Clinical Evaluation of a New Electronic Periodontal Probe: A Randomized Controlled Clinical Trial
Abstract
:1. Introduction
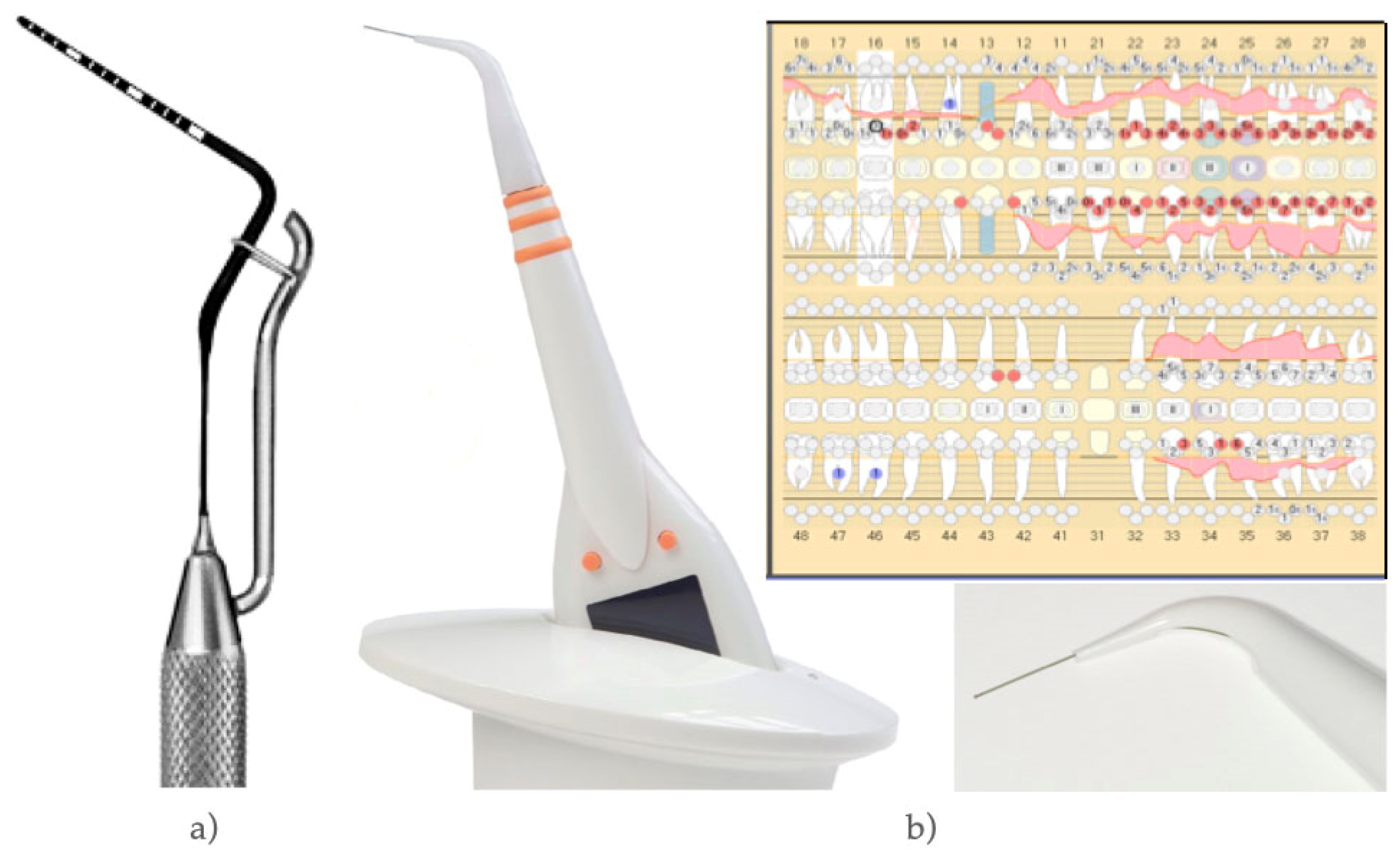
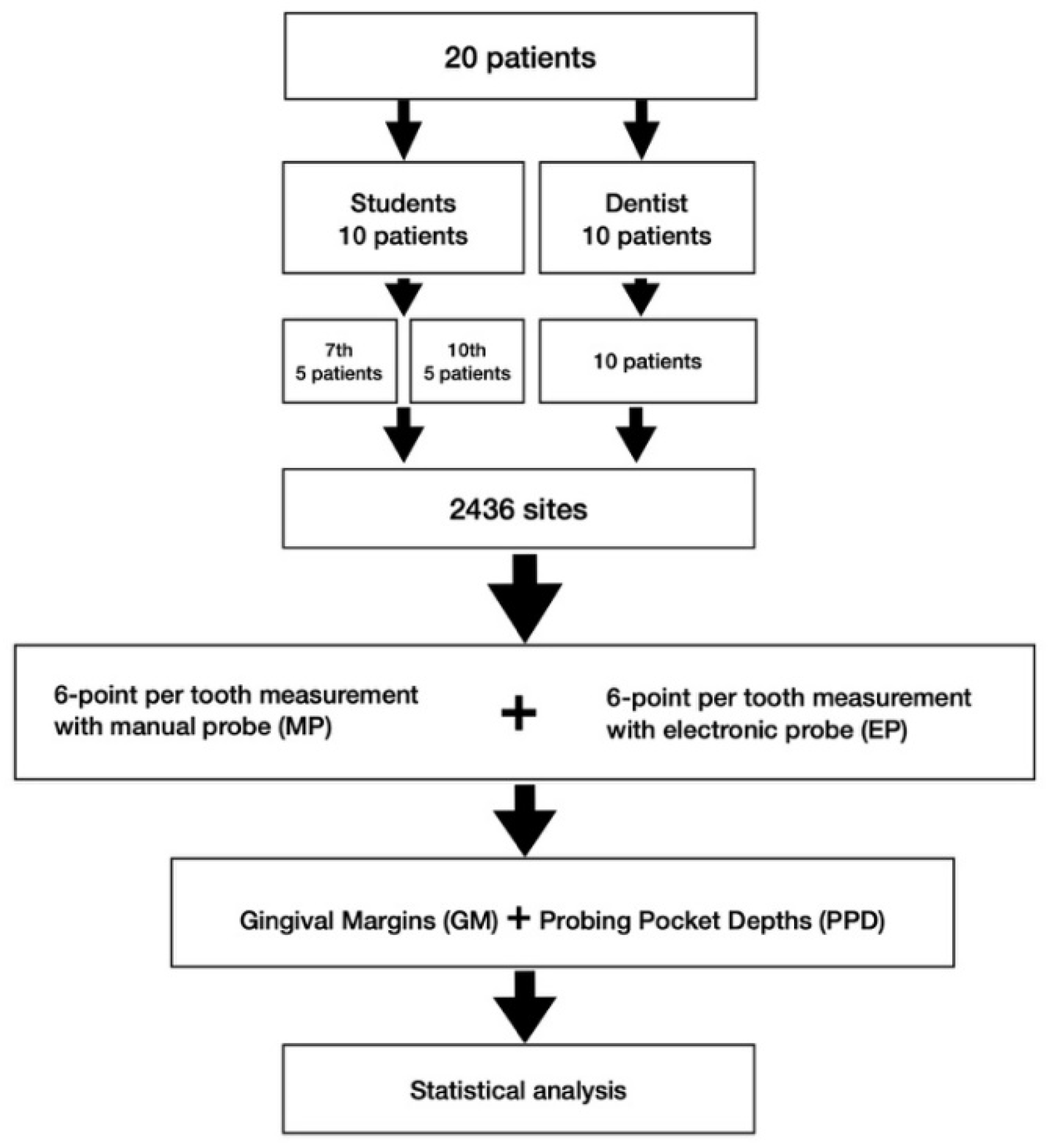
2. Materials and Methods
2.1. Study Center and Subjects
2.2. Sample Size Calculation
2.3. Study Design and Procedure
2.4. Clinical Parameters
2.5. Further Parameters
- Time needed to complete periodontal charting was counted for each method and each examiner and measured in minutes using a stopwatch;
- Questionnaires by means of visual analogue scale (VAS) were used to gain information concerning patient’s pain-sensation (0 [no pain] to 10 [extreme pain]) during probing;
- The subjective experience of the patients was determined by an independently developed questionnaire in the style of Quality of life (QoL);
- An evaluation by dental professionals was performed in order to determine expectations and satisfaction (VAS) with MP compared to EP.
