Impact of Antibiotic Prophylaxis on Infection Rate after Endoscopic Ultrasound Through-the-Needle Biopsy of Pancreatic Cysts: A Propensity Score-Matched Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Procedures
2.3. Follow-Up and Outcomes
2.4. Statistical Analysis
3. Results
3.1. Patients
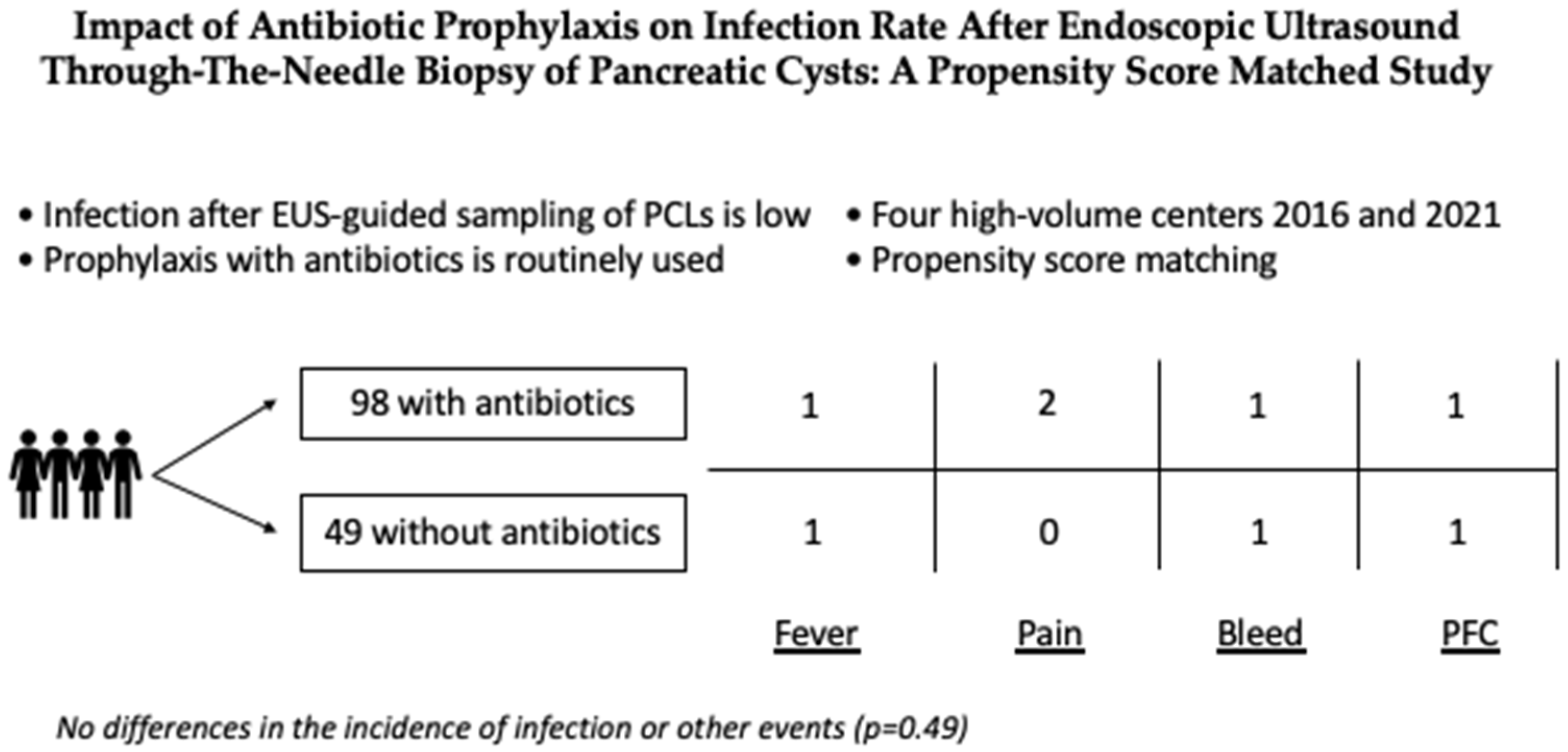
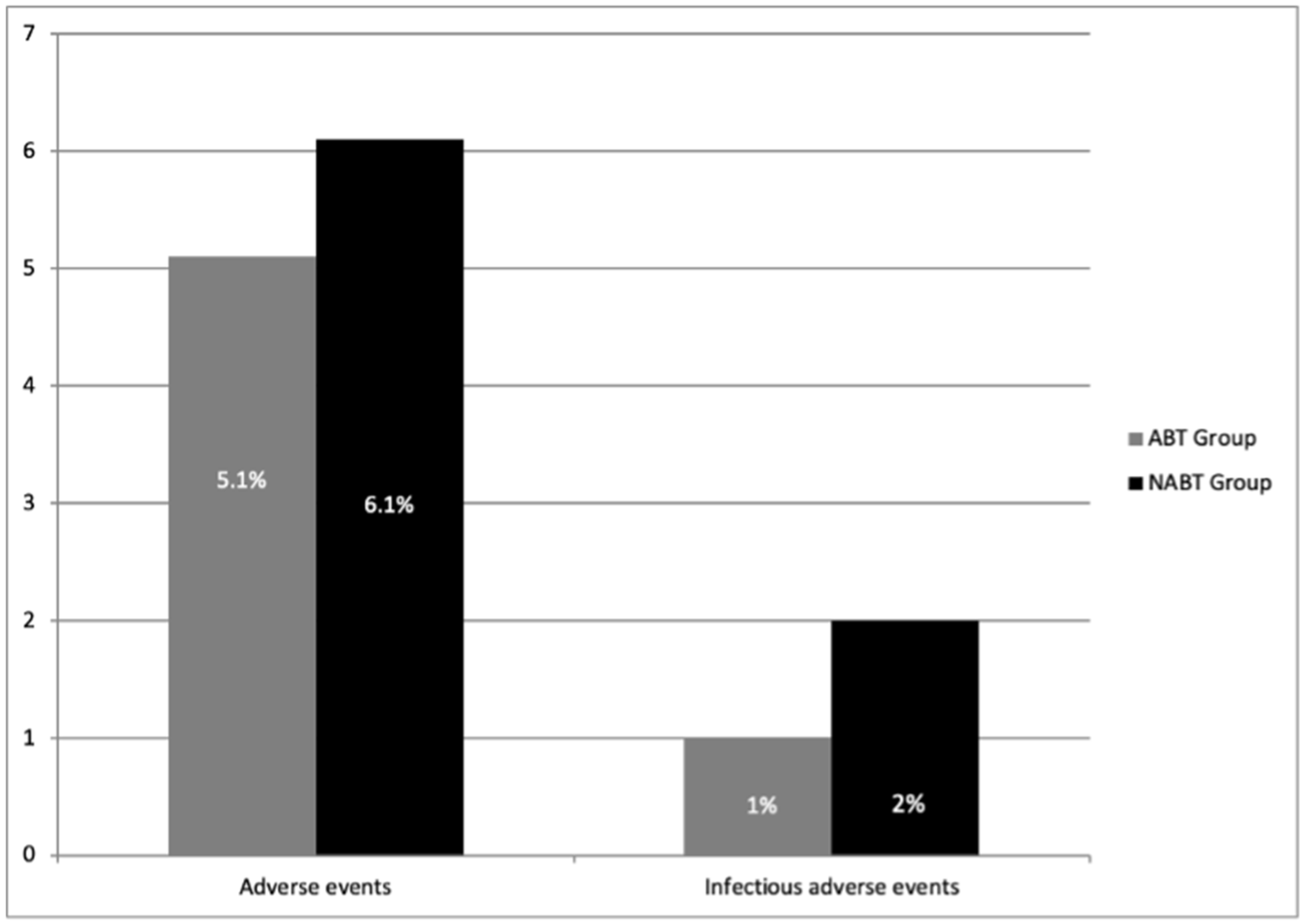
3.2. Adverse Events
3.3. Secondary Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- DiMaio, C.J. Current Guideline Controversies in the Management of Pancreatic Cystic Neoplasms. Gastrointest. Endosc. Clin. N. Am. 2018, 28, 529–547. [Google Scholar] [CrossRef]
- Uribarri-Gonzalez, L.; Keane, M.G.; Pereira, S.P.; Iglesias-García, J.; Dominguez-Muñoz, J.E.; Lariño-Noia, J. Agreement among Magnetic Resonance Imaging/Magnetic Resonance Cholangiopancreatography (MRI-MRCP) and Endoscopic Ultrasound (EUS) in the evaluation of morphological features of Branch Duct Intraductal Papillary Mucinous Neoplasm (BD-IPMN). Pancreatology 2018, 18, 170–175. [Google Scholar] [CrossRef]
- Do, R.K.; Katz, S.S.; Gollub, M.J.; Li, J.; LaFemina, J.; Zabor, E.C.; Moskowitz, C.S.; Klimstra, D.S.; Allen, P.J. Interobserver Agreement for Detection of Malignant Features of Intraductal Papillary Mucinous Neoplasms of the Pancreas on MDCT. Am. J. Roentgenol. 2014, 203, 973–979. [Google Scholar] [CrossRef] [Green Version]
- Crinò, S.; Bernardoni, L.; Manfrin, E.; Parisi, A.; Gabbrielli, A. Endoscopic ultrasound features of pancreatic schwannoma. Endosc. Ultrasound 2016, 5, 396–398. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Polkowski, M.; Jenssen, C.C.; Kaye, P.V.; Carrara, S.; Deprez, P.; Ginès, A.; Fernández-Esparrach, G.G.; Eisendrath, P.; Aithal, G.P.; Arcidiacono, P.P.; et al. Technical aspects of endoscopic ultrasound (EUS)-guided sampling in gastroenterology: European Society of Gastrointestinal Endoscopy (ESGE) Technical Guideline—March 2017. Endoscopy 2017, 249, 989–1006. