Commercially Available Molecular Approaches to Evaluate Endometrial Receptivity: A Systematic Review and Critical Analysis of the Literature
Abstract
1. Introduction
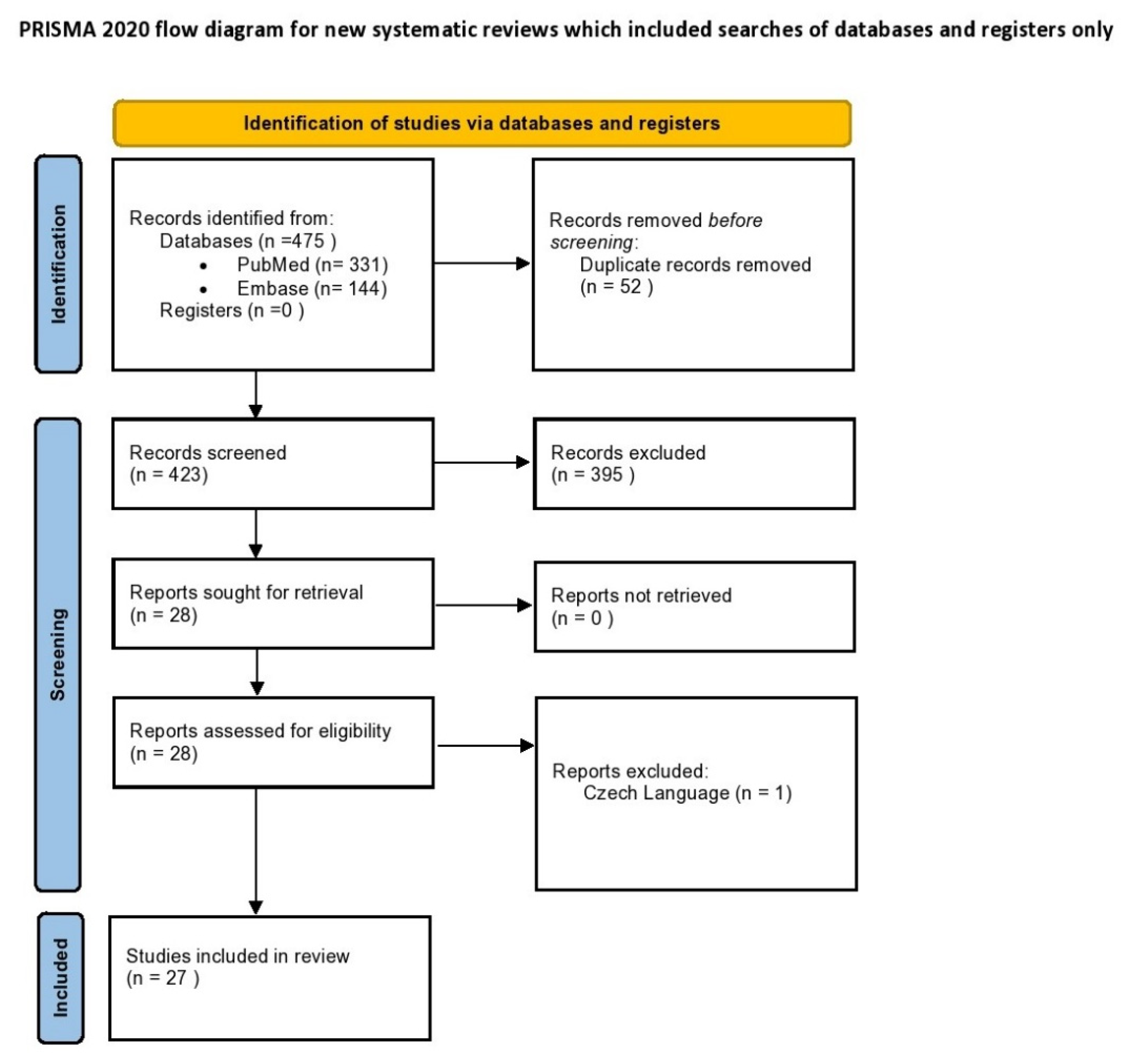
2. Materials and Methods
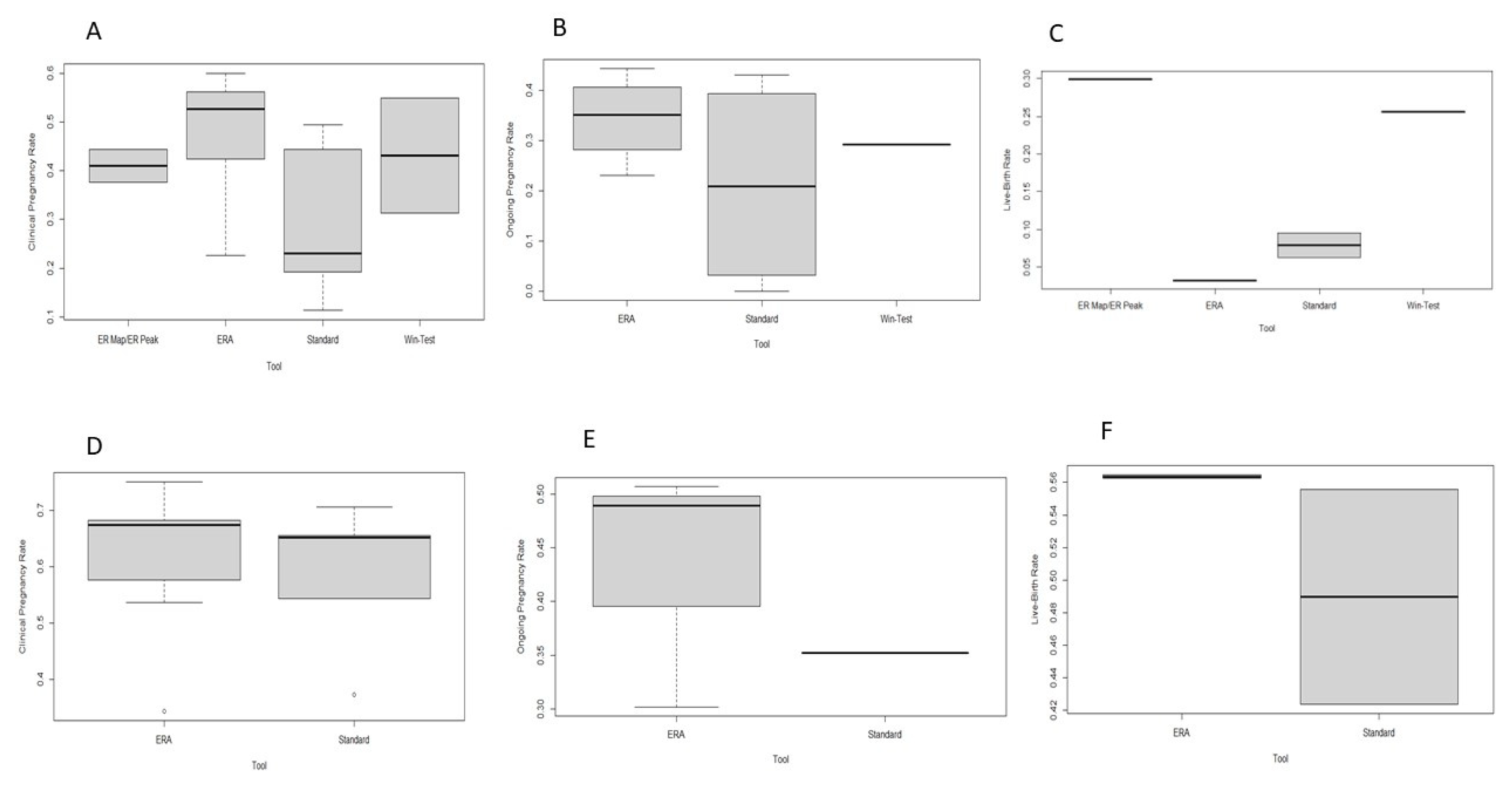
3. Results
3.1. Evolution of Commercially Available Tools for Endometrial Receptivity
3.2. Window of Implantation Test (WIN-TEST)
3.3. Endometrial Receptivity Array (ERA)
3.4. ER Map/ER Peak
3.5. BeREady Test
3.6. The Future of Transcriptomic Analysis for Identification of Endometrial Receptivity (ER)
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mani, S.; Mainigi, M. Embryo Culture Conditions and the Epigenome. Semin. Reprod. Med. 2018, 36, 211–220. [Google Scholar] [CrossRef] [PubMed]
- Simopoulou, M.; Sfakianoudis, K.; Rapani, A.; Giannelou, P.; Anifandis, G.; Bolaris, S.; Pantou, A.; Lambropoulou, M.; Pappas, A.; Deligeoroglou, E.; et al. Considerations Regarding Embryo Culture Conditions: From Media to Epigenetics. In Vivo 2018, 32, 451–460. [Google Scholar] [CrossRef]
- Kirkegaard, K.; Agerholm, I.E.; Ingerslev, H.J. Time-lapse monitoring as a tool for clinical embryo assessment. Hum. Reprod. 2012, 27, 1277–1285. [Google Scholar] [CrossRef]
- Gardner, D.K.; Balaban, B. Assessment of human embryo development using morphological criteria in an era of time-lapse, algorithms and ‘OMICS’: Is looking good still important? Mol. Hum. Reprod. 2016, 22, 704–718. [Google Scholar] [CrossRef] [PubMed]
- Kontopoulos, G.; Simopoulou, M.; Zervomanolakis, I.; Prokopakis, T.; Dimitropoulos, K.; Dedoulis, E.; Grigorakis, S.; Agapitou, K.; Nikitos, E.; Rapani, A.; et al. Cleavage Stage versus Blastocyst Stage Embryo Transfer in Oocyte Donation Cycles. Medicina 2019, 55, 293. [Google Scholar] [CrossRef] [PubMed]
- Simopoulou, M.; Sfakianoudis, K.; Tsioulou, P.; Rapani, A.; Maziotis, E.; Giannelou, P.; Grigoriadis, S.; Pantou, A.; Nikolettos, K.; Vlahos, N.; et al. Should the flexibility enabled by performing a day-4 embryo transfer remain as a valid option in the IVF laboratory? A systematic review and network meta-analysis. J. Assist. Reprod. Genet. 2019, 36, 1049–1061. [Google Scholar] [CrossRef]
