholar] [CrossRef]
- Scheurer, M.E.; Guillaud, M.; Tortolero-Luna, G.; Follen, M.; Adler-Storthz, K. Epidemiologic modeling of cervical dysplasia with molecular and cytopathological markers. Gynecol. Oncol. 2007, 107 (Suppl. 1), S163–S169. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Karakitsos, P.; Chrelias, C.; Pouliakis, A.; Koliopoulos, G.; Spathis, A.; Kyrgiou, M.; Meristoudis, C.; Chranioti, A.; Kottaridi, C.; Valasoulis, G.; et al. Identification of Women for Referral to Colposcopy by Neural Networks: A Preliminary Study Based on LBC and Molecular Biomarkers. J. Biomed. Biotechnol. 2012, 2012, 303192. [Google Scholar] [CrossRef][Green Version]
- Rothberg, M.B.; Hu, B.; Lipold, L.; Schramm, S.; Jin, X.W.; Sikon, A.; Taksler, G.B. A risk prediction model to allow personalized screening for cervical cancer. Cancer Causes Control. 2018, 29, 297–304. [Google Scholar] [CrossRef]
- Bornstein, J.; Bentley, J.; Bösze, P.; Girardi, F.; Haefner, H.; Menton, M.; Perrotta, M.; Prendiville, W.; Russell, P.; Sideri, M.; et al. 2011 Colposcopic Terminology of the International Federation for Cervical Pathology and Colposcopy. Obstet. Gynecol. 2012, 120, 166–172. [Google Scholar] [CrossRef]
- Chan, P.K.; Chang, A.R.; Yu, M.Y.; Li, W.-H.; Chan, M.Y.; Yeung, A.C.; Cheung, T.-H.; Yau, T.-N.; Wong, S.-M.; Yau, C.-W.; et al. Age distribution of human papillomavirus infection and cervical neoplasia reflects caveats of cervical screening policies. Int. J. Cancer 2010, 126, 297–301. [Google Scholar] [CrossRef]
- International Collaboration of Epidemiological Studies of Cervical Cancer. Cervical carcinoma and reproductive factors: Collaborative reanalysis of individual data on 16,563 women with cervical carcinoma and 33,542 women without cervical carcinoma from 25 epidemiological studies. Int. J. Cancer. 2006, 119, 1108–1124. [Google Scholar] [CrossRef]
- Kim, J.M.; Yang, Y.S.; Lee, S.H.; Jee, S.H. Association between Early Menopause, Gynecological Cancer, and Tobacco Smoking: A Cross-Sectional Study. Asian Pac. J. Cancer Prev. 2021, 22, 3165–3170. [Google Scholar] [CrossRef]
- Bai, A.; Wang, J.; Li, Q.; Seery, S.; Xue, P.; Jiang, Y. Assessing colposcopic accuracy for high-grade squamous intraepithelial lesion detection: A retrospective, cohort study. BMC Women’s Health 2022, 22, 9. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Wang, W.; Yang, P.; Chen, J.; Dai, Q.; Hua, P.; Liu, D. Analysis of the agreement between colposcopic impression and histopathological diagnosis of cervical biopsy in a single tertiary center of Chengdu. Arch. Gynecol. Obstet. 2021, 304, 1033–1041. [Google Scholar] [CrossRef] [PubMed]
- Wei, B.; Zhang, B.; Xue, P.; Seery, S.; Wang, J.; Li, Q.; Jiang, Y.; Qiao, Y. Improving colposcopic accuracy for cervical precancer detection: A retrospective multicenter study in China. BMC Cancer 2022, 22, 388. [Google Scholar] [CrossRef] [PubMed]
- Ranga, R.; Rai, S.; Kumari, A.; Mathur, S.; Kriplani, A.; Mahey, R.; Agarwal, N.; Kachhawa, G.; Vanamail, P.; Bhatla, N. A Comparison of the Strength of Association of Reid Colposcopic Index and Swede Score With Cervical Histology. J. Low. Genit. Tract Dis. 2017, 21, 55–58. [Google Scholar] [CrossRef]
