A Systematic Review of the Inclusion of Non-Inflammatory Ultrasonographic Enthesopathy Findings in Enthesitis Scoring Indices
Abstract
1. Introduction
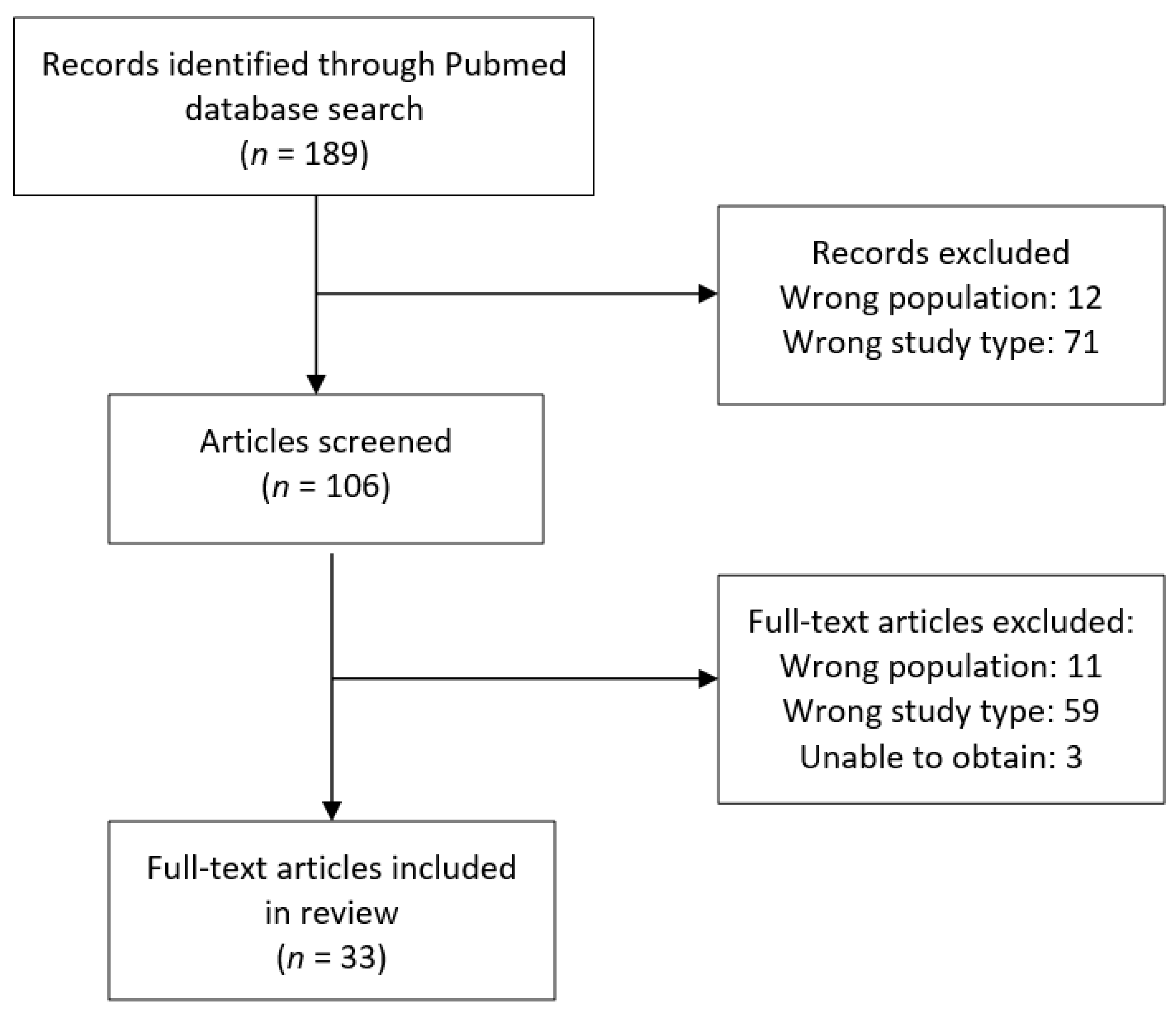
2. Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kamel, M.; Eid, H.; Mansour, R. Ultrasound detection of heel enthesitis: A comparison with magnetic resonance imaging. J. Rheumatol. 2003, 30, 774–778. [Google Scholar]
- D’Agostino, M.-A.; Breban, M. Ultrasonography in inflammatory joint disease: Why should rheumatologists pay attention? Jt. Bone Spine 2002, 69, 252–255. [Google Scholar] [CrossRef]
- Grassi, W.; Salaffi, F.; Filippucci, E. Ultrasound in rheumatology. Best Pract. Res. Clin. Rheumatol. 2005, 19, 467–485. [Google Scholar] [CrossRef] [PubMed]
- D’Agostino, M.A. Ultrasound imaging in spondyloarthropathies. Best Pract. Res. Clin. Rheumatol. 2010, 24, 693–700. [Google Scholar] [CrossRef] [PubMed]
- Grassi, W.; Filippucci, E.; Farina, A.; Cervini, C. Sonographic imaging of tendons. Arthritis Rheum. 2000, 43, 969–976. [Google Scholar] [CrossRef]
- Aagesen, A.L.; Melek, M. Choosing the Right Diagnostic Imaging Modality in Musculoskeletal Diagnosis. Prim. Care Clin. Off. Pract. 2013, 40, 849–861. [Google Scholar] [CrossRef]
- Grechenig, W.; Clement, H.; Bratschitsch, G.; Fankhauser, F.; Peicha, G. Sonographische Achillessehnendiagnostik [Ultrasound diagnosis of the Achilles tendon]. Orthopade 2002, 31, 319–325. [Google Scholar] [CrossRef]
- Carroll, M.; Dalbeth, N.; Boocock, M.; Rome, K. The assessment of lesions of the Achilles tendon by ultrasound imaging in inflammatory arthritis: A systematic review and meta-analysis. Semin. Arthritis Rheum. 2015, 45, 103–114. [Google Scholar] [CrossRef]
- Paavola, M.; Paakkala, T.; Kannus, P.; Järvinen, M. Ultrasonography in the differential diagnosis of Achilles tendon injuries and related disorders. A comparison between pre-operative ultrasonography and surgical findings. Acta Radiol. 1998, 39, 612–619. [Google Scholar] [CrossRef]
- Lampman, J.H. Origin of enthesopathy. J. Rheumatol. 1985, 12, 1030–1031. [Google Scholar]
- Kehl, A.S.; Orr, M.; Weisman, M.H. Enthesitis: New insights into pathogenesis, diagnostic modalities and treatment. Arthritis Rheumatol. 2016, 68, 312–322. [Google Scholar] [CrossRef] [PubMed]
- McGonagle, D.; Gibbon, W.; Emery, P. Classification of inflammatory arthritis by enthesitis. Lancet 1998, 352, 1137–1140. [Google Scholar] [CrossRef]
- D’Agostino, M.-A.; Olivieri, I. Enthesitis. Best Pract. Res. Clin. Rheumatol. 2006, 20, 473–486. [Google Scholar] [CrossRef]