- Li, Y.-X.; Wang, J.; Sun, T.-Z.; Lv, M.-Q.; Ge, P.; Li, H.-N.; Zhou, D.-X. Pregnancy outcomes after day 5 versus day 6 blastocyst-stage embryo transfer: A systematic review and meta-analysis. J. Obstet. Gynaecol. Res. 2020, 46, 595–605. [Google Scholar] [CrossRef]
- Tomari, H.; Kawamura, T.; Asanoma, K.; Egashira, K.; Kawamura, K.; Honjo, K.; Nagata, Y.; Kato, K. Contribution of senescence in human endometrial stromal cells during proliferative phase to embryo receptivity †. Biol. Reprod. 2020, 103, 104–113. [Google Scholar] [CrossRef]
- Luddi, A.; Pavone, V.; Semplici, B.; Governini, L.; Criscuoli, M.; Paccagnini, E.; Gentile, M.; Morgante, G.; De Leo, V.; Belmonte, G.; et al. Organoids of Human Endometrium: A Powerful In Vitro Model for the Endometrium-Embryo Cross-Talk at the Implantation Site. Cells 2020, 9, 1121. [Google Scholar] [CrossRef]
- Craciunas, L.; Gallos, I.; Chu, J.; Bourne, T.; Quenby, S.; Brosens, J.J.; Coomarasamy, A. Conventional and modern markers of endometrial receptivity: A systematic review and meta-analysis. Hum. Reprod. Update 2019, 25, 202–223. [Google Scholar] [CrossRef]
- Cha, J.; Vilella, F.; Dey, S.; Simón, C. Molecular Interplay in Successful Implantation: Ten Critical Topics in Reproductive Medicine—A Sponsored Supplement to Science. Science 2013, 44–48. [Google Scholar] [CrossRef]
- Massimiani, M.; Lacconi, V.; La Civita, F.; Ticconi, C.; Rago, R.; Campagnolo, L. Molecular Signaling Regulating Endometrium–Blastocyst Crosstalk. Int. J. Mol. Sci. 2019, 21, 23. [Google Scholar] [CrossRef]
- Kieu, V.; Lantsberg, D.; Mizrachi, Y.; Stern, C.; Polyakov, A.; Teh, W.T. A survey study of endometrial receptivity tests and immunological treatments in in vitro fertilisation (IVF). Aust. N. Zealand J. Obstet. Gynaecol. 2021, 62, 306–311. [Google Scholar] [CrossRef] [PubMed]
- Salamonsen, L.A.; Evans, J.; Nguyen, H.P.; Edgell, T.A. The Microenvironment of Human Implantation: Determinant of Reproductive Success. Am. J. Reprod. Immunol. 2015, 75, 218–225. [Google Scholar] [CrossRef] [PubMed]
- Sternberg, A.; Buck, V.; Classen-Linke, I.; Leube, R. How Mechanical Forces Change the Human Endometrium during the Menstrual Cycle in Preparation for Embryo Implantation. Cells 2021, 10, 2008. [Google Scholar] [CrossRef]
- Emiliani, S.; Delbaere, A.; Devreker, F.; Englert, Y. Embryo–maternal interactive factors regulating the implantation process: Implications in assisted reproductive treatment. Reprod. Biomed. Online 2005, 10, 527–540. [Google Scholar] [CrossRef]