2.6. Data Management/Data Collection Forms
2.7. Statistical Analysis
3. Results
3.1. Measurements of Probing Pocket Depths (PPD) and Gingival Margins (GM)
3.2. Time Needed for Measurements
3.3. Patients Pain Sensitivity (VAS)
3.4. Patients’ Subjective Experience
3.5. Evaluation by Dental Professionals
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Eke, P.I.; Wei, L.; Borgnakke, W.S.; Thornton-Evans, G.; Zhang, X.; Lu, H.; McGuire, L.C.; Genco, R.J. Periodontitis prevalence in adults ≥65 years of age, in the USA. Periodontology 2000 2016, 72, 76–95. [Google Scholar] [CrossRef]
- Botelho, J.; Machado, V.; Leira, Y.; Proença, L.; Chambrone, L.; Mendes, J.J. Economic burden of periodontitis in the United States and Europe—An updated estimation. J. Periodontol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Willis, J.R.; Gabaldón, T. The Human Oral Microbiome in Health and Disease: From Sequences to Ecosystems. Microorganisms 2020, 8, 308. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramseier, C.A.; Anerud, A.; Dulac, M.; Lulic, M.; Cullinan, M.; Seymour, G.; Faddy, M.J.; Bürgin, W.; Schätzle, M.; Lang, N.P. Natural history of periodontitis: Disease progression and tooth loss over 40 years. J. Clin. Periodontol. 2017, 44, 1182–1191. [Google Scholar] [CrossRef] [Green Version]
- Khumaedi, A.I.; Purnamasari, D.; Wijaya, I.P.; Soeroso, Y. The relationship of diabetes, periodontitis and cardiovascular disease. Diabetes Metab. Syndr. Clin. Res. Rev. 2019, 13, 1675–1678. [Google Scholar] [CrossRef] [PubMed]
- Sanz, M.; Del Castillo, A.M.; Jepsen, S.; Juanatey, J.R.G.; D’Aiuto, F.; Bouchard, P.; Chapple, I.; Dietrich, T.; Gotsman, I.; Graziani, F.; et al. Periodontitis and cardiovascular diseases: Consensus report. J. Clin. Periodontol. 2020, 47, 268–288. [Google Scholar] [CrossRef]
- Sapey, E.; Yonel, Z.; Edgar, R.; Parmar, S.; Hobbins, S.; Newby, P.; Crossley, D.; Usher, A.; Johnson, S.; Walton, G.; et al. The clinical and inflammatory relationships between periodontitis and chronic obstructive pulmonary disease. J. Clin. Periodontol. 2020, 47, 1040–1052. [Google Scholar] [CrossRef]
- Minty, M.; Canceill, T.; Serino, M.; Burcelin, R.; Tercé, F.; Blasco-Baque, V. Oral microbiota-induced periodontitis: A new risk factor of metabolic diseases. Rev. Endocr. Metab. Disord. 2019, 20, 449–459. [Google Scholar] [CrossRef]
