Diabetic Striatopathy: Parenchymal Transcranial Sonography as a Supplement to Diagnosis at the Emergency Department
Abstract
1. Introduction
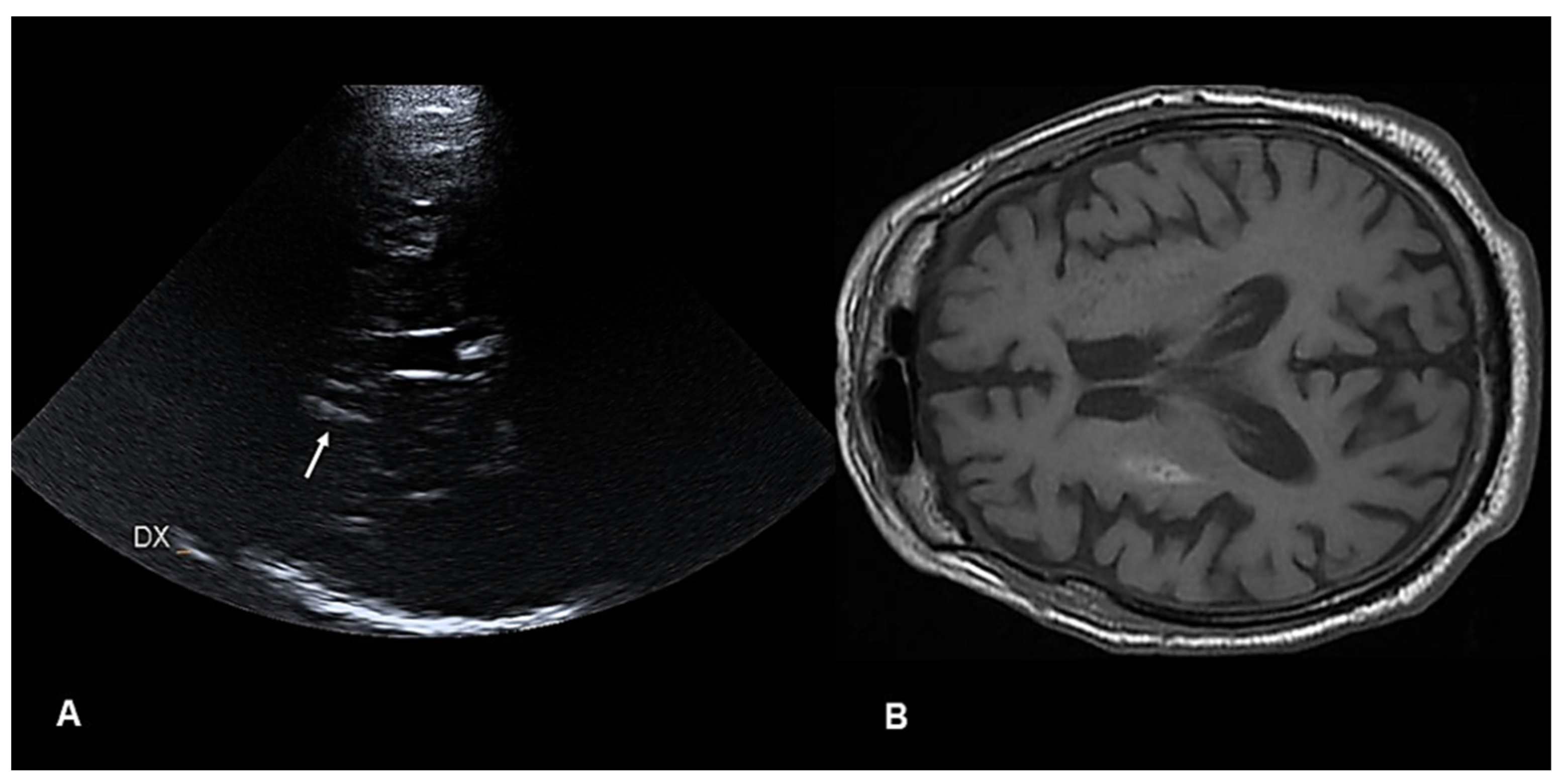
2. Case Report
3. Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Herath, H.; Pahalagamage, S.; Senanayake, S. Case report of hyperglycemic nonketotic chorea with rapid radiological resolution. BMC Med. Imaging 2017, 17, 54. [Google Scholar] [CrossRef] [PubMed]
- Carrion, D.M.; Carrion, A.F. Non-ketotic hyperglycaemia hemichorea–hemiballismus and acute is-chaemic stroke. BMJ Case Rep. 2013, 2013, bcr2012008359. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Song, C. Chorea associated with nonketotic hyperglycemia: An uncommon patient with bilateral movements. J. Clin. Neurosci. 2015, 22, 1068–1069. [Google Scholar] [CrossRef] [PubMed]
- Qi, X.; Yan, Y.-y.; Gao, Y.; Zheng, Z.-s.; Chang, Y. Hemichorea associated with non-ketotic hyperglycaemia: A case report. Diabetes Res. Clin. Pract. 2012, 95, e1–e3. [Google Scholar] [CrossRef]
- Oh, S.-H.; Lee, K.-Y.; Im, J.-H.; Lee, M.-S. Chorea associated with non-ketotic hyperglycemia and hyperintensity basal ganglia lesion on T1-weighted brain MRI study: A meta-analysis of 53 cases including four present cases. J. Neurol. Sci. 2022, 200, 57–62. [Google Scholar] [CrossRef]
- Son, B.C.; Choi, J.G.; Ko, H.C. Globus Pallidus Internus Deep Brain Stimulation for Disabling Diabetic Hemiballism/Hemichorea. Case Rep. Neurol. Med. 2017, 2017, 2165905. [Google Scholar] [CrossRef]
- Bizet, J.; Cooper, C.J.; Quansah, R.; Rodriguez, E.; Teleb, M.; Hernandez, G.T. Chorea, hyperglycemia, basal ganglia syndrome (CH-BG) in an uncontrolled diabetic patient with normal glucose levels on presentation. Am. J. Case Rep. 2014, 15, 143–146. [Google Scholar]
- Abe, Y.; Yamamoto, T.; Soeda, T.; Kumagai, T.; Tanno, Y.; Kubo, J.; Ishihara, T.; Katayama, S. Diabetic striatal disease: Clinical presentation, neuroimaging, and pathology. Int. Med. 2009, 48, 1135–1141. [Google Scholar] [CrossRef]
- Chua, C.B.; Sun, C.K.; Hsu, C.W.; Tai, Y.C.; Liang, C.Y.; Tsai, I.T. “Diabetic striatopathy”: Clinical presentations, controversy, pathogenesis, treatments, and outcomes. Sci. Rep. 2020, 10, 1594. [Google Scholar] [CrossRef]
- Ryan, C.; Ahlskog, J.E.; Savica, R. Hyperglycemic chorea/ballism ascertained over 15 years at a referral medical center. Park. Relat. Disord. 2018, 48, 97–100. [Google Scholar] [CrossRef]
- Huang, X.; Qi, J.; Li, Y.; Li, J.; Yang, M.G. Diabetic Striatopathy Complicated with Acute Ischemic Stroke: A Case Report. Front. Neurosci. 2022, 16, 877479. [Google Scholar] [CrossRef]
