Seroprevalence of SARS-CoV-2 Antibodies in HIV-Infected Patients in Rome, Italy during the COVID-19 Outbreak
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Cohort
2.2. Evaluation of SARS-CoV-2 Seroprevalence
2.3. Statistical Analysis
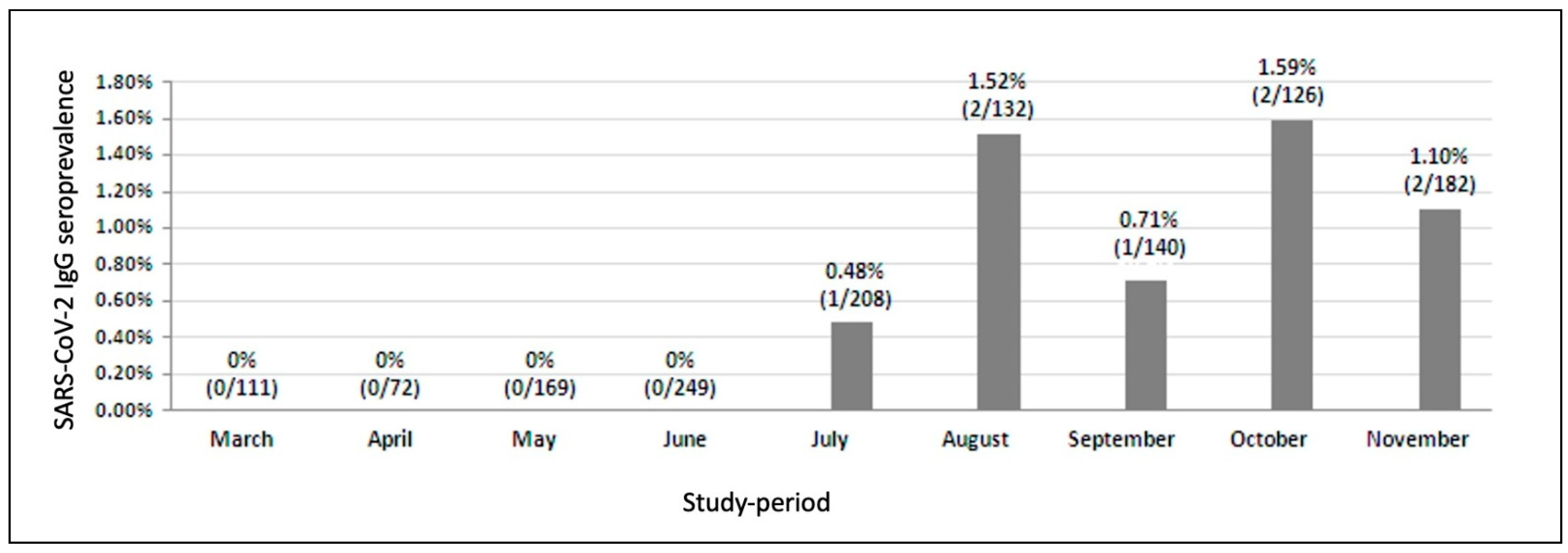
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cooper, T.J.; Woodward, B.L.; Alom, S.; Harky, A. Coronavirus disease 2019 (COVID-19) outcomes in HIV/AIDS patients: A systematic review. HIV Med. 2020, 21, 567–577. [Google Scholar] [CrossRef]
- Prabhu, S.; Poongulali, S.; Kumarasamy, N. Impact of COVID-19 on people living with HIV: A review. J. Virus Erad. 2020, 6, 100019. [Google Scholar] [CrossRef]
- Shiau, S.; Krause, K.D.; Valera, P.; Swaminathan, S.; Halkitis, P.N.J.A. The burden of COVID-19 in people living with HIV: A syndemic perspective. AIDS Behav. 2020, 24, 2244–2249. [Google Scholar] [CrossRef] [PubMed]
- Tesoriero, J.M.; Swain, C.-A.E.; Pierce, J.L.; Zamboni, L.; Wu, M.; Holtgrave, D.R.; Gonzalez, C.J.; Udo, T.; Morne, J.E.; Hart-Malloy, R.; et al. COVID-19 outcomes among persons living with or without diagnosed HIV infection in New York State. JAMA Netw. Open 2021, 4, e2037069. [Google Scholar] [CrossRef]
- Chang, J.J.; Bruxvoort, K.; Chen, L.H.; Rodriguez, J.; Akhavan, B.; Hechter, R.C. COVID-19 testing, characteristics, and outcomes among people living with HIV in an integrated health system. Open Forum Infect. Dis. 2020, 7 (Suppl. 1), S171–S172. [Google Scholar] [CrossRef]
- Inciarte, A.; Gonzalez-Cordon, A.; Rojas, J.; Torres, B.; De Lazzari, E.; De La Mora, L.; Martinez-Rebollar, M.; Laguno, M.; Callau, P.; Gonzalez-Navarro, A.; et al. Clinical characteristics, risk factors, and incidence of symptomatic COVID-19 in adults living with HIV: A single-center, prospective observational study. AIDS 2020, 34, 1775–1780. [Google Scholar] [CrossRef] [PubMed]
- Del Amo, J.; Polo, R.; Moreno, S.; Diaz, A.; Martinez, E.; Arribas, J.R.; Jarrín, I.; Hernán, M.A. Incidence and severity of COVID-19 in HIV-positive persons receiving antiretroviral therapy: A cohort study. Ann. Intern. Med. 2020, 173, 536–541. [Google Scholar] [CrossRef] [PubMed]
