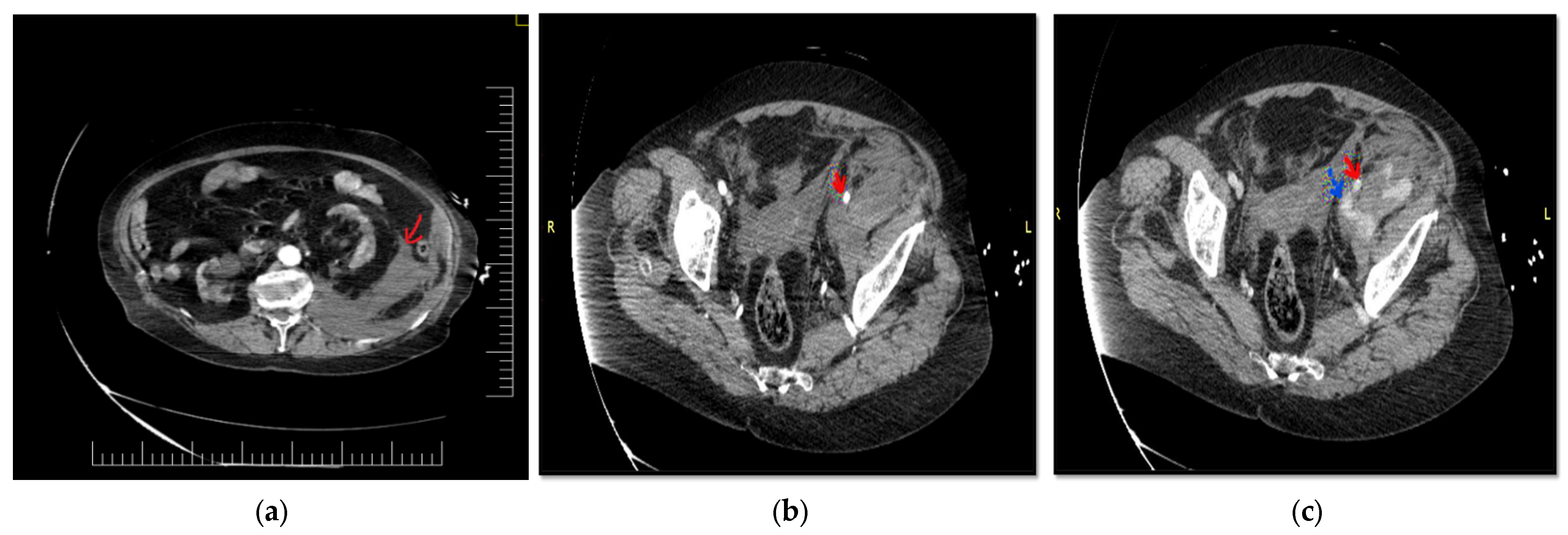
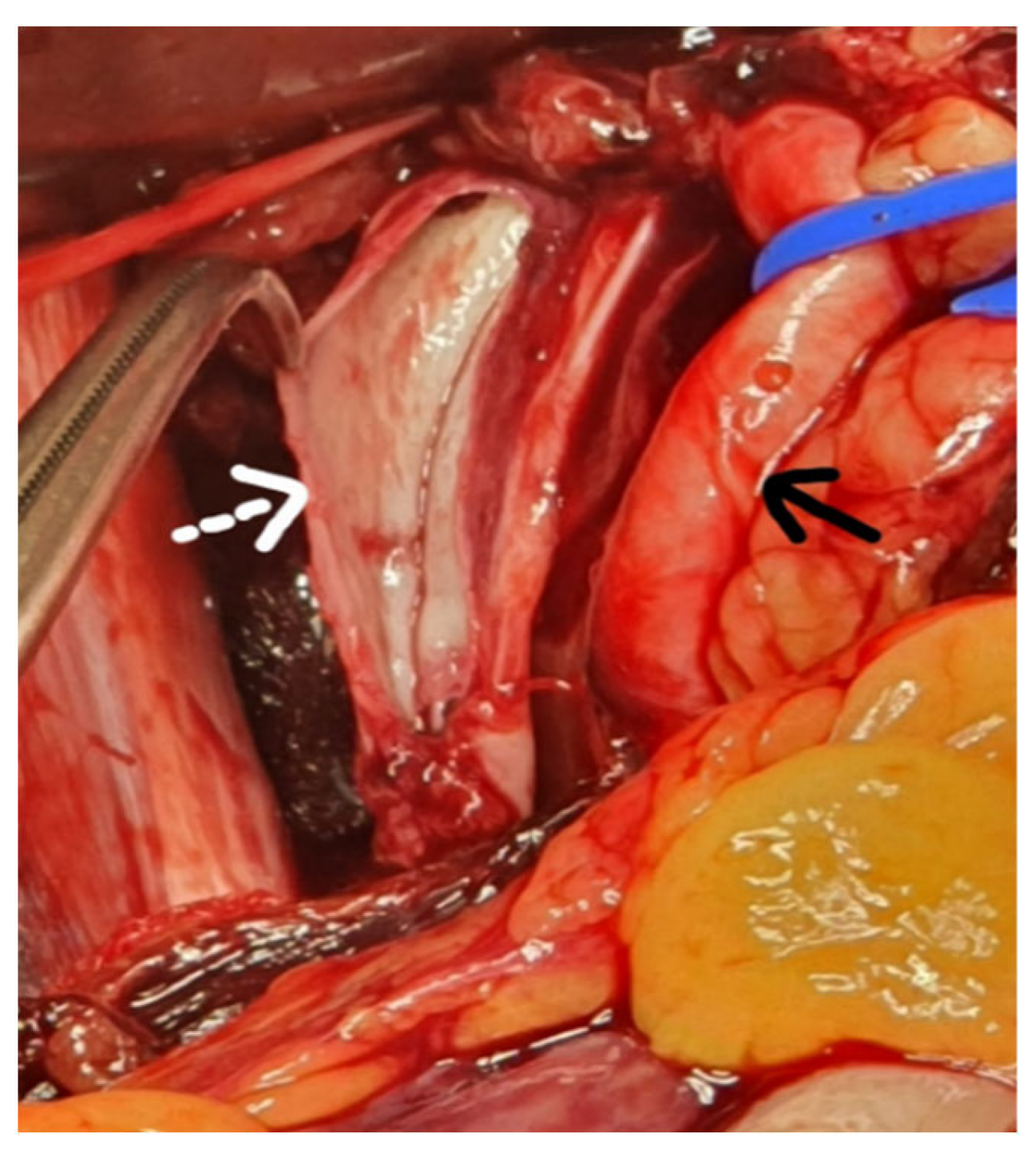
Spontaneous Left External Iliac Vein Rupture
Abstract
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- McCready, R.A.; Kiell, C.S.; Webb, T.H. Spontaneous iliac vein rupture: An uncommon, but frequently lethal, event. J. Vasc. Surg. Cases Innov. Tech. 2021, 7, 558–562. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Ding, X.; Zhang, G.; Su, Q.; Wang, Z.; Hu, S. Spontaneous retroperitoneal hematoma associated with iliac vein rupture. J. Vasc. Surg. 2010, 52, 1278–1282. [Google Scholar] [CrossRef] [PubMed]
- Zang, H.; Zhang, T.; Liu, A.L.; Wang, F.; Shi, H. Spontaneous rupture of the right external iliac vein. Ann. Vasc. Surg. 2011, 25, 701.e1–701.e4. [Google Scholar] [CrossRef] [PubMed]
- Nishimoto, Y.; Toma, M.; Iwasa, K.; Sato, Y. Successful staged management of a spontaneous iliac vein rupture associated with May-Thurner syndrome: A case report. Eur. Heart J. Case Rep. 2021, 5, ytab316. [Google Scholar] [CrossRef] [PubMed]
- Mangla, A.; Hamad, H. May-Thurner Syndrome. In StatPearls [Internet]; Treasure Island (FL) StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Joseph, R.; Owsley, J. Spontaneous rupture of the iliac vein. Am. J. Emerg. Med. 2017, 35, 1585.e3–1585.e4. [Google Scholar] [CrossRef] [PubMed]
- Kwon, T.W.; Yang, S.M.; Kim, D.K.; Kim, G.E. Spontaneous rupture of the left external iliac vein. Yonsei Med. J. 2004, 45, 174–176. [Google Scholar] [CrossRef] [PubMed]