- Ashary, N.; Tiwari, A.; Modi, D. Embryo Implantation: War in Times of Love. Endocrinology 2018, 159, 1188–1198. [Google Scholar] [CrossRef] [PubMed]
- Pantos, K.; Grigoriadis, S.; Maziotis, E.; Pistola, K.; Xystra, P.; Pantou, A.; Kokkali, G.; Pappas, A.; Lambropoulou, M.; Sfakianoudis, K.; et al. The Role of Interleukins in Recurrent Implantation Failure: A Comprehensive Review of the Literature. Int. J. Mol. Sci. 2022, 23, 2198. [Google Scholar] [CrossRef]
- Mao, X.; Wu, L.; Chen, Q.; Kuang, Y.; Zhang, S. Effect of hysteroscopy before starting in-vitro fertilization for women with recurrent implantation failure: A Meta-Analysis and Systematic Review. Medicine 2019, 98, e14075. [Google Scholar] [CrossRef]
- Makrigiannakis, A.; Makrygiannakis, F.; Vrekoussis, T. Approaches to Improve Endometrial Receptivity in Case of Repeated Implantation Failures. Front. Cell Dev. Biol. 2021, 9, 613277. [Google Scholar] [CrossRef]
- Dieamant, F.; Vagnini, L.D.; Petersen, C.G.; Mauri, A.L.; Renzi, A.; Petersen, B.; Mattila, M.C.; Nicoletti, A.; Oliveira, J.B.A.; Baruffi, R.; et al. New therapeutic protocol for improvement of endometrial receptivity (PRIMER) for patients with recurrent implantation failure (RIF)—A pilot study. JBRA Assist. Reprod. 2019, 23, 250–254. [Google Scholar] [CrossRef] [PubMed]
- Mouanness, M.; Ali-Bynom, S.; Jackman, J.; Seckin, S.; Merhi, Z. Use of Intra-uterine Injection of Platelet-rich Plasma (PRP) for Endometrial Receptivity and Thickness: A Literature Review of the Mechanisms of Action. Reprod. Sci. 2021, 28, 1659–1670. [Google Scholar] [CrossRef] [PubMed]
- Altmäe, S.; Koel, M.; Võsa, U.; Adler, P.; Suhorutšenko, M.; Laisk-Podar, T.; Kukushkina, V.; Saare, M.; Velthut-Meikas, A.; Krjutškov, K.; et al. Meta-signature of human endometrial receptivity: A meta-analysis and validation study of transcriptomic biomarkers. Sci. Rep. 2017, 7, 10077. [Google Scholar] [CrossRef] [PubMed]
- Macklon, N. Recurrent implantation failure is a pathology with a specific transcriptomic signature. Fertil. Steril. 2017, 108, 9–14. [Google Scholar] [CrossRef]
- Endometrial Receptivity Array (ERA)|HFEA. Available online: https://www.hfea.gov.uk/treatments/treatment-add-ons/endometrial-receptivity-array-era/ (accessed on 22 March 2022).