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- ASGE Standards of Practice Committee; Muthusamy, V.R.; Chandrasekhara, V.; Acosta, R.D.; Bruining, D.H.; Chathadi, K.V.; Eloubeidi, M.A.; Faulx, A.L.; Fonkalsrud, L.; Gurudu, S.R.; et al. The role of endoscopy in the diagnosis and treatment of cystic pancreatic neoplasms. Gastrointest. Endosc. 2016, 84, 481–488. [Google Scholar] [CrossRef] [Green Version]
- Van der Waaij, L.A.; van Dullemen, H.M.; Porte, R.J. Cyst fluid analysis in the differential diagnosis of pancreatic cystic lesions: A pooled analysis. Gastrointest. Endosc. 2005, 62, 383–389. [Google Scholar] [CrossRef]
- Facciorusso, A.; Buccino, V.R.; Sacco, R. Needle-based confocal laser endomicroscopy in pancreatic cysts: A meta-analysis. Eur. J. Gastroenterol. Hepatol. 2020, 32, 1084–1090. [Google Scholar] [CrossRef]
- Crinò, S.F.; Bernardoni, L.; Gabbrielli, A.; Capelli, P.; Salvia, R.; Rusev, B.C.; Scarpa, A.; Manfrin, E. Beyond Pancreatic Cyst Epithelium: Evidence of Ovarian-Like Stroma in EUS-Guided Through-the-Needle Micro-Forceps Biopsy Specimens. Am. J. Gastroenterol. 2018, 113, 1059–1060. [Google Scholar] [CrossRef]
- Facciorusso, A.; Del Prete, V.; Antonino, M.; Buccino, V.R.; Wani, S. Diagnostic yield of EUS-guided through-the-needle biopsy in pancreatic cysts: A meta-analysis. Gastrointest. Endosc. 2020, 92, 1–8.e3. [Google Scholar] [CrossRef]
- Tacelli, M.; Celsa, C.; Magro, B.; Barchiesi, M.; Barresi, L.; Capurso, G.; Arcidiacono, P.G.; Cammà, C.; Crinò, S.F. Diagnostic performance of endoscopic ultrasound through-the-needle microforceps biopsy of pancreatic cystic lesions: Systematic review with meta-analysis. Dig. Endosc. 2020, 32, 1018–1030. [Google Scholar] [CrossRef] [Green Version]
- Kovacevic, B.; Klausen, P.; Rift, C.V.; Toxværd, A.; Grossjohann, H.; Karstensen, J.G.; Brink, L.; Hassan, H.; Kalaitzakis, E.; Storkholm, J.; et al. Clinical impact of endoscopic ultrasound-guided through-the-needle microbiopsy in patients with pancreatic cysts. Endoscopy 2021, 53, 44–52. [Google Scholar] [CrossRef]