- Shan, D.-E.; Ho, D.; Chang, C.; Pan, H.-C.; Teng, M. Hemichorea-hemiballism: An explanation for MR signal changes. Am. J. Neuroradiol. 1998, 19, 863–870. [Google Scholar] [PubMed]
- Ottaviani, S.; Arecco, A.; Boschetti, M.; Ottaviani, E.; Renzetti, P.; Marinelli, L. Prevalence of diabetic striatopathy and predictive role of glycated hemoglobin level. Neurol. Sci. 2022, 43, 6059–6065. [Google Scholar] [CrossRef] [PubMed]
- Das, L.; Pal, R.; Dutta, P.; Bhansali, A. “Diabetic striatopathy” and ketoacidosis: Report of two cases and review of literature. Diabetes Res. Clin. Pract. 2017, 128, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Nath, J.; Jambhekar, K.; Rao, C.; Armitano, E. Radiological and pathological changes in hemiballism-hemichorea with striatal hyperintensity. J. Magn. Reson. Imaging 2006, 23, 564–568. [Google Scholar] [CrossRef] [PubMed]
- Shafran, I.; Greenberg, G.; Grossman, E.; Leibowitz, A. Diabetic striatopathy-Does it exist in non-Asian subjects? Eur. J. Intern. Med. 2016, 35, 51–54. [Google Scholar] [CrossRef] [PubMed]
- Cosentino, C.; Torres, L.; Nuñez, Y.; Suarez, R.; Velez, M.; Flores, M. Hemichorea/Hemiballism associated with hyperglycemia: Report of 20 cases. Tremor Other Hyperkinet. Mov. 2016, 6, 402. [Google Scholar] [CrossRef]
- Dubey, S.; Biswas, P.; Ghosh, R.; Chatterjee, S.; Kanti Ray, B.; Benito-León, J. Neuroimaging of Diabetic Striatopathy: More Questions than Answers. Eur. Neurol. 2022, 85, 371–376. [Google Scholar] [CrossRef] [PubMed]
- Chua, C.B.; Chen, H.C.; Su, H.Y.; Tsai, I.T.; Sun, C.K. Images of the month 1: Diabetic striatopathy without hemichorea/hemiballism. Clin. Med. 2019, 19, 412–413. [Google Scholar] [CrossRef]
- Cho, H.-S.; Hong, C.-T.; Chan, L. Hemichorea after hyperglycemia correction: A case report and a short review of hyperglycemiarelated hemichorea at the euglycemic state. Medicine 2018, 97, e0067. [Google Scholar] [CrossRef]
- Rai, S.; Kaul, V.; Singh, S.; Kaur, S.; Thenmurugan, P. Diabetic Striatopathy: A New Challenge in Type 1 Pediatric Diabetic Patients. Oman Med. J. 2022, 37, e332. [Google Scholar] [CrossRef] [PubMed]
- Suárez-Vega, V.M.; Sánchez Almaraz, C.; Bernardo, A.I.; Rodríguez-Díaz, R.; Díez Barrio, A.; Martín Gil, L. CT and MR Unilateral Brain Features Secondary to Nonketotic Hyperglycemia Presenting as Hemichorea-Hemiballism. Case Rep. Radiol. 2016, 2016, 5727138. [Google Scholar] [CrossRef] [PubMed]
