Lung Ultrasonography in the Monitoring of Intraoperative Recruitment Maneuvers
Abstract
1. Introduction
2. Material and Methods
2.1. Ethic Statement
2.2. Patient Qualification
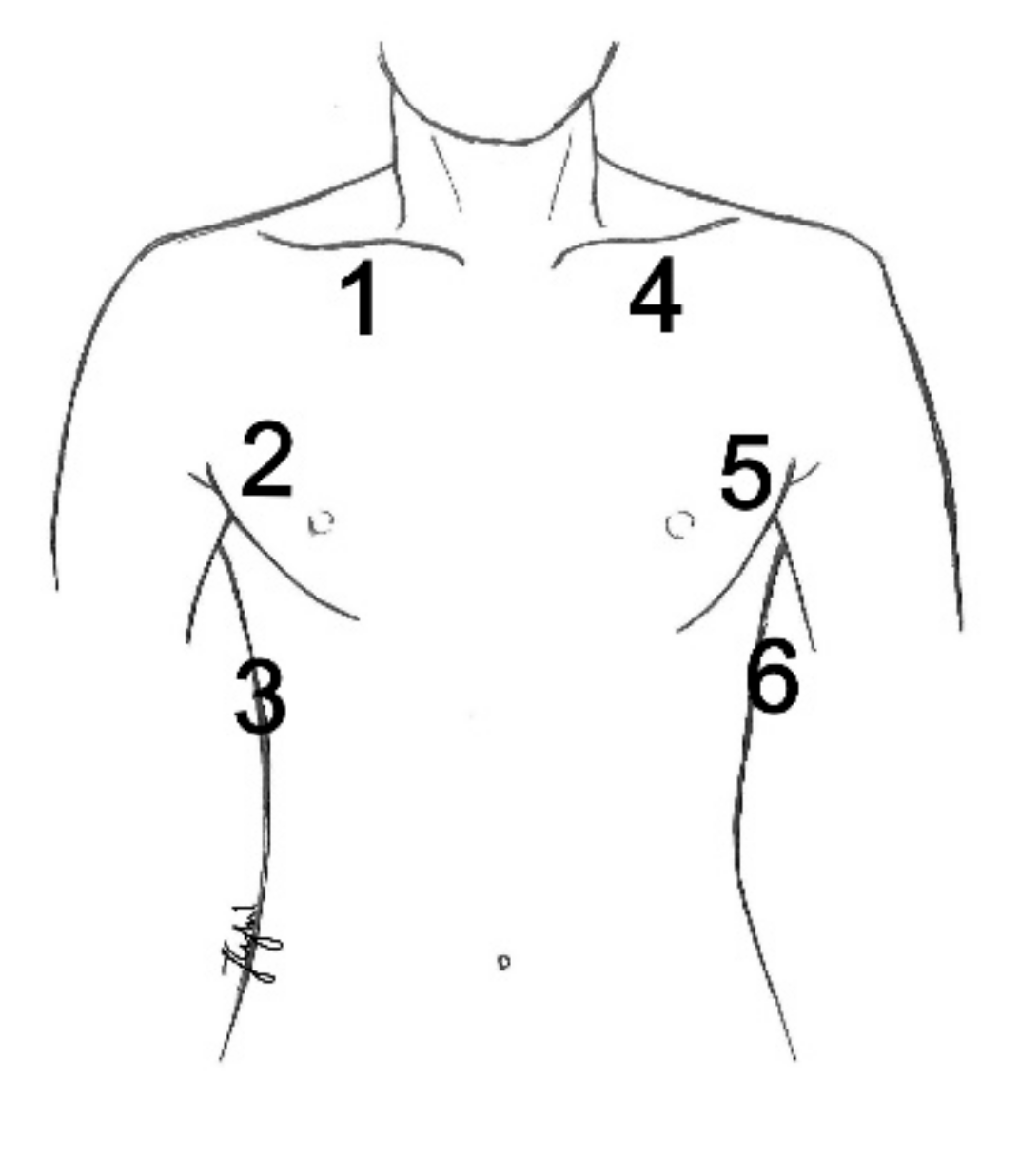
2.3. Ultrasound Technique and Settings
2.4. Initial Mechanical Ventilation Parameters
2.5. Intraoperative Ultrasound Assessment Protocol
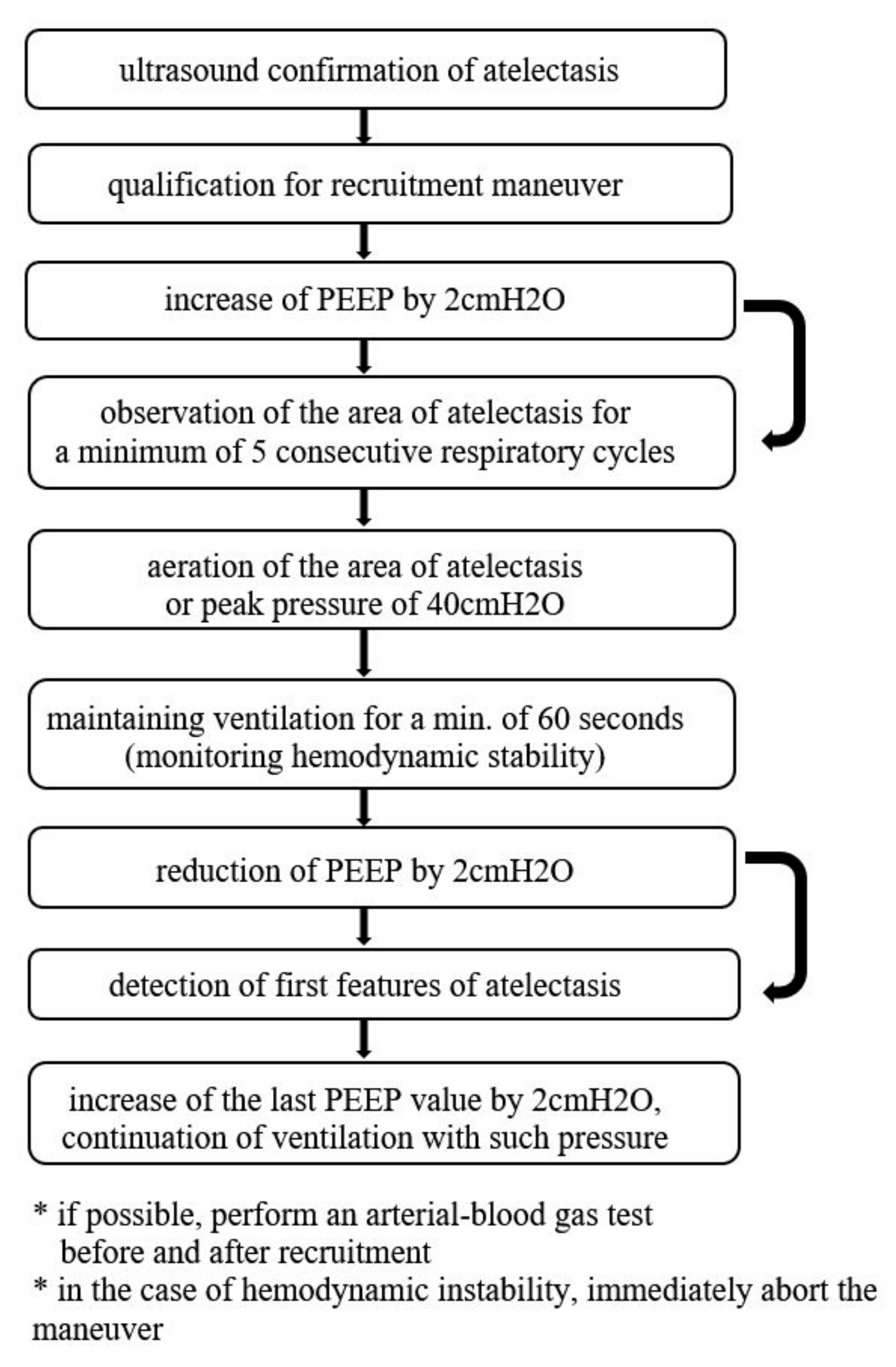
2.6. Recruitment Protocol in the Study Group
2.7. Statistical Analysis
3. Results
3.1. Analysis of the Study Group and the Control Group
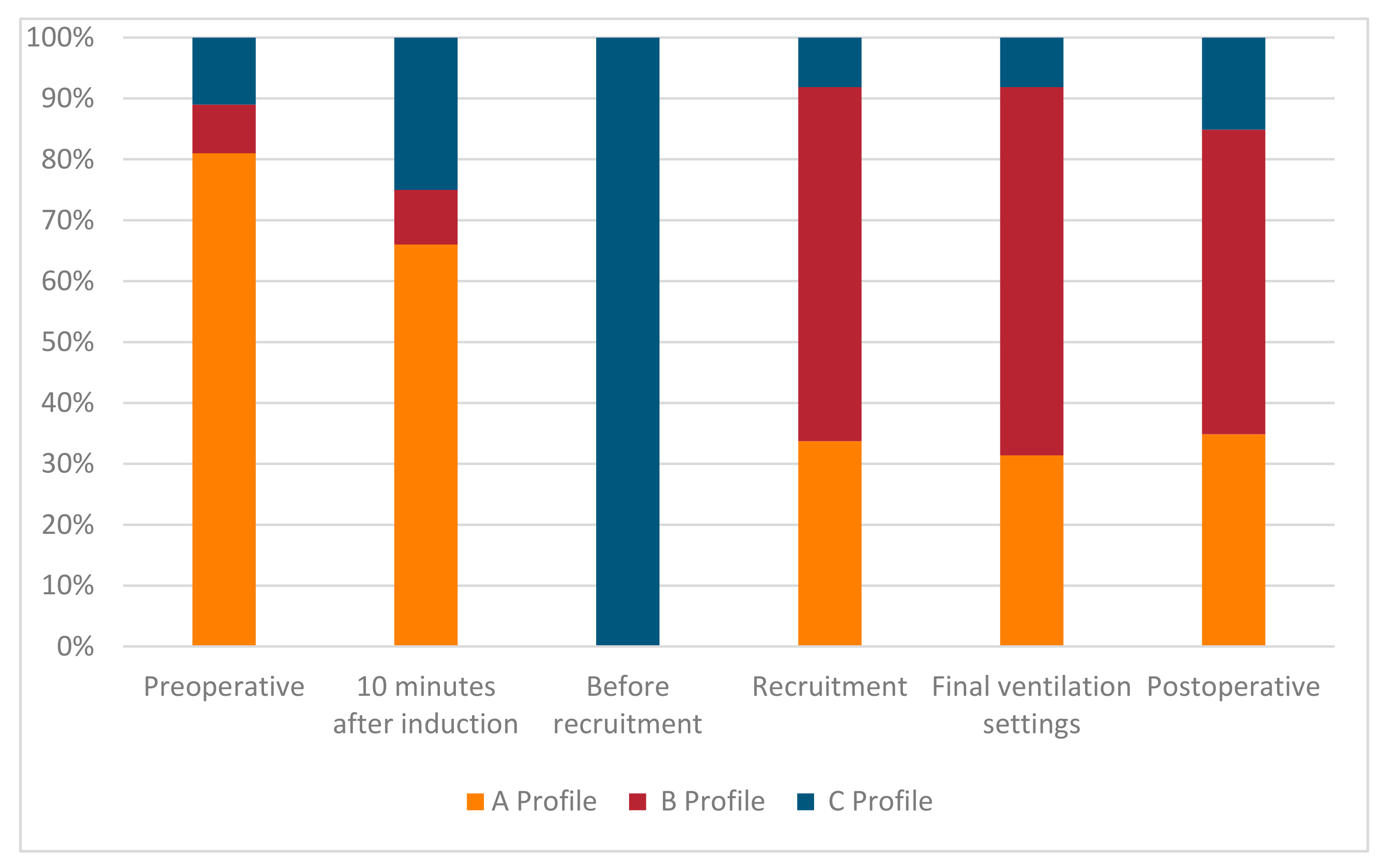
3.2. Preoperative Ultrasound Assessment
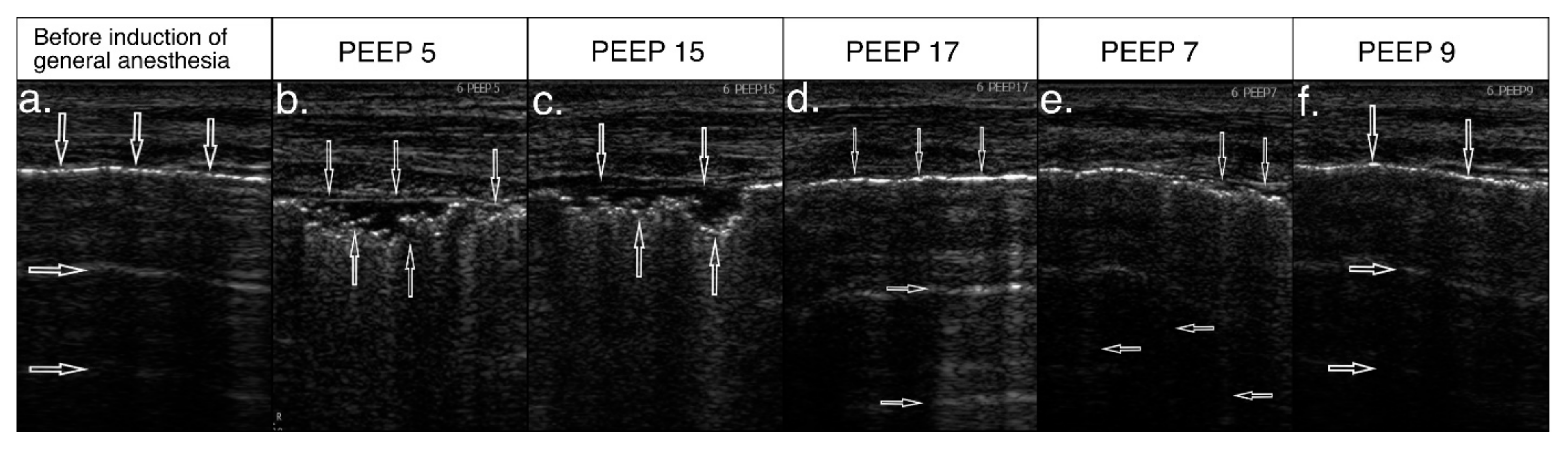
3.3. Intraoperative Ultrasound Assessment
3.4. Effect of Ultrasound-Guided Recruitment Maneuver
3.5. Postoperative Ultrasound Assessment
3.6. Analysis of Intraoperative Mechanical Ventilation Parameters
3.7. Analysis of Transcutaneous Oxygen Saturation in the Perioperative Period
3.8. Analysis of Changes in Lung Compliance in the Perioperative Period
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Brismar:, B.; Hedenstierna, G.; Lundquist, H.; Strandberg, Å.; Svensson, L.; Tokics, L. Pulmonary Densities during Anesthesia with Muscular Relaxation—A Proposal of Atelectasis. Anesthesiology 1985, 62, 422–428. [Google Scholar] [CrossRef] [PubMed]
- Ladha, K.; Vidal Melo, M.F.; McLean, D.J.; Wanderer, J.P.; Grabitz, S.D.; Kurth, T.; Eikermann, M. Intraoperative protective mechani-cal ventilation and risk of postoperative respiratory complications: Hospital-based registry study. BMJ 2015, 351, h3646. [Google Scholar] [CrossRef]
- Güldner, A.; Kiss, T.; Serpa Neto, A.; Hemmes, S.N.; Canet, J.; Spieth, P.M.; Rocco, P.R.; Schultz, M.J.; Pelosi, P.; Gama de Abreu, M. In-traoperative protective mechanical ventilation for prevention of postoperative pulmonary complications: A comprehensive review of the role of tidal volume, positive end-expiratory pressure, and lung recruitment maneuvers. Anesthesiology 2015, 123, 692–713. [Google Scholar] [CrossRef]