- Wu, Z.; Li, T.; Han, Y.; Jiang, M.; Yu, Y.; Xu, H.; Yu, L.; Cui, J.; Bin Liu, B.; Chen, F.; et al. Development of models for cervical cancer screening: Construction in a cross-sectional population and validation in two screening cohorts in China. BMC Med. 2021, 19, 197. [Google Scholar] [CrossRef]
- Del Pino, M.; Angeles, M.A.; Martí, C.; Henere, C.; Munmany, M.; Marimon, L.; Saco, A.; Rakislova, N.; Ordi, J.; Torné, A. Colposcopic Impression Has a Key Role in the Estimation of the Risk of HSIL/CIN3. Cancers 2021, 13, 1224. [Google Scholar] [CrossRef]
- Silver, M.I.; Andrews, J.; Cooper, C.K.; Gage, J.C.; Gold, M.A.; Khan, M.J.; Massad, L.S.; Parvu, V.; Perkins, R.B.; Schiffman, M.; et al. Risk of Cervical Intraepithelial Neoplasia 2 or Worse by Cytology, Human Papillomavirus 16/18, and Colposcopy Impression: A Systematic Review and Meta-analysis. Obstet. Gynecol. 2018, 132, 725–735. [Google Scholar] [CrossRef]
- Zhang, B.; Hong, S.; Zhang, G.; Rong, F. Clinical application of the 2011 IFCPC colposcope terminology. BMC Women’s Health 2021, 21, 257. [Google Scholar] [CrossRef]
- Tekalegn, Y.; Sahiledengle, B.; Woldeyohannes, D.; Atlaw, D.; Degno, S.; Desta, F.; Bekele, K.; Aseffa, T.; Gezahegn, H.; Kene, C. High parity is associated with increased risk of cervical cancer: Systematic review and meta-analysis of case–control studies. Women’s Health 2022, 18, 17455065221075904. [Google Scholar] [CrossRef]
- Khan, I.U.; Aslam, N.; Alshehri, R.; Alzahrani, S.; Alghamdi, M.; Almalki, A.; Balabeed, M. Cervical Cancer Diagnosis Model Using Extreme Gradient Boosting and Bioinspired Firefly Optimization. Sci. Program. 2021, 2021, 5540024. [Google Scholar] [CrossRef]
- Zhong, F.; Yu, T.; Ma, X.; Wang, S.; Cong, Q.; Tao, X. Extensive HPV Genotyping Reveals High Association between Multiple Infections and Cervical Lesions in Chinese Women. Dis. Markers 2022, 2022, 8130373. [Google Scholar] [CrossRef] [PubMed]
- Chaturvedi, A.K.; Katki, H.A.; Hildesheim, A.; Rodríguez, A.C.; Quint, W.; Schiffman, M.; Van Doorn, L.-J.; Porras, C.; Wacholder, S.; Gonzalez, P.; et al. Human Papillomavirus Infection with Multiple Types: Pattern of Coinfection and Risk of Cervical Disease. J. Infect. Dis. 2011, 203, 910–920. [Google Scholar] [CrossRef] [PubMed]
- Salazar, K.L.; Zhou, H.S.; Xu, J.; Peterson, L.E.; Schwartz, M.R.; Mody, D.R.; Ge, Y. Multiple Human Papilloma Virus Infections and Their Impact on the Development of High-Risk Cervical Lesions. Acta Cytol. 2015, 59, 391–398. [Google Scholar] [CrossRef] [PubMed]
- Trottier, H.; Mahmud, S.; Costa, M.C.; Sobrinho, J.P.; Duarte-Franco, E.; Rohan, T.E.; Ferenczy, A.; Villa, L.L.; Franco, E.L. Human Papillomavirus Infections with Multiple Types and Risk of Cervical Neoplasia. Cancer Epidemiol. Biomark. Prev. 2006, 15, 1274–1280. [Google Scholar] [CrossRef] [PubMed]
- Antoniadis, P. Decision Tree vs. Naive Bayes Classifier. 2022. Available online: https://www.baeldung.com/cs/decision-tree-vs-naive-bayes (accessed on 20 June 2022).