- Ben Rafael, Z. Endometrial Receptivity Analysis (ERA) test: An unproven technology. Hum. Reprod. Open 2021, 2021, hoab010. [Google Scholar] [CrossRef]
- Ruiz-Alonso, M.; Valbuena, D.; Gomez, C.; Cuzzi, J.; Simon, C. Endometrial Receptivity Analysis (ERA): Data versus opinions. Hum. Reprod. Open 2021, 2021, hoab011. [Google Scholar] [CrossRef]
- Bolón-Canedo, V.; Alonso-Betanzos, A.; López-De-Ullibarri, I.; Cao, R. Challenges and Future Trends for Microarray Analysis. Methods Mol. Biol. 2019, 1986, 283–293. [Google Scholar] [CrossRef]
- Golub, T.R.; Slonim, D.K.; Tamayo, P.; Huard, C.; Gaasenbeek, M.; Mesirov, J.P.; Coller, H.; Loh, M.L.; Downing, J.R.; Caligiuri, M.A.; et al. Molecular Classification of Cancer: Class Discovery and Class Prediction by Gene Expression Monitoring. Science 1999, 286, 531–537. [Google Scholar] [CrossRef]
- Arango, D.; Laiho, P.; Kokko, A.; Alhopuro, P.; Sammalkorpi, H.; Salovaara, R.; Nicorici, D.; Hautaniemi, S.; Alazzouzi, H.; Mecklin, J.-P.; et al. Gene-Expression Profiling Predicts Recurrence in Dukes’ C Colorectal Cancer. Gastroenterology 2005, 129, 874–884. [Google Scholar] [CrossRef]
- Díaz-Gimeno, P.; Horcajadas, J.A.; Martinez-Conejero, J.A.; Esteban, F.J.; Alama, P.; Pellicer, A.; Simon, C. A genomic diagnostic tool for human endometrial receptivity based on the transcriptomic signature. Fertil. Steril. 2011, 95, 50–60.e15. [Google Scholar] [CrossRef]
- Haouzi, D.; Mahmoud, K.; Fourar, M.; Bendhaou, K.; Dechaud, H.; De Vos, J.; Rème, T.; Dewailly, D.; Hamamah, S. Identification of new biomarkers of human endometrial receptivity in the natural cycle. Hum. Reprod. 2008, 24, 198–205. [Google Scholar] [CrossRef] [PubMed]
- Carson, D.D.; Lagow, E.; Thathiah, A.; Al-Shami, R.; Farach-Carson, M.; Vernon, M.; Yuan, L.; Fritz, M.A.; Lessey, B. Changes in gene expression during the early to mid-luteal (receptive phase) transition in human endometrium detected by high-density microarray screening. Mol. Hum. Reprod. 2002, 8, 871–879. [Google Scholar] [CrossRef] [PubMed]
- Messaoudi, S.; El Kasmi, I.; Bourdiec, A.; Crespo, K.; Bissonnette, L.; Le Saint, C.; Bissonnette, F.; Kadoch, I.-J. 15 years of transcriptomic analysis on endometrial receptivity: What have we learnt? Fertil. Res. Pract. 2019, 5, 9. [Google Scholar] [CrossRef] [PubMed]
- Talbi, S.; Hamilton, A.E.; Vo, K.C.; Tulac, S.; Overgaard, M.T.; Dosiou, C.; Le Shay, N.; Nezhat, C.N.; Kempson, R.; Lessey, B.A.; et al. Molecular Phenotyping of Human Endometrium Distinguishes Menstrual Cycle Phases and Underlying Biological Processes in Normo-Ovulatory Women. Endocrinology 2006, 147, 1097–1121. [Google Scholar] [CrossRef] [PubMed]
- Mirkin, S.; Arslan, M.; Churikov, D.; Corica, A.; Diaz, J.; Williams, S.; Bocca, S.; Oehninger, S. In search of candidate genes critically expressed in the human endometrium during the window of implantation. Hum. Reprod. 2005, 20, 2104–2117. [Google Scholar] [CrossRef]
- Riesewijk, A.; Martín, J.; Van Os, R.; Horcajadas, J.A.; Polman, J.; Pellicer, A.; Mosselman, S.; Simón, C. Gene expression profiling of human endometrial receptivity on days LH+2 versus LH+7 by microarray technology. Mol. Hum. Reprod. 2003, 9, 253–264. [Google Scholar] [CrossRef]
- Haouzi, D.; Assou, S.; Mahmoud, K.; Tondeur, S.; Rème, T.; Hedon, B.; De Vos, J.; Hamamah, S. Gene expression profile of human endometrial receptivity: Comparison between natural and stimulated cycles for the same patients. Hum. Reprod. 2009, 24, 1436–1445. [Google Scholar] [CrossRef]
- Jain, M.; Samokhodskaya, L.; Mladova, E.; Panina, O. Mucosal biomarkers for endometrial receptivity: A promising yet underexplored aspect of reproductive medicine. Syst. Biol. Reprod. Med. 2022, 68, 13–24. [Google Scholar] [CrossRef]
- He, A.; Zou, Y.; Wan, C.; Zhao, J.; Zhang, Q.; Yao, Z.; Tian, F.; Wu, H.; Huang, X.; Fu, J.; et al. The role of transcriptomic biomarkers of endometrial receptivity in personalized embryo transfer for patients with repeated implantation failure. J. Transl. Med. 2021, 19, 176. [Google Scholar] [CrossRef]
- Hamamah, S.; Haouzi, D. Methods for Assessing Endometrium Receptivity of a Patient. 2016. Available online: https://patents.google.com/patent/US9260748B2/en (accessed on 28 March 2022).