- Colan-Hernandez, J.; Sendino, O.; Loras, C.; Pardo, A.; Gornals, J.B.; Concepción, M.; Sánchez-Montes, C.; Murzi, M.; Andujar, X.; Velasquez-Rodriguez, J.; et al. Antibiotic Prophylaxis Is Not Required for Endoscopic Ultrasonography-Guided Fine-Needle Aspiration of Pancreatic Cystic Lesions, Based on a Randomized Trial. Gastroenterology 2020, 158, 1642–1649.e1. [Google Scholar] [CrossRef] [PubMed]
- Facciorusso, A.; Buccino, V.R.; Turco, A.; Antonino, M.; Muscatiello, N. Antibiotics Do Not Decrease the Rate of Infection after Endoscopic Ultrasound Fine-Needle Aspiration of Pancreatic Cysts. Dig. Dis. Sci. 2019, 64, 2308–2315. [Google Scholar] [CrossRef] [PubMed]
- Facciorusso, A.; Mohan, B.P.; Tacelli, M.; Crinò, S.F.; Antonini, F.; Fantin, A.; Barresi, L. Use of antibiotic prophylaxis is not needed for endoscopic ultrasound-guided fine-needle aspiration of pancreatic cysts: A meta-analysis. Expert Rev. Gastroenterol. Hepatol. 2020, 14, 999–1005. [Google Scholar] [CrossRef]
- Cotton, P.B.; Eisen, G.M.; Aabakken, L.; Baron, T.H.; Hutter, M.M.; Jacobson, B.C.; Mergener, K.; Nemcek, A., Jr.; Petersen, B.T.; Petrini, J.L.; et al. A lexicon for endoscopic adverse events: Report of an ASGE workshop. Gastrointest. Endosc. 2010, 71, 446–454. [Google Scholar] [CrossRef]
- Larghi, A.; Manfrin, E.; Fabbri, C.; Crinò, S.F.; Correale, L.; Chiarello, G.; Barresi, L.; Van Velthuysen, M.L.; Poley, J.W.; Rahal, D.; et al. Interobserver agreement among expert pathologists on through-the-needle microforceps biopsy samples for evaluation of pancreatic cystic lesions. Gastrointest. Endosc. 2019, 90, 784–792. [Google Scholar] [CrossRef]
- Austin, P.C. A critical appraisal of propensity-score matching in the medical literature between 1996 and 2003. Stat. Med. 2007, 27, 2037–2049. [Google Scholar] [CrossRef]
- Austin, P.C. An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivar. Behav. Res. 2011, 46, 399–424. [Google Scholar] [CrossRef] [Green Version]
