Development and Validation of a Smartphone Application for Telenutrition in Patients with Inflammatory Bowel Disease
Abstract
1. Introduction
2. Materials and Methods
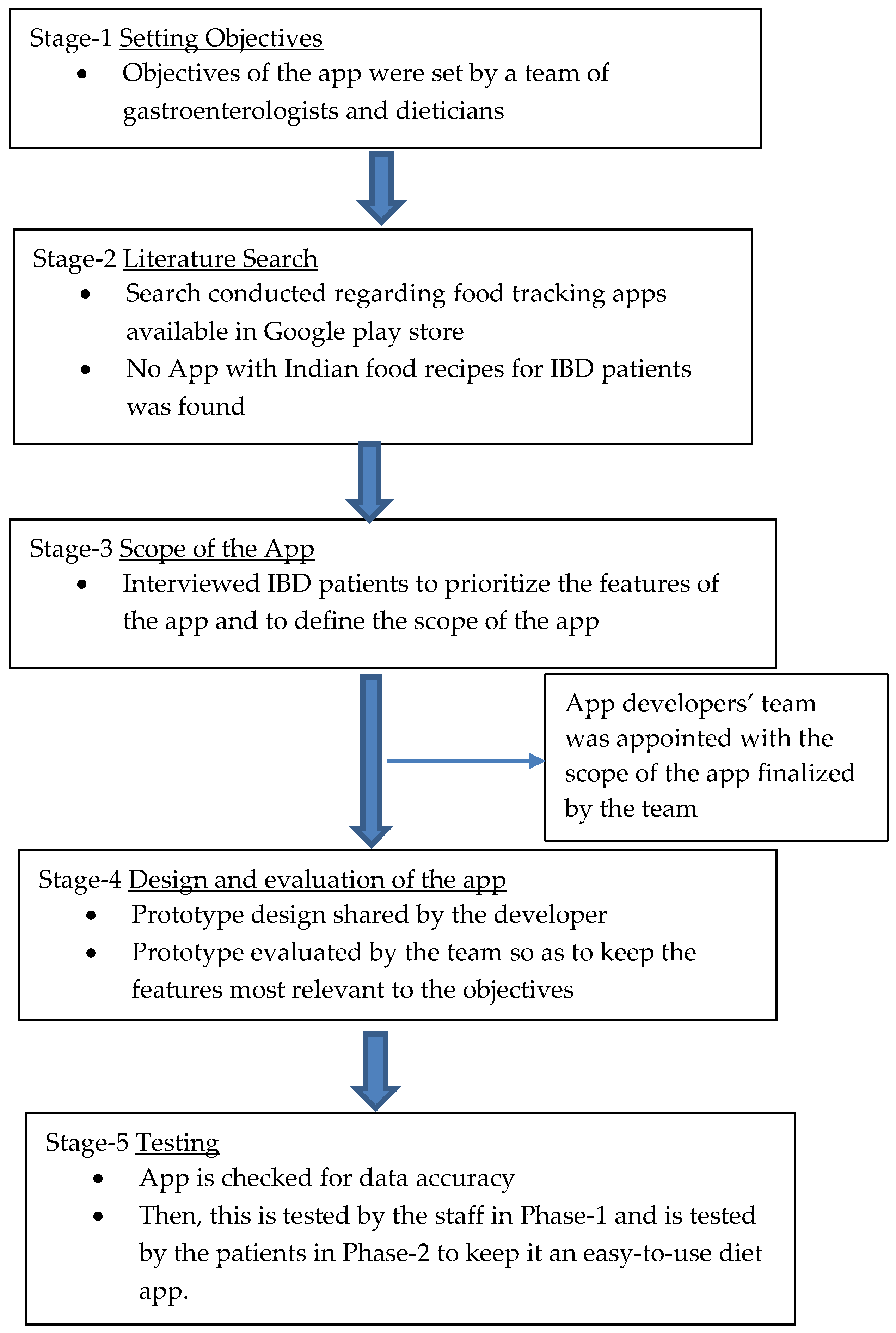
2.1. Development of the Smartphone Application (App)
2.2. App Validation
2.3. Data Pre-Processing
2.4. Data Analysis
3. Results
3.1. IBD NutriCare Mobile App
3.1.1. IBD NutriCare Mobile App—For the Patients
3.1.2. IBD NutriCare Mobile App—For the Researchers
3.2. App Validation Study
3.2.1. Baseline Characteristics
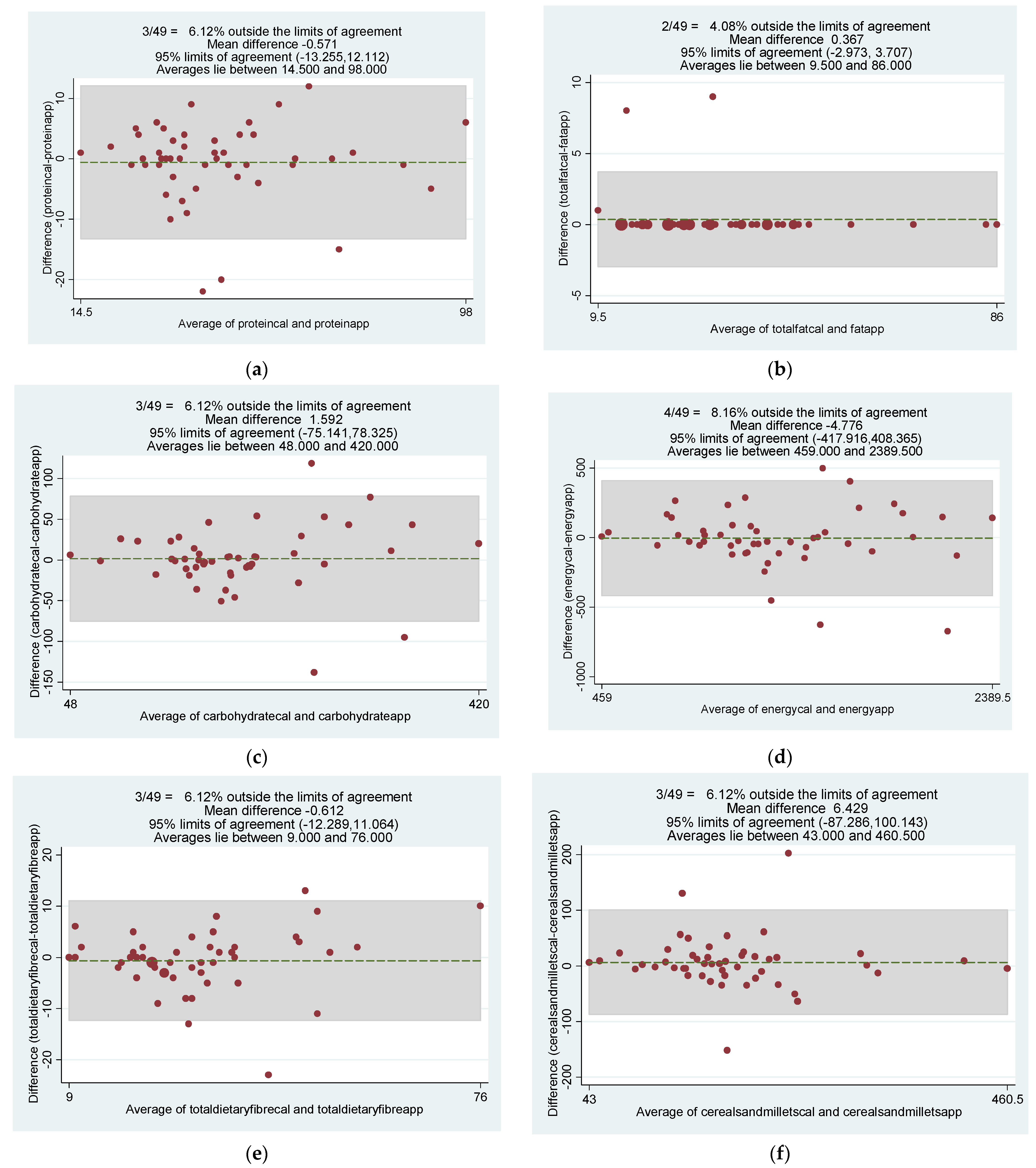
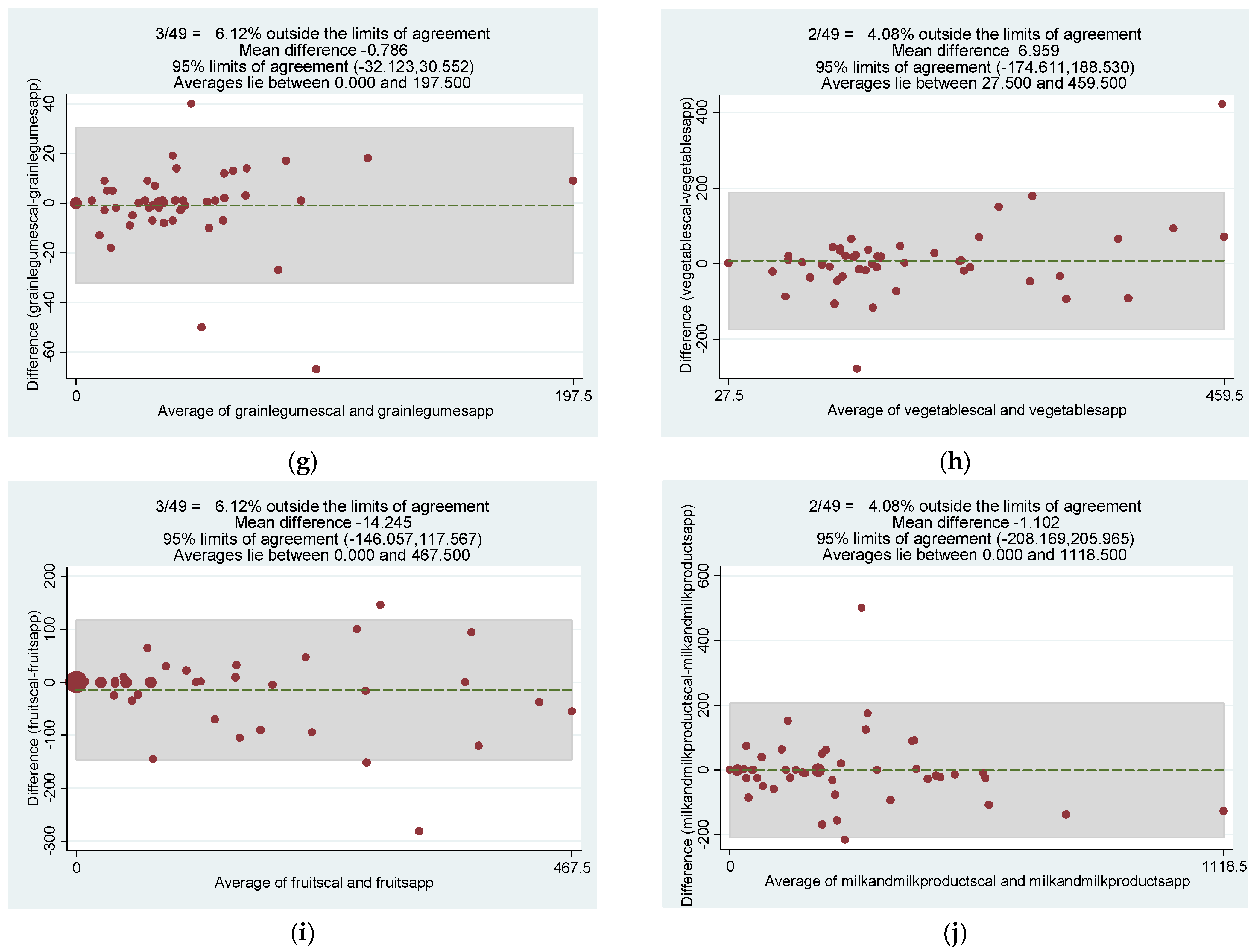
3.2.2. Diet App Based vs. 24-hr Diet Recall Assessment
3.2.3. Acceptability of the App
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kedia, S.; Ahuja, V. Is the emergence of inflammatory bowel disease a prime example of “the third epidemiological transition”? Indian J. Gastroenterol. 2018, 37, 183–185. [Google Scholar] [CrossRef]
- Singh, P.; Ananthakrishnan, A.; Ahuja, V. Pivot to Asia: Inflammatory bowel disease burden. Intest. Res. 2017, 15, 138. [Google Scholar] [CrossRef] [PubMed]
- Mak, W.Y.; Zhao, M.; Ng, S.C.; Burisch, J. The epidemiology of inflammatory bowel disease: East meets west. J. Gastroenterol. Hepatol. 2020, 35, 380–389. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, G.G.; Windsor, J.W. The four epidemiological stages in the global evolution of inflammatory bowel disease. Nat. Rev. Gastroenterol. Hepatol. 2021, 18, 56–66. [Google Scholar] [CrossRef]
- Park, J.; Cheon, J.H. Incidence and Prevalence of Inflammatory Bowel Disease across Asia. Yonsei Med. J. 2021, 62, 99–108. [Google Scholar] [CrossRef]
- Kedia, S.; Ahuja, V. Epidemiology of Inflammatory Bowel Disease in India: The Great Shift East. Inflamm. Intest. Dis. 2017, 2, 102–115. [Google Scholar] [CrossRef] [PubMed]