- Ullah, A.; Marwat, A.; Suresh, K.; Khalil, A.; Waseem, S. Spontaneous Retroperitoneal Hematoma: A Rare Presentation of Polyarteritis Nodosa. J. Investig. Med. High Impact Case Rep. 2019, 7, 2324709619858120. [Google Scholar] [CrossRef] [PubMed]
- Marzano, L.A.; Tauchmanova, L.; Marzano, E.; Arienzo, R.; Guarino, R.; Ciancia, G.; Porcelli, A.; Lombardi, G.; Rossi, R. Large idiopathic unilateral adrenal hematoma in a young woman. J. Endocrinol. Investig. 2007, 30, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.; Downing, R.; Vijay, S. Spontaneous rupture of the adrenal artery successfully treated using the endovascular approach: A report of 2 cases. Vasc. Endovasc. Surg. 2013, 47, 124–127. [Google Scholar] [CrossRef] [PubMed]
- Hng, J.; Su, S.; Atkinson, N. May-Thurner syndrome, a diagnosis to consider in young males with no risk factors: A case report and review of the literature. J. Med. Case Rep. 2021, 15, 141. [Google Scholar] [CrossRef] [PubMed]
- Sunga, K.L.; Bellolio, M.F.; Gilmore, R.M.; Cabrera, D. Spontaneous retroperitoneal hematoma: Etiology, characteristics, management, and outcome. J. Emerg. Med. 2012, 43, e157–e161. [Google Scholar] [CrossRef] [PubMed]
- Tannous, H.; Nasrallah, F.; Marjani, M. Spontaneous Iliac vein rupture: Case report and comprehensive review of the literature. Ann. Vasc. Surg. 2006, 20, 258–262. [Google Scholar] [CrossRef] [PubMed]
- Pedley, D.; Nagy, J.; Nichol, N. Spontaneous iliac vein rupture: Case report and literature review. J. R. Coll. Surg. Edinb. 2002, 47, 510–511. [Google Scholar] [PubMed]
- Nishida, S.; Arikawa, K.; Yamashita, M.; Kawashima, S.; Shiota, K.; Tabata, D. Spontaneous rupture of left external iliac vein--a case report. Nihon Geka Gakkai Zasshi 1993, 94, 424–426. [Google Scholar] [PubMed]