- Hemmes, S.N.; Serpa Neto, A.; Schultz, M.J. Intraoperative ventilatory strategies to prevent postoperative pulmonary complica-tions: A meta-analysis. Curr. Opin. Anaesthesiol. 2013, 26, 126–133. [Google Scholar] [CrossRef]
- Tusman, G.; Böhm, S.H. Prevention and reversal of lung collapse during the intra-operative period. Best Pr. Res. Clin. Anaesthesiol. 2010, 24, 183–197. [Google Scholar] [CrossRef]
- Tusman, G.; Böhm, S.H.; Warner, D.O.; Sprung, J. Atelectasis and perioperative pulmonary complications in high-risk patients. Curr. Opin. Anaesthesiol. 2012, 25, 1–10. [Google Scholar] [CrossRef]
- Steinberg, J.M.; Schiller, H.J.; Halter, J.M.; Gatto, L.A.; Lee, H.M.; Pavone, L.A.; Nieman, G.F. Alveolar instability causes early ventilator-induced lung injury independent of neutrophils. Am. J. Respir. Crit. Care Med. 2004, 169, 57–63. [Google Scholar] [CrossRef]
- Tremblay, L.N.; Slutsky, A.S. Ventilator-induced injury: From barotrauma to biotrauma. Proc. Assoc. Am. Physicians 1998, 110, 482–488. [Google Scholar] [PubMed]
- Halbertsma, F.J.J.; Vaneker, M.; Scheffer, G.J.; Van Der Hoeven, J.G. Cytokines and biotrauma in ventilator-induced lung injury: A critical review of the literature. Neth. J. Med. 2005, 63, 382–392. [Google Scholar]
- Hartland, B.L.; Newell, T.J.; Damico, N. Alveolar Recruitment Maneuvers Under General Anesthesia: A Systematic Review of the Literature. Respir. Care 2014, 60, 609–620. [Google Scholar] [CrossRef]
- Martin, J.B.; Garbee, D.; Bonanno, L. Effectiveness of positive end-expiratory pressure, decreased fraction of inspired oxygen and vital capacity recruitment maneuver in the prevention of pulmonary atelectasis in patients undergoing general anesthesia: A systematic review. JBI Database Syst. Rev. Implement. Rep. 2015, 13, 211–249. [Google Scholar] [CrossRef]
- He, H.; Yuan, S.; Yi, C.; Long, Y.; Zhang, R.; Zhao, Z. Titration of extra-PEEP against intrinsic-PEEP in severe asthma by electrical impedance tomography: A case report and literature review. Medicine 2020, 99, e20891. [Google Scholar] [CrossRef]