- Levine, A.; Boneh, R.S.; Wine, E. Evolving role of diet in the pathogenesis and treatment of inflammatory bowel diseases. Gut 2018, 67, 1726–1738. [Google Scholar] [CrossRef]
- Ananthakrishnan, A.N. Impact of Diet on Risk of IBD. Crohn’s Colitis 360 2020, 2, otz054. [Google Scholar] [CrossRef]
- Serrano-Moreno, C.; Brox-Torrecilla, N.; Arhip, L.; Romero, I.; Morales, Á.; Carrascal, M.L.; Cuerda, C.; Motilla, M.; Camblor, M.; Velasco, C.; et al. Diets for inflammatory bowel disease: What do we know so far? Eur. J. Clin. Nutr. 2022, 76, 1222–1233. [Google Scholar] [CrossRef]
- Fitzpatrick, J.A.; Melton, S.L.; Yao, C.K.; Gibson, P.R.; Halmos, E.P. Dietary management of adults with IBD—The emerging role of dietary therapy. Nat. Rev. Gastroenterol. Hepatol. 2022, 19(10), 652–669. [Google Scholar] [CrossRef]
- Roncoroni, L.; Gori, R.; Elli, L.; Tontini, G.E.; Doneda, L.; Norsa, L.; Cuomo, M.; Lombardo, V.; Scricciolo, A.; Caprioli, F.; et al. Nutrition in Patients with Inflammatory Bowel Diseases: A Narrative Review. Nutrients 2022, 14, 751. [Google Scholar] [CrossRef] [PubMed]
- Levine, A.; Rhodes, J.M.; Lindsay, J.O.; Abreu, M.T.; Kamm, M.A.; Gibson, P.R.; Gasche, C.; Silverberg, M.S.; Mahadevan, U.; Boneh, R.S.; et al. Dietary Guidance From the International Organization for the Study of In-flammatory Bowel Diseases. Clin. Gastroenterol. Hepatol. 2020, 18, 1381–1392. [Google Scholar] [CrossRef] [PubMed]
- Shafiee, N.H.; Manaf, Z.A.; Mokhtar, N.M.; Ali, R.A. Anti-inflammatory diet and inflammatory bowel disease: What clinicians and patients should know? Intest. Res. 2021, 19, 171. [Google Scholar] [CrossRef] [PubMed]
- Carter, M.C.; Burley, V.J.; Nykjaer, C.; Cade, J.E. ‘My Meal Mate’ (MMM): Validation of the diet measures captured on a smartphone application to facilitate weight loss. Br. J. Nutr. 2013, 109, 539–546. [Google Scholar] [CrossRef]
- India to Have 1 bn Smartphone Users by 2026: Deloitte Study. Available online: https://www.businesstoday.in/technology/story/india-to-have-1-bn-smartphone-users-by-2026-deloitte-study-323519-2022-02-22 (accessed on 8 May 2022).