- Jepsen, S.; Suvan, J.; Deschner, J. The association of periodontal diseases with metabolic syndrome and obesity. Periodontology 2000 2020, 83, 125–153. [Google Scholar] [CrossRef]
- Caton, J.G.; Armitage, G.; Berglundh, T.; Chapple, I.L.; Jepsen, S.; Kornman, K.S.; Mealey, B.L.; Papapanou, P.N.; Sanz, M.; Tonetti, M.S. A new classification scheme for periodontal and peri-implant diseases and conditions—Introduction and key changes from the 1999 classification. J. Clin. Periodontol. 2018, 45 (Suppl. 20), S1–S8. [Google Scholar] [CrossRef]
- Sanz, M.; Herrera, D.; Kebschull, M.; Chapple, I.; Jepsen, S.; Berglundh, T.; Sculean, A.; Tonetti, M.S.; Aass, A.M.; Aimetti, M.; et al. Treatment of stage I–III periodontitis—The EFP S3 level clinical practice guideline. J. Clin. Periodontol. 2020, 47 (Suppl. 22), 4–60. [Google Scholar] [CrossRef] [PubMed]
- Räisänen, I.T.; Lähteenmäki, H.; Gupta, S.; Grigoriadis, A.; Sahni, V.; Suojanen, J.; Seppänen, H.; Tervahartiala, T.; Sakellari, D.; Sorsa, T. An aMMP-8 Point-of-Care and Questionnaire Based Real-Time Diagnostic Toolkit for Medical Practitioners. Diagnostics 2021, 11, 711. [Google Scholar] [CrossRef] [PubMed]
- Deng, K.; Pelekos, G.; Jin, L.; Tonetti, M.S. Diagnostic accuracy of a point-of-care aMMP-8 test in the discrimination of periodontal health and disease. J. Clin. Periodontol. 2021, 48, 1051–1065. [Google Scholar] [CrossRef] [PubMed]
- Lähteenmäki, H.; Umeizudike, K.A.; Heikkinen, A.M.; Räisänen, I.T.; Rathnayake, N.; Johannsen, G.; Tervahartiala, T.; Nwhator, S.O.; Sorsa, T. aMMP-8 Point-of-Care/Chairside Oral Fluid Technology as a Rapid, Non-Invasive Tool for Periodontitis and Peri-Implantitis Screening in a Medical Care Setting. Diagnostics 2020, 10, 562. [Google Scholar] [CrossRef] [PubMed]
- Krishna, R.; De Stefano, J.A. Ultrasonic vs. hand instrumentation in periodontal therapy: Clinical outcomes. Periodontology 2000 2016, 71, 113–127. [Google Scholar] [CrossRef] [PubMed]
- Jepsen, S.; Caton, J.G.; Albandar, J.M.; Bissada, N.F.; Bouchard, P.; Cortellini, P.; Demirel, K.; de Sanctis, M.; Ercoli, C.; Fan, J.; et al. Periodontal manifestations of systemic diseases and developmental and acquired conditions: Consensus report of workgroup 3 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Clin. Periodontol. 2018, 45 (Suppl. 20), S219–S229. [Google Scholar] [CrossRef]
- Listgarten, M.A. Periodontal probing: What does it mean? J. Clin. Periodontol. 1980, 7, 165–176. [Google Scholar] [CrossRef]