- Haouzi, D.; Entezami, F.; Torre, A.; Innocenti, C.; Antoine, Y.; Mauries, C.; Vincens, C.; Bringer-Deutsch, S.; Gala, A.; Ferrieres-Hoa, A.; et al. Customized Frozen Embryo Transfer after Identification of the Receptivity Window with a Transcriptomic Approach Improves the Implantation and Live Birth Rates in Patients with Repeated Implantation Failure. Reprod. Sci. 2020, 28, 69–78. [Google Scholar] [CrossRef]
- Drissennek, L.; Baron, C.; Brouillet, S.; Entezami, F.; Hamamah, S.; Haouzi, D. Endometrial miRNome profile according to the receptivity status and implantation failure. Hum. Fertil. 2020, 25, 356–368. [Google Scholar] [CrossRef] [PubMed]
- Bissonnette, L.; Drissennek, L.; Antoine, Y.; Tiers, L.; Hirtz, C.; Lehmann, S.; Perrochia, H.; Bissonnette, F.; Kadoch, I.-J.; Haouzi, D.; et al. Human S100A10 plays a crucial role in the acquisition of the endometrial receptivity phenotype. Cell Adhes. Migr. 2016, 10, 282–298. [Google Scholar] [CrossRef]
- Bissonnette, L.; Choi, J.; LeSaint, C.; Bissonnette, F.; Kadoch, I. Three Different Endometrial Receptivity Profiles Can Be Defined in Patients with Previous Failed Embryo Transfer; Oxford University Press: Oxford, UK, 2019; Volume 34, pp. 308–309. [Google Scholar]
- Clemente-Ciscar, M.; Ruiz-Alonso, M.; Blesa, D.; Jimenez-Almazan, J.; Bahceci, M.; Banker, M.; Vladimirov, I.; Mackens, S.; Miller, C.; Valbuena, D.; et al. Endometrial Receptivity Analysis (ERA) Using a next Generation Sequencing (NGS) Predictor Improves Reproductive Outcome in Recurrent Implantation Failure (RIF) Patients When Compared to ERA Arrays. In Proceedings of the Human Reproduction and Embryology, Barcelona, Spain, 1–4 July 2018; Oxford University Press: Oxford, UK, 2018; Volume 33, p. 8. [Google Scholar]
- Díaz-Gimeno, P.; Ruiz-Alonso, M.; Blesa, D.; Bosch, N.; Martínez-Conejero, J.A.; Alamá, P.; Garrido, N.; Pellicer, A.; Simón, C. The accuracy and reproducibility of the endometrial receptivity array is superior to histology as a diagnostic method for endometrial receptivity. Fertil. Steril. 2013, 99, 508–517. [Google Scholar] [CrossRef]
- Garrido-Gómez, T.; Ruiz-Alonso, M.; Blesa, D.; Diaz-Gimeno, P.; Vilella, F.; Simón, C. The endometrial receptivity array for diagnosis and personalized embryo transfer as a treatment for patients with repeated implantation failure. Fertil. Steril. 2013, 100, 818–824. [Google Scholar] [CrossRef]
- Simón, C.; Gómez, C.; Cabanillas, S.; Vladimirov, I.; Castillón, G.; Giles, J.; Boynukalin, K.; Findikli, N.; Bahçeci, M.; Ortega, I.; et al. A 5-year multicentre randomized controlled trial comparing personalized, frozen and fresh blastocyst transfer in IVF. Reprod. Biomed. Online 2020, 41, 402–415. [Google Scholar] [CrossRef]
- Alonso, M.R.; Díaz-Gimeno, P.; Gómez, E.; Rincón-Bertolín, A.; Vladimirov, Y.; Garrido, N.; Simón, C. Clinical efficiency of embryo transfer performed in receptive vs non-receptive endometrium diagnosed by the endometrial receptivity array (era) test. Fertil. Steril. 2014, 102, e292. [Google Scholar] [CrossRef]
- Mahajan, N. Endometrial receptivity array: Clinical application. J. Hum. Reprod. Sci. 2015, 8, 121–129. [Google Scholar] [CrossRef]
- Hashimoto, T.; Koizumi, M.; Doshida, M.; Toya, M.; Sagara, E.; Oka, N.; Nakajo, Y.; Aono, N.; Igarashi, H.; Kyono, K. Efficacy of the endometrial receptivity array for repeated implantation failure in Japan: A retrospective, two-centers study. Reprod. Med. Biol. 2017, 16, 290–296. [Google Scholar] [CrossRef]
- Tan, J.; Kan, A.; Hitkari, J.; Taylor, B.; Tallon, N.; Warraich, G.; Yuzpe, A.; Nakhuda, G. The role of the endometrial receptivity array (ERA) in patients who have failed euploid embryo transfers. J. Assist. Reprod. Genet. 2018, 35, 683–692. [Google Scholar] [CrossRef]
- Bassil, R.; Casper, R.; Samara, N.; Hsieh, T.-B.; Barzilay, E.; Orvieto, R.; Haas, J. Does the endometrial receptivity array really provide personalized embryo transfer? J. Assist. Reprod. Genet. 2018, 35, 1301–1305. [Google Scholar] [CrossRef]