- Elamin, S.; Cohen, J. Telenutrition for Inflammatory Bowel Disease: A Tipping Point for Dietary Wellness. Crohn’s Colitis 360 2021, 3, otab017. [Google Scholar] [CrossRef]
- de Jong, M.; van der Meulen-de Jong, A.; Romberg-Camps, M.; Degens, J.; Becx, M.; Markus, T.; Tomlow, H.; Cilissen, M.; Ipenburg, N.; Verwey, M.; et al. Development and feasibility study of a telemedicine tool for all patients with IBD: MyIBD-coach. Inflamm. Bowel Dis. 2017, 23, 485–493. [Google Scholar] [CrossRef]
- Bosworth, T.; Kling, J. AGA Tech Summit Telemedicine Proving to Be an Efficient Platform for Delivering Nutritional Services; MDedge News: Parsippany, NJ, USA, 2019. [Google Scholar]
- Walmsley, R.S.; Ayres, R.C.S.; Pounder, R.E.; Allan, R.N. A simple clinical colitis activity index. Gut 1998, 43, 29–32. [Google Scholar] [CrossRef]
- Harvey, R.F.; Bradshaw, J.M. A simple index of crohn’s-disease activity. Lancet 1980, 1, 514. [Google Scholar] [CrossRef]
- Klein, S. A primer of nutritional support for gastroenterologists. Gastroenterology 2002, 122, 1677–1687. [Google Scholar] [CrossRef]
- Cross, R.K.; Cheevers, N.; Finkelstein, J. Home telemanagement for patients with ulcerative colitis (UC HAT). Dig. Dis. Sci. 2009, 54, 2463–2472. [Google Scholar] [CrossRef]
- Yin, A.L.; Hachuel, D.; Pollak, J.P.; Scherl, E.J.; Estrin, D. Digital Health Apps in the Clinical Care of Inflammatory Bowel Disease: Scoping Review. J. Med. Internet Res. 2019, 21, e14630. [Google Scholar] [CrossRef] [PubMed]
- Ambrosini, G.L.; Hurworth, M.; Giglia, R.; Trapp, G.; Strauss, P. Feasibility of a commercial smartphone application for dietary assessment in epidemiological research and comparison with 24-h dietary recalls. Nutr. J. 2018, 17, 5. [Google Scholar] [CrossRef] [PubMed]