- D’Agostino, M.-A.; Said-Nahal, R.; Brasseur, J.-L.; Dougados, M.; Breban, M. Assessment of peripheral enthesitis in the spondylarthropathies by ultrasonography combined with power Doppler: A cross-sectional study. Arthritis Rheum. 2003, 48, 523–533. [Google Scholar] [CrossRef]
- D’Agostino, M.A.; Aegerter, P.; Bechara, K.; Salliot, C.; Judet, O.; Chimenti, M.S.; Monnet, D.; le Parc, J.-M.; Landais, P.; Breban, M. How to diagnose spondyloarthritis early? Accuracy of peripheral enthesitis detection by power Doppler ultrasonography. Ann. Rheum. Dis. 2011, 70, 1433–1440. [Google Scholar] [CrossRef]
- Mease, P.J. Measures of psoriatic arthritis: Tender and Swollen Joint Assessment, Psoriasis Area and Severity Index (PASI), Nail Psoriasis Severity Index (NAPSI), Modified Nail Psoriasis Severity Index (mNAPSI), Mander/Newcastle Enthesitis Index (MEI), Leeds Enthesit. Arthritis Rheum. 2011, 63, S64–S85. [Google Scholar] [CrossRef] [PubMed]
- Enthesitis and Enthesopathy. An Evolving Understanding of the Enthesis. 12 October 2014. Available online: Enthuses.info/anatomy/traditional_concept.html (accessed on 10 January 2021).
- Sudoł-Szopińska, I.; Kwiatkowska, B.; Prochorec-Sobieszek, M.; Maśliński, W. Enthesopathies and enthesitis. Part 1. Etiopathogenesis. J. Ultrason. 2015, 15, 72–84. [Google Scholar] [CrossRef]
- Valouch, P.; Pazderka, V.; Gatterova, J. Enthesopathy of the hip joint. Clin. Rheumatol. 1985, 4, 150–154. [Google Scholar] [CrossRef]
- Niepel, G.; Kostka, D.; Kopecky, S. Enthesopathy. Acta Rheumatol. Balneol. Pist. 1966, 1, 1–64. [Google Scholar]
- Niepel, G.; Sitaj, S. Enthesopathy. Clin. Rheum. Dis. 1979, 5, 857–872. [Google Scholar]
- Ball, J. Enthesopathy of rheumatoid and ankylosing spondylitis. Ann. Rheum. Dis. 1971, 30, 213–223. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, A.M.; Petty, R.E. A syndrome of seronegative enthesopathy and arthropathy in children. Arthritis Rheum. 1982, 25, 1041–1047. [Google Scholar] [CrossRef] [PubMed]
- Dougados, M.; van der Linden, S.; Juhlin, R.; Huitfeldt, B.; Amor, B.; Calin, A.; Cats, A.; Dijkmans, B.; Olivieri, I.; Pasero, G.; et al. The European Spondyloarthropathy Study Group preliminary criteria for the classification of spondyloarthropathy. Arthritis Rheum. 1991, 34, 1218–1227. [Google Scholar] [CrossRef]
- Stone, W.L.; Basit, H.; Burns, B. Pathology, Inflammation; StatPearls Publishing: Treasure Island, FL, USA, 2020. Available online: https://www.ncbi.nlm.nih.gov/books/NBK534820/ (accessed on 30 January 2021).