- Roy, U.; Das, S.K.; Mukherjee, A.; Biswas, D.; Pan, K.; Biswas, A.; Panwar, A. Irreversible Hemichorea-Hemiballism in a Case of Nonketotic Hyperglycemia Presenting as the Initial Manifestation of Diabetes Mellitus. Tremor Other Hyperkinet. Mov. 2016, 6, 393. [Google Scholar] [CrossRef]
- Nakajima, N.; Ueda, M.; Nagayama, H.; Katayama, Y. Putaminal changes before the onset of clinical symptoms in diabetic hemichorea-hemiballism. Intern. Med. 2014, 53, 489–491. [Google Scholar] [CrossRef] [PubMed]
- Baizabal-Carvallo, J.F.; Ondo, W.G. Stereotypies as a manifestation of acute hyperglycemia without ketosis. J. Neurol. Sci. 2012, 315, 176–177. [Google Scholar] [CrossRef]
- Battisti, C.; Forte, F.; Rubenni, E.; Dotti, M.T.; Bartali, A.; Gennari, P.; Federico, A.; Cerase, A. Two cases of hemichorea-hemiballism with nonketotic hyperglycemia: A new point of view. Neurol. Sci. 2009, 30, 179–183. [Google Scholar] [CrossRef]
- Patel, B.; Ladva, Z.R.; Khan, U. Hemichorea–hemiballism: A case report. Pract. Neurol. 2015, 15, 222–223. [Google Scholar] [CrossRef]
- Ohmori, H.; Hirashima, K.; Ishihara, D.; Maeda, Y.; Hirano, T.; Uyama, E.; Uchino, M. Two cases of hemiballism-hemichorea with T1-weighted MR image hyperintensities. Intern. Med. 2005, 44, 1280–1285. [Google Scholar] [CrossRef]
- Danve, A.; Kulkarni, S.; Bhoite, G. Non-ketotic hyperglycemia unmasks hemichorea. J. Community Hosp. Intern. Med. Perspect. 2015, 5, 27825. [Google Scholar] [CrossRef]
- Pisani, A.; Diomedi, M.; Rum, A.; Cianciulli, P.; Floris, R.; Orlacchio, A.; Bernardi, G.; Calabresi, P. Acanthocytosis as a predisposing factor for non-ketotic hyperglycaemia induced chorea-ballism. J. Neurol. Neurosurg. Psychiatry 2005, 76, 1717–1719. [Google Scholar] [CrossRef]
- Shobha, N.; Sinha, S.; Taly, A.; Pal, P.; Chandrasekhar, H. Diabetic nonketotic hyperosmolar state: Interesting imaging observations in 2 patients with involuntary movements and seizures. Neurol. India 2006, 54, 440–442. [Google Scholar] [PubMed]
- Kitagawa, M.; Yamanaka, Y.; Adachi, T.; Ito, J.; Fukase, K.; Ohta, I.; Katagiri, T. Hemichorea-hemiballism afer Prompt Improvement in Hyperglycemia. Intern. Med. 2017, 56, 3073–3076. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pinsker, J.E.; Shalileh, K.; Rooks, V.J.; Pinsker, R.W. Hemichorea-hemiballism secondary to non-ketotic hyperglycemia. J. Clin. Med. Res. 2015, 7, 729–730. [Google Scholar] [CrossRef] [PubMed]
- Ruhangisa, F.; Stephen, H.; Senkondo, J.; Mwasamwaja, A.; Kanenda, S.; Mbarak, S.; Chamba, N.; Kilonzo, K.; Howlett, W.; Lyaruu, I.; et al. Acute hemichorea in a newly diagnosed type II diabetes patient: A diagnostic challenge in resource-limited setting: A case report. BMC Res. Notes 2016, 9, 413. [Google Scholar] [CrossRef] [PubMed]
