Systematic Review and Meta-Analysis of the Diagnostic Accuracy of Mobile-Linked Point-of-Care Diagnostics in Sub-Saharan Africa
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection
2.3. Eligibility Criteria
2.3.1. Inclusion Criteria
- Articles that presented evidence on Health Professionals using mHealth devices at POC diagnostics.
- Articles that presented evidence on diseases diagnosed at POC diagnostics.
- Studies that published evidence on other diagnostic tools linked to POC diagnostics.
- Articles published on the diagnostic accuracy of mobile-linked POC diagnostics.
- Articles that presented evidence from Sub-Saharan Africa.
2.3.2. Exclusion Criteria
- Studies that presented evidence of patients using mHealth devices at POC diagnostics.
- Articles that reported evidence on typical diagnostic devices.
- Articles published on mHealth devices support treatment in appointment reminders, medication and treatment compliance, and others.
- Studies that showed evidence on mHealth for disease surveillance.
- Studies that published evidence on using mHealth for communication purposes.
- Articles that published evidence outside Sub-Saharan Africa.
2.4. Data Extraction
2.5. Assessment of Methodological Quality
2.6. Data Analysis
3. Results
3.1. Search
3.2. Characteristics of the Included Articles
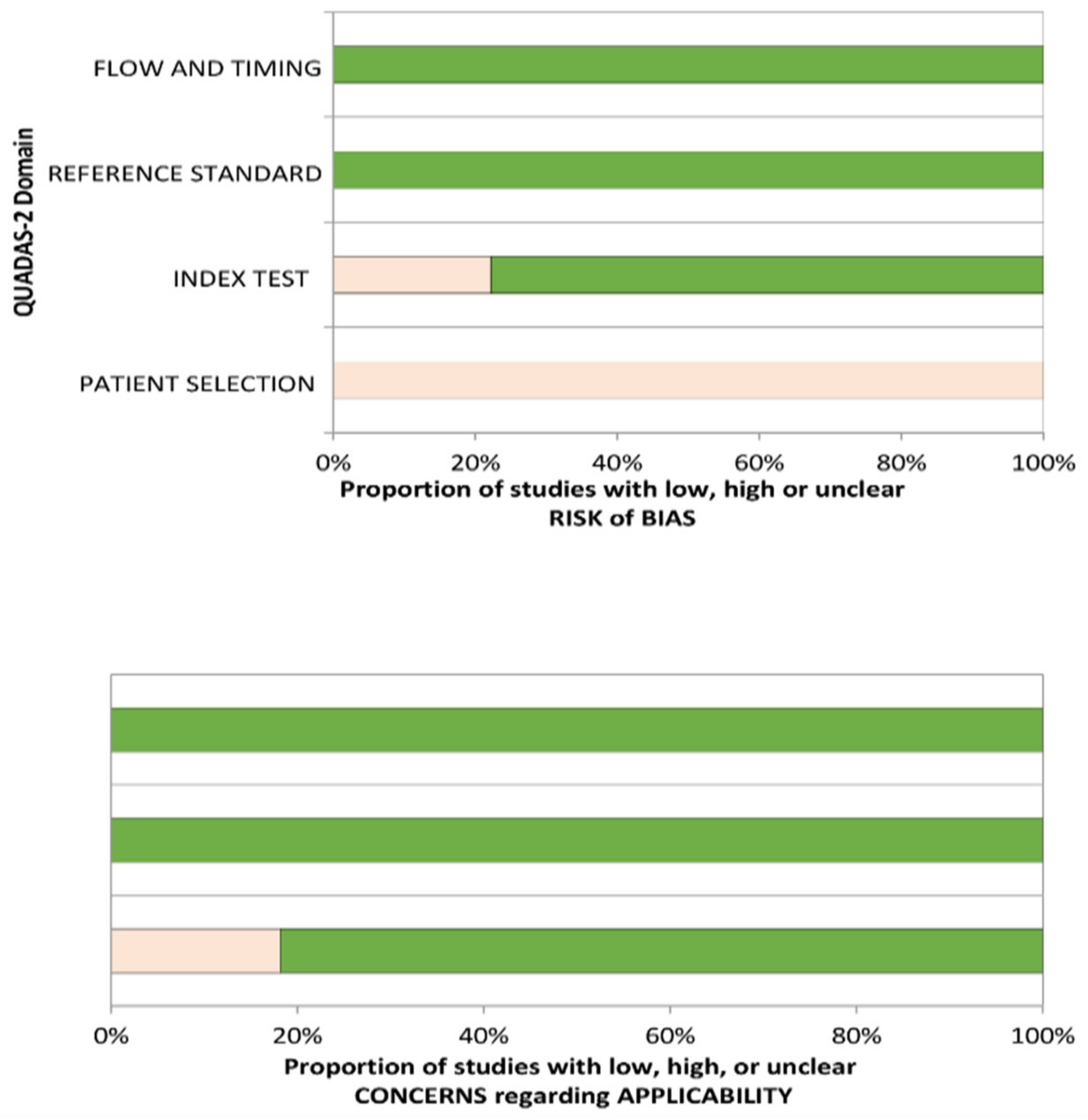
3.3. Assessment of Risk and Applicability
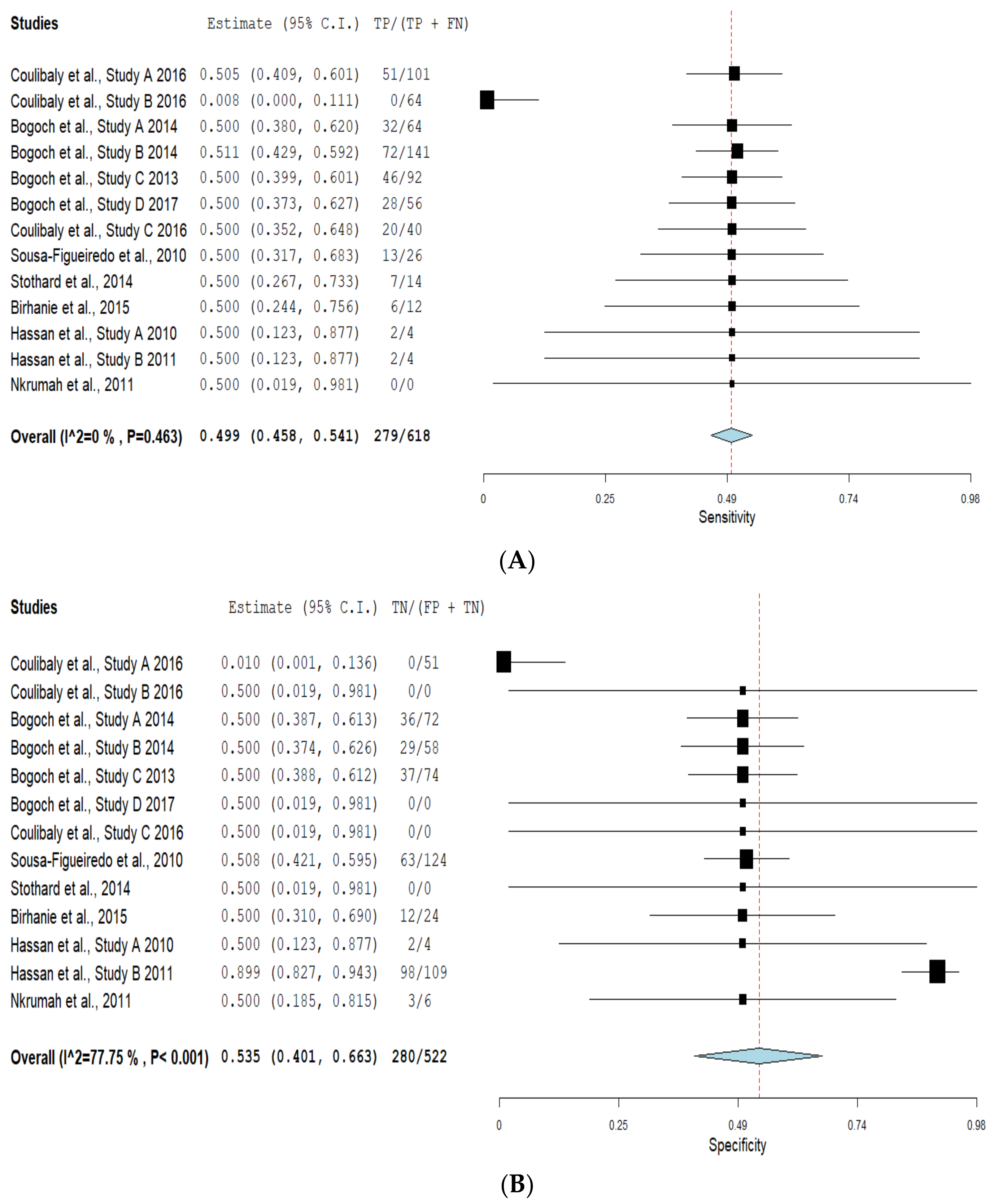
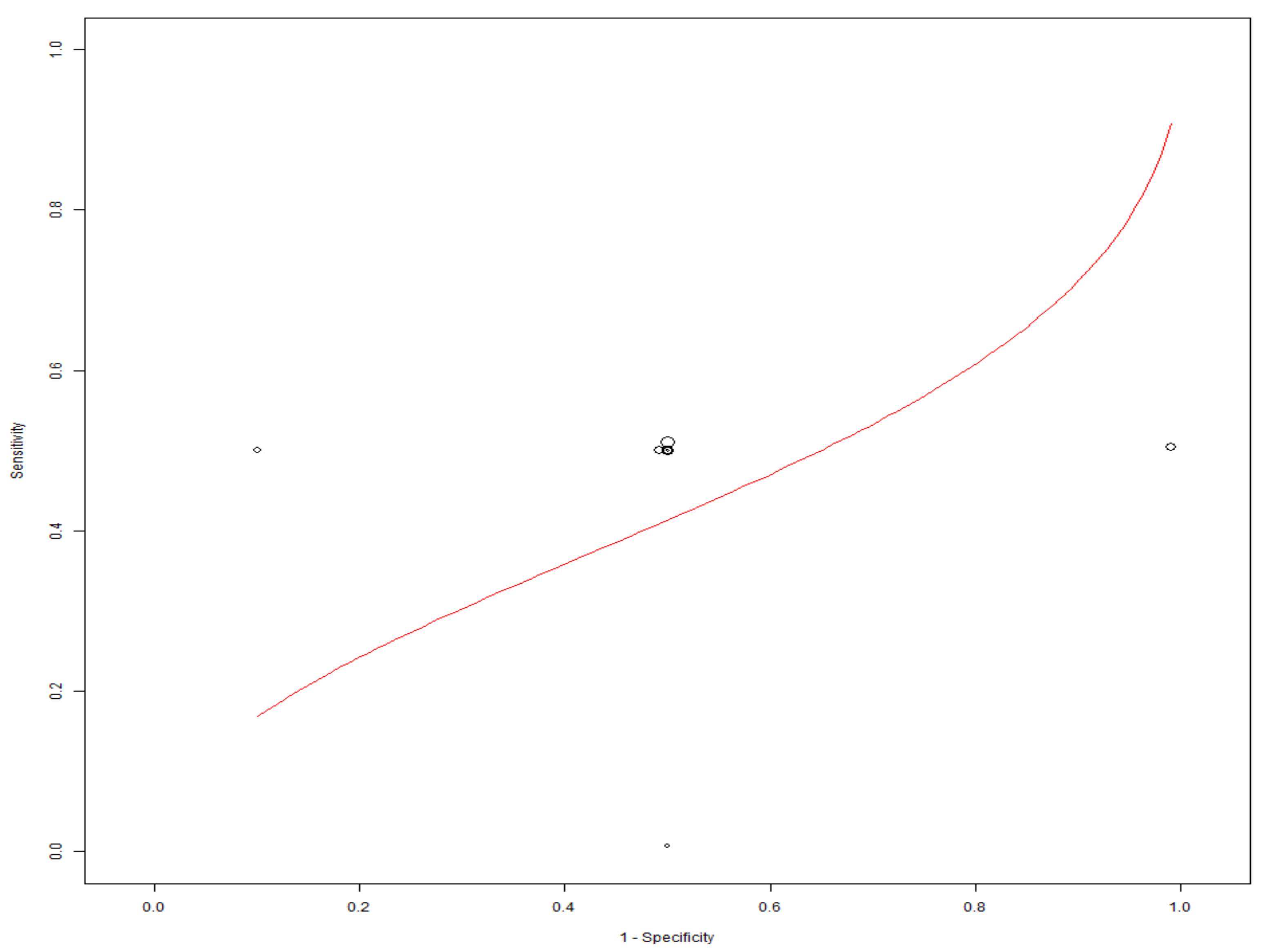
3.4. Diagnostic Accuracy of Mobile-Linked Diagnostic Devices
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Prospero Registration
References
- Wood, C.S.; Thomas, M.R.; Budd, J.; Mashamba-Thompson, T.P.; Herbst, K.; Pillay, D.; Peeling, R.W.; Johnson, A.M.; McKendry, R.A.; Stevens, M.M. Taking connected mobile-health diagnostics of infectious diseases to the field. Nature 2019, 566, 467–474. [Google Scholar] [CrossRef]
- Hardy, V.; O’Connor, Y.; Heavin, C.; Mastellos, N.; Tran, T.; O’Donoghue, J.; Fitzpatrick, A.L.; Ide, N.; Wu, T.-S.J.; Chirambo, G.B.J.T. The added value of a mobile application of Community Case Management on referral, re-consultation and hospitalization rates of children aged under 5 years in two districts in Northern Malawi: Study protocol for a pragmatic, stepped-wedge cluster-randomized controlled trial. Trial 2017, 18, 475. [Google Scholar]
- Smillie, K.; Borek, N.V.; Kop, M.L.v.d.; Lukhwaro, A.; Li, N.; Karanja, S.; Patel, A.R.; Ojakaa, D.; Lester, R.T. Mobile health for early retention in HIV care: A qualitative study in Kenya (WelTel Retain). Afr. J. AIDS Res. 2014, 13, 331–338. [Google Scholar] [CrossRef]
- Nelissen, H.E.; Cremers, A.L.; Okwor, T.J.; Kool, S.; van Leth, F.; Brewster, L.; Makinde, O.; Gerrets, R.; Hendriks, M.E.; Schultsz, C. Pharmacy-based hypertension care employing mHealth in Lagos, Nigeria–a mixed methods feasibility study. BMC Health Serv. Res. 2018, 18, 1–14. [Google Scholar] [CrossRef]