- Listgarten, M.A.; Mao, R.; Robinson, P.J. Periodontal Probing and the Relationship of the Probe Tip to Periodontal Tissues. J. Periodontol. 1976, 47, 511–513. [Google Scholar] [CrossRef]
- Watts, T. Constant force probing with and without a stent in untreated periodontal disease: The clinical reproducibility problem and possible sources of error. J. Clin. Periodontol. 1987, 14, 407–411. [Google Scholar] [CrossRef]
- Kingman, A.; Morrison, E.; Löe, H.; Smith, J. Systematic Errors in Estimating Prevalence and Severity of Periodontal Disease. J. Periodontol. 1988, 59, 707–713. [Google Scholar] [CrossRef]
- Gabathuler, H.; Hassell, T. A pressure-sensitive periodontal probe. Helvetica Odontol. Acta 1971, 15, 114–117. [Google Scholar]
- Polson, A.M.; Caton, J.G.; Yeaple, R.N.; Zander, H.A. Histological determination of probe tip penetration into gingival sulcus of humans using an electronic pressure-sensitive probe. J. Clin. Periodontol. 1980, 7, 479–488. [Google Scholar] [CrossRef] [PubMed]
- Oringer, R.J.; Fiorellini, J.P.; Koch, G.G.; Sharp, T.J.; Nevins, M.L.; Davis, G.H.; Howell, T.H. Comparison of Manual and Automated Probing in an Untreated Periodontitis Population. J. Periodontol. 1997, 68, 1156–1162. [Google Scholar] [CrossRef] [PubMed]
- Holtfreter, B.; Alte, D.; Schwahn, C.; Desvarieux, M.; Kocher, T. Effects of different manual periodontal probes on periodontal measurements. J. Clin. Periodontol. 2012, 39, 1032–1041. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Erriu, M.; Genta, G.; Pili, F.M.G.; Barbato, G.; Denotti, G.; Levi, R. Probing depth in periodontal pockets: In vitro evaluation of contributions to variability due to probe type and operator skill. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2015, 229, 743–749. [Google Scholar] [CrossRef] [PubMed]
- Araujo, M.W.; Benedek, K.M.; Benedek, J.R.; Grossi, S.G.; Dorn, J.; Wactawski-Wende, J.; Genco, R.J.; Trevisan, M. Reproducibility of Probing Depth Measurements Using a Constant-Force Electronic Probe: Analysis of Inter- and Intraexaminer Variability. J. Periodontol. 2003, 74, 1736–1740. [Google Scholar] [CrossRef]
- Grossi, S.G.; Dunford, R.G.; Ho, A.; Koch, G.; Machtei, E.E.; Genco, R.J. Sources of error for periodontal probing measurements. J. Periodontal Res. 1996, 31, 330–336. [Google Scholar] [CrossRef]
- Biddle, A.J.; Palmer, R.M.; Wilson, R.F.; Watts, T.L.P. Comparison of the validity of periodontal probing measurements in smokers and non-smokers. J. Clin. Periodontol. 2001, 28, 806–812. [Google Scholar] [CrossRef]