- Facciorusso, A.; Di Maso, M.; Antonino, M.; Del Prete, V.; Panella, C.; Barone, M.; Muscatiello, N. Polidocanol injection de-creases the bleeding rate after colon polypectomy: A propensity score analysis. Gastrointest. Endosc. 2015, 82, 350–358. [Google Scholar] [CrossRef] [PubMed]
- Lee, L.S.; Saltzman, J.R.; Bounds, B.C.; Poneros, J.M.; Brugge, W.R.; Thompson, C.C. EUS-guided fine needle aspiration of pancreatic cysts: A retrospective analysis of complications and their predictors. Clin. Gastroenterol. Hepatol. 2005, 3, 231–236. [Google Scholar] [CrossRef]
- Guarner-Argente, C.; Shah, P.; Buchner, A.; Ahmad, N.A.; Kochman, M.L.; Ginsberg, G.G. Use of antimicrobials for EUS-guided FNA of pancreatic cysts: A retrospective, comparative analysis. Gastrointest. Endosc. 2011, 74, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Crinò, S.F. Through-the-needle microforceps biopsy: A powerful tool but for selected patients. Endoscopy 2021, 53, 53–54. [Google Scholar] [CrossRef] [PubMed]
- Facciorusso, A.; Ramai, D.; Gkolfakis, P.; Shapiro, A.; Arvanitakis, M.; Lisotti, A.; Triantafyllou, K.; Fusaroli, P.; Papanikolaou, I.S.; Crinò, S.F. Through-the-needle biopsy of pancreatic cystic lesions: Current evidence and implications for clinical practice. Expert Rev. Med. Devices 2021, 21, 1–10. [Google Scholar] [CrossRef] [PubMed]

| Variable | No Antibiotic Prophylaxis (n = 49) | Antibiotic Prophylaxis (n = 98) | p Value |
|---|---|---|---|
| Age (years) | 62 (46–75) | 63 (48–76) | 0.79 |
| Gender—Male | 13 (26.5%) | 26 (26.5%) | 1.0 |
| Charlson comorbidity index | 4 (2–5) | 4 (2–5) | 0.4 |
| Body mass index | 24 (21–30) | 23 (20–28) | 0.51 |
| Symptoms | |||
| Asymptomatic | 30 (61.2%) | 64 (65.3%) | 0.37 |
| Upper abdominal pain | 10 (20.4%) | 19 (19.4%) | |
| Acute pancreatitis | 3 (6.1%) | 5 (5.1%) | |
| Jaundice | 6 (12.3%) | 10 (10.2%) | |
| Indications to the procedure | |||
| Unilocular/oligocystic lesion without | 3 (6.1%) | 6 (6.1%) | |
| communication with MPD | |||