- Alwashmi, M.F. The use of digital health in the detection and management of COVID-19. Int. J. Environ. Res. Health 2020, 17, 2906. [Google Scholar] [CrossRef]
- Cao, Y.; Liu, C.; Liu, B.; Brunette, M.J.; Zhang, N.; Sun, T.; Zhang, P.; Peinado, J.; Garavito, E.S.; Garcia, L.L. Improving tuberculosis diagnostics using deep learning and mobile health technologies among resource-poor and marginalized communities. In Proceedings of the 2016 IEEE first international conference on connected health: Applications, systems and engineering technologies (CHASE), Washington, DC, USA, 27–29 June 2016. [Google Scholar]
- Schwartz, A.B.; Siddiqui, G.; Barbieri, J.S.; Akhtar, A.L.; Kim, W.; Littman-Quinn, R.; Conant, E.F.; Gupta, N.K.; Pukenas, B.A.; Ramchandani, P. The accuracy of mobile teleradiology in the evaluation of chest X-rays. Telemed. Telecare 2014, 20, 460–463. [Google Scholar] [CrossRef]
- Leveille, T.M. Mobile Health and Its Role in Addressing Maternal Health in Sub-Saharan Africa. Master’s Thesis, Clark University, Worcester, MA, USA, 2016. [Google Scholar]
- Zhang, H.; Dimitrov, D.; Simpson, L.; Singh, B.; Plaks, N.; Penney, S.; Charles, J.; Sheehan, R.; Flammini, S.; Murphy, S. A web-based, mobile responsive application to screen healthcare workers for COVID symptoms: Descriptive study. Medrxiv 2020. [Google Scholar] [CrossRef]
- Rao, A.S.S.; Vazquez, J.A. Identification of COVID-19 can be quicker through artificial intelligence framework using a mobile phone–based survey when cities and towns are under quarantine. Infect. Control Hosp. Epidemiol. 2020, 41, 826–830. [Google Scholar] [CrossRef] [PubMed]
- Osei, E.; Mashamba-Thompson, T.P. Mobile health applications for disease screening and treatment support in low-and middle-income countries: A narrative review. Heliyon 2021, 7, e06639. [Google Scholar] [CrossRef]
- Udugama, B.; Kadhiresan, P.; Kozlowski, H.N.; Malekjahani, A.; Osborne, M.; Li, V.Y.; Chen, H.; Mubareka, S.; Gubbay, J.B.; Chan, W.C. Diagnosing COVID-19: The disease and tools for detection. ACS Nano 2020, 14, 3822–3835. [Google Scholar] [CrossRef]
- Yang, T.; Wang, Y.-C.; Shen, C.-F.; Cheng, C.-M. Point-of-care RNA-based diagnostic device for COVID-19. Diagnostics 2020, 10, 165. [Google Scholar] [CrossRef]
- Wang, J.; Du, Y.; Coleman, D.; Peck, M.; Myneni, S.; Kang, H.; Gong, Y. Mobile and Connected Health Technology Needs for Older Adults Aging in Place: Cross-Sectional Survey Study. JMIR Aging 2019, 2, e13864. [Google Scholar] [CrossRef]
- Warshaw, E.M.; Lederle, F.A.; Grill, J.P.; Gravely, A.A.; Bangerter, A.K.; Fortier, L.A.; Bohjanen, K.A.; Chen, K.; Lee, P.K.; Rabinovitz, H.S. Accuracy of teledermatology for nonpigmented neoplasms. J. Am. Acad. Dermatol. 2009, 60, 579–588. [Google Scholar] [CrossRef]
- Šimundić, A.-M. Measures of diagnostic accuracy: Basic definitions. EJIFCC 2009, 19, 203. [Google Scholar]