- Almekinders, L.C.; Temple, J.D. Etiology, diagnosis, and treatment of tendonitis: An analysis of the literature. Med. Sci. Sports Exerc. 1998, 30, 1183–1190. [Google Scholar] [CrossRef]
- Mascarenhas, S. A Narrative Review of the Classification and Use of Diagnostic Ultrasound for Conditions of the Achilles Tendon. Diagnostics 2020, 10, 944. [Google Scholar] [CrossRef]
- Mander, M.; Simpson, J.M.; McLellan, A.; Walker, D.A.; Goodacre, J.; Dick, W.C. Studies with an enthesis index as a method of clinical assessment in ankylosing spondylitis. Ann. Rheum. Dis. 1987, 46, 197–202. [Google Scholar] [CrossRef]
- Klauser, A.S.; Wipfler, E.; Dejaco, C.; Moriggl, B.; Duftner, C.; Schirmer, M. Diagnostic values of history and clinical examination to predict ultrasound signs of chronic and acute enthesitis. Clin. Exp. Rheumatol. 2008, 26, 548–553. [Google Scholar] [PubMed]
- Milutinovic, S.; Radunovic, G.; Veljkovic, K.; Zlatanovic, M.; Svenda, M.Z.; Radak, M.P.; Dolijanovic, S.P.; Stojic, B.; Damjanov, N. Development of ultrasound enthesitis score to identify patients with enthesitis having spondyloarthritis: Prospective, double-blinded, controlled study. Clin. Exp. Rheumatol. 2015, 33, 812–817. [Google Scholar]
- Balint, P.V.; Kane, D.; Wilson, H.; McInnes, I.B.; Sturrock, R.D. Ultrasonography of entheseal insertions in the lower limb in spondyloarthropathy. Ann. Rheum. Dis. 2002, 61, 905–910. [Google Scholar] [CrossRef]
- de Miguel, E.; Cobo, T.; Muñoz-Fernández, S.; Naredo, E.; Usón, J.; Acebes, J.C.; Andréu, J.L.; Martín-Mola, E. Validity of enthesis ultrasound assessment in spondyloarthropathy. Ann. Rheum. Dis. 2009, 68, 169–174. [Google Scholar] [CrossRef]
- Heuft-Dorenbosch, L.; Spoorenberg, A.; van Tubergen, A.; Landewé, R.; Tempel, H.V.V.; Mielants, H.; Dougados, M.; van der Heijde, D. Assessment of enthesitis in ankylosing spondylitis. Ann. Rheum. Dis. 2003, 62, 127–132. [Google Scholar] [CrossRef]
- Maksymowych, W.P.; Mallon, C.; Morrow, S.; Shojania, K.; Olszynski, W.P.; Wong, R.L.; Sampalis, J.; Conner-Spady, B. Development and validation of the Spondyloarthritis Research Consortium of Canada (SPARCC) Enthesitis Index. Ann. Rheum. Dis. 2008, 68, 948–953. [Google Scholar] [CrossRef] [PubMed]
- Healy, P.J.; Helliwell, P.S. Measuring clinical enthesitis in psoriatic arthritis: Assessment of existing measures and development of an instrument specific to psoriatic arthritis. Arthritis Rheum. 2008, 59, 686–691. [Google Scholar] [CrossRef]
- Bigeleisen, P.E.; Gofeld, M.; Orebaugh, S.L. Ultrasound-Guided Regional Anesthesia and Pain Medicine; Bigeleisen, P.E., Ed.; Lippincott Williams and Wilkins: London, UK, 2010. [Google Scholar]
- Kainberger, F.M.; Engel, A.; Barton, P.; Huebsch, P.; Neuhold, A.; Salomonowitz, E. Injury of the Achilles tendon: Diagnosis with sonography. Am. J. Roentgenol. 1990, 155, 1031–1036. [Google Scholar] [CrossRef]
- El-Khalek, A.M.A.; Borga, M.; El-Essawya, S.; El Sallab, R.M.; Ezzata, A. Role of ultrasonography in the evaluation of Achilles tendon disorders. Benha Med. J. 2016, 33, 54. [Google Scholar] [CrossRef]
- Sudoł-Szopińska, I.; Kwiatkowska, B.; Prochorec-Sobieszek, M.; Pracoń, G.; Walentowska-Janowicz, M.; Maslinski, W. Enthesopathies and enthesitis. Part 2: Imaging studies. J. Ultrason. 2015, 15, 196–207. [Google Scholar] [CrossRef]
- Shaibani, A.; Workman, R.; Rothschild, B.M. The significance of enthesopathy as a skeletal phenomenon. Clin. Exp. Rheumatol. 1993, 11, 399–403. [Google Scholar]
- Gencc, H.; Cakit, B.D.; Tuncbilek, I.; Erdem, H.R.; Tuncbilek, I. Ultrasonographic evaluation of tendons and enthesal sites in rheumatoid arthritis: Comparison with ankylosing spondylitis and healthy subjects. Clin. Rheumatol. 2004, 24, 272–277. [Google Scholar] [CrossRef]
- Hardcastle, S.A.; Dieppe, P.; Gregson, C.L.; Arden, N.K.; Spector, T.D.; Hart, D.J.; Edwards, M.H.; Dennison, E.M.; Cooper, C.; Williams, M.; et al. Osteophytes, enthesophytes, and high bone mass: A bone-forming triad with potential relevance in osteoarthritis. Arthritis Rheumatol. 2014, 66, 2429–2439. [Google Scholar] [CrossRef] [PubMed]
- Abraham, A.M.; Goff, I.; Pearce, M.S.; Francis, R.M.; Birrell, F. Reliability and validity of ultrasound imaging of features of knee osteoarthritis in the community. BMC Musculoskelet. Disord. 2011, 12, 70. [Google Scholar] [CrossRef]
- Poulain, C.; D’Agostino, M.A.; Thibault, S.; Daures, J.P.; Ferkal, S.; le Corvoisier, P.; Rahmouni, A.; Loeuille, D.; Dougados, M.; Claudepierre, P. Can power Doppler ultrasound of the entheses help in classifying recent axial spondyloarthritis? Data from the DESIR cohort. RMD Open 2018, 4, e000686. [Google Scholar] [CrossRef]