- Kim, I.H.; Chon, G.R.; Jo, Y.S.; Park, S.B.; Han, S.D. Spontaneous left external iliac vein rupture. J. Korean Surg. Soc. 2011, 81 (Suppl. S1), S82–S84. [Google Scholar] [CrossRef] [PubMed]
- Fischer, J.E.; Ellison, E.C.; Upchurch, G.R., Jr.; Galandiuk, S.; Gould, J.C.; Klimberg, V.S. Mastery of Surgery, 7th ed.; Wolters Kluwer: Philadelphia, Pennsylvania, 2019; Volume 2, pp. 2499–2504. [Google Scholar]
- Chen, Y.C.; Huang, C.L.; Huang, J.W. Endovascular Stent Can Be the Treatment of Choice for Spontaneous Iliac Vein Rupture: A Case Report. Vasc. Endovasc. Surg. 2018, 52, 131–134. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fugărețu, C.; Mișarca, C.; Vlada, G.; Cîrnațiu, A.; Buzea, C.; Marinescu, D. Spontaneous Left External Iliac Vein Rupture. Diagnostics 2022, 12, 2820. https://doi.org/10.3390/diagnostics12112820
Fugărețu C, Mișarca C, Vlada G, Cîrnațiu A, Buzea C, Marinescu D. Spontaneous Left External Iliac Vein Rupture. Diagnostics. 2022; 12(11):2820. https://doi.org/10.3390/diagnostics12112820
Chicago/Turabian StyleFugărețu, Cosmina, Cătalin Mișarca, Gina Vlada, Andrada Cîrnațiu, Cosmin Buzea, and Daniela Marinescu. 2022. "Spontaneous Left External Iliac Vein Rupture" Diagnostics 12, no. 11: 2820. https://doi.org/10.3390/diagnostics12112820
APA StyleFugărețu, C., Mișarca, C., Vlada, G., Cîrnațiu, A., Buzea, C., & Marinescu, D. (2022). Spontaneous Left External Iliac Vein Rupture. Diagnostics, 12(11), 2820. https://doi.org/10.3390/diagnostics12112820