- Lester, R.; Park, J.J.; Bolten, L.M.; Enjetti, A.; Johnston, J.C.; Schwartzman, K.; Tilahun, B.; von Delft, A. Mobile phone short message service for adherence support and care of patients with tuberculosis infection: Evidence and opportunity. Clin. Tuberc. Other Mycobacter. Dis. 2019, 16, 100108. [Google Scholar] [CrossRef]
- Modena, B.D.; Bellahsen, O.; Nikzad, N.; Chieh, A.; Parikh, N.; Dufek, D.M.; Ebner, G.; Topol, E.J.; Steinhubl, S.J.H. Advanced and accurate mobile health tracking devices record new cardiac vital signs. Hypertension 2018, 72, 503–510. [Google Scholar] [CrossRef]
- Leon, N.; Namadingo, H.; Bobrow, K.; Cooper, S.; Crampin, A.; Pauly, B.; Levitt, N.; Farmer, A. Intervention development of a brief messaging intervention for a randomised controlled trial to improve diabetes treatment adherence in sub-Saharan Africa. BMC Public Health 2021, 21, 1–14. [Google Scholar] [CrossRef]
- Vélez, O.; Okyere, P.B.; Kanter, A.S.; Bakken, S. A usability study of a mobile health application for rural Ghanaian midwives. J. Midwifery Women’s Health 2014, 59, 184–191. [Google Scholar] [CrossRef]
- Nhavoto, J.A.; Grönlund, Å.; Klein, G.O. Mobile health treatment support intervention for HIV and tuberculosis in Mozambique: Perspectives of patients and healthcare workers. PLoS ONE 2017, 12, e0176051. [Google Scholar] [CrossRef]
- Osei, E.; Kuupiel, D.; Vezi, P.N.; Mashamba-Thompson, T.P. Mapping evidence of mobile health technologies for disease diagnosis and treatment support by health workers in sub-Saharan Africa: A scoping review. BMC Med. Inform. Mak. 2021, 21, 1–18. [Google Scholar]
- Choi, S. Powering point-of-care diagnostic devices. Biotechnol. Adv. 2016, 34, 321–330. [Google Scholar] [CrossRef]
- Rasooly, R.; Bruck, H.A.; Balsam, J.; Prickril, B.; Ossandon, M.; Rasooly, A. Improving the sensitivity and functionality of mobile webcam-based fluorescence detectors for point-of-care diagnostics in global health. Diagnostics 2016, 6, 19. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Akay, A.; Wei, H.; Wang, S.; Pingguan-Murphy, B.; Erlandsson, B.-E.; Li, X.; Lee, W.; Hu, J.; Wang, L. Advances in smartphone-based point-of-care diagnostics. Proc. IEEE 2015, 103, 236–247. [Google Scholar] [CrossRef]
- Berg, B.; Cortazar, B.; Tseng, D.; Ozkan, H.; Feng, S.; Wei, Q.; Chan, R.Y.-L.; Burbano, J.; Farooqui, Q.; Lewinski, M. Cellphone-based hand-held microplate reader for point-of-care testing of enzyme-linked immunosorbent assays. ACS Nano 2015, 9, 7857–7866. [Google Scholar] [CrossRef]
- Srinivasan, B.; O’Dell, D.; Finkelstein, J.L.; Lee, S.; Erickson, D.; Mehta, S. ironPhone: Mobile device-coupled point-of-care diagnostics for assessment of iron status by quantification of serum ferritin. Biosens. Bioelectron. 2018, 99, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Van Haelst, R. The Diagnostic Accuracy of Smartphone Applications to Detect Atrial Fibrillation: A Head-to-Head Comparison between Fibricheck and AliveCor. Available online: file:///C:/Users/MDPI/AppData/Local/Temp/%7Bf64e46c5-911e-6356-d131-f3901a3f16ac%7D_Masterproef_Ruth_Van_Haelst.pdf (accessed on 10 June 2021).