- Kiris, A.; Kaya, A.; Ozgocmen, S.; Kocakoc, E. Assessment of enthesitis in ankylosing spondylitis by power Doppler ultrasonography. Skelet. Radiol. 2006, 35, 522–528. [Google Scholar] [CrossRef]
- Balint, P.V.; Terslev, L.; Aegerter, P.; Bruyn, G.A.W.; Chary-Valckenaere, I.; Gandjbakhch, F.; Iagnocco, A.; Jousse-Joulin, S.; Möller, I.; Naredo, E.; et al. Reliability of a consensus-based ultrasound definition and scoring for enthesitis in spondyloarthritis and psoriatic arthritis: An OMERACT US initiative. Ann. Rheum. Dis. 2018, 77, 1730–1735. [Google Scholar] [CrossRef]
- Elalouf, O.; Ureyen, S.B.; Touma, Z.; Anderson, M.; Kaeley, G.S.; Aydin, S.Z.; Eder, L. Psoriatic Arthritis Sonographic Enthesitis Instruments: A Systematic Review of the Literature. J. Rheum. 2019, 46, 43–56. [Google Scholar] [CrossRef]
- Zuliani, F.; Zabotti, A.; Errichetti, E.; Tinazzi, I.; Zanetti, A.; Carrara, G.; Quartuccio, L.; Sacco, S.; Giovannini, I.; Stinco, G.; et al. Ultrasonographic detection of subclinical enthesitis and synovitis: A possible stratification of psoriatic patients without clinical musculoskeletal involvement. Clin. Exp. Rheumatol. 2019, 37, 593–599. [Google Scholar] [PubMed]
- Hartung, W.; Nigg, A.; Strunk, J.; Wolff, B. Clinical assessment and ultrasonography in the follow-up of enthesitis in patients with spondyloarthritis: A multicenter ultrasound study in daily clinical practice. Open Access Rheumatol. Res. Rev. 2018, 10, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Florescu, A.; Vere, C.C.; Florescu, L.M.; Mușetescu, A.E.; Bondari, A.; Ciurea, P.L. Clinical and Ultrasound Assessment of Enthesis in Psoriatic Arthritis in a Romanian Cohort. Curr. Health Sci. J. 2018, 44, 347–351. [Google Scholar] [CrossRef]
- Milutinovic, S.; Radunovic, G.; Veljkovic, K.; Zlatanovic, M.; Damjanov, N. Construct validity and sensitivity to change of Belgrade Ultrasound Enthesitis Score in patients with spondyloarthritis: A pilot study. Rheumatol. Int. 2018, 38, 383–391. [Google Scholar] [CrossRef]
- Yadav, A.; Mehra, N.; Pal, S.; Hlawndo, J.; Sachdev, N.; Yadav, T.P. Evaluation of enthesitis in patients with juvenile idiopathic arthritis by power color and spectral Doppler ultrasonography. Eur. J. Rheumatol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Liang, J.; Qiu, J.; Wang, F.; Sun, L. Ultrasonographic evaluation of enthesitis in patients with ankylosing spondylitis. J. Biomed. Res. 2017, 31, 162–169. [Google Scholar] [CrossRef]
- Alhussain, F.A.; Gunal, E.K.; Kurum, E.; Bakirci, S.; Ozturk, A.B.; McGonagle, D.; Aydin, S.Z. Greater magnitude of entheseal microdamage and repair in psoriatic arthritis compared with ankylosing spondylitis on ultrasound. Rheumatology 2019, 58, 299–303. [Google Scholar] [CrossRef] [PubMed]
- Moshrif, A.; Mosallam, A.; Mohamed, E.E.M.; Gouda, W.; Doma, M. Subclinical enthesopathy in patients with psoriasis and its association with other disease parameters: A power Doppler ultrasonographic study. Eur. J. Rheumatol. 2017, 4, 24–28. [Google Scholar] [CrossRef] [PubMed]
- Collada, J.M.; Macía-Villa, C.; Plasencia, C.; Álvaro-Gracia, J.M.; de Miguel, E. Doppler enthesitis: A potential useful outcome in the assessment of axial spondyloarthritis and psoriatic arthritis. Clin. Rheumatol. 2020. [Google Scholar] [CrossRef]
- Vyas, K.; Jain, S.K.; Mittal, A.; Kumar, R.; Saxena, S.; Malviya, S. Sonographic Evaluation of Subclinical Enthesopathy in Patients of Chronic Plaque Psoriasis. Indian Dermatol. Online J. 2020, 11, 580–585. [Google Scholar] [CrossRef] [PubMed]
- Macía-Villa, C.; Falcao, S.; Gutierrez, M.; Medina, J.; Hammer, H.B.; de Miguel, E. Peritenon extensor tendon inflammation in psoriatic arthritis is an enthesitis-related lesion. J. Rheumatol. 2019, 46, 1295–1298. [Google Scholar] [CrossRef]
- Ishida, S.N.; Furtado, R.N.V.; Rosenfeld, A.; Proglhof, J.E.P.; Estrela, G.B.Q.; Natour, J. Ultrasound of entheses in ankylosing spondylitis patients: The importance of the calcaneal and quadriceps entheses for differentiating patients from healthy individuals. Clinics 2019, 74, e727. [Google Scholar] [CrossRef]
- Wervers, K.; Herrings, I.; Luime, J.J.; Tchetverikov, I.; Gerards, A.H.; Hazes, J.M.W.; Vis, M. Association of physical activity and medication with enthesitis on ultrasound in psoriatic arthritis. J. Rheumatol. 2019, 46, 1290–1294. [Google Scholar] [CrossRef]
- Wervers, K.; Vis, M.; Rasappu, N.; van der Ven, M.; Tchetverikov, I.; Kok, M.R.; Gerards, A.H.; Hazes, J.; Luime, J.J. Modification of a sonographic enthesitis score to differentiate between psoriatic arthritis and young healthy volunteers. Scand. J. Rheumatol. 2018, 47, 291–294. [Google Scholar] [CrossRef] [PubMed]
- Polachek, A.; Cook, R.; Chandran, V.; Gladman, D.D.; Eder, L. The association between sonographic enthesitis and radiographic damage in psoriatic arthritis. Arthritis Res. Ther. 2017, 19, 189. [Google Scholar] [CrossRef]