- Suzumura, E.A.; Amato, M.B.P.; Cavalcanti, A.B. Understanding recruitment maneuvers. Intensiv. Care Med. 2016, 42, 908–911. [Google Scholar] [CrossRef] [PubMed]
- Santos, R.S.; Silva, P.L.; Pelosi, P.; Rocco, P.R. Recruitment maneuvers in acute respiratory distress syndrome: The safe way is the best way. World J. Crit. Care Med. 2015, 4, 278–286. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.; Zhai, Z.; Zhao, Y.; Zhu, Z.; Tong, J.; Yan, J.; Ouyang, W. Performance of Lung Ultrasound in Detecting Peri-Operative Atelec-tasis after General Anesthesia. Ultrasound Med. Biol. 2016, 42, 2775–2784. [Google Scholar] [CrossRef] [PubMed]
- Monastesse, A.; Girard, F.; Massicotte, N.; Chartrand-Lefebvre, C.; Girard, M. Lung Ultrasonography for the Assessment of Peri-operative Atelectasis: A Pilot Feasibility Study. Anesth. Analg. 2017, 124, 494–504. [Google Scholar] [CrossRef]
- Wang, J.; Zhou, H.Y.; Du, Y.; Cao, F.F.; Zhang, Y.H.; Zhang, H.T. Diagnosis and treatment value of bedside pulmonary ultrasound for atelectasis in patients after cardiac surgery. Zhonghua Yi Xue Za Zhi 2020, 100, 220–224. [Google Scholar]
- Volpicelli, G.; Elbarbary, M.; Blaivas, M.; Lichtenstein, D.A.; Mathis, G.; Kirkpatrick, A.W.; Melniker, L.; Gargani, L.; Noble, V.E.; Via, G.; et al. International Liaison Committee on Lung Ultrasound (ILC-LUS) for International Consensus Conference on Lung Ultrasound (ICC-LUS). International evidence-based recommen-dations for point-of-care lung ultrasound. Intensiv. Care Med. 2012, 38, 577–591. [Google Scholar] [CrossRef]
- Bouhemad, B.; Mongodi, S.; Via, G.; Rouquette, I. Ultrasound for “lung monitoring” of ventilated patients. Anesthesiology 2015, 122, 437–447. [Google Scholar] [CrossRef]
- Myatra, S.N. Hemodynamic effects of alveolar recruitment maneuvres in the operating room: Proceed with caution. J. Anaesthesiol. Clin. Pharmacol. 2019, 35, 431–433. [Google Scholar] [CrossRef]