- Sood, A.; Ahuja, V.; Kedia, S.; Midha, V.; Mahajan, R.; Mehta, V.; Sudhakar, R.; Singh, A.; Kumar, A.; Puri, A.S.; et al. Diet and inflammatory bowel disease: The Asian Working Group guidelines. Indian J. Gastroenterol. 2019, 38, 220–246. [Google Scholar] [CrossRef] [PubMed]
- Shoda, R.; Matsueda, K.; Yamato, S.; Umeda, N. Epidemiologic analysis of Crohn disease in Japan: Increased dietary intake of n-6 polyunsaturated fatty acids and animal protein relates to the increased incidence of Crohn disease in Japan. Am. J. Clin. Nutr. 1996, 63, 741–745. [Google Scholar] [CrossRef] [PubMed]
- Wellard-Cole, L.; Chen, J.; Davies, A.; Wong, A.; Huynh, S.; Rangan, A.; Allman-Farinelli, M. Relative Validity of the Eat and Track (EaT) Smartphone App for Collection of Dietary Intake Data in 18-to-30-Year Olds. Nutrients 2019, 11, 621. [Google Scholar] [CrossRef]
- Rollo, M.E.; Ash, S.; Lyons-Wall, P.; Russell, A.W. Evaluation of a Mobile Phone Image-Based Dietary Assessment Method in Adults with Type 2 Diabetes. Nutrients 2015, 7, 4897–4910. [Google Scholar] [CrossRef]
- Sharp, D.B.; Allman-Farinelli, M. Feasibility and validity of mobile phones to assess dietary intake. Nutrition 2014, 30, 1257–1266. [Google Scholar] [CrossRef]
- Sahu, P.; Kedia, S.; Ahuja, V.; Tandon, R.K. Diet and nutrition in the management of inflammatory bowel disease. Indian J. Gastroenterol. 2021, 40, 253–264. [Google Scholar] [CrossRef]
- Available online: https://economictimes.indiatimes.com/nri/migrate/at-18-million-india-has-the-worlds-largest-diaspora-population/articleshow/80290768.cms (accessed on 5 May 2022).

| Parameter | Result n (%) |
|---|---|
| Mean Age at onset (years, SD) | 32.4 ±11.2 |
| Gender | |
| Male | 37 (75.5%) |
| Female | 12 (24.5%) |
| Mean Height (m) | |
| Male | 1.69 ± 0.07 |
| Female | 1.62 ± 0.06 |
| Mean Weight (kg) | |
| Male | 60.5 ± 11.1 |
| Female | 50.1 ± 8.7 |
| Mean BMI (kg/m2) | |
| Male | 21 ± 3.6 |