- Brown, L.B.; Spinelli, M.A.; Gandhi, M. The interplay between HIV and COVID-19: Summary of the data and responses to date. Curr. Opin. HIV AIDS 2021, 16, 63–73. [Google Scholar] [CrossRef] [PubMed]
- Lipsitch, M.; Swerdlow, D.L.; Finelli, L. Defining the Epidemiology of Covid-19—Studies Needed. N. Engl. J. Med. 2020, 382, 1194–1196. [Google Scholar] [CrossRef]
- Signorelli, C.; Odone, A.; Gianfredi, V.; Bossi, E.; Bucci, D.; Oradini-Alacreu, A.; Frascella, B.; Capraro, M.; Chiappa, F.; Blandi, L.; et al. The spread of COVID-19 in six western metropolitan regions: A false myth on the excess of mortality in Lombardy and the defense of the city of Milan. Acta Biomed. 2020, 9, 23–30. [Google Scholar]
- Italian Ministry of Health (Ministero della Salute). Novel Coronavirus. Available online: http://www.salute.gov.it/portale/nuovocoronavirus/homeNuovoCoronavirus.jsp?lingua=english (accessed on 11 December 2020).
- Noe, S.; Schabaz, F.; Heldwein, S.; Mayer, W.; Ruecker, K.; Tiller, F.W.; Von Krosigk, A.; Wiese, C.; Balogh, A.; Gersbacher, E.; et al. HIV and SARS-CoV-2 co-infection: Cross-sectional findings from a German ‘hotspot’. Infection 2021, 2, 1–8. [Google Scholar] [CrossRef]
- Papalini, C.; Paciosi, F.; Schiaroli, E.; Pierucci, S.; Busti, C.; Bozza, S.; Mencacci, A.; Francisci, D. Seroprevalence of anti-SARS-CoV2 antibodies in Umbrian persons living with HIV. Mediterr, J. Hematol Infect. Dis. 2020, 12, e2020080. [Google Scholar] [CrossRef] [PubMed]
- Spinelli, M.A.; Lynch, K.L.; Yun, C.; Glidden, D.V.; Peluso, M.J.; Henrich, T.J.; Gandhi, M.; Brown, L.B. SARS-CoV-2 seroprevalence, and IgG concentration and pseudovirus neutralising antibody titres after infection, compared by HIV status: A matched case-control observational study. Lancet HIV 2021. [Google Scholar] [CrossRef]
- Available online: https://www.istat.it/it/files/2020/08/ReportPrimiRisultatiIndagineSiero.pdf (accessed on 3 March 2021).