- Hanouz, J.L.; Coquerel, A.; Persyn, C.; Radenac, D.; Gérard, J.L.; Fischer, M.O. Changes in stroke volume during an alveolar recruit-ment maneuvers through a stepwise increase in positive end expiratory pressure and transient continuous positive airway pressure in anesthetized patients. A prospective observational pilot study. J. Anaesthesiol. Clin. Pharmacol. 2019, 35, 453–459. [Google Scholar] [CrossRef]
- Tusman, G.; Acosta, C.M.; Costantini, M. Ultrasonography for the assessment of lung recruitment maneuvers. Crit. Ultrasound J. 2016, 8, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Bello, G.; Blanco, P. Lung Ultrasonography for Assessing Lung Aeration in Acute Respiratory Distress Syndrome: A Narrative Review. J. Ultrasound Med. 2019, 38, 27–37. [Google Scholar] [CrossRef]
- Malbouisson, L.M.; Muller, J.C.; Constantin, J.M.; Lu, Q.; Puybasset, L.; Rouby, J.J.; CT Scan ARDS Study Group. Computed tomography assessment of positive end-expiratory pressure-induced alveolar recruitment in patients with acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 2001, 163, 1444–1450. [Google Scholar] [CrossRef]
- Caironi, P.; Gattinoni, L. How to monitor lung recruitment in patients with acute lung injury. Curr. Opin. Crit. Care 2007, 13, 338–343. [Google Scholar] [CrossRef]
- Wrigge, H.; Zinserling, J.; Muders, T.; Varelmann, D.; Günther, U.; von der Groeben, C.; Magnusson, A.; Hedenstierna, G.; Putensen, C. Electrical impedance tomography compared with thoracic computed tomography during a slow inflation maneuver in exper-imental models of lung injury. Crit. Care Med. 2008, 36, 903–909. [Google Scholar] [CrossRef]
- Spadaro, S.; Mauri, T.; Böhm, S.H.; Scaramuzzo, G.; Turrini, C.; Waldmann, A.D.; Ragazzi, R.; Pesenti, A.; Volta, C.A. Variation of poor-ly ventilated lung units (silent spaces) measured by electrical impedance tomography to dynamically assess recruitment. Crit. Care 2018, 22, 26. [Google Scholar] [CrossRef]
- Bouhemad, B.; Brisson, H.; Le-Guen, M.; Arbelot, C.; Lu, Q.; Rouby, J.-J. Bedside Ultrasound Assessment of Positive End-Expiratory Pressure–induced Lung Recruitment. Am. J. Respir. Crit. Care Med. 2011, 183, 341–347. [Google Scholar] [CrossRef]