- Ahrberg, C.D.; Manz, A.; Neuzil, P. Palm-sized device for point-of-care Ebola detection. Anal. Chem. 2016, 88, 4803–4807. [Google Scholar] [CrossRef]
- Song, J.; Mauk, M.G.; Hackett, B.A.; Cherry, S.; Bau, H.H.; Liu, C. Instrument-free point-of-care molecular detection of Zika virus. J. Anal. Chem. 2016, 88, 7289–7294. [Google Scholar] [CrossRef]
- Zarei, M. Portable biosensing devices for point-of-care diagnostics: Recent developments and applications. TrAC Trends Anal. Chem. 2017, 91, 26–41. [Google Scholar] [CrossRef]
- Bempong, N.-E.; De Castañeda, R.R.; Schütte, S.; Bolon, I.; Keiser, O.; Escher, G.; Flahault, A. Precision Global Health–The case of Ebola: A scoping review. Glob. Health 2019, 9, 010404. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Whiting, P.F.; Rutjes, A.W.; Westwood, M.E.; Mallett, S.; Deeks, J.J.; Reitsma, J.B.; Leeflang, M.M.G.; Sterne, J.A.C.; Bossuyt, P.M.M. The QUADAS-2 Group: A revised tool for the quality assessment of diagnostic accuracy studies. Ann. Intern. Med. 2011, 155, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Wallace, B.C.; Dahabreh, I.J.; Trikalinos, T.A.; Lau, J.; Trow, P.; Schmid, C.H. Closing the gap between methodologists and end-users: R as a computational back-end. J. Stat. Softw. 2012, 49, 1–15. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- Coulibaly, J.T.; Ouattara, M.; D’Ambrosio, M.V.; Fletcher, D.A.; Keiser, J.; Utzinger, J.; N’Goran, E.K.; Andrews, J.R.; Bogoch, I.I. Accuracy of mobile phone and handheld light microscopy for the diagnosis of schistosomiasis and intestinal protozoa infections in Côte d’Ivoire. PLoS Negl. Trop. Dis. 2016, 10, e0004768. [Google Scholar] [CrossRef] [PubMed]
- Coulibaly, J.T.; Ouattara, M.; Keiser, J.; Bonfoh, B.; N’Goran, E.K.; Andrews, J.R.; Bogoch, I.I. Evaluation of malaria diagnoses using a handheld light microscope in a community-based setting in rural Côte d’Ivoire. Am. J. Trop. Med. Hyg. 2016, 95, 831–834. [Google Scholar] [CrossRef] [PubMed]
- Bogoch, I.I.; Koydemir, H.C.; Tseng, D.; Ephraim, R.K.; Duah, E.; Tee, J.; Andrews, J.R.; Ozcan, A. Evaluation of a mobile phone-based microscope for screening of Schistosoma haematobium infection in rural Ghana. Am. J. Trop. Med. Hyg. 2017, 96, 1468–1471. [Google Scholar] [CrossRef] [PubMed]
- Nkrumah, B.; Acquah, S.E.; Ibrahim, L.; May, J.; Brattig, N.; Tannich, E.; Nguah, S.B.; Adu-Sarkodie, Y.; Huenger, F. Comparative evaluation of two rapid field tests for malaria diagnosis: Partec rapid malaria test® and Binax now® malaria rapid diagnostic test. BMC Infect. Dis. 2011, 11, 1–8. [Google Scholar] [CrossRef]