- Ralli, M.; Arcangeli, A.; Soave, P.M.; Voglino, M.C.; De-Giorgio, F. SARS-CoV-2 seroprevalence in the Vatican City State. Eur. J. Intern. Med. 2021, 86, 98–99. [Google Scholar] [CrossRef]
- Santi, M.; Diotallevi, A.; Brandi, G. Seroprevalence of Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) infection in an Italian cohort in Marche Region, Italy. Acta Biomed. 2021, 92, e2021070. [Google Scholar] [CrossRef]
- Maggiolo, F.; Zoboli, F.; Arosio, M.; Valenti, D.; Guarneri, D.; Sangiorgio, L.; Ripamonti, D.; Callegaro, A. SARS-CoV-2 infection in persons living with HIV: A single center prospective cohort. J. Med. Virol. 2021, 93, 1145–1149. [Google Scholar] [CrossRef] [PubMed]
- Chou, R.; Dana, T.; Buckley, D.I.; Selph, S.; Fu, R.; Totten, A.M. Epidemiology of and risk factors for coronavirus infection in health care workers. Ann. Intern. Med. 2020, 173, 120–136. [Google Scholar] [CrossRef]
- Joob, B.; Wiwanitkit, V. SARS-CoV-2 and HIV. J. Med. Virol. 2020, 92, 1415. [Google Scholar] [CrossRef] [Green Version]
- Gervasoni, C.; Meraviglia, P.; Riva, A.; Giacomelli, A.; Oreni, L.; Minisci, D.; Atzori, C.; Ridolfo, A.; Cattaneo, D. Clinical features and outcomes of HIV patients with coronavirus disease 2019. Clin. Infect. Dis. 2020, 71, 2276–2278. [Google Scholar] [CrossRef] [PubMed]
- Elfiky, A.A. Ribavirin, remdesivir, sofosbuvir, galidesivir, and tenofovir against SARS-CoV-2 RNA dependent RNA polymerase (RdRp): A molecular docking study. Life Sci. 2020, 253, 117592. [Google Scholar] [CrossRef]
- Jockusch, S.; Tao, C.; Li, X.; Anderson, K.T.; Chien, M.; Kumar, S.; Russo, J.J.; Kirchdoerfer, R.; Ju, J. Triphosphates of the two components in DESCOVY and TRUVADA are inhibitors of the SARS-CoV-2 polymerase. bioRxiv 2020. [Google Scholar] [CrossRef]
- Epicentro. Available online: https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19.pdf (accessed on 2 April 2020).
- Centers for Disease Control and Prevention Interim Guidelines for COVID-19 Antibody Testing in Clinical and Public Health Settings. 2020; (Updated August 1). Available online: https://www.cdc.gov/coronavirus/2019-ncov/lab/resources/antibody-tests-guidelines.html (accessed on 3 November 2020).
- Long, Q.-X.; Liu, B.-Z.; Deng, H.-J.; Wu, G.-C.; Deng, K.; Chen, Y.-K.; Liao, P.; Qiu, J.-F.; Lin, Y.; Cai, X.-F.; et al. Antibody responses to SARS-CoV-2 in patients with COVID-19. Nat. Med. 2020, 26, 845–848. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.unaids.org/en/regionscountries/countries/italy (accessed on 3 November 2020).
| (A). Demographic Characteristics | ||||||||||
| March 2021 n = 111 | April 2021 n = 72 | May 2021n = 169 | June 2021 n = 249 | July 2021 n = 208 | August 2021 n = 132 | September 2021 n = 140 | October 2021 n = 126 | November 2021 n = 182 | PLWH Population n = 1106 | |
| Gender, n (%) | ||||||||||
| Male | 74 (66.7) | 51 (70.8) | 114 (67.5) | 169 (67.9) | 135 (64.9) | 85 (64.4) | 102 (72.9) | 91 (72.2) | 131 (72.0) | 760 (68.7) |