- Xue, P.; Ng, M.T.A.; Qiao, Y. The challenges of colposcopy for cervical cancer screening in LMICs and solutions by artificial intelligence. BMC Med. 2020, 18, 169. [Google Scholar] [CrossRef]
- Xue, P.; Tang, C.; Li, Q.; Li, Y.; Shen, Y.; Zhao, Y.; Chen, J.; Wu, J.; Li, L.; Wang, W.; et al. Development and validation of an artificial intelligence system for grading colposcopic impressions and guiding biopsies. BMC Med. 2020, 18, 406. [Google Scholar] [CrossRef]
- Li, Y.; Liu, Z.-H.; Xue, P.; Chen, J.; Ma, K.; Qian, T.; Zheng, Y.; Qiao, Y.-L. GRAND: A large-scale dataset and benchmark for cervical intraepithelial Neoplasia grading with fine-grained lesion description. Med. Image Anal. 2021, 70, 102006. [Google Scholar] [CrossRef]

| Variables | Total (n = 7458) | Training and Internal Validation Set (n = 6564) | External Validation Set (n = 894) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| <HSIL † | HSIL+ ‡ | p | <HSIL † | HSIL+ ‡ | p | <HSIL † | HSIL+ ‡ | p | |
| Numbers | 5663 (75.9) | 1795 (24.1) | 4932 (75.1) | 1632 (24.9) | 731 (81.8) | 163 (18.2) | |||
| Age | 0.003 | 0.02 | 0.031 | ||||||
| <30 | 984 (17.4) | 251 (14.0) | 850 (17.2) | 233 (14.3) | 134 (18.3) | 18 (11.0) | |||
| 30–45 | 3099 (54.7) | 1036 (57.7) | 2761 (56.0) | 945 (57.9) | 338 (46.2) | 91 (55.8) | |||
| >45 | 1580 (27.9) | 508 (28.3) | 1321 (26.8) | 454 (27.8) | 259 (35.4) | 54 (33.1) | |||
| Gravidity | <0.001 | <0.001 | 0.001 | ||||||
| 0 | 681 (12.0) | 139 (7.7) | 584 (11.8) | 133 (8.1) | 97 (13.3) | 6 (3.7) | |||
| 1–2 | 3839 (67.8) | 1240 (69.1) | 3392 (68.8) | 1137 (69.7) | 447 (61.1) | 103 (63.2) | |||
| ≥3 | 1143 (20.2) | 416 (23.2) | 956 (19.4) | 362 (22.2) | 187 (25.6) | 54 (33.1) | |||
| Parity | <0.001 | <0.001 | 0.022 | ||||||
| 0 | 1029 (18.2) | 246 (13.7) | 892 (18.1) | 226 (13.8) | 137 (18.7) | 20 (12.3) | |||
| 1–2 | 4525 (79.9) | 1493 (83.2) | 3946 (80.0) | 1358 (83.2) | 579 (79.2) | 135 (82.8) | |||
| ≥3 | 109 (1.9) | 56 (3.1) | 94 (1.9) | 48 (2.9) | 15 (2.1) | 8 (4.9) | |||
| Menopause | 0.321 | 0.422 | 0.863 | ||||||
| No | 4760 (84.1) | 1527 (85.1) | 4201 (85.2) | 1404 (86.0) | 559 (76.5) | 123 (75.5) | |||
| Yes | 903 (15.9) | 268 (14.9) | 731 (14.8) | 228 (14.0) | 172 (23.5) | 40 (24.5) | |||
| Cytology | <0.001 | <0.001 | <0.001 | ||||||
| NILM | 2931 (51.8) | 454 (25.3) | 2418 (49.0) | 400 (24.5) | 513 (70.2) | 54 (33.1) | |||