- Sousa-Figueiredo, J.C.; Oguttu, D.; Adriko, M.; Besigye, F.; Nankasi, A.; Arinaitwe, M.; Namukuta, A.; Betson, M.; Kabatereine, N.B.; Stothard, J.R.J.M. Investigating portable fluorescent microscopy (CyScope®) as an alternative rapid diagnostic test for malaria in children and women of child-bearing age. Malar. J. 2010, 9, 1–8. [Google Scholar] [CrossRef]
- Stothard, J.R.; Nabatte, B.; Sousa-Figueiredo, J.C.; Kabatereine, N.B. Towards malaria microscopy at the point-of-contact: An assessment of the diagnostic performance of the Newton Nm1 microscope in Uganda. J. Parasitol. 2014, 141, 1819. [Google Scholar] [CrossRef]
- Hassan, S.E.-D.H.; Abd Elrahium, D.H.; Mohammed-Elhassan, E.B.; Malik, E.M.; Adam, I. Fluorescence microscope (Cyscope®) for malaria diagnosis in pregnant women in Medani Hospital, Sudan. Diagn. Pathol. 2011, 6, 1–5. [Google Scholar] [CrossRef]
- Hassan, S.E.-D.H.; Okoued, S.I.; Mudathir, M.A.; Malik, E.M. Testing the sensitivity and specificity of the fluorescence microscope (Cyscope®) for malaria diagnosis. Malar. J. 2010, 9, 1–4. [Google Scholar] [CrossRef]
- Bogoch, I.I.; Andrews, J.R.; Speich, B.; Utzinger, J.; Ame, S.M.; Ali, S.M.; Keiser, J. Mobile phone microscopy for the diagnosis of soil-transmitted helminth infections: A proof-of-concept study. Am. J. Trop. Med. Hyg. 2013, 88, 626–629. [Google Scholar] [CrossRef]
- Birhanie, M. Comparison of Partec rapid malaria test with conventional light microscopy for diagnosis of malaria in Northwest Ethiopia. J. Parasitol. Res. 2016, 3479457. [Google Scholar] [CrossRef][Green Version]
- World Health Organization. Prevention and Control of Schistosomiasis and Soil-Transmitted Helminthiasis: Report of a WHO Expert Committee; World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- Koydemir, H.C.; Feng, S.; Liang, K.; Nadkarni, R.; Benien, P.; Ozcan, A. Comparison of supervised machine learning algorithms for waterborne pathogen detection using mobile phone fluorescence microscopy. Nanophotonics 2017, 6, 731–741. [Google Scholar] [CrossRef]
- Holmström, O.; Linder, N.; Ngasala, B.; Mårtensson, A.; Linder, E.; Lundin, M.; Moilanen, H.; Suutala, A.; Diwan, V.; Lundin, J. Point-of-care mobile digital microscopy and deep learning for the detection of soil-transmitted helminths and Schistosoma haematobium. Glob. Health Action 2017, 10, 1337325. [Google Scholar] [CrossRef]
- Sowerby, S.J.; Crump, J.A.; Johnstone, M.C.; Krause, K.L.; Hill, P.C. Smartphone microscopy of parasite eggs accumulated into a single field of view. Am. J. Trop. Med. Hyg. 2016, 94, 227–230. [Google Scholar] [CrossRef]
- Rosado, L.; Da Costa, J.M.C.; Elias, D.; Cardoso, J.S. Mobile-based analysis of malaria-infected thin blood smears: Automated species and life cycle stage determination. Sensors 2017, 17, 2167. [Google Scholar] [CrossRef]