- Walsh, T.F.; Saxby, M.S. Inter-and intra-examiner variability using standard and constant force periodontal probes. J. Clin. Periodontol. 1989, 16, 140–143. [Google Scholar] [CrossRef]
- Mombelli, A.; Graf, H. Depth-force-patterns in periodontal probing. J. Clin. Periodontol. 1986, 13, 126–130. [Google Scholar] [CrossRef]
- Drucker, S.D.; Prieto, L.E.; Kao, D.W. Periodontal Probing Calibration in an Academic Setting. J. Dent. Educ. 2012, 76, 1466–1473. [Google Scholar] [CrossRef] [PubMed]
- Renatus, A.; Trentzsch, L.; Schönfelder, A.; Schwarzenberger, F.; Jentsch, H. Evaluation of an Electronic Periodontal Probe Versus a Manual Probe. J. Clin. Diagn. Res. 2016, 10, ZH03–ZH07. [Google Scholar] [CrossRef] [PubMed]
- Mayfield, L.; Bratthall, G.; Attstrom, R. Periodontal probe precision using 4 different periodontal probes. J. Clin. Periodontol. 1996, 23, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Hull, P.; Clerehugh, V.; Ghassemi-Aval, A. An Assessment of the Validity of a Constant Force Electronic Probe in Measuring Probing Depths. J. Periodontol. 1995, 66, 848–851. [Google Scholar] [CrossRef] [PubMed]
- Perry, D.A.; Taggart, E.J.; Leung, A.; Newbrun, E. Comparison of a Conventional Probe With Electronic and Manual Pressure-Regulated Probes. J. Periodontol. 1994, 65, 908–913. [Google Scholar] [CrossRef] [PubMed]
- Pistorius, A.; Patrosio, C.; Willershausen, B.; Mildenberger, P.; Rippin, G. Periodontal probing in comparison to diagnosis by CT-Scan. Int. Dent. J. 2001, 51, 339–347. [Google Scholar] [CrossRef]
- Schneider, D.; Ender, A.; Truninger, T.; Leutert, C.; Sahrmann, P.; Roos, M.; Schmidlin, P. Comparison between Clinical and Digital Soft Tissue Measurements. J. Esthet. Restor. Dent. 2014, 26, 191–199. [Google Scholar] [CrossRef]
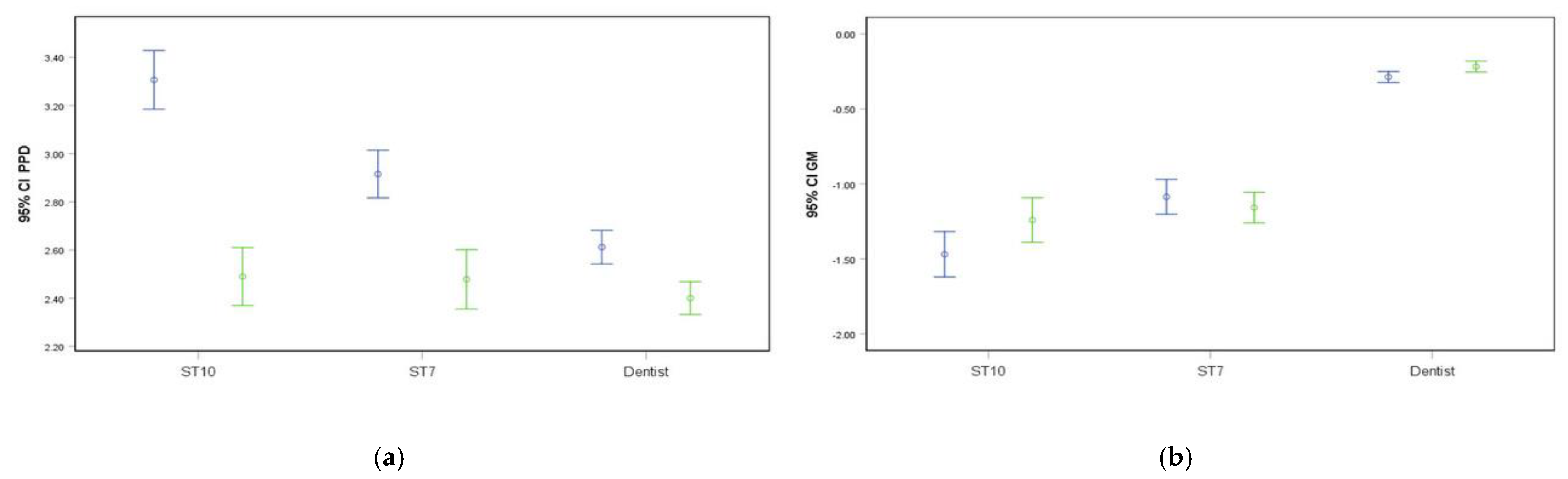
| MP | EP | p-Value | Correlation (Spearman’s Rho) | |
|---|---|---|---|---|
| PPD (in mm) | 2.82 ± 1.33 | 2.44 ± 1.35 | <0.001 * | 0.685 * |
| ΔPPD | 0.38 | |||
| GM (in mm) | −0.71 ± 1.25 | −0.64 ± 1.19 | 0.195 | 0.674 * |
| ΔGM | 0.07 | |||
| Examiner | MP | EP | p-Value | Correlation (Spearman’s Rho) | |
|---|---|---|---|---|---|
| PPD (in mm) | Dentist | 2.61 ± 1.33 | 2.40 ± 1.29 | 0.002 * | 0.810 * |
| ΔPPD | 0.21 | ||||
| PPD (in mm) | ST10 | 3.31 ± 1.37 | 2.49 ± 1.35 | <0.001 * | 0.617 * |
| ΔPPD | 0.82 | ||||
| PPD (in mm) | ST7 | 2.92 ± 1.19 | 2.48 ± 1.48 | 0.195 | 0.476 * |