| Age, years, (IQR) | 54.1 (45.2–59.3) | 48.5 (36.6–58.9) | 51.9 (44.7–60.1) | 53.3 (46.4–58.9) | 55.4 (43.8–60.4) | 52.2 (42.1–56.4) | 53.2 (43.4–59.7) | 54.0 (44.6–63.6) | 53.1 (46.1–59.4) | 52.9 (44.8–59.3) |
| Italian, n (%) | 88 (79.3) | 59 (81.9) | 139 (82.2) | 198 (79.5) | 165 (79.3) | 110 (83.3) | 111 (79.3) | 108 (85.7) | 159 (87.4) | 912 (82.5) |
| Risk factor, n (%) | ||||||||||
| Homo/bi-sexual | 34 (30.6) | 20 (27.8) | 60 (35.5) | 72 (28.9) | 61 (29.3) | 40 (30.3) | 53 (37.9) | 43 (34.1) | 70 (38.5) | 362 (32.6) |
| Heterosexual | 40 (36.0) | 16 (22.2) | 61 (36.1) | 111 (44.6) | 77 (37.0) | 61 (46.2) | 48 (34.3) | 50 (39.7) | 71 (39.0) | 431(38.5) |
| IVDU | 15 (13.5) | 11 (15.3) | 21 12.4) | 30 (12.0) | 31 (14.9) | 20 (15.2) | 22 (15.7) | 9 (7.1) | 18 (9.9) | 146 (13.2) |
| Time since HIV diagnosis, years, median (IQR) | 15.6 (7.6–23.8) | 9.8 (1.18–22.4) | 14.7 (6.5–22.4) | 16.6 (7.5–23.9) | 16.5 (7.4–25.8) | 16.2 (8.9–26.1) | 16.0 (6.3–24.3) | 13.0 (6.5–22.4) | 18.7 (11.5–24.3) | 15.9 (7.6–23.7) |
| Pre-ART HIV-RNA, log10 copies/mL, median (IQR) | 5.0 (4.1–5.4) | 4.9 (3.8–5.5) | 5.0 (4.2–5.4) | 4.9 (4.1–5.4) | 4.9 (4.1–5.4) | 4.9 (4.4–5.4) | 4.9 (4.5–5.4) | 4.9 (4.1–5.6) | 4.9 (4.2–5.5) | 4.9 (4.2–5.4) |
| CD4 cell count nadir, cells/mm3, median (IQR) | 205 (67–336) | 171 (36–320) | 170 (43–327) | 173 (50–291) | 200 (85–322) | 201 (74–285) | 125 (41–277) | 159 (36–353) | 176 (50–299) | 190 (56–315) |
| CD4 count, cells/mm3, median (IQR) | 577 (477–773) | 487 (275–730) | 615 (355–786) | 559 (379–781) | 619 (463–859) | 630 (486–865) | 587 (436–830) | 603 (434–871) | 676 (474–844) | 610 (436–822) |
| CD4/CD8 ratio, median (IQR) | 0.79 (0.52–1.13) | 0.74 (0.39–1.08) | 0.82 (0.53–1.25) | 0.85 (0.50–1.18) | 0.89 (0.61–1.32) | 0.88 (0.59–1.24) | 0.85 (0.62–1.16) | 0.84 (0.55–1.18) | 0.90 (0.59–1.27) | 0.87 (0.57–1.23) |
| HIV-RNA <50 copies/mL, n (%) | 100 (90.1) | 56 (77.8) | 154 (91.1) | 238 (95.6) | 192 (92.3) | 121 (91.7) | 126 (90.0) | 114 (90.5) | 173 (95.1) | 1029 (93.0) |
| Past Aids-defining events (CDC stage C), n (%) | 32 (28.8) | 18 (25) | 50 (29.6) | 87 (34.9) | 55 (26.4) | 35 (26.5) | 48 (34.3) | 49 (38.9) | 58 (31.9) | 335 (30.3) |
| (B). Clinical Characteristics | ||||||||||
| March 2021 n = 111 | April 2021 n = 72 | May 2021 n = 169 | June 2021 n = 249 | July 2021 n = 208 | August 2021 n = 132 | September 2021 n = 140 | October 2021 n = 126 | November 2021 n = 182 | PLWH Population n = 1106 | |
| Patients with at least one comorbidity, n (%) | 47 (42.3) | 22 (30.6) | 77 (45.6) | 124 (49.8) | 94 (45.2) | 51 (38.6) | 72 (51.4) | 58 (46.0) | 90 (49.5) | 498 (45.0) |
| Dyslipidemia, n (%) | 4 (3.6) | 2 (2.8) | 10 (5.9) | 13 (5.2) | 3 (5.2) | 3 (2.3 | 8 (5.7) | 7 (5.6) | 6 (3.3) | 44 (4.0) |
| Hypertension, n (%) | 11 (9.9) | 2 (2.8) | 19 (11.2) | 30 (12.0) | 24 (11.5) | 15 (11.4) | 12 (8.6) | 15 (11.9) | 24 (13.2) | 118 (10.7) |
| HCV co-infection, n (%) | 23 (20.7) | 10 (13.9) | 27 (16.0) | 39 (15.7) | 43 (20.7) | 26 (19.7) | 33 (23.6) | 12 (9.5) | 33 (18.1) | 193 (17.5) |