- Slusarewicz, P.; Pagano, S.; Mills, C.; Popa, G.; Chow, K.M.; Mendenhall, M.; Rodgers, D.W.; Nielsen, M.K. Automated parasite faecal egg counting using fluorescence labelling, smartphone image capture and computational image analysis. Int. J. Parasitol. 2016, 46, 485–493. [Google Scholar] [CrossRef]
- LaBounty, T.M.; Kim, R.J.; Lin, F.Y.; Budoff, M.J.; Weinsaft, J.W.; Min, J.K. Diagnostic accuracy of coronary computed tomography angiography as interpreted on a mobile handheld phone device. JACC Cardiovasc. Imaging 2010, 3, 482–490. [Google Scholar] [CrossRef]



| Determinants | Description |
|---|---|
| P-Population | Diseases such as communicable and non-communicable ones |
| I-Intervention | Type of mobile-linked POC diagnostics |
| C-Comparison | Other forms of diagnostic devices |
| O-Outcome | Diagnostic accuracy is defined as the actual results that contain both true positives (sensitivity) and true negatives (specificity) of a disease condition in a population [15]. |
| Author and Date | Country of Study | Aim of the Study | Geographical Setting (Urban/Semi-urban/Rural) | Study Setting | Study Design | Study Population (Diseases) | Type of mHealth Devices | Other Diagnostic Devices (Gold Standard) | Sample Size |
|---|---|---|---|---|---|---|---|---|---|
| Coulibaly et al., 2016a [41] | Côte d’Ivoire | To compare the accuracy of mobile phone and handheld devices to that of light microscopy to diagnose Schistosoma haematobium, S. mansoni, and intestinal protozoa infections in a community-based survey | Rural | Grand Moutcho community | Cross-sectional survey | Schistosoma haematobium Schistosoma mansoni, and Intestinal Protozoa Infections | Newton Nm1 reversed lens CellScope | Olympus Cx21 microscope | 226 |
| Bogoch et al., 2014 [42] | Côte d’Ivoire | To examine the utility of a novel commercial, portable light microscope and a simple mobile phone microscope to diagnose S. mansoni, S. haematobium, and soil-transmitted helminths. | Rural | Azaguié Makouguié | Cohort study | Schistosoma mansoni, Schistosoma haematobium and Soil-transmitted helminths | iPhone add-on, Newton Nm1 | Olympus Cx21 microscope | 180 |
| Nkrumah et al., 2011 [43] | Ghana | To compare the novel Partec Rapid Malaria Test and the Binax Now Malaria Rapid Diagnostic Test with conventional Giemsa stain microscopy for malaria diagnosis in children at the clinical laboratory of a health facility in a rural endemic area of Ghana | Rural | Agogo Presbyterian hospital | Cross-sectional survey | Malaria (Plasmodium falciparum) | CyScope | Thick Giemsa Smear | 263 |
| Bogoch et al., 2017 [44] | Ghana | To test the performance of the handheld microscope in the diagnosis of Schistosoma. | Rural | Sorodofo–Abaasa Village | Cross-sectional survey | Schistosoma haematobium | Novel Mobile phone microscope | Olympus Cx21 microscope | 60 |