| Female | 19.5 ± 2.6 |
| BMI (n) | |
| <18 (Undernourished) | 16 (32.6%) |
| ≥18 to ≤22.9 (Normal) | 18 (36.7%) |
| ≥23 to ≤24.9 (Overweight) | 10 (20.4%) |
| ≥25 (Obese) | 5 (10.2%) |
| Disease Type | |
| Ulcerative Colitis Crohn’s disease IBD-U | 38 (77.6%) 6 (12.2%) 5 (10.2%) |
| Mean number of data entry days by patients using the app in 4 weeks | 15.7 days |
| Variable | 24 Hr Recall Mean ± SD (N = 49) | IBD NutriCare Mean ± SD (N = 49) | Difference in Mean ± SD | Intraclass Correlation Coefficient |
|---|---|---|---|---|
| Protein (g) | 44.2 ± 17.9 | 44.7 ± 17.9 | −0.57 ± 6.47 | 0.93 * |
| Fat (g) | 32 ± 16.59 | 32 ± 16.80 | 0.37 ± 1.7 | 0.99 * |
| Carbohydrate (g) | 204 ± 83.33 | 203 ± 86.62 | 1.59 ± 39.15 | 0.93 * |
| Energy (kcal) | 1318 ± 447.53 | 1323 ± 463.62 | −4.81 ± 210.78 | 0.94 * |
| Fiber (g) | 29 ± 13.82 | 30 ± 12.94 | 0.61 ± 5.95 | 0.94 * |
| Cereals and millets (g) | 188 ± 82.77 | 182 ± 85.59 | 6.42 ± 47.81 | 0.91 * |
| Grains and Legumes (g) | 42.90 ± 34.58 | 43.65 ± 34.44 | −0.78 ± 15.98 | 0.94 * |
| Vegetables (g) | 190.27 ± 128.25 | 183.39 ± 92.48 | 6.88 ± 92.55 | 0.79 * |
| Fruits (g) | 114.43 ± 129.55 | 128.70 ± 143.02 | −14.27 ± 67.27 | 0.93 * |
| Milk (g) | 257.59 ± 217.02 | 258.67 ± 233.73 | −1.09 ± 105.58 | 0.94 * |
| Sl. No. | Statement (n = Number of Responders) | Agree/Strongly Agree n (%) | Undecided n (%) | Disagree/Strongly Disagree n (%) |
|---|---|---|---|---|
| 1 | Have you used any previous apps before? (n = 49) | 44 (90) | 0 | 5 (10) |
| 2 | Was the learning process regarding app usage easy? (n = 49) | 45 (92) | 3 (6) | 1(2) |
| 3 | Did you find the app convenient? (n = 49) | 47 (96) | 2 (4) | 0 |
| 4 | Were the food items easily identifiable in the app? (n = 49) | 40 (82) | 4 (8) | 5(10) |
| 5 | Was the app accurate? (n = 49) | 42 (86) | 6 (12) | 1(2) |
| 6 | Easy to estimate portion size (n = 49) | 42 (86) | 3 (6) | 4 (8) |