- Neves, A.R.; Devesa, M.; Martínez, F.; Garcia-Martinez, S.; Rodriguez, I.; Polyzos, N.P.; Coroleu, B. What is the clinical impact of the endometrial receptivity array in PGT-A and oocyte donation cycles? J. Assist. Reprod. Genet. 2019, 36, 1901–1908. [Google Scholar] [CrossRef] [PubMed]
- Patel, J.A.; Patel, A.J.; Banker, J.M.; Shah, S.I.; Banker, M.R. Personalized embryo transfer helps in improving In vitro fertilization/ICSI outcomes in patients with recurrent implantation failure. J. Hum. Reprod. Sci. 2019, 12, 59–66. [Google Scholar] [CrossRef] [PubMed]
- Cohen, A.M.; Ye, X.Y.; Colgan, T.J.; Greenblatt, E.M.; Chan, C. Comparing endometrial receptivity array to histologic dating of the endometrium in women with a history of implantation failure. Syst. Biol. Reprod. Med. 2020, 66, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Cozzolino, M.; Diaz-Gimeno, P.; Pellicer, A.; Garrido, N. Evaluation of the endometrial receptivity assay and the preimplantation genetic test for aneuploidy in overcoming recurrent implantation failure. J. Assist. Reprod. Genet. 2020, 37, 2989–2997. [Google Scholar] [CrossRef]
- Barrenetxea, G.; Romero, I.; Celis, R.; Abio, A.; Bilbao, M. Correlation between plasmatic progesterone, endometrial receptivity genetic assay and implantation rates in frozen-thawed transferred euploid embryos. A multivariate analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2021, 263, 192–197. [Google Scholar] [CrossRef]
- Fodina, V.; Dudorova, A.; Erenpreiss, J. Evaluation of embryo aneuploidy (PGT-A) and endometrial receptivity (ERA) testing in patients with recurrent implantation failure in ICSI cycles. Gynecol. Endocrinol. 2021, 37, 17–20. [Google Scholar] [CrossRef]
- Eisman, L.E.; Pisarska, M.D.; Wertheimer, S.; Chan, J.L.; Akopians, A.L.; Surrey, M.W.; Danzer, H.C.; Ghadir, S.; Chang, W.Y.; Alexander, C.J.; et al. Clinical utility of the endometrial receptivity analysis in women with prior failed transfers. J. Assist. Reprod. Genet. 2021, 38, 645–650. [Google Scholar] [CrossRef]
- Riestenberg, C.; Kroener, L.; Quinn, M.; Ching, K.; Ambartsumyan, G. Routine endometrial receptivity array in first embryo transfer cycles does not improve live birth rate. Fertil. Steril. 2021, 115, 1001–1006. [Google Scholar] [CrossRef]
- Jia, Y.; Dong, Y.; Sha, Y.; Cai, S.; Diao, L.; Qiu, Z.; Guo, Y.; Huang, Y.; Ye, H.; Liu, S. Effectiveness comparison between endometrial receptivity array, immune profiling and the combination in treating patients with multiple implantation failure. Am. J. Reprod. Immunol. 2021, 87, e13513. [Google Scholar] [CrossRef]
- Horcajadas Almansa, J.; Enciso, M.; Sarasa, J.; Carrascosa, J.; Martinez-Ortiz, P.; Aizpurua, J.; Munne, S. ER Map: A New Comprehensive and Reliable Endometrial Receptivity Test; Oxford University Press: Oxford, UK, 2016; Volume 31, pp. 49–50. [Google Scholar]
- Horcajadas, J.; Enciso, M.; Sarasa, J.; Carrascosa, J.; Martinez, P.; Aizpurua, J.; Munne, S. ER Map allow the reliable determination of the window of implantation in infertile women. Fertil. Steril. 2016, 106, e216. [Google Scholar] [CrossRef][Green Version]
- Enciso, M.; Carrascosa, J.P.; Sarasa, J.; Martínez-Ortiz, P.A.; Munné, S.; Horcajadas, J.A.; Aizpurua, J. Development of a new comprehensive and reliable endometrial receptivity map (ER Map/ER Grade) based on RT-qPCR gene expression analysis. Hum. Reprod. 2018, 33, 220–228. [Google Scholar] [CrossRef] [PubMed]
- Enciso, M.; Aizpurua, J.; Rodríguez-Estrada, B.; Jurado, I.; Ferrández-Rives, M.; Rodríguez, E.; Pérez-Larrea, E.; Climent, A.B.; Marron, K.; Sarasa, J. The precise determination of the window of implantation significantly improves ART outcomes. Sci. Rep. 2021, 11, 13420. [Google Scholar] [CrossRef] [PubMed]
- Saare, M.; Laisk, T.; Teder, H.; Paluoja, P.; Palta, P.; Koel, M.; Kirss, F.; Karro, H.; Sõritsa, D.; Salumets, A.; et al. A molecular tool for menstrual cycle phase dating of endometrial samples in endometriosis transcriptome studies. Biol. Reprod. 2019, 101, 1–3. [Google Scholar] [CrossRef]