- Harman, H.; Süleyman, E. Features of the Achilles tendon, paratenon, and enthesis in inflammatory rheumatic diseases: A clinical and ultrasonographic study. J. Rheumatol. 2018, 77, 511–521. [Google Scholar] [CrossRef]
- Lanfranchi, M.A.; Leluc, O.; Tavano, A.; Wormser, C.; Morange, S.; Chagnaud, C.; Pradel, V.; Lafforgue, P.; Pham, T. Are ultrasound findings similar in patients with axial spondyloarthritis and in athlete entheses? J. Rheumatol. 2017, 44, 609–612. [Google Scholar] [CrossRef]
- Fujikawa, K.; Kawashiri, S.-Y.; Endo, Y.; Mizokami, A.; Tsukada, T.; Mine, M.; Uetani, M.; Kawakami, A. Diagnostic efficacy of ultrasound detection of enthesitis in peripheral spondyloarthritis. Mod. Rheumatol. 2020, 30, 1060–1066. [Google Scholar] [CrossRef]
- Elnady, B.; el Shaarawy, N.K.; Dawoud, N.M.; Elkhouly, T.; de Desouky, S.; ElShafey, E.N.; el Husseiny, M.S.; Rasker, J.J. Subclinical synovitis and enthesitis in psoriasis patients and controls by ultrasonography in Saudi Arabia; incidence of psoriatic arthritis during two years. Clin. Rheumatol. 2019, 38, 1627–1635. [Google Scholar] [CrossRef]
- Macchioni, P.; Salvarani, C.; Possemato, N.; Gutierrez, M.; Grassi, W.; Gasparini, S.; Perricone, C.; Perrotta, F.M.; Grembiale, R.D.; Bruno, C.; et al. Ultrasonographic and clinical assessment of peripheral enthesitis in patients with psoriatic arthritis, psoriasis, and fibromyalgia syndrome: The ULISSE study. J. Rheumatol. 2019, 46, 904–911. [Google Scholar] [CrossRef]
- Tom, S.; Zhong, Y.; Cook, R.; Aydin, S.Z.; Kaeley, G.; Eder, L. Development of a preliminary ultrasonographic enthesitis score in psoriatic arthriti-GRAPPA ultrasound working group. J. Rheumatol. 2019, 46, 384–390. [Google Scholar] [CrossRef]
- Graceffa, D.; Bonifati, C.; Lora, V.; Saraceni, P.L.; de Felice, C.; Chimenti, M.S.; Perricone, R.; Morrone, A. Ultrasound assessment of enthesis thickness in psoriasis and psoriatic arthritis: A cross-sectional study. Indian J. Dermatol. Venereol. Leprol. 2019, 85, 175–181. [Google Scholar] [PubMed]
- Ruyssen-Witrand, A.; Jamard, B.; Cantagrel, A.; Nigon, D.; Loeuille, D.; Degboe, Y.; Constantin, A. Relationships between ultrasound enthesitis, disease activity and axial radiographic structural changes in patients with early spondyloarthritis: Data from DESIR cohort. RMD Open 2017, 3. [Google Scholar] [CrossRef]
- Ahmed, M.M.; Elolemy, G.G.; Alfeeli, A.K.; Baqer, A.B.; Gad, A.M. Ultrasonographic Enthesopathy and Disease Activity in Psoriatic Arthritis. Open Access Maced. J. Med. Sci. 2017, 5, 651–656. [Google Scholar] [CrossRef] [PubMed]
- Wink, F.; Bruyn, G.A.; Maas, F.; Griep, E.N.; van der Veer, E.; Bootsma, H.; Brouwer, E.; Arends, S.; Spoorenberg, A. Ultrasound evaluation of the entheses in daily clinical practice during tumor necrosis factor-α blocking therapy in patients with ankylosing spondylitis. J. Rheumatol. 2017, 44, 587–593. [Google Scholar] [CrossRef] [PubMed]
- Ward, I.M.; Kissin, E.; Kaeley, G.; Scott, J.N.; Newkirk, M.; Hildebrand, B.A.; Lospinoso, J.; Kohler, M.J.; Higgs, J.B. Ultrasound Features of the Posterior Tibialis Tendon and Peroneus Brevis Tendon Entheses: Comparison Study between Healthy Adults and Those With Inflammatory Arthritis. Arthritis Care Res. 2017, 69, 1519–1525. [Google Scholar] [CrossRef] [PubMed]
- Bertolini, E.; Macchioni, P.; Rizzello, F.; Salice, M.; Vukatana, G.; Sandri, G.; Bertani, A.; Ciancio, G.; Govoni, M.; Zelante, A.; et al. Ultrasonographic and clinical assessment of peripheral enthesitis and arthritis in an Italian cohort of inflammatory bowel disease patients. Semin. Arthritis Rheum. 2020, 50, 436–443. [Google Scholar] [CrossRef]
- Martinis, F.; Tinazzi, I.; Bertolini, E.; Citriniti, G.; Variola, A.; Geccherle, A.; Marchetta, A.; McGonagle, D.; MacChioni, P. Clinical and sonographic discrimination between fibromyalgia and spondyloarthopathy in inflammatory bowel disease with musculoskeletal pain. Rheumatology 2020, 59, 2857–2863. [Google Scholar] [CrossRef] [PubMed]
- Seven, S.; Pedersen, S.J.; Østergaard, M.; Felbo, S.K.; Sørensen, I.J.; Døhn, U.M.; Terslev, L. Peripheral Enthesitis Detected by Ultrasonography in Patients with Axial Spondyloarthritis—Anatomical Distribution, Morphology, and Response to Tumor Necrosis Factor-Inhibitor Therapy. Front. Med. 2020, 7, 341. [Google Scholar] [CrossRef]
- Ozsoy-Unubol, T.; Yagci, I. Is ultrasonographic enthesitis evaluation helpful for diagnosis of non-radiographic axial spondyloarthritis? Rheumatol. Int. 2018, 38, 2053–2061. [Google Scholar] [CrossRef] [PubMed]