- Sato, H.; Hamano, M.; Fushimi, E.; Takahashi, T.; Horikawa, Y.; Horiguchi, S. Diabetic striatopathy manifesting as severe consciousness disturbance with no involuntary movements. Diabet. Med. 2017, 34, 1795–1799. [Google Scholar] [CrossRef]
- Safan, A.S.; Sharma, O.; Almasri, M.; D’Souza, A.I.; Suliman, O. Is diabetic striatopathy the culprit of seizures in a patient with ketotic hyperglycemia-induced hemichorea-hemiballismus? BMC Neurol. 2022, 22, 133. [Google Scholar] [CrossRef]
- Evers Smith, C.M.; Chaurasia, K.K.; Dekoski, D.C. Non-ketotic Hyperglycemic Hemichorea-Hemiballismus: A Case of a Male with Diabetes Mellitus and Speech Disturbances. Cureus 2022, 14, e25073. [Google Scholar] [CrossRef]
- Tung, C.-S.; Guo, Y.-C.; Lai, C.-L.; Liou, L.-M. Irreversible striatal neuroimaging abnormalities secondary to prolonged, uncontrolled diabetes mellitus in the setting of progressive focal neurological symptoms. Neurol. Sci. 2010, 31, 57–60. [Google Scholar] [CrossRef]
- Chatterjee, S.; Ghosh, R.; Ojha, U.K.; Diksha Biswas, P.; Benito-León, J.; Dubey, S. Recurrent Facial Focal Seizures with Chronic Striatopathy and Caudate Atrophy-A Double Whammy in an Elderly Woman with Diabetes Mellitus. Neurohospitalist 2022, 12, 147–150. [Google Scholar] [CrossRef]
- Lin, Y.T.; Chen, S.C.; Yip, P.K.; Wang, V. Magnetic resonance imaging volumetric analysis for diabetic striatopathy with two episodes of hemichorea-hemiballism syndrome: A case report. Medicine 2019, 98, e17249. [Google Scholar] [CrossRef]
- Sitburana, O.; Ondo, W.G. Tetrabenazine for hyperglycemic-induced hemichorea–hemiballismus. Mov. Disord. 2006, 21, 2023–2025. [Google Scholar] [CrossRef] [PubMed]
- Walter, U. Transcranial sonography in brain disorders with trace metal accumulation. Int. Rev. Neurobiol. 2010, 90, 166–178. [Google Scholar] [PubMed]
- Godani, M.; Lanza, G.; Trevisan, L.; Ferri, R.; Bella, R. An unusual gait disorder at the Emergency Department: Role of the quantitative assessment of parenchymal transcranial Doppler sonography. Quant. Imaging Med. Surg. 2021, 11, 2195–2200. [Google Scholar] [CrossRef] [PubMed]
- Godani, M.; Canavese, F.; Del Sette, M.; Walter, U. Update on transcranial sonography applications in movement disorders. J Diagn. Imaging Ther. 2014, 1, 110–128. [Google Scholar] [CrossRef][Green Version]
- Richter, D.; Katsanos, A.H.; Schroeder, C.; Tsivgoulis, G.; Paraskevas, G.P.; Müller, T.; Alexandrov, A.V.; Gold, R.; Tönges, L.; Krogias, C. Lentiform Nucleus Hyperechogenicity in Parkinsonian Syndromes: A Systematic Review and Meta-Analysis with Consideration of Molecular Pathology. Cells 2019, 9, 2. [Google Scholar] [CrossRef] [PubMed]