- Teder, H.; Koel, M.; Paluoja, P.; Jatsenko, T.; Rekker, K.; Laisk-Podar, T.; Kukuškina, V.; Velthut-Meikas, A.; Fjodorova, O.; Peters, M.; et al. TAC-seq: Targeted DNA and RNA sequencing for precise biomarker molecule counting. npj Genom. Med. 2018, 3, 34. [Google Scholar] [CrossRef]
- Saxtorph, M.H.; Persson, G.; Hallager, T.; Petersen, K.B.; Eriksen, J.O.; Larsen, L.G.; Macklon, N.; Hviid, T.V.F. Are different markers of endometrial receptivity telling us different things about endometrial function? Am. J. Reprod. Immunol. 2020, 84, e13323. [Google Scholar] [CrossRef]
- Giacomini, E.; Scotti, G.M.; Vanni, V.S.; Lazarevic, D.; Makieva, S.; Privitera, L.; Signorelli, S.; Cantone, L.; Bollati, V.; Murdica, V.; et al. Global transcriptomic changes occur in uterine fluid-derived extracellular vesicles during the endometrial window for embryo implantation. Hum. Reprod. 2021, 36, 2249–2274. [Google Scholar] [CrossRef]
- Kasvandik, S.; Saarma, M.; Kaart, T.; Rooda, I.; Velthut-Meikas, A.; Ehrenberg, A.; Gemzell, K.; Lalitkumar, P.G.; Salumets, A.; Peters, M. Uterine Fluid Proteins for Minimally Invasive Assessment of Endometrial Receptivity. J. Clin. Endocrinol. Metab. 2019, 105, 219–230. [Google Scholar] [CrossRef]
- von Grothusen, C.; Frisendahl, C.; Modhukur, V.; Lalitkumar, P.G.; Peters, M.; Faridani, O.R.; Salumets, A.; Boggavarapu, N.R.; Gemzell-Danielsson, K. Uterine fluid microRNAs are dysregulated in women with recurrent implantation failure. Hum. Reprod. 2022, 37, 734–746. [Google Scholar] [CrossRef]
- Basatvat, S.; Russell, J.M.; Saare, M.; Thurston, L.M.; Salumets, A.; Fazeli, A. Potential innate immunity-related markers of endometrial receptivity and recurrent implantation failure (RIF). Reprod. Biol. 2021, 21, 100569. [Google Scholar] [CrossRef]
- Tan, X.; Ding, J.; Pu, D.; Wu, J. Anti-phospholipid antibody may reduce endometrial receptivity during the window of embryo implantation. J. Gynecol. Obstet. Hum. Reprod. 2020, 50, 101912. [Google Scholar] [CrossRef]
- Quinn, K.E.; Matson, B.C.; Wetendorf, M.; Caron, K.M. Pinopodes: Recent advancements, current perspectives, and future directions. Mol. Cell. Endocrinol. 2019, 501, 110644. [Google Scholar] [CrossRef] [PubMed]
- Xue, P.; Zhou, W.; Fan, W.; Jiang, J.; Kong, C.; Zhou, W.; Zhou, J.; Huang, X.; Yang, H.; Han, Q.; et al. Increased METTL3-mediated m6A methylation inhibits embryo implantation by repressing HOXA10 expression in recurrent implantation failure. Reprod. Biol. Endocrinol. 2021, 19, 187. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Han, M.; Zhou, M.; Liu, M.; Li, Y.; Xu, B.; Zhang, A. Down-regulation of S100P induces apoptosis in endometrial epithelial cell during GnRH antagonist protocol. Reprod. Biol. Endocrinol. 2021, 19, 99. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; He, D.; Zeng, H.; Luo, J.; Yang, S.; Chen, J.; Abdullah, R.K.; Liu, N. Expression and significance of miR-30d-5p and SOCS1 in patients with recurrent implantation failure during implantation window. Reprod. Biol. Endocrinol. 2021, 19, 138. [Google Scholar] [CrossRef]
- Zhao, F.; Guo, Y.; Shi, Z.; Wu, M.; Lv, Y.; Song, W. hsa_circ_001946 elevates HOXA10 expression and promotes the development of endometrial receptivity via sponging miR-135b. Diagn. Pathol. 2021, 16, 44. [Google Scholar] [CrossRef]
- Diaz-Gimeno, P.; Sebastian-Leon, P.; Sanchez-Reyes, J.M.; Spath, K.; Aleman, A.; Vidal, C.; Devesa-Peiro, A.; Labarta, E.; Sánchez-Ribas, I.; Ferrando, M.; et al. Identifying and optimizing human endometrial gene expression signatures for endometrial dating. Hum. Reprod. 2021, 37, 284–296. [Google Scholar] [CrossRef]
- Bashiri, A.; Halper, K.I.; Orvieto, R. Recurrent Implantation Failure-update overview on etiology, diagnosis, treatment and future directions. Reprod. Biol. Endocrinol. 2018, 16, 121. [Google Scholar] [CrossRef]
- Ata, B.; Kalafat, E.; Somigliana, E. A new definition of recurrent implantation failure on the basis of anticipated blastocyst aneuploidy rates across female age. Fertil. Steril. 2021, 116, 1320–1327. [Google Scholar] [CrossRef]