| HBV co-infection, n (%) | 2 (1.8) | 1 (1.4) | 5 (3.0) | 9 (3.6) | 4 (1.9) | 3 (2.3) | 6 (4.3) | 5 (4.0) | 5 (2.7) | 30 (2.7) |
| Diabetes mellitus, n (%) | 3 (2.07) | 2 (2.8) | 4 (2.4) | 5 (2.0) | 2 (1.0) | 1 (0.8) | 5 (3.6) | 3 (2.4) | 3 (1.6) | 22 (2.0) |
| Renal diseases, n (%) | 3 (2.7) | 1 (1.4) | 2 (1.2) | 9 (3.6) | 7 (3.4) | 2 (1.5) | 3 (2.1) | 5 (4.0) | 5 (2.7) | 29 (2.6) |
| Cardiovascular diseases, n (%) | 11 (9.9) | 8 (11.1) | 21 (12.4) | 38 (15.3) | 27 (13.0) | 9 (6.8) | 15 (10.7) | 17 (13.5) | 26 (14.3) | 130 (11.8) |
| History of neoplasms, n (%) | 18 (16.2) | 6 (8.3) | 26 (15.4) | 54 (21.7) | 30 (14.4) | 14 (10.6) | 27 (19.3) | 22 (17.5) | 30 (16.5) | 174 (15.7) |
| (C). Therapeutic Characteristics | ||||||||||
| March 2021 n = 111 | April 2021 n = 72 | May 2021 n = 169 | June 2021 n = 249 | July 2021 n = 208 | August 2021 n = 132 | September 2021 n = 140 | October 2021 n = 126 | November 2021 n = 182 | PLWH Population n = 1106 | |
| Currently on ART, n (%) | 97 (87.4) | 52 (72.2) | 161 (95.3) | 237 (95.2) | 200 (96.2) | 130 (98.5) | 135 (96.4) | 121 (96.0) | 178 (97.8) | 1038 (93.9) |
| Time on ART, years, median (IQR) | 12.1 (5.5–20.5) | 9.7 (0.68–17.6) | 11.2 (5.7–21.0) | 14.0 (6.5–22.1) | 11.9 (5.3–20.9) | 14.5 (7.0–21.6) | 12.5 (5.9–22.0) | 11.1 (5.6–21.3) | 15.8 (9.4–22.2) | 12.7 (6.4–21.2) |
| Type of ARTs, n (% = n/currently on ART) | ||||||||||
| Triple regimen | 71 (73.2) | 45 (86.5) | 113 (70.2) | 176 (74.3) | 155 (77.5) | 94 (72.3) | 96 (71.1) | 82 (67.8) | 116 (65.2) | 750 (67.8) |
| Dual regimen | 25 (25.8) | 7 (13.5) | 48 (29.8) | 58 (24.5) | 41 (20.5) | 36 (27.7) | 39 (28.9) | 38 (31.4) | 60 (33.7) | 279 (25.2) |
| Other combinations | 1 (1.0) | 0 (0.0) | 0 (0.0) | 3 (1.3) | 4 (2.0) | 0 (0.0) | 0 (0.0) | 1 (0.8) | 2 (1.1) | 9 (0.80) |
| Triple regimen based, n (%) | ||||||||||
| INSTI-based | 47 (66.2) | 30 (66.7) | 67 (59.3) | 92 (52.3) | 100 (64.5) | 53 (56.4) | 67 (69.8) | 57 (69.5) | 74 (63.8) | 446 (59.5) |
| PI-based | 6 (8.5) | 4 (8.9) | 12 (10.6) | 18 (10.2) | 11 (7.1) | 8 (8.5) | 11 (11.5) | 7 (8.5) | 8 (6.9) | 68 (9.1) |
| NNRTI-based | 18 (25.4) | 11 (24.4) | 34 (30.1) | 66 (37.5) | 44 (28.4) | 33 (35.1) | 18 (18.8) | 18 (22.0) | 34 (29.3) | 236 (31.5) |
| Dual regimen based, n (%) | ||||||||||
| INSTI-based | 17 (68.0) | 6 (85.7) | 34 (70.8) | 40 (69.0) | 29 (70.7) | 19 (52.8) | 23 (59.0) | 27 (71.1) | 43 (71.7) | 186 (66.7) |
| PI-based | 2 (8.0) | 0 (0.0) | 6 (12.5) | 9 (15.5) | 6 (14.6) | 6 (16.7) | 6 (15.4) | 6 (15.8) | 8 (13.3) | 44 (15.8) |
| Other dual | 6 (24.0) | 1 (14.3) | 8 (16.7) | 9 (15.5) | 6 (14.6) | 11 (30.6) | 10 (25.6) | 5 (13.2) | 9 (15.0) | 49 (17.6) |
| Pz | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| Month | July | August | August | September | October | October | November | November |
| Gender | F | F | F | F | M | M | M | M |
| Age, years | 61.5 | 55.5 | 39.5 | 47.9 | 39.6 | 66.5 | 51.4 | 58.5 |
| Italian | Yes | Yes | Yes | No, Uganda | Yes | Yes | Yes | Yes |
| Risk factor | Heterosexual | Heterosexual | Heterosexual | Heterosexual | Unknown | Heterosexual | Homo/bi-sexual | Homo/bi-sexual |