| Stothard et al., 2014 [45] | Uganda | To assess the diagnostic performance of the Newton Nm1 microscope towards malaria microscopy | Urban | Kampala | Cross-sectional study | Malaria (Plasmodium spp.) | Newton Nm1 | Olympus Cx22 microscope | 50 |
| Sousa-Figueiredo et al., 2010 [46] | Uganda | To assess the diagnostic performance of the CyScope microscope and the lateral-flow Paracheck-Pf test as RDTs for malaria in children under five and in women | Rural | Bugoigo, Walukuba, Piida, Bugoto, Bukoba, Lwanika | Cross-sectional survey | Malaria (Plasmodium spp.) | CyScope | Thick Giemsa Smear | 1530 |
| Hassan et al., 2011 [47] | Sudan | To compare the performance of the CyScope fluorescence microscope with that of Giemsa-stained light microscopy for the diagnosis of malaria among pregnant women | Urban | Medani Maternity hospital | Cross-sectional study | Malaria (Plasmodium falciparum) | CyScope | Thick Giemsa Smear | 128 |
| Hassan et al., 2010 [48] | Sudan | To examine the specificity and sensitivity of the CyScope microscope compared to the gold standard of light microscopy | Urban | Sinnar hospital | Cross-sectional study | Malaria (Plasmodium falciparum) | CyScope | Thick Giemsa Smear | 293 |
| Bogoch et al., 2013 [49] | Tanzania | To compare the diagnostic accuracy of our mobile phone microscope with that of conventional light microscopy | Rural | Pemba Island | Cross-sectional survey | Trichuris trichiura | iPhone add-on | Olympus Cx21 microscope | 199 |
| Birhanie et al., 2015 [50] | Ethiopia | To assess the diagnostic performance of the Partec rapid malaria test regarding light microscopy for the diagnosis of malaria in Northwest Ethiopia | Rural | Gendewuha health center | Cross-sectional study | Malaria (Plasmodium spp.) | CyScope | Thick Giemsa Smear | 180 |
| Coulibaly et al., 2016b [51] | Côte d’Ivoire | To evaluate the “real-world” diagnostic operating characteristics of a handheld light microscope with mobile phone attachment integrated into a community-based screening program for malaria in rural Côte d’Ivoire | Rural | Grand Moutcho community | Cross-sectional survey | Malaria (Plasmodium falciparum) | Newton Nm1 | Olympus Cx22 microscope | 223 |
| Risk of Bias | Applicability Concerns | ||||||
|---|---|---|---|---|---|---|---|
| Author and Year of Publication | Patient Selection | Index Test | Reference Standard | Flow and Timing | Patient Selection | Index Test | Reference Standard |
| Bogoch et al., 2014 |  |  |  |  |  |  |  |
| Coulibaly et al., 2016a |  |  |  |  |  |  |  |
| Coulibaly et al., 2016b |  |  |  |  |  |  |  |
| Bogoch et al., 2017 |  |  |  |  |  |  |  |
| Stothard et al., 2014 |  |  |  |  |  |  |  |
| Bogoch et al., 2013 |  |  |  |  |  |  |  |
| Sousa-Figueiredo et al., 2010 |  |  |  |  |  |  |  |
| Birhanie et al., 2015 |  |  |  |  |  |  |  |
| Hassan et al., 2010 |  |  |  |  |  |  |  |
| Hassan et al., 2011 |  |  |  |  |  |  |  |
| Nkrumah et al., 2011 |  |  |  |  |  |  |  |
 Low Risk;
Low Risk;  High Risk; ? Unclear Risk.