| ΔPPD | 0.44 | ||||
| GM (in mm) | Dentist | −0.29 ± 0.70 | −0.22 ± 0.70 | 0.047 * | 0.622 * |
| ΔGM | 0.07 | ||||
| GM (in mm) | ST10 | −1.47 ± 1.70 | −1.24 ± 1.67 | 0.203 | 0.699 * |
| ΔGM | 0.23 | ||||
| GM (in mm) | ST7 | −1.09 ± 1.40 | −1.16 ± 1.23 | 0.497 | 0.598 * |
| ΔGM | 0.07 | ||||
| PPD (in mm) | −7 | −6 | −5 | −4 | −3 | −2 | −1 | 0 | 1 | 2 | 3 | 4 | 5 |
| Dentist | 0.07 | 0.65 | 10.34 | 58.48 | 28.66 | 1.29 | 0.29 | 0.14 | 0.07 | ||||
| ST10 | 0.6 | 1.0 | 6.2 | 31.5 | 35.6 | 20.0 | 4.5 | 0.4 | 0.2 | ||||
| ST7 | 0.2 | 0.7 | 2.5 | 5.0 | 12.7 | 25.0 | 34.6 | 15.3 | 3.2 | 0.7 | |||
| GM (in mm) | −7 | −6 | −5 | −4 | −3 | −2 | −1 | 0 | 1 | 2 | 3 | 4 | 5 |
| Dentist | 0.3 | 0.4 | 2.5 | 7.0 | 85.0 | 3.1 | 1.4 | 0.3 | 0.1 | ||||
| ST10 | 0.4 | 0.4 | 0.4 | 1.9 | 8.2 | 20.2 | 51.1 | 10.5 | 5.4 | 1.0 | 0.4 | ||
| ST7 | 0.2 | 0.6 | 2.2 | 5.2 | 14.4 | 43.5 | 27.0 | 4.4 | 1.7 | 0.7 |
| Examiner | MP | EP | p-Value |
|---|---|---|---|
| Dentist | 14 ± 4 | 16 ± 4 | 0.152 |
| ST10 | 21 ± 10 | 21 ± 13 | 0.875 |
| ST7 | 33 ± 14 | 37 ± 9 | 0.500 |
| All | 21 ± 11 | 23 ± 11 | 0.272 |
| Examiner | MP | EP | p-Value |
|---|---|---|---|
| Dentist | 3.47 ± 2.23 | 2.76 ± 2.32 | 0.177 |
| ST10 | 3.68 ± 2.04 | 1.72 ± 2.26 | 0.105 |
| ST7 | 3.80 ± 1.60 | 6.00 ± 1.41 | 0.198 |
| All | 3.61 ± 2.04 | 3.31 ± 2.66 | 0.615 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Laugisch, O.; Auschill, T.M.; Heumann, C.; Sculean, A.; Arweiler, N.B. Clinical Evaluation of a New Electronic Periodontal Probe: A Randomized Controlled Clinical Trial. Diagnostics 2022, 12, 42. https://doi.org/10.3390/diagnostics12010042
Laugisch O, Auschill TM, Heumann C, Sculean A, Arweiler NB. Clinical Evaluation of a New Electronic Periodontal Probe: A Randomized Controlled Clinical Trial. Diagnostics. 2022; 12(1):42. https://doi.org/10.3390/diagnostics12010042
Chicago/Turabian StyleLaugisch, Oliver, Thorsten M. Auschill, Christian Heumann, Anton Sculean, and Nicole B. Arweiler. 2022. "Clinical Evaluation of a New Electronic Periodontal Probe: A Randomized Controlled Clinical Trial" Diagnostics 12, no. 1: 42. https://doi.org/10.3390/diagnostics12010042
APA StyleLaugisch, O., Auschill, T. M., Heumann, C., Sculean, A., & Arweiler, N. B. (2022). Clinical Evaluation of a New Electronic Periodontal Probe: A Randomized Controlled Clinical Trial. Diagnostics, 12(1), 42. https://doi.org/10.3390/diagnostics12010042