- Bai, X.; Zheng, L.; Li, D.; Xu, Y. Research progress of endometrial receptivity in patients with polycystic ovary syndrome: A systematic review. Reprod. Biol. Endocrinol. 2021, 19, 122. [Google Scholar] [CrossRef]
- Zhao, J.; Chen, Q.; Xue, X. An Update on the Progress of Endometrial Receptivity in Women with Polycystic Ovary Syndrome. Reprod. Sci. 2021, 29, 2136–2144. [Google Scholar] [CrossRef]
| Study | pET RIF | pET Without RIF | RIF (Control) | Without RIF (Control) | Outcome | Study Design |
|---|---|---|---|---|---|---|
| Ruiz-Alonso, 2013 [48] | 9/16 | 6/8 | N/A | N/A | Clinical pregnancy | Prospective multicenter |
| Ruiz-Alonso, 2014 [50] | 123/205 | N/A | 12/52 | N/A | Clinical pregnancy 1 | Retrospective |
| 91/205 | N/A | 0/52 | N/A | Ongoing pregnancy 1 | ||
| Mahajan, 2015 [51] | 28/66 | 38/66 | N/A | N/A | Clinical pregnancy | Retrospective |
| Hashimoto, 2017 [52] | 25/44 | N/A | N/A | N/A | Clinical pregnancy | Retrospective |
| Tan, 2018 [53] | N/A | 36/71 | N/A | N/A | Ongoing Pregnancy 2 | Retrospective |
| Bassil, 2018 [54] | N/A | 16/53 | N/A | 177/503 | Ongoing pregnancy | Retrospective |
| Neves, 2019 [55] | N/A | 14/24 | N/A | 84/119 | Clinical pregnancy 3 | Retrospective |
| N/A | 11/32 | N/A | 103/158 | Clinical pregnancy 4 | ||
| Patel, 2019 [56] | 116/220 | N/A | N/A | N/A | Clinical pregnancy | Retrospective |
| Simon, 2020 [49] | N/A | 58/80 | N/A | 50/92 | Clinical pregnancy | RCT |
| N/A | 45/80 | N/A | 39/92 | Live birth | ||
| Cohen, 2020 [57] | 21/93 | N/A | N/A | N/A | Clinical pregnancy | Retrospective |
| 3/93 | N/A | N/A | N/A | Live birth | ||
| Cozzolino, 2020 [58] | 72/195 | N/A | 1147/3227 | N/A | Ongoing pregnancy 5,7 | Retrospective |
| 9/27 | N/A | 110/255 | N/A | Ongoing pregnancy 6,7 | ||
| Barrenetxa, 2021 [59] | N/A | 58/85 | N/A | N/A | Clinical pregnancy | Retrospective |
| Fodina, 2021 [60] | 8/22 | N/A | 32/72 | N/A | Clinical pregnancy 5 | Retrospective |
| 40/72 | N/A | 43/87 | N/A | Clinical pregnancy 6 | ||
| Eisman 2021 [61] | 13/28 | 189/280 | N/A | N/A | Clinical pregnancy | Retrospective |
| 6/26 | 137/280 | N/A | N/A | Ongoing Pregnancy | ||
| Riestenberg 2021 [62] | N/A | 99/147 | N/A | 53/81 | Clinical pregnancy | Prospective single-center |
| N/A | 83/147 | N/A | 45/81 | Live birth | ||
| Jia 2022 [63] | N/A | 15/28 | N/A | 19/51 | Clinical pregnancy | Retrospective |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maziotis, E.; Kalampokas, T.; Giannelou, P.; Grigoriadis, S.; Rapani, A.; Anifantakis, M.; Kotsifaki, A.; Pantou, A.; Triantafyllidou, O.; Tzanakaki, D.; et al. Commercially Available Molecular Approaches to Evaluate Endometrial Receptivity: A Systematic Review and Critical Analysis of the Literature. Diagnostics 2022, 12, 2611. https://doi.org/10.3390/diagnostics12112611
Maziotis E, Kalampokas T, Giannelou P, Grigoriadis S, Rapani A, Anifantakis M, Kotsifaki A, Pantou A, Triantafyllidou O, Tzanakaki D, et al. Commercially Available Molecular Approaches to Evaluate Endometrial Receptivity: A Systematic Review and Critical Analysis of the Literature. Diagnostics. 2022; 12(11):2611. https://doi.org/10.3390/diagnostics12112611
Chicago/Turabian StyleMaziotis, Evangelos, Theodoros Kalampokas, Polina Giannelou, Sokratis Grigoriadis, Anna Rapani, Marios Anifantakis, Amalia Kotsifaki, Agni Pantou, Olga Triantafyllidou, Despoina Tzanakaki, and et al. 2022. "Commercially Available Molecular Approaches to Evaluate Endometrial Receptivity: A Systematic Review and Critical Analysis of the Literature" Diagnostics 12, no. 11: 2611. https://doi.org/10.3390/diagnostics12112611
APA StyleMaziotis, E., Kalampokas, T., Giannelou, P., Grigoriadis, S., Rapani, A., Anifantakis, M., Kotsifaki, A., Pantou, A., Triantafyllidou, O., Tzanakaki, D., Neofytou, S., Vogiatzi, P., Bakas, P., Simopoulou, M., & Vlahos, N. (2022). Commercially Available Molecular Approaches to Evaluate Endometrial Receptivity: A Systematic Review and Critical Analysis of the Literature. Diagnostics, 12(11), 2611. https://doi.org/10.3390/diagnostics12112611