High Risk; ? Unclear Risk.| Mobile Phone Microscope/CyScope | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Author, Date | Disease | Sensitivity (95% CI) | Specificity (95% CI) | PPV (95% CI) | NPV (95% CI) | TP (95% CI) | FP (95% CI) | TN (95% CI) | FN (95% CI) |
| Coulibaly et al., 2016a | Schistosoma mansoni | 50.0 (25.4–74.6) | 99.5 (97.0–100) | 85.7 (42.0–99.2) | 97.3 (93.9–98.9) | 51.0 | 0.5 | 0.51 | 50 |
| Schistosoma haematobium | 35.6 (25.9–46.4) | 100 (96.6–100) | 100 (86.7–100) | 70.1 (63.1–76.3) | 66.2 | 0.0 | 0.0 | 64.4 | |
| Bogoch et al., 2014a | Schistosoma mansoni | 68.2 (60.1–75.5) | 64.3 (35.1–87.2) | 95.4 (89.5–98.5) | 15.8 (7.5–27.9) | 32.2 | 35.7 | 36.2 | 31.8 |
| Trichuris trichiura | 30.8 (19.9–43.4) | 71.0 (61.1–79.6) | 40.8 (27.0–55.8) | 61.2 (51.7–70.1) | 71.5 | 29.0 | 29.0 | 69.2 | |
| Bogoch et al., 2013 | Trichuris trichiura | 54.4(46.3–62.3) | 63.4 (46.9–77.4) | 85.1 (76.4–91.2) | 26.5 (18.4–36.6) | 46.4 | 36.6 | 37.2 | 45.6 |
| Bogoch et al., 2017 | Schistosoma haematobium | 72.1 (56.1–84.2 | 100.0 (75.9–100.0) | 100.0 (86.3–100.0) | 57.1 (37.4–75.0) | 28.3 | 0.0 | 0.0 | 27.9 |
| Coulibaly et al., 2016b | Malaria | 80.2 (73.1–85.9) | 100 (92.6–100.0), | 100 (96.4–100.0) | 65.6 (54.9–74.9) | 20.0 | 0.0 | 0.0 | 19.8 |
| Sousa-Figueiredo et al., 2010 | Malaria | 86.7 (79.3–92.2) | 38.8 (33.6–44.1) | 32.8 (27.7–38.3) | 89.4 (83.4–93.8) | 13.3 | 61.2 | 62.8 | 13.3 |
| Stothard et al., 2014 | Malaria | 93.5 (78.6–99.2) | 100 (82.4–100) | 100 (88.1–100) | 90.5 (69.6–98.8) | 6.5 | 0.0 | 0.0 | 6.5 |
| Birhanie et al., 2015 | Malaria | 93.8 (87.1–100) | 87.9 (79.7–96.1) | 86.4 (77.2–95.5) | 94.6 (88.7–100) | 6.3 | 12.1 | 12.2 | 6.2 |
| Hassan et al., 2010 | Malaria | 98.2 (90.6–100) | 98.3 (95.7–99.5) | 93.3 (83.8–98.2) | 99.6 (97.6–100) | 1.8 | 1.7 | 1.72 | 1.8 |
| Hassan et al., 2011 | Malaria | 97.6 (92.2–99.6) | 89.1 (77.5–95.9) | 94.1 (87.4–97.8) | 95.3 (85.4–99.2) | 2.43 | 10.9 | 98.2 | 2.4 |
| Nkrumah et al., 2011 | Malaria | 100 (96.6–100) | 97.4 (93.6–99.3) | 96.4 (91–99) | 100 (97.6–100) | 0.0 | 2.6 | 2.63 | 0.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Osei, E.; Nkambule, S.J.; Vezi, P.N.; Mashamba-Thompson, T.P. Systematic Review and Meta-Analysis of the Diagnostic Accuracy of Mobile-Linked Point-of-Care Diagnostics in Sub-Saharan Africa. Diagnostics 2021, 11, 1081. https://doi.org/10.3390/diagnostics11061081
Osei E, Nkambule SJ, Vezi PN, Mashamba-Thompson TP. Systematic Review and Meta-Analysis of the Diagnostic Accuracy of Mobile-Linked Point-of-Care Diagnostics in Sub-Saharan Africa. Diagnostics. 2021; 11(6):1081. https://doi.org/10.3390/diagnostics11061081
Chicago/Turabian StyleOsei, Ernest, Sphamandla Josias Nkambule, Portia Nelisiwe Vezi, and Tivani P. Mashamba-Thompson. 2021. "Systematic Review and Meta-Analysis of the Diagnostic Accuracy of Mobile-Linked Point-of-Care Diagnostics in Sub-Saharan Africa" Diagnostics 11, no. 6: 1081. https://doi.org/10.3390/diagnostics11061081
APA StyleOsei, E., Nkambule, S. J., Vezi, P. N., & Mashamba-Thompson, T. P. (2021). Systematic Review and Meta-Analysis of the Diagnostic Accuracy of Mobile-Linked Point-of-Care Diagnostics in Sub-Saharan Africa. Diagnostics, 11(6), 1081. https://doi.org/10.3390/diagnostics11061081