- Rode, B.; Vučić, M.; Siranovi, ć; Siranović, M.; Horvat, A.; Krolo, H.; Kelečić, M.; Gopčević, A. Positive end-expiratory pressure lung recruitment: comparison between lower inflection point and ultrasound assessment. Wien. Klin. Wochenschr. 2012, 124, 842–847. [Google Scholar] [CrossRef]
- Chari, A.; Bousselmi, K.; Assar, W.; Kumar, V.; Khalil, E.; Kauts, V.; Abdelhakim, K. Usefulness of ultrasound in the management of acute respiratory distress syndrome. Int. J. Crit. Illn. Inj. Sci. 2019, 9, 11–15. [Google Scholar] [CrossRef]
- Lichtenstein, D.A. Lung Ultrasound in the Critically Ill; Springer: Berlin, Germany, 2016; Volume 20, pp. 315–322. [Google Scholar] [CrossRef]
- Volpicelli, G.; Melniker, L.A.; Cardinale, L.; Lamorte, A.; Frascisco, M.F. Lung ultrasound in diagnosing and monitoring pulmonary interstitial fluid. Radiol. Med. 2012, 118, 196–205. [Google Scholar] [CrossRef]
- Mojoli, F.; Bouhemad, B.; Mongodi, S.; Lichtenstein, D. Lung Ultrasound for Critically Ill Patients. Am. J. Respir. Crit. Care Med. 2019, 199, 701–714. [Google Scholar] [CrossRef]
- Buda, N.; Kosiak, W.; Wełnicki, M.; Skoczylas, A.; Olszewski, R.; Piotrkowski, J.; Skoczyński, S.; Radzikowska, E.; Jassem, E.; Grabczak, E.M.; et al. Recommendations for Lung Ultrasound in Internal Medicine. Diagnostics 2020, 10, 597. [Google Scholar] [CrossRef]
- Volpicelli, G.; Silva, F.; Radeos, M. Real-time lung ultrasound for the diagnosis of alveolar consolidation and interstitial syn-drome in the emergency department. Eur. J. Emerg. Med. 2010, 17, 63–72. [Google Scholar] [CrossRef]
- Généreux, V.; Chassé, M.; Girard, F.; Massicotte, N.; Chartrand-Lefebvre, C.; Girard, M. Effects of positive end-expiratory pres-sure/recruitment manoeuvres compared with zero end-expiratory pressure on atelectasis during open gynaecological surgery as assessed by ultrasonography: A randomised controlled trial. Br. J. Anaesth. 2020, 124, 101–109. [Google Scholar] [CrossRef]
- Song, I.-K.; Kim, E.-H.; Lee, J.-H.; Ro, S.; Kim, H.-S.; Kim, J.-T. Effects of an alveolar recruitment manoeuvre guided by lung ultrasound on anaesthesia-induced atelectasis in infants: A randomised, controlled trial. Anaesthesia 2017, 72, 214–222. [Google Scholar] [CrossRef]