| Size greater than 3 cm | 30 (61.2%) | 58 (59.1%) | 0.28 |
| Increased dimension | 5 (10.2%) | 6 (10.2%) | |
| Suspected mural nodules | 4 (10.2%) | 8 (10.2%) | |
| Thickened walls | 7 (12.3%) | 20 (14.4%) | |
| Lesion location | |||
| Head | 20 (40.8%) | 39 (39.7%) | 0.36 |
| Body | 13 (26.5%) | 26 (26.5%) | |
| Tail | 16 (32.7%) | 33 (33.8%) | |
| Lesion size (mm) | 33 (27–41) | 35 (29–40) | 0.76 |
| Cyst type | |||
| Unilocular | 34 (69.3%) | 68 (69.3%) | 1.0 |
| Oligocystic | 15 (30.7%) | 15 (30.7%) | |
| Cyst wall | |||
| Thin | 39 (79.5%) | 80 (81.6%) | 0.92 |
| Thick | 8 (16.3%) | 14 (14.2%) | |
| Nodules | 2 (4.2%) | 4 (4.2%) | |
| Puncture site | |||
| Stomach | 34 (69.3%) | 68 (69.3%) | 0.98 |
| Duodenal bulb | 12 (24.4%) | 24 (24.4%) | |
| Descending duodenum | 3 (6.3%) | 6 (12.6%) | |
| Number of needle passes | 1 (1–2) | 1 (1–2) | 0.54 |
| Number of microforceps passes | 2 (1–3) | 2 (1–3) | 0.54 |
| Complete aspiration of the cyst | 40 (81.6%) | 78 (79.5%) | 0.87 |
| Use of rectal indomethacin/diclofenac | 8 (16.3%) | 16 (16.3%) | 0.98 |
| Follow-up length (months) | 17 (10–25) | 18 (12–26) | 0.74 |
| Final diagnosis | |||
| IPMN | 3 (6.1%) | 6 (6.1%) | 0.23 |
| Serous cystadenoma | 18 (36.7%) | 37 (37.7%) | |
| Mucinous cystadenoma | 16 (32.6%) | 32 (32.6%) | |
| Pseudocyst | 2 (4%) | 4 (4%) | |
| Neuroendocrine tumor | 2 (4%) | 4 (4%) | |
| PDAC | 2 (4%) | 5 (5.1%) | |
| Undefined | 6 (12.6%) | 10 (10.5%) |
| Outcome | No Antibiotic Prophylaxis (49 pts) | Antibiotic Prophylaxis (98 pts) | p Value |
|---|---|---|---|
| Adverse event rate | 3 (6.1%) | 5 (5.1%) | 0.49 |
| Type of adverse event | |||
| Abdominal pain | 0 (0%) | 2 (2%) | 0.48 |
| Peri-pancreatic fluid collection | 1 (2%) | 1 (1%) | |
| Fever | 1 (2%) | 1 (1%) | |
| Bleeding | 1 (2%) | 1 (1%) | |
| Severity adverse event | |||
| Incident | 0 (0%) | 0 (0%) | 0.61 |
| Mild | 2 (4%) | 4 (4%) | |
| Moderate | 1 (2%) | 1 (1%) | |
| Severe | 0 (0%) | 0 (0%) | |
| Fatal | 0 (0%) | 0 (0%) | |