| ASC-US | 1660 (29.3) | 396 (22.1) | 1528 (31.0) | 364 (22.3) | 132 (18.1) | 32 (19.6) | |||
| LSIL | 827 (14.6) | 314 (17.5) | 768 (15.6) | 298 (18.3) | 59 (8.1) | 16 (9.8) | |||
| ASC-H | 113 (2.0) | 189 (10.5) | 96 (1.9) | 164 (10.0) | 17 (2.3) | 25 (15.3) | |||
| HSIL | 132 (2.3) | 442 (24.6) | 122 (2.5) | 406 (24.9) | 10 (1.4) | 36 (22.1) | |||
| HR-HPV | <0.001 | <0.001 | <0.001 | ||||||
| Negative | 1311 (23.2) | 81 (4.5) | 1006 (20.4) | 67 (4.1) | 305 (41.7) | 14 (8.6) | |||
| Other HR-HPV positive | 2906 (51.3) | 681 (37.9) | 2645 (53.6) | 624 (38.2) | 261 (35.7) | 57 (35.0) | |||
| HPV16/18 positive | 1446 (25.5) | 1033 (57.5) | 1281 (26.0) | 941 (57.7) | 165 (22.6) | 92 (56.4) | |||
| HR-HPV multi-infection | <0.001 | <0.001 | <0.001 | ||||||
| Negative | 1311 (23.2) | 81 (4.5) | 1006 (20.4) | 67 (4.1) | 305 (41.7) | 14 (8.6) | |||
| Single infection | 2864 (50.5) | 1189 (66.3) | 2476 (50.2) | 1044 (64.0) | 388 (53.1) | 145 (88.9) | |||
| Multiple infections | 1488 (26.3) | 525 (29.2) | 1450 (29.4) | 521 (31.9) | 38 (5.2) | 4 (2.5) | |||
| Transformation zone | <0.001 | <0.001 | <0.001 | ||||||
| Type 1 | 1646 (29.1) | 557 (31.0) | 1288 (26.1) | 454 (27.8) | 358 (49.0) | 103 (63.2) | |||
| Type 2 | 1730 (30.5) | 678 (37.8) | 1632 (33.1) | 651 (39.9) | 98 (13.4) | 27 (16.6) | |||
| Type 3 | 2287 (40.4) | 560 (31.2) | 2012 (40.8) | 527 (32.3) | 275 (37.6) | 33 (20.2) | |||
| Colposcopy | <0.001 | <0.001 | <0.001 | ||||||
| Normal | 2080 (36.7) | 54 (3.0) | 1775 (36.0) | 40 (2.5) | 305 (41.7) | 14 (8.6) | |||
| LSIL | 3262 (57.6) | 433 (24.1) | 2893 (58.7) | 380 (23.3) | 369 (50.5) | 53 (32.5) | |||
| HSIL | 318 (5.6) | 1249 (69.6) | 264 (5.4) | 1172 (71.8) | 54 (7.4) | 77 (47.2) | |||
| Cancer | 3 (0.1) | 59 (3.3) | 0 (0.0) | 40 (2.5) | 3 (0.4) | 19 (11.7) | |||
| Model | AUC (95% CI) | Accuracy % (95% CI) | Sensitivity % (95% CI) | Specificity % (95% CI) | MCC (95% CI) |
|---|---|---|---|---|---|
| Internal validation set | |||||
| LR | 0.909 (0.896–0.922) | 82.31 (80.63–83.99) | 83.87 (81.55–86.20) | 80.83 (78.40–83.26) | 0.647 (0.626–0.668) |
| SVM | 0.914 (0.901–0.926) | 83.83 (82.21–85.46) | 83.66 (81.33–86.00) | 83.99 (81.73–86.25) | 0.677 (0.656–0.697) |
| DT | 0.929 (0.918–0.940) | 84.85 (83.26–86.43) | 85.74 (83.53–87.95) | 83.99 (81.73–86.25) | 0.697 (0.677–0.717) |