- Ebstein, E.; Coustet, B.; Masson-Behar, V.; Forien, M.; Palazzo, E.; Dieudé, P.; Ottaviani, S. Enthesopathy in rheumatoid arthritis and spondyloarthritis: An ultrasound study. Jt. Bone Spine 2018, 85, 577–581. [Google Scholar] [CrossRef] [PubMed]
- Gandjbakhch, F.; Terslev, L.; Joshua, F.; Wakefield, R.J.; Naredo, E.; D’Agostino, M.-A.; Force, O.U.T. Ultrasound in the evaluation of enthesitis: Status and perspectives. Arthritis Res. Ther. 2011, 13, R188. [Google Scholar] [CrossRef]
- Terslev, L.; Naredo, E.; Iagnocco, A.; Balint, P.V.; Wakefield, R.J.; Aegerter, P.; Aydin, S.Z.; Bachta, A.; Hammer, H.B.; Bruyn, G.A.W.; et al. Defining Enthesitis in Spondyloarthritis by Ultrasound: Results of a Delphi Process and of a Reliability Reading Exercise. Arthritis Rheum. 2014, 66, 741–748. [Google Scholar] [CrossRef]
- Wakefield, R.J.; Balint, P.V.; Szkudlarek, M.; Filippucci, E.; Backhaus, M.; D’Agostino, M.-A.; Sanchez, E.N.; Iagnocco, A.; Schmidt, W.A.; Bruyn, G.A.W.; et al. Musculoskeletal ultrasound including definitions for ultrasonographic pathology. J. Rheumatol. 2005, 32, 2485–2487. [Google Scholar]
- Naredo, E.; Batlle-Gualda, E.; García-Vivar, M.L.; García-Aparicio, A.M.; Fernández-Sueiro, J.L.; Fernández-Prada, M.; Giner, E.; Rodriguez-Gomez, M.; Pina, M.F.; Medina-Luezas, J.A.; et al. Power Doppler ultrasonography assessment of entheses in spondyloarthropathies: Response to therapy of entheseal abnormalities. J. Rheumatol. 2010, 37, 2110–2117. [Google Scholar] [CrossRef] [PubMed]
- Hoksrud, A.; Ohberg, L.; Alfredson, H.; Bahr, R. Color doppler ultrasound findings in patellar tendinopathy (jumper’s knee). Am. J. Sports Med. 2008, 36, 1813–1820. [Google Scholar] [CrossRef]
- Czyrny, Z. Diagnostic anatomy and diagnostics of enthesal pathologies of the rotator cuff. J. Ultrason. 2012, 12, 178–187. [Google Scholar] [CrossRef] [PubMed]
- Dębek, A.; Nowicki, P.; Czyrny, Z. Ultrasonographic diagnostics of pain in the lateral cubital compartment and proximal forearm. J. Ultrason. 2012, 12, 188–201. [Google Scholar] [CrossRef][Green Version]
- Feydy, A.; Lavie-Brion, M.-C.; Gossec, L.; Lavie, F.; Guerini, H.; Nguyen, C.; Rannou, F.; Drapé, J.-L.; Dougados, M. Comparative study of MRI and power Doppler ultrasonography of the heel in patients with spondyloarthritis with and without heel pain and in controls. Ann. Rheum. Dis. 2011, 71, 498–503. [Google Scholar] [CrossRef] [PubMed]
- Czyrny, Z. Sonographic and histological appearance of heel enthesopathy, what the “heel spurs” really are and what are their consequences. J. Ortop. Trauma Surg. Relat. Res. 2010, 2, 23–36. [Google Scholar]
- Maffulli, N.; Kader, D. Tendonopathy of tendo Achillis. J. Bone Jt. Surg. 2002, 84, 1–8. [Google Scholar] [CrossRef]
- D’Agostino, M.A.; Aegerter, P.; Jousse-Joulin, S.; Chary-Valckenaere, I.; Lecoq, B.; Gaudin, P.; Brault, I.; Schmitz, J.; Dehaut, F.-X.; le Parc, J.-M.; et al. How to evaluate and improve the reliability of power Doppler ultrasonography for assessing enthesitis in spondyloarthritis. Arthritis Rheum. 2009, 61, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Helliwell, P.S.; Fitzgerald, O.; Fransen, J.; Gladman, D.D.; Kreuger, G.G.; Duffin, K.C.; McHugh, N.; Mease, P.; Strand, V.; Waxman, R.; et al. The development of candidate composite disease activity and responder indices for psoriatic arthritis (GRACE project). Ann. Rheum. Dis. 2012, 72, 986–991. [Google Scholar] [CrossRef]
- Kaeley, G.S. Enthesitis in psoriatic arthritis (Part 2): Imaging. Rheumatology 2020, 59, i15–i20. [Google Scholar] [CrossRef]
- Maffulli, N.; Denaro, V.; Loppini, M. Letters to the Editor. Foot Ankle Int. 2012, 33, 807–808. [Google Scholar] [CrossRef] [PubMed]
- Eder, L.; Jayakar, J.; Thavaneswaran, A.; Haddad, A.; Chandran, V.; Salonen, D.; Rosen, C.F.; Gladman, D.D. Is the Madrid Sonographic Enthesitis Index Useful for Differentiating Psoriatic Arthritis from Psoriasis Alone and Healthy Controls? J. Rheumatol. 2014, 41, 466–472. [Google Scholar] [CrossRef]
- van der Linden, S.; Valkenburg, H.A.; Cats, A. Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modifi cation of the New York criteria. Arthritis Rheum. 1984, 27, 361–368. [Google Scholar] [CrossRef]
- Spoorenberg, A.; de Vlam, K.; van der Heijde, D.; de Klerk, E.; Dougados, M.; Mielants, H.; van der Tempel, H.; Boers, M.; van der Linden, S. Radiological scoring methods in ankylosing spondylitis. Reliability and change over 1 and 2years. J. Rheumatol. 2004, 31, 125–132. [Google Scholar]
- Rahman, P.; Gladman, D.D.; Cook, R.J.; Zhou, Y.; Young, G.; Salonen, D. Radiological assessment in psoriatic arthritis. Br. J. Rheumatol. 1998, 37, 760–765. [Google Scholar] [CrossRef]