- Lichtenstein, D. Fluid administration limited by lung sonography: The place of lung ultrasound in assessment of acute circula-tory failure (the FALLS-protocol). Expert Rev. Respir. Med. 2012, 6, 155–162. [Google Scholar] [CrossRef]
- Ricci, F.; Aquilani, R.; Radico, F.; Bianco, F.; Dipace, G.G.; Miniero, E.; De Caterina, R.; Gallina, S. Role and importance of ultrasound lung comets in acute cardiac care. Eur. Heart J. Acute Cardiovasc. Care 2015, 4, 103–112. [Google Scholar] [CrossRef]
- Bedetti, G.; Gargani, L.; Corbisiero, A.; Frassi, F.; Poggianti, E.; Mottola, G. Evaluation of ultrasound lung comets by hand-held echocardiography. Cardiovasc. Ultrasound 2006, 4, 34. [Google Scholar] [CrossRef]
- Frassi, F.; Gargani, L.; Gligorova, S.; Ciampi, Q.; Mottola, G.; Picano, E. Clinical and echocardiographic determinants of ultrasound lung comets. Eur. J. Echocardiogr. 2007, 8, 474–479. [Google Scholar] [CrossRef]
- Zawadka, M.; Marchel, M.; Andruszkiewicz, P. Diastolic dysfunction of the left ventricle—A practical approach for an anaesthe-tist. Anaesthesiol. Intensiv. Ther. 2020, 52, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Piotrkowski, J.; Buda, N.; Januszko-Giergielewicz, B.; Kosiak, W. Use of bedside ultrasound to assess fluid status: A literature re-view. Pol. Arch. Intern Med. 2019, 129, 692–699. [Google Scholar]
- Barbosa, F.T.; Castro, A.A.; De Sousa-Rodrigues, C.F. Positive end-expiratory pressure (PEEP) during anaesthesia for prevention of mortality and postoperative pulmonary complications. Cochrane Database Syst. Rev. 2014. [Google Scholar] [CrossRef]
- Bluth, T.; Serpa Neto, A.; Schultz, M.J.; Pelosi, P.; Gama de Abreu, M.; PROBESE Collaborative Group; Bluth, T.; Bobek, I.; Canet, J.C.; Cinnela, G.; et al. Effect of Intraoperative High Posi-tive End-Expiratory Pressure (PEEP) With Recruitment Maneuvers vs. Low PEEP on Postoperative Pulmonary Complications in Obese Patients: A Randomized Clinical Trial. JAMA 2019, 321, 2292–2305. [Google Scholar]