| NB | 0.897 (0.883–0.911) | 81.65 (79.94–83.36) | 83.35 (81.00–85.71) | 80.04 (77.58–82.50) | 0.634 (0.613–0.655) |
| RF | 0.919 (0.907–0.931) | 83.78 (82.15–85.41) | 82.41 (80.01–84.82) | 85.08 (82.88–87.27) | 0.675 (0.655–0.696) |
| XGBoost | 0.919 (0.907–0.930) | 82.31 (80.63–83.99) | 84.81 (82.54–87.08) | 79.94 (77.47–82.41) | 0.648 (0.627–0.669) |
| Colposcopists | 0.830 (0.810–0.849) | 83.27 (81.63–84.92) | 70.86 (67.99–73.74) | 95.06 (93.72–96.39) | 0.695 (0.674–0.715) |
| External validation set | |||||
| LR | 0.862 (0.830–0.895) | 78.52 (75.83–81.22) | 80.37 (74.27–86.47) | 78.11 (75.11–81.11) | 0.482 (0.449–0.515) |
| SVM | 0.844 (0.807–0.882) | 77.96 (75.25–80.68) | 79.75 (73.59–85.92) | 77.56 (74.54–80.59) | 0.471 (0.438–0.504) |
| DT | 0.842 (0.808–0.876) | 74.38 (71.52–77.25) | 77.91 (71.55–84.28) | 73.60 (70.40–76.79) | 0.415 (0.383–0.447) |
| NB | 0.874 (0.843–0.905) | 78.19 (75.48–80.90) | 80.98 (74.96–87.01) | 77.56 (74.54–80.59) | 0.480 (0.448–0.513) |
| RF | 0.869 (0.838–0.900) | 80.87 (78.29–83.45) | 76.07 (69.52–82.62) | 81.94 (79.15–84.73) | 0.496 (0.463–0.528) |
| XGBoost | 0.847 (0.814–0.881) | 77.85 (75.13–80.57) | 77.91 (71.55–84.28) | 77.84 (74.83–80.85) | 0.460 (0.428–0.493) |
| Colposcopists | 0.755 (0.708–0.803) | 86.13 (83.86–88.40) | 58.90 (51.34–66.45) | 92.20 (90.26–94.15) | 0.524 (0.491–0.557) |
| Model | Age | Gravidity | Parity | Menopause | Cytology | HR-HPV | HR-HPV Multi-Infection | Transformation Zone | Colposcopy |
|---|---|---|---|---|---|---|---|---|---|
| LR | 8 | 9 | 7 | 6 | 5 | 2 | 3 | 4 | 1 |
| SVM | 4 | 7 | 5 | 6 | 2 | 3 | 8 | 9 | 1 |
| DT | 6 | 5 | 8 | 9 | 2 | 3 | 7 | 4 | 1 |
| NB | 4 | 6 | 7 | 8 | 2 | 3 | 9 | 5 | 1 |
| RF | 7 | 9 | 6 | 8 | 3 | 2 | 5 | 4 | 1 |
| XGBoost | 8 | 6 | 9 | 5 | 3 | 2 | 4 | 7 | 1 |
| Overall † | 6 | 7 | 7 | 7 | 3 | 2 | 5 | 4 | 1 |
| Model | AUC (95% CI) | Accuracy % (95% CI) | Sensitivity % (95% CI) | Specificity % (95% CI) | MCC (95% CI) |
|---|---|---|---|---|---|
| Internal validation set | |||||
| LR | 0.755 (0.733–0.777) | 63.99 (62.67–65.31) | 74.52 (70.36–78.69) | 63.05 (61.66–64.43) | 0.211 (0.200–0.222) |
| SVM | 0.781 (0.759–0.803) | 81.47 (80.40–82.53) | 55.24 (50.48–59.99) | 83.83 (82.77–84.88) | 0.272 (0.260–0.284) |
| DT | 0.836 (0.819–0.854) | 64.33 (63.01–65.64) | 87.38 (84.21–90.56) | 62.25 (60.86–63.64) | 0.277 (0.265–0.289) |