- Aydin, S.Z.; Ash, Z.R.; Tinazzi, I.; Castillo-Gallego, C.; Kwok, C.; Wilson, C.; Goodfield, M.; Gisondi, P.; Tan, A.L.; Marzo-Ortega, H.; et al. The link between enthesitis and arthritis in psoriatic arthritis: A switch to a vascular phenotype at insertions may play a role in arthritis development. Ann. Rheum. Dis. 2013, 72, 992–995. [Google Scholar] [CrossRef]
- Zellers, J.A.; Bley, B.C.; Pohlig, R.T.; Alghamdi, N.H.; Silbernagel, K.G. Frequency of Pathology on Diagnostic Ultrasound and Relationship to Patient Demographics in Individual with Insertional Achilles Tendonopathy. Int. J. Sports Phys. Ther. 2019, 14, 761–769. [Google Scholar] [CrossRef]
- Franceschi, F.; Papalia, R.; Paciotti, M.; Franceschetti, E.; Di Martino, A.; Maffulli, N.; Denaro, V. Obesity as a risk factor for tendonopathy: A systematic review. Int. J. Endocrinol. 2014, 1, 10. [Google Scholar]
- Scott, R.T.; Hyer, C.F.; Granata, A. The correlation of Achilles tendonopathy and body mass index. Foot Ankle Spec. 2013, 6, 283–285. [Google Scholar] [CrossRef] [PubMed]
- Gisondi, P.; Tinazzi, I.; El-Dalati, G.; Gallo, M.; Biasi, D.; Barbara, L.M.; Girolomoni, G. Lower limb enthesopathy in patients with psoriasis without clinical signs of arthropathy: A hospital-based case-control study. Ann. Rheum. Dis. 2008, 67, 26–30. [Google Scholar] [CrossRef] [PubMed]
- Aydin, S.Z.; Can, M.; Alibaz-Oner, F.; Keser, G.; Kurum, E.; Inal, V.; Yazisiz, V.; Birlik, M.; Emmungil, H.; Atagunduz, P.; et al. A relationship between spinal new bone formation in ankylosing spondylitis and the sonographically determined Achilles tendon enthesophytes. Rheumatol. Int. 2016, 36, 397–404. [Google Scholar] [CrossRef] [PubMed]
- Aydin, S.Z.; Filippucci, E.; Atagunduz, P.; Yavuz, S.; Grassi, W.; Direskeneli, H.; Aydin, S.Z. Sonographic measurement of Achilles tendon thickness in seronegative spondyloarthropathies. Eur. J. Rheumatol. 2014, 1, 7–10. [Google Scholar] [CrossRef]
- Fassio, A.; Giovannini, I.; Idolazzi, L.; Zabotti, A.; Iagnocco, A.; Sakellariou, G. Nail ultrasonography for psoriatic arthritis and psoriasis patients: A systematic literature review. Clin. Rheumatol. 2020, 39, 1391–1404. [Google Scholar] [CrossRef] [PubMed]
- Lai, T.L.; Pang, H.T.; Cheuk, Y.Y.; Yip, M.L. Psoriatic nail involvement and its relationship with distal interphalangeal joint disease. Clin. Rheumatol. 2016, 35, 2031–2037. [Google Scholar] [CrossRef]
- Alvarado, P.M.; Crespo, E.R.; Muñoz-Garza, F.; López-Ferrer, A.; Alonso, A.L.; Rull, E.V.; I Pou, J.C.; Sanz, L.P.; Casademont, J. Subclinical enthesopathy of extensor digitorum tendon is highly prevalent and associated with clinical and ultrasound alterations of the adjacent fingernails in patients with psoriatic disease. J. Eur. Acad. Dermatol. Venereol. 2018, 32, 1728–1736. [Google Scholar] [CrossRef] [PubMed]
- el Miedany, Y.; el Gaafary, M.; Youssef, S.; Ahmed, I.; Nasr, A. Tailored approach to early psoriatic arthritis patients: Clinical and ultrasonographic predictors for structural joint damage. Clin. Rheumatol. 2015, 34, 307–313. [Google Scholar] [CrossRef] [PubMed]
- Idolazzi, L.; Zabotti, A.; Fassio, A.; Errichetti, E.; Benini, C.; Vantaggiato, E.; Rossini, M.; de Vita, S.; Viapiana, O. The ultrasonographic study of the nail reveals differences in patients affected by inflammatory and degenerative conditions. Clin. Rheumatol. 2019, 38, 913–920. [Google Scholar] [CrossRef]
- Acosta-Felquer, M.L.; Ruta, S.; Rosa, J.; Marin, J.; Ferreyra-Garrot, L.; Galimberti, M.L.; Galimberti, R.; Garcia-Monaco, R.; Soriano, E.R. Ultrasound entheseal abnormalities at the distal interphalangeal joints and clinical nail involvement in patients with psoriasis and psoriatic arthritis, supporting the nail-enthesitis theory. Semin. Arthritis Rheum. 2017, 47, 338–342. [Google Scholar] [CrossRef] [PubMed]
- Kaeley, G.S.; Eder, L.; Aydin, S.Z.; Gutierrez, M.; Bakewell, C. Enthesitis: A hallmark of psoriatic arthritis. Semin. Arthritis Rheum. 2018, 48, 35–43. [Google Scholar] [CrossRef] [PubMed]
| Study | Up Ext | Low Ext | Sites | Hypo-Echo | Enthes-Ophytes | PD | Eros | Index | Ref. |
|---|---|---|---|---|---|---|---|---|---|
| BUSES | |||||||||
| Zuliani (2019) | CETLA | AT | 12 | Yes | Yes | Yes | Yes | BUSES | [48] |
| PF | |||||||||
| PT (P,D) | |||||||||
| QT | |||||||||
| Hartung (2018) | CETLA CFTME | AT | 14 | No | No | Yes | No | BUSES | [49] |
| PF | |||||||||
| PT (P,D) | |||||||||
| QT | |||||||||
| Florescu (2018) | CETLA | AT | 12 | Yes | Yes | Yes | Yes | BUSES | [50] |
| PF | |||||||||
| PT (P,D) | |||||||||
| QT | |||||||||
| Milutonivic (2017) | CETLA | AT | 12 | Yes | Yes | Yes | Yes | BUSES | [51] |
| PF | |||||||||
| PT (P,D) | |||||||||
| QT | |||||||||
| D’Agostino Score | |||||||||
| Yadav (2020) | CETLA CFTME | AT | 10 | Yes | Yes | Yes | Yes | D’Agostino | [52] |
| PT | |||||||||
| QT | |||||||||
| Zhang (2017) | CETLA | AT | 12 | Yes | Yes | Yes | Yes | D’Agostino | [53] |