- Suzumura, E.A.; Figueiró, M.; Normilio-Silva, K.; Laranjeira, L.; Oliveira, C.; Buehler, A.M.; Bugano, D.; Amato, M.B.P.; Carvalho, C.R.R.; Berwanger, O.; et al. Effects of alveolar recruitment maneuvers on clinical outcomes in patients with acute respiratory distress syndrome: A systematic review and meta-analysis. Intensiv. Care Med. 2014, 40, 1227–1240. [Google Scholar] [CrossRef] [PubMed]
- Mauri, T.; Yoshida, T.; Bellani, G.; Goligher, E.; Carteaux, G.; Rittayamai, N.; Mojoli, F.; Chiumello, D.; Piquilloud, L.; Grasso, S.; et al. Esophageal and transpulmonary pres-sure in the clinical setting: Meaning, usefulness and perspectives. Int. Care Med. 2016, 42, 1360–1373. [Google Scholar] [CrossRef]
- Dreyfuss, D.; Soler, P.; Basset, G.; Saumon, G. High Inflation Pressure Pulmonary Edema: Respective Effects of High Airway Pressure, High Tidal Volume, and Positive End-expiratory Pressure. Am. Rev. Respir. Dis. 1988, 137, 1159–1164. [Google Scholar] [CrossRef]

| Variable | Data (n = 100) |
|---|---|
| Gender n (%) | |
| Females | 66 (66.0) |
| Males | 34 (34.0) |
| Age M(SD) | 63.90 (11.34) |
| BMI M(SD) | 28.31 (5.08) |
| ASA Score n (%) | |
| 1 | 1 (1.0) |
| 2 | 27 (27.0) |
| 3 | 66 (66.0) |
| 4 | 6 (6.0) |
| MRC Score n (%) | |
| 0 | 49 (49.0) |
| 1 | 40 (40.0) |
| 2 | 11 (11.0) |
| Coexisting chronic disease n (%) | |
| Hypertension | 55 (55.0) |
| Ischemic heart disease | 13 (13.0) |
| COPD | 1 (1.0) |
| Asthma | 6 (6.0) |
| Diabetes | 24 (24.0) |
| Atherosclerosis | 12 (12.0) |
| Type of surgery n (%) | |
| Elective | 90 (90.0) |
| Emergency | 10 (10.0) |
| Method n (%) | |
| Classic | 82 (82.0) |
| Laparoscopy | 18 (18.0) |
| Surgery duration n (%) | |
| <2 h | 45 (45.0) |
| 2–4 h | 44 (44.0) |
| >4 h | 11 (11.0) |
| Assessment | Atelectasis (N) n (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | Q(5) | p | |
| preoperative | 1% | 3% | 9% | 1% | 3% | 9% | 30.59 | <0.001 |
| 10 min. after induction | 1% | 3% | 20% | 1% | 5% | 23% | 85.17 | <0.001 |