- Walter, U.; Skowrońska, M.; Litwin, T.; Szpak, G.M.; Jabłonka-Salach, K.; Skoloudík, D.; Bulska, E.; Członkowska, A. Lenticular nucleus hyperechogenicity in Wilson’s disease reflects local copper, but not iron accumulation. J. Neural. Transm. 2014, 121, 1273–1279. [Google Scholar] [CrossRef] [PubMed]
- Martin, M.; Thomas, T.; Ekkehard, H.; Katharina, S. Transcranial ultrasound of the basal ganglia in sporadic Creutzfeldt-Jakob disease. J. Neuroimaging 2008, 18, 154–157. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, Y.C.; Sheng, Y.J.; Chen, X.F.; Wang, C.S.; Ma, Q.; Chen, H.B.; Yu, L.F.; Mao, C.J.; Xiong, K.P.; et al. Sonographic Alteration of Basal Ganglia in Different Forms of Primary Focal Dystonia: A Cross-sectional Study. Chin. Med. J. 2016, 129, 942–945. [Google Scholar] [CrossRef]
- Toscano, M.; Canevelli, M.; Giacomelli, E.; Zuco, C.; Fiorelli, M.; Di Piero, V.; Lenzi, G.L.; Vicenzini, E. Transcranial sonography of basal ganglia calcifications in Fahr disease. J. Ultrasound Med. 2011, 30, 1032–1033. [Google Scholar] [CrossRef]
- Kostić, V.S.; Svetel, M.; Mijajlović, M.; Pavlović, A.; Ječmenica-Lukić, M.; Kozić, D. Transcranial sonography in pantothenate kinase-associated neurodegeneration. J. Neurol. 2012, 259, 959–964. [Google Scholar] [CrossRef]
- Mestre, T.A.; Ferreira, J.J.; Pimentel, J. Putaminal petechial haemorrhage as the cause of non-ketotic hyperglycaemic chorea: A neuropathological case correlated with MRI findings. J. Neurol. Neurosurg. Psychiatry 2007, 78, 549–550. [Google Scholar] [CrossRef] [PubMed]
- Duker, A.P.; Espay, A.J. Hemichorea–hemiballism afer diabetic ketoacidosis. N. Engl. J. Med. 2010, 363, e27. [Google Scholar] [CrossRef] [PubMed]
- Altafullah, I.; Pascual-Leone, A.; Duvall, K.; Anderson, D.; Taylor, S. Putaminal hemorrhage accompanied by hemichorea/hemiballism. Stroke 1990, 21, 1093–1094. [Google Scholar] [CrossRef] [PubMed]
- Chu, K.; Kang, D.-W.; Kim, D.-E.; Park, S.-H.; Roh, J.-K. Diffusion-weighted and gradient echo magnetic resonance fndings of hemichorea-hemiballismus associated with diabetic hyperglycemia: A hyperviscosity syndrome? Arch. Neurol. 2002, 59, 448–452. [Google Scholar] [CrossRef] [PubMed]
- Dharsono, F.; Thompson, A.; van Heerden, J.; Cheung, A. Susceptibility weighted imaging as a useful imaging adjunct in hemichorea hyperglycaemia. Case Rep. Radiol. 2013, 2013, 456156. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.J.; Huang, P. Delayed onset diabetic striatopathy: Hemichorea-hemiballism one month after a hyperglycemic episode. Am. J. Emerg. Med. 2017, 35, e3–e1036. [Google Scholar] [CrossRef]