| PF | |||||||||
| PT (D) | |||||||||
| QT | |||||||||
| GT | |||||||||
| GUESS | |||||||||
| Alhussain (2019) | None | AT | 10 | Yes | Yes | Yes | Yes | GUESS | [54] |
| PF | |||||||||
| PT (P,D) | |||||||||
| QT | |||||||||
| Moshrif (2017) | None | AT | 10 | Yes | Yes | Yes | Yes | GUESS | [55] |
| PF | |||||||||
| PT (P,D) | |||||||||
| QT | |||||||||
| MASEI | |||||||||
| Juan Molina Collada (2020) | TT | AT | 12 | Yes | Yes | Yes | Yes | MASEI | [56] |
| PF | |||||||||
| PT (P,D) | |||||||||
| QT | |||||||||
| Vyas (2020) | TT | AT | 12 | Yes | Yes | Yes | Yes | MASEI | [57] |
| PF | |||||||||
| PT (P,D) | |||||||||
| QT | |||||||||
| Macia-Villa (2019) | TT | AT | 12 | Yes | Yes | Yes | Yes | MASEI | [58] |
| PF | |||||||||
| PT (P,D) | |||||||||
| QT | |||||||||
| Ishida (2019) | TT | AT | 12 | Yes | Yes | Yes | Yes | MASEI | [59] |
| PF | |||||||||
| PT (P,D) | |||||||||
| QT | |||||||||
| Wervers (2019) | TT CETLA | AT | 14 | Yes | Yes | Yes | Yes | MASEI | [60] |
| PF | |||||||||
| PT (P,D) | |||||||||
| QT | |||||||||
| Wervers (2018) | TT CETLA | AT | 14 | Yes | Yes | Yes | Yes | MASEI | [61] |
| PF | |||||||||
| PT (P,D) | |||||||||
| QT | |||||||||
| Polachek (2017) | TT | AT | 12 | Yes | Yes | Yes | Yes | MASEI | [62] |
| PF | |||||||||
| PT (P,D) | |||||||||
| QT | |||||||||
| Harman (2018) | AT | 2 | Yes | Yes | Yes | Yes | MASEI | [63] | |
| Lanfranchi (2017) | TT | AT | Yes | Yes | Yes | Yes | MASEI | [64] | |
| PF | |||||||||
| PT (P,D) | |||||||||
| QT | |||||||||
| Other | |||||||||
| Fujikawa (2020) | CETLA | AT | 14 | No | Yes | Yes | Yes | Other | [65] |
| PT (P,D) | |||||||||
| QT | |||||||||
| MCL | |||||||||
| LCL | |||||||||
| Elnady (2019) | CETLA CFTME | AT | 12 | Yes | Yes | Yes | Yes | Other | [66] |
| PF | |||||||||
| PT (P, D) | |||||||||
| Macchioni (2019) | CETLA | AT | 14 | Yes | Yes | Yes | Yes | Other | [67] |
| PF | |||||||||
| PT (P,D) | |||||||||
| QT | |||||||||
| MCL | |||||||||
| Tom (2019) | CETLA | AT | 22 | Yes | Yes | Yes | Yes | Other | [68] |
| CFTME | PF | ||||||||
| TT | PT (P,D) | ||||||||
| ST | QT | ||||||||
| Deltoid | TPT | ||||||||
| Graceffa (2019) | TT CETLA | AT | 16 | No | Yes | Yes | Yes | Other | [69] |
| PF | |||||||||
| PT (P,D) | |||||||||
| PL | |||||||||
| MCL | |||||||||
| Poulain (2018) | CETLA | AT | 8 | No | No | Yes | No | Other | [44] |
| PT (P,D) | |||||||||
| Balint (2018) | CETLA | AT | 8 | Yes | Yes | Yes | Yes | Other | [46] |
| PT (P & D) | |||||||||
| Ruyssen-Witrand (2017) | CETLA | AT | 8 | No | Yes | Yes | Yes | Other | [70] |
| PT (P,D) | |||||||||
| Ahmed (2017) | None | AT | 4 | No | Yes | Yes | Yes | Other | [71] |
| PF | |||||||||
| Wink (2017) | CETLA CFTME | AT | 18 | Yes | Yes | Yes | Yes | Other | [72] |
| PF | |||||||||
| PT (P,D) | |||||||||
| QT | |||||||||
| PA | |||||||||
| GT | |||||||||
| Ward (2017) | None | PTT | 4 | Yes | Yes | Yes | Yes | Other | [73] |
| PBT | |||||||||
| Multiple Scores | |||||||||
| Bertolini (2020) | CETLA | AT | 12 | Yes | Yes | Yes | Yes | GUESS, MASEI | [74] |
| PF | |||||||||
| PT (P,D) | |||||||||
| QT | |||||||||
| Martinis (2020) | CETLA | AT | 12 | Yes | Yes | Yes | Yes | GUESS, MASEI | [75] |
| PF | |||||||||
| PT (P,D) | |||||||||
| QT | |||||||||
| Seven (2020) | CETLA TT | AT | 14 | Yes | Yes | Yes | Yes | GUESS, MASEI, SEI | [76] |
| PT (P,D) | |||||||||
| QT | |||||||||
| GT | |||||||||
| Ozsoy-Unubol (2018) | TT CETLA CFTME | AT | 18 | Yes | Yes | Yes | Yes | GUESS, MASEI, D’Agostino | [77] |
| PF | |||||||||
| PT (P,D) | |||||||||
| QT | |||||||||
| TA | |||||||||
| Ebstein (2018) | TT CETLA | AT | 14 | Yes | Yes | Yes | Yes | GUESS, MASEI | [78] |
| PF | |||||||||
| PT (P,D) | |||||||||
| QT |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mascarenhas, S.; Couette, N. A Systematic Review of the Inclusion of Non-Inflammatory Ultrasonographic Enthesopathy Findings in Enthesitis Scoring Indices. Diagnostics 2021, 11, 669. https://doi.org/10.3390/diagnostics11040669
Mascarenhas S, Couette N. A Systematic Review of the Inclusion of Non-Inflammatory Ultrasonographic Enthesopathy Findings in Enthesitis Scoring Indices. Diagnostics. 2021; 11(4):669. https://doi.org/10.3390/diagnostics11040669
Chicago/Turabian StyleMascarenhas, Sheryl, and Nina Couette. 2021. "A Systematic Review of the Inclusion of Non-Inflammatory Ultrasonographic Enthesopathy Findings in Enthesitis Scoring Indices" Diagnostics 11, no. 4: 669. https://doi.org/10.3390/diagnostics11040669
APA StyleMascarenhas, S., & Couette, N. (2021). A Systematic Review of the Inclusion of Non-Inflammatory Ultrasonographic Enthesopathy Findings in Enthesitis Scoring Indices. Diagnostics, 11(4), 669. https://doi.org/10.3390/diagnostics11040669