| before recruitment | 2% | 10% | 92% | 2% | 13% | 92% | 343.00 | <0.001 |
| recruitment | 2% | 2% | 6% | 2% | 2% | 7% | 21.15 | 0.001 |
| final PEEP settings | 2% | 2% | 6% | 2% | 2% | 7% | 21.15 | 0.001 |
| 2 h after extubation | 2% | 2% | 10% | 2% | 2% | 13% | 40.33 | <0.001 |
| Assessment | Me | IQR | Min. | Max. |
|---|---|---|---|---|
| preoperatively | ||||
| Saturation | 96.00 | 2.00 | 88.00 | 99.00 |
| 10 min. after induction | ||||
| Saturation | 99.00 | 1.00 | 92.00 | 100.00 |
| Peak pressure | 15.50 | 3.00 | 12.00 | 25.00 |
| Compliance | 42.00 | 11.00 | 20.00 | 70.00 |
| PEEP | 5.00 | 0.00 | 5.00 | 5.00 |
| before recruitment | ||||
| Saturation | 99.00 | 2.00 | 92.00 | 100.00 |
| Peak pressure | 18.00 | 3.00 | 12.00 | 26.00 |
| Compliance | 34.00 | 11.25 | 19.00 | 60.00 |
| PEEP | 5.00 | 0.00 | 5.00 | 5.00 |
| recruitment | ||||
| Saturation | 99.00 | 0.00 | 96.00 | 100.00 |
| Peak pressure | 29.00 | 4.00 | 19.00 | 34.00 |
| PEEP | 17.00 | 2.50 | 9.00 | 19.00 |
| final ventilation settings | ||||
| Saturation | 99.00 | 0.00 | 98.00 | 100.00 |
| Peak pressure | 18.00 | 4.00 | 13.00 | 26.00 |
| Compliance | 47.00 | 15.50 | 29.00 | 89.00 |
| PEEP | 9.00 | 2.00 | 5.00 | 11.00 |
| 2 h after extubation | ||||
| Saturation | 99.00 | 0.00 | 97.00 | 100.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cylwik, J.; Buda, N. Lung Ultrasonography in the Monitoring of Intraoperative Recruitment Maneuvers. Diagnostics 2021, 11, 276. https://doi.org/10.3390/diagnostics11020276
Cylwik J, Buda N. Lung Ultrasonography in the Monitoring of Intraoperative Recruitment Maneuvers. Diagnostics. 2021; 11(2):276. https://doi.org/10.3390/diagnostics11020276
Chicago/Turabian StyleCylwik, Jolanta, and Natalia Buda. 2021. "Lung Ultrasonography in the Monitoring of Intraoperative Recruitment Maneuvers" Diagnostics 11, no. 2: 276. https://doi.org/10.3390/diagnostics11020276
APA StyleCylwik, J., & Buda, N. (2021). Lung Ultrasonography in the Monitoring of Intraoperative Recruitment Maneuvers. Diagnostics, 11(2), 276. https://doi.org/10.3390/diagnostics11020276