| Time since HIV diagnosis, years | 27.1 | 21.0 | 24.2 | 14.0 | 3.0 | 22.6 | 12.7 | 24.3 |
| Currently on ART | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Type of ARTs | Triple | Triple | Triple | Dual | Dual | Dual | Triple | Dual |
| INSTI-based | INSTI-based | NN-based | PI-based | INSTI-based | NN/INSTI | NN-based | PI-based | |
| 3TC,ABC,DTG | FTC,TAF,RGV | FTC,TDF,EFV | 3TC,ATV,cob | 3TC,DTG | RPV,DTG | FTC,TAF,RPV | 3TC,DRV,RTV | |
| Time on ART, years | 27.1 | 20.8 | 23.8 | 13.9 | 3.0 | 12.3 | 11.8 | 20.9 |
| Pre-ART HIV-RNA, Log10 cps/mL | 4.15 | 5.24 | 5.70 | 5.70 | 4.54 | 5.20 | 4.7 | 5.70 |
| CD4 cell count nadir, cells/mm3 | 206 | 298 | 36 | 119 | 390 | 326 | 258 | 328 |
| CD4 count, cells/mm3 | 524 | 1304 | 1095 | 783 | 859 | 885 | 423 | 804 |
| CD8 count, cells/mm3 | 620 | 1094 | 459 | 899 | 1205 | 1415 | 673 | 555 |
| CD4/CD8 ratio | 0.84 | 1.19 | 2.39 | 0.87 | 0.71 | 0.63 | 0.62 | 1.45 |
| HIV-RNA, copies/mL | 0 | 18 | 0 | 0 | 0 | 0 | 0 | 0 |
| Past Aids-defining events (CDC stage C) | / | / | Yes | Yes | / | / | / | / |
| Dyslipidemia | / | / | / | / | / | / | / | / |
| Hypertension | / | / | / | / | / | / | / | Yes |
| HCV/HBV co-infection | / | / | / | / | / | / | / | / |
| Diabetes mellitus | / | / | / | / | / | / | / | / |
| Renal diseases | / | / | / | / | / | / | / | / |
| Cardiovascular diseases | / | / | / | / | / | Yes | / | / |
| History of neoplasms | / | / | / | Yes | / | / | / | / |
| SARS-CoV-2 IgG | 1.2 | 1.5 | 1 | 4.5 | 1.1 | 3.3 | 1.8 | 2.2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lombardi, F.; Ricci, R.; Belmonti, S.; Fabbiani, M.; Borghetti, A.; Baldin, G.; Ciccullo, A.; Tamburrini, E.; Visconti, E.; Sanguinetti, M.; et al. Seroprevalence of SARS-CoV-2 Antibodies in HIV-Infected Patients in Rome, Italy during the COVID-19 Outbreak. Diagnostics 2021, 11, 1154. https://doi.org/10.3390/diagnostics11071154
Lombardi F, Ricci R, Belmonti S, Fabbiani M, Borghetti A, Baldin G, Ciccullo A, Tamburrini E, Visconti E, Sanguinetti M, et al. Seroprevalence of SARS-CoV-2 Antibodies in HIV-Infected Patients in Rome, Italy during the COVID-19 Outbreak. Diagnostics. 2021; 11(7):1154. https://doi.org/10.3390/diagnostics11071154
Chicago/Turabian StyleLombardi, Francesca, Rosalba Ricci, Simone Belmonti, Massimiliano Fabbiani, Alberto Borghetti, Gianmaria Baldin, Arturo Ciccullo, Enrica Tamburrini, Elena Visconti, Maurizio Sanguinetti, and et al. 2021. "Seroprevalence of SARS-CoV-2 Antibodies in HIV-Infected Patients in Rome, Italy during the COVID-19 Outbreak" Diagnostics 11, no. 7: 1154. https://doi.org/10.3390/diagnostics11071154
APA StyleLombardi, F., Ricci, R., Belmonti, S., Fabbiani, M., Borghetti, A., Baldin, G., Ciccullo, A., Tamburrini, E., Visconti, E., Sanguinetti, M., & Di Giambenedetto, S. (2021). Seroprevalence of SARS-CoV-2 Antibodies in HIV-Infected Patients in Rome, Italy during the COVID-19 Outbreak. Diagnostics, 11(7), 1154. https://doi.org/10.3390/diagnostics11071154