| NB | 0.741 (0.718–0.764) | 61.97 (60.64–63.30) | 74.29 (70.11–78.47) | 60.86 (59.46–62.26) | 0.196 (0.185–0.207) |
| RF | 0.788 (0.768–0.807) | 76.53 (75.37–77.70) | 61.90 (57.26–66.55) | 77.85 (76.66–79.04) | 0.251 (0.239–0.263) |
| XGBoost | 0.789 (0.769–0.809) | 73.98 (72.77–75.18) | 63.81 (59.21–68.41) | 74.89 (73.65–76.14) | 0.236 (0.225–0.248) |
| External validation set | |||||
| LR | 0.752 (0.693–0.812) | 61.67 (58.17–65.17) | 71.64 (60.85–82.43) | 60.68 (56.99–64.37) | 0.188 (0.160–0.216) |
| SVM | 0.714 (0.644–0.784) | 77.33 (74.31–80.34) | 52.24 (40.28–64.20) | 79.82 (76.79–82.85) | 0.218 (0.189–0.248) |
| DT | 0.714 (0.656–0.772) | 62.89 (59.41–66.37) | 56.72 (44.85–68.58) | 63.50 (59.87–67.14) | 0.120 (0.096–0.143) |
| NB | 0.781 (0.725–0.837) | 62.89 (59.41–66.37) | 76.12 (65.91–86.33) | 61.57 (57.90–65.25) | 0.219 (0.189–0.249) |
| RF | 0.773 (0.717–0.828) | 75.71 (72.62–78.80) | 61.19 (49.53–72.86) | 77.15 (73.98–80.32) | 0.250 (0.219–0.281) |
| XGBoost | 0.725 (0.667–0.784) | 63.97 (60.51–67.42) | 64.18 (52.70–75.66) | 63.95 (60.32–67.57) | 0.166 (0.139–0.193) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, M.; Wang, J.; Xue, P.; Li, Q.; Jiang, Y.; Qiao, Y. Evaluating the Feasibility of Machine-Learning-Based Predictive Models for Precancerous Cervical Lesions in Patients Referred for Colposcopy. Diagnostics 2022, 12, 3066. https://doi.org/10.3390/diagnostics12123066
Chen M, Wang J, Xue P, Li Q, Jiang Y, Qiao Y. Evaluating the Feasibility of Machine-Learning-Based Predictive Models for Precancerous Cervical Lesions in Patients Referred for Colposcopy. Diagnostics. 2022; 12(12):3066. https://doi.org/10.3390/diagnostics12123066
Chicago/Turabian StyleChen, Mingyang, Jiaxu Wang, Peng Xue, Qing Li, Yu Jiang, and Youlin Qiao. 2022. "Evaluating the Feasibility of Machine-Learning-Based Predictive Models for Precancerous Cervical Lesions in Patients Referred for Colposcopy" Diagnostics 12, no. 12: 3066. https://doi.org/10.3390/diagnostics12123066
APA StyleChen, M., Wang, J., Xue, P., Li, Q., Jiang, Y., & Qiao, Y. (2022). Evaluating the Feasibility of Machine-Learning-Based Predictive Models for Precancerous Cervical Lesions in Patients Referred for Colposcopy. Diagnostics, 12(12), 3066. https://doi.org/10.3390/diagnostics12123066