| Sl. No | Comparing two methods (n = 49) | App | 24-h recall | Undecided |
| 1 | Preferred Method | 44 (90) | 5(10) | 0 |
| 2 | More convenient method | 42 (86) | 5 (10) | 2 (4) |
| 3 | Found Easier to complete | 43 (88) | 4 (8) | 2 (4) |
| 4 | More accurate | 40 (82) | 5 (10) | 4 (8) |
| 5 | Less time consuming | 46 (94) | 3 (6) | 0 |
| 6 | Easy to remember | 44(90) | 4 (8) | 1 (2) |
| 7 | Disease awareness | 42 (86) | 5 (10) | 2 (4) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gupta, A.; Singh, N.; Madan, D.; Farooqui, M.; Singh, N.; Thomas, D.M.; Kante, B.; Singh, M.; Virmani, S.; Verma, M.; et al. Development and Validation of a Smartphone Application for Telenutrition in Patients with Inflammatory Bowel Disease. Diagnostics 2022, 12, 2482. https://doi.org/10.3390/diagnostics12102482
Gupta A, Singh N, Madan D, Farooqui M, Singh N, Thomas DM, Kante B, Singh M, Virmani S, Verma M, et al. Development and Validation of a Smartphone Application for Telenutrition in Patients with Inflammatory Bowel Disease. Diagnostics. 2022; 12(10):2482. https://doi.org/10.3390/diagnostics12102482
Chicago/Turabian StyleGupta, Arti, Namrata Singh, Divya Madan, Mariyam Farooqui, Neha Singh, David Mathew Thomas, Bhaskar Kante, Mukesh Singh, Shubi Virmani, Mehak Verma, and et al. 2022. "Development and Validation of a Smartphone Application for Telenutrition in Patients with Inflammatory Bowel Disease" Diagnostics 12, no. 10: 2482. https://doi.org/10.3390/diagnostics12102482
APA StyleGupta, A., Singh, N., Madan, D., Farooqui, M., Singh, N., Thomas, D. M., Kante, B., Singh, M., Virmani, S., Verma, M., Bajaj, A., Markandey, M., Kumar, P., Vuyyuru, S. K., Sahu, P., Monga, N., Makharia, G., Kedia, S., & Ahuja, V. (2022). Development and Validation of a Smartphone Application for Telenutrition in Patients with Inflammatory Bowel Disease. Diagnostics, 12(10), 2482. https://doi.org/10.3390/diagnostics12102482