- Lee, E.J.; Choi, J.Y.; Lee, S.H.; Song, S.-Y.; Lee, Y.S. Hemichorea-hemiballism in primary diabetic patients: MR correlation. J. Comput. Assist. Tomogr. 2002, 26, 905–911. [Google Scholar] [CrossRef]
- Ohara, S.; Nakagawa, S.; Tabata, K.; Hashimoto, T. Hemiballism with hyperglycemia and striatal T1-MRI hyperintensity: An autopsy report. Mov. Disord. 2001, 16, 521–525. [Google Scholar] [CrossRef]
- Mansueto, G.; Lanza, G.; Fisicaro, F.; Alaouieh, D.; Hong, E.; Girolami, S.; Montella, M.; Feola, A.; Di Napoli, M. Central and Peripheral Nervous System Complications of Vasculitis Syndromes from Pathology to Bedside: Part 1-Central Nervous System. Curr. Neurol. Neurosci. Rep. 2022, 22, 47–69. [Google Scholar] [CrossRef]
- Tsalta-Mladenov, M.E.; Georgieva, D.K.; Andonova, S.P. Hyperglycemic hemichorea due to diabetic striatopathy: Case-based review. Curr. Med. Res. Opin. 2022, 38, 365–369. [Google Scholar] [CrossRef]
- Park, G.; Kesserwani, H.N. A Case Report of Diabetic Striatopathy: An Approach to Diagnosis Based on Clinical and Radiological Findings. Cureus 2022, 14, e25089. [Google Scholar] [CrossRef] [PubMed]

| Location | CT (n = 126) | MRI (n = 153) |
|---|---|---|
| Caudate nucleus | 1 | 2 |
| Caudate nucleus and putamen | 29 | 26 |
| Caudate nucleus, putamen, and globus pallidus | 30 | 36 |
| Globus pallidus | 0 | 0 |
| Globus pallidus and caudate nucleus | 0 | 0 |
| Globus pallidus and putamen | 5 | 15 |
| Putamen | 35 | 67 |
| No abnormality | 26 | 7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Godani, M.; Lanza, G. Diabetic Striatopathy: Parenchymal Transcranial Sonography as a Supplement to Diagnosis at the Emergency Department. Diagnostics 2022, 12, 2838. https://doi.org/10.3390/diagnostics12112838
Godani M, Lanza G. Diabetic Striatopathy: Parenchymal Transcranial Sonography as a Supplement to Diagnosis at the Emergency Department. Diagnostics. 2022; 12(11):2838. https://doi.org/10.3390/diagnostics12112838
Chicago/Turabian StyleGodani, Massimiliano, and Giuseppe Lanza. 2022. "Diabetic Striatopathy: Parenchymal Transcranial Sonography as a Supplement to Diagnosis at the Emergency Department" Diagnostics 12, no. 11: 2838. https://doi.org/10.3390/diagnostics12112838
APA StyleGodani, M., & Lanza, G. (2022). Diabetic Striatopathy: Parenchymal Transcranial Sonography as a Supplement to Diagnosis at the Emergency Department. Diagnostics, 12(11), 2838. https://doi.org/10.3390/diagnostics12112838