| Timing of adverse event occurrence | |||
| Intraprocedure | 1 (2%) | 1 (1%) | 0.43 |
| <14 days | 1 (2%) | 4 (4%) | |
| >14 days | 1 (2%) | 0 (0%) | |
| Diagnostic yield | 44 (89.7%) | 89 (90.8%) | 0.7 |
| Diagnostic accuracy | 40 (81.6%) | 80 (81.6%) | 1.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Facciorusso, A.; Arevalo-Mora, M.; Conti Bellocchi, M.C.; Bernardoni, L.; Ramai, D.; Gkolfakis, P.; Loizzi, D.; Muscatiello, N.; Ambrosi, A.; Tartaglia, N.; et al. Impact of Antibiotic Prophylaxis on Infection Rate after Endoscopic Ultrasound Through-the-Needle Biopsy of Pancreatic Cysts: A Propensity Score-Matched Study. Diagnostics 2022, 12, 211. https://doi.org/10.3390/diagnostics12010211
Facciorusso A, Arevalo-Mora M, Conti Bellocchi MC, Bernardoni L, Ramai D, Gkolfakis P, Loizzi D, Muscatiello N, Ambrosi A, Tartaglia N, et al. Impact of Antibiotic Prophylaxis on Infection Rate after Endoscopic Ultrasound Through-the-Needle Biopsy of Pancreatic Cysts: A Propensity Score-Matched Study. Diagnostics. 2022; 12(1):211. https://doi.org/10.3390/diagnostics12010211
Chicago/Turabian StyleFacciorusso, Antonio, Martha Arevalo-Mora, Maria Cristina Conti Bellocchi, Laura Bernardoni, Daryl Ramai, Paraskevas Gkolfakis, Domenico Loizzi, Nicola Muscatiello, Antonio Ambrosi, Nicola Tartaglia, and et al. 2022. "Impact of Antibiotic Prophylaxis on Infection Rate after Endoscopic Ultrasound Through-the-Needle Biopsy of Pancreatic Cysts: A Propensity Score-Matched Study" Diagnostics 12, no. 1: 211. https://doi.org/10.3390/diagnostics12010211
APA StyleFacciorusso, A., Arevalo-Mora, M., Conti Bellocchi, M. C., Bernardoni, L., Ramai, D., Gkolfakis, P., Loizzi, D., Muscatiello, N., Ambrosi, A., Tartaglia, N., Robles-Medranda, C., Stasi, E., Ofosu, A., & Crinò, S. F. (2022). Impact of Antibiotic Prophylaxis on Infection Rate after Endoscopic Ultrasound Through-the-Needle Biopsy of Pancreatic Cysts: A Propensity Score-Matched Study. Diagnostics, 12(1), 211. https://doi.org/10.3390/diagnostics12010211








